Abstract
Free full text

Epidemiology of Type 2 Diabetes – Global Burden of Disease and Forecasted Trends
Abstract
The rising burden of type 2 diabetes is a major concern in healthcare worldwide. This research aimed to analyze the global epidemiology of type 2 diabetes. We analyzed the incidence, prevalence, and burden of suffering of diabetes mellitus based on epidemiological data from the Global Burden of Disease (GBD) current dataset from the Institute of Health Metrics, Seattle. Global and regional trends from 1990 to 2017 of type 2 diabetes for all ages were compiled. Forecast estimates were obtained using the SPSS Time Series Modeler. In 2017, approximately 462 million individuals were affected by type 2 diabetes corresponding to 6.28% of the world’s population (4.4% of those aged 15–49 years, 15% of those aged 50–69, and 22% of those aged 70+), or a prevalence rate of 6059 cases per 100,000. Over 1 million deaths per year can be attributed to diabetes alone, making it the ninth leading cause of mortality. The burden of diabetes mellitus is rising globally, and at a much faster rate in developed regions, such as Western Europe. The gender distribution is equal, and the incidence peaks at around 55 years of age. Global prevalence of type 2 diabetes is projected to increase to 7079 individuals per 100,000 by 2030, reflecting a continued rise across all regions of the world. There are concerning trends of rising prevalence in lower-income countries. Urgent public health and clinical preventive measures are warranted.
1. INTRODUCTION
Type 2 diabetes is recognized as a serious public health concern with a considerable impact on human life and health expenditures. Rapid economic development and urbanization have led to a rising burden of diabetes in many parts of the world [1]. Diabetes affects individuals’ functional capacities and quality of life, leading to significant morbidity and premature mortality [2]. Recently, concerns have been raised that more than one-third of the diabetes-related deaths occur in people under the age of 60 [3]. Increased consumption of unhealthy diets and sedentary lifestyles, resulting in elevated Body Mass Index (BMI) and fasting plasma glucose, have been blamed for these trends [4]. In particular, persons with higher BMI are more likely to have type 2 diabetes [5]. The aging of the human population is another contributor, as diabetes tends to affect older individuals [6]. The cost of diabetes care is at least 3.2 times greater than the average per capita healthcare expenditure, rising to 9.4 times in presence of complications [7]. Control of blood glucose, blood pressure, and other targets remains suboptimal for many patients [8]. This has been partly attributed to the lack of awareness and health promotion needed for diabetes control [9].
Unfortunately, the global epidemiology of diabetes has not been re-evaluated since the availability of recent high-quality data [10]. We found no studies providing global forecasts for the intermediate future, which would be a critical piece of information for health policymakers.
This research project examines the latest dataset of the Global Burden of Disease (GBD) to assess the burden of type 2 diabetes worldwide. The aim is to study the current global epidemiology of diabetes and highlight the current distribution of disease and emerging epidemiologic trends.
2. MATERIALS AND METHODS
We analyzed descriptive epidemiological data from the GBD dataset managed by the Institute of Health Metrics and Evaluation at the University of Washington, Seattle [11]. The GBD dataset is actively maintained and updated based on research data, epidemiology studies, and governmental publications from more than 100,000 sources. As a systematic public health project, it carefully builds models and statistical estimates for health loss due to illness, injury, and risk factors based on empirical data. GBD produces annual estimates of disease measures, such as prevalence, incidence, deaths, and Disability-Adjusted Life Years (DALYs). DALYs combine years of life lost due to premature death and years lived with disability, and are a more accurate reflection of human suffering resulting from a disease than prevalence or mortality alone.
We used the latest data refresh from GBD (the 2017 update). This dataset includes annual figures from 1990 to 2017 for type 2 diabetes in all countries and regions. We selected four world regions (Asia, Europe, America, and Africa) instead of other classification schemes based on economic development. All data were directly retrieved from GBD without any adjustments. Estimates were not age adjusted for differences in underlying population age distributions. Thus, the rates for different countries represent the actual burden on their respective health systems.
2.1. Statistical Data Analysis
Forecasting was conducted using IBM SPSS version 25 (IBM Corp., Armonk, NY, USA). The Time Series Modeler was used to develop a forecast model using the Expert Modeler option without any events. None of the observed values were marked as outliers.
3. RESULTS
Globally, an estimated 462 million individuals are affected by type 2 diabetes, corresponding to 6.28% of the world’s population (Table 1). More than 1 million deaths were attributed to this condition in 2017 alone, ranking it as the ninth leading cause of mortality. This is an alarming rise when compared with 1990, when type 2 diabetes was ranked as the eighteenth leading cause of deaths. In terms of human suffering (DALYs), diabetes ranks as the seventh leading disease.
Table 1
Disease burden of type 2 diabetes, 2017
| Region | Prevalence (cases per 100,000) | Burden of suffering (DALY per 100,000) |
|---|---|---|
| Global | 6059 | 751 |
| Europe | 8529 | 842 |
  Germany Germany | 9091 | 820 |
  France France | 6843 | 564 |
  Italy Italy | 9938 | 1083 |
  Spain Spain | 8796 | 773 |
  Netherlands Netherlands | 11,344 | 924 |
  Switzerland Switzerland | 10,040 | 815 |
  Sweden Sweden | 10,448 | 877 |
  Turkey Turkey | 6483 | 889 |
  Russia Russia | 6865 | 740 |
  United Kingdom United Kingdom | 8663 | 644 |
| Asia | 5961 | 729 |
  China China | 6262 | 635 |
  India India | 4770 | 663 |
  Japan Japan | 6737 | 553 |
  South Korea South Korea | 8835 | 1044 |
  Taiwan Taiwan | 10,012 | 1294 |
  Saudi Arabia Saudi Arabia | 7661 | 623 |
  Iran Iran | 7000 | 851 |
  Australia Australia | 5235 | 593 |
| America | 7060 | 1036 |
  United States United States | 8911 | 1046 |
  Canada Canada | 7095 | 829 |
  Brazil Brazil | 4240 | 780 |
| Africa | 3916 | 537 |
  South Africa South Africa | 7360 | 1374 |
The prevalence of type 2 diabetes shows a distribution pattern that matches socio-economic development (Figure 1). Developed regions, such as Western Europe, show considerably higher prevalence rates that continue to rise despite public health measures (Figure 2). The rate of increase does not appear to be slowing down.

Global distribution of diabetes mellitus type 2 prevalence. Note: Colors indicate prevalence rates per 100,000 population in 2017.
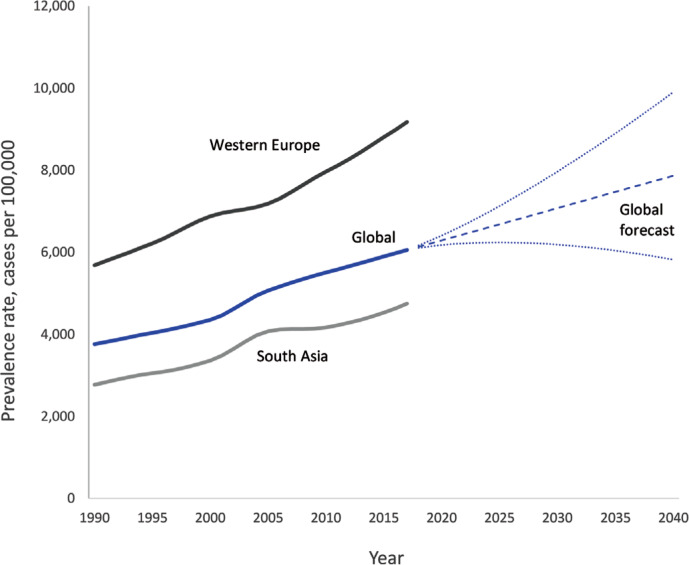
Trends in the prevalence of type 2 diabetes. Note: Forecast estimates using SPSS Time Series Modeler (Ljung Box Q, p = 0.16). Dotted lines indicate upper and lower confidence limits.
Remarkably, certain regions, such as Pacific Ocean island nations, are sustaining the highest prevalence of disease. These countries include Fiji (20,277 per 100,000), Mauritius (18,545), American Samoa (18,312), and Kiribati (17,432). Southeast Asian countries, such as Indonesia, Malaysia, Thailand, and Vietnam, have moved up the ranks in the last two decades. Owing to their large population sizes, China (88.5 million individuals with type 2 diabetes), India (65.9 million), and the US (28.9 million) retain the top spots as the countries with the greatest total number of individuals with this condition.
Males show a slightly higher prevalence than females (6219 compared with 5898 cases per 100,000), although this difference is within the margin of uncertainty. The age of onset of new diagnosis is also somewhat earlier among males and shows expected patterns of rising prevalence with increasing age, whereas the incidence peaks at 55–59 years (Figure 3). There appears to be no major shift in the age distribution from 1990 to 2017.

Age distribution of diabetes mellitus type 2, worldwide. (A) Incidence vs. prevalence (both 2017). (B) Incidence in 1990 vs. 2017. p < 0.0001, chi-square test.
Even though it afflicts individuals later in life, type 2 diabetes ranks seventh among the leading causes of disability and years of life lost (DALYs). It has jumped ranks from nineteenth position in 1990, indicating a global transition in disease patterns toward noncommunicable diseases.
Statistical forecasting using a model based on the 1990–2017 data showed that global diabetes prevalence could increase to 7079 per 100,000 by 2030 and 7862 by 2040. This estimate for 2040 is flanked by an upper confidence limit of 9904 and a lower limit of 5821 per 100,000.
4. DISCUSSION
This study reports on the current trends in the global burden of diabetes with emphasis on the burden of human suffering. The high prevalence of type 2 diabetes worldwide continues to rise, and there are no signs of it stabilizing. A concerning finding is the rapidly rising burden in lower-income countries. These findings have implications for health policy planners, physicians, healthcare professionals, and the public.
The burden of suffering due to diabetes, as measured by DALYs, is increasing despite significant investment in clinical care and pharmaceutical research. This increase is in excess of population growth and aging. Notably, Western Europe has a rate of increase greater than that of global and Asian averages. Even with the high levels of clinical and public health expenditure, this region is losing the battle against diabetes. One explanation might be non-modifiable risk factors, such as age and family history [12]. However, factors like a highly processed, calorie-dense western diet and a sedentary lifestyle may also be contributing. Developed countries like Italy and the US endure the highest burdens of human suffering (DALYs) due to diabetes. Advanced economies in Asia, such as South Korea and Taiwan, are joining the ranks of these countries, based on GBD data. Thus, our findings support the correlation between diabetes and economic development [13]. We speculate that our current approach to diabetes management, which focuses on expensive oral medications and insulin, is not working. Lowering blood glucose levels is perhaps not sufficient by itself nor effective in reducing all-cause mortality among these patients.
Prevention of new cases of diabetes appears to be not working as well based on our findings from global data. Although research is ongoing to reduce the progression from metabolic syndrome and prediabetes to diabetes, most interventions being tried seem to be unsuccessful in affecting the incidence. According to our data, there is no evidence of a decrease in incidence. Alarmingly high incidence rates recorded in island nations in the Pacific region are an indication of the interaction between genetic predisposition and the effect of rapid nutritional change on these indigenous populations. Meanwhile, the sheer number of individuals with diabetes is testing health systems in China, India, and the US to the limit. Rapid urbanization and its effects on diet and lifestyle has been implicated [14]. These findings have direct implications for health systems planning and resource allocation. Clearly, hospital-based management and subspecialist care are not sustainable strategies. Resource allocation in healthcare budgets for prevention of diabetes needs to be comparable to expenditures on treatment. Strengthening of primary care and community restructuring for active lifestyles and healthy nutrition are perhaps more likely to be cost effective [15]. Sadly, the rising tide of type 2 diabetes is out pacing preventive efforts by a wide margin [16].
The rising incidence of type 2 diabetes at earlier ages warrants closer attention. Previous clinic-based studies have reported a high number of young adults being diagnosed with type 2 diabetes, most of whom are obese [17]. There appears to be an age gradient with early-onset type 2 diabetes patients (those younger than 45) showing more obesity, dyslipidemia, smoking, sedentary lifestyles, and low-grade inflammation [18]. In our study, although the incidence of diabetes in young adults has increased over the past decades, the rise is across all ages. Thus, there appears to be no clear indication that the age of onset of type 2 diabetes has shifted to younger age groups. In any case, rising life expectancy in many countries will lead to a substantially greater burden of diabetes in the elderly.
The main limitations of our study include reliance on secondary data, which in turn is affected by the accuracy of measurement, changes in case definition, and heterogeneity in study designs. Yet as GBD evolves and matures, its estimation techniques have become more accurate and reliable. These statistical estimates provide a more complete and continuous picture of disease epidemiology than relying on raw data from isolated studies [11]. Ultimately, the goal is to guide decision making in clinical care and public health policy.
5. CONCLUSION
Type 2 diabetes continues to increase in prevalence, incidence, and as a leading cause of human suffering and deaths. Despite significant investments in clinical care, research, and public health interventions, there appears to be no sign of reduction in the rate of increase. Certain regions of the world, such as Western Europe and island states in the Pacific, are experiencing a disproportionately high burden. This epidemic will require an urgent and unwavering commitment to aggressive solutions at national levels with public policies, public health funding, and economic incentives for local communities to start diabetes prevention programs. Healthy eating options need to be subsidized, and unhealthy foods need to be taxed or otherwise disincentivized. Healthcare organizations and individual healthcare providers from multiple disciplines (doctors, nurses, pharmacists, dieticians, and diabetes educators) must be given time and resources to collaborate as they educate and care for individual and groups of patients. Unless urgent measures are instituted to reduce unhealthy eating, sedentary lifestyles, rapid urbanization, and other factors related to economic development, the burden of diabetes is expected to continue rising.
ACKNOWLEDGMENT
We would like to thank the Institute of Health Metrics, Seattle for compiling global epidemiological statistics and allowing access to data.
Footnotes
Data availability statement: The data that support the findings of this study are openly available in Global Health Data Exchange by the Institute of Health Metrics at http://ghdx.healthdata.org/gbd-results-tool.
AUTHORS’ CONTRIBUTION
MK contributed to writing the manuscript including the literature review. MJH designed the study/basic concept, wrote sections of the manuscript, analyzed the data, and provided overall supervision of the study. JK wrote parts of the manuscripts, proofread, and provided insights into the interpretation. RDG revised the manuscript and provided additional interpretation of results. HM compiled data and wrote the table. JAK revised and proofread the manuscript and provided additional interpretation of results.
FUNDING
This study did not receive any external grants from government, private or commercial sources.
REFERENCES
Articles from Journal of Epidemiology and Global Health are provided here courtesy of Springer
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/104420413
Article citations
Development of a Core Outcome Set for Studies Assessing Interventions for Diabetes-Related Foot Ulceration.
Diabetes Care, 47(11):1958-1968, 01 Nov 2024
Cited by: 0 articles | PMID: 39240785 | PMCID: PMC11502534
Review Free full text in Europe PMC
Relationship of serum calcium concentration with chronic kidney disease and mortality in type 2 diabetes mellitus patients: evidence from the NHANES 1999-2018.
Int Urol Nephrol, 15 Nov 2024
Cited by: 0 articles | PMID: 39546190
Integrative analysis of gene expression, protein abundance, and metabolomic profiling elucidates complex relationships in chronic hyperglycemia-induced changes in human aortic smooth muscle cells.
J Biol Eng, 18(1):61, 29 Oct 2024
Cited by: 0 articles | PMID: 39473010 | PMCID: PMC11523773
Association of ultra-processed food consumption with cardiovascular risk factors among patients with type-2 diabetes mellitus.
Nutr Diabetes, 14(1):89, 22 Oct 2024
Cited by: 0 articles | PMID: 39433734 | PMCID: PMC11494205
The population-specific Thr44Met OCT3 coding variant affects metformin pharmacokinetics with subsequent effects on insulin sensitivity in C57Bl/6J mice.
Diabetologia, 18 Oct 2024
Cited by: 0 articles | PMID: 39422716
Go to all (949) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017.
BMC Med, 17(1):191, 24 Oct 2019
Cited by: 170 articles | PMID: 31647003 | PMCID: PMC6813111
The burden of diabetes and hyperglycemia in Brazil: a global burden of disease study 2017.
Popul Health Metr, 18(suppl 1):9, 30 Sep 2020
Cited by: 12 articles | PMID: 32993680 | PMCID: PMC7526086
Trends in prevalence and incidence of scabies from 1990 to 2017: findings from the global Burden of disease study 2017.
Emerg Microbes Infect, 9(1):813-816, 01 Dec 2020
Cited by: 18 articles | PMID: 32284022 | PMCID: PMC7241492
Tuberculosis
The International Bank for Reconstruction and Development / The World Bank, Washington (DC), 14 Sep 2018
Cited by: 0 articles | PMID: 30212088
ReviewBooks & documents Free full text in Europe PMC



