Abstract
Free full text

Correction to: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China
Correction to: Intensive Care Med https://doi.org/10.1007/s00134-020-05991-x
The original version of this article unfortunately contained mistakes. There is an incorrect unit of IL-6 in Fig. 1 and Supplementary Table 1. It should be pg/mL rather than ng/mL. The corrected Fig. 1 and Supplementary Table 1 can be found below. The authors apologize for the mistakes.
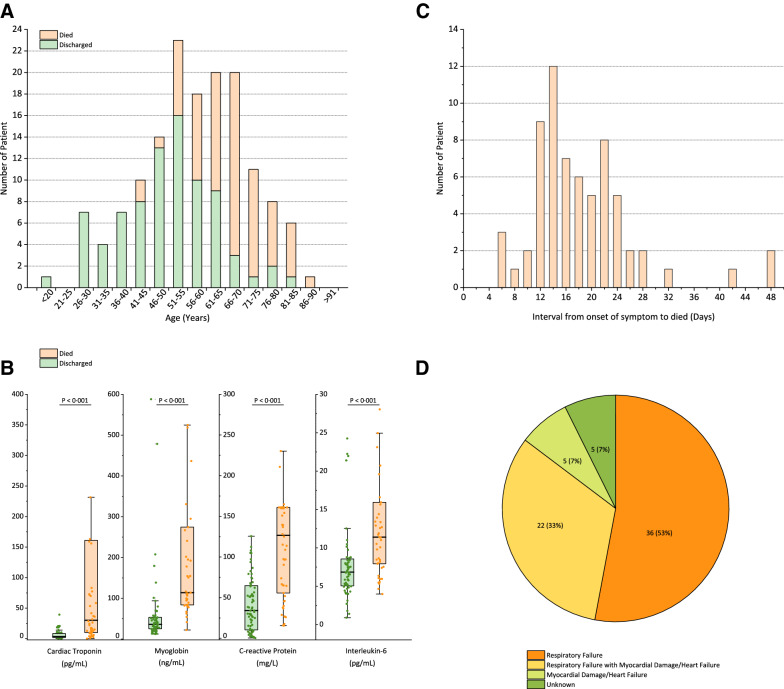
a Age distribution of patients with confirmed COVID-19; b key laboratory parameters for the outcomes of patients with confirmed COVID-19; c interval from onset of symptom to death of patients with confirmed COVID-19; d summary of the cause of death of 68 died patients with confirmed COVID-19
Supplementary Table 1: Summary of clinical features and laboratory results of the patients with confirmed COVID-19
| Normal Range | Died
(N  = = 68) 68)
| Discharged
(N  = = 82) 82)
| p-value | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 67 (15-81) | 50 (44-81) | <0.001 | |
| Sex | ||||
| Male | 49 (72%) | 53 (65%) | ||
| Female | 19 (28%) | 29 (35%) | ||
| Comorbidities | 43 (63%) | 34 (41%) | 0.01 | |
| Hypertension | 29 (43%) | 23 (28%) | 0.07 | |
| Cardiovascular disease | 13 (19%) | 0 | <0.001 | |
| Diabetes | 12 (18%) | 13 (16%) | 0.88 | |
| Cerebrovascular disease | 7 (10%) | 5 (6%) | 0.49 | |
| Chronic obstructive pulmonary disease | 2 (3%) | 1 (1%) | 0.59 | |
| Chronic kidney disease | 2 (3%) | 0 | 0.20 | |
| Malignancy | 2 (3%) | 1 (1%) | 0.59 | |
| Chronic liver disease | 1 (1%) | 3 (4%) | 0.63 | |
| Connective tissue disease | 1 (1%) | 0 | 0.45 | |
| Signs and Symptoms | ||||
| Fever | 59 (87%) | 68 (83%) | 0.67 | |
| Cough | 51 (75%) | 59 (72%) | 0.81 | |
| Sputum production | 29 (43%) | 25 (30%) | 0.17 | |
| Fatigue | 15 (22%) | 22 (27%) | 0.63 | |
| Myalgia | 9 (13%) | 10 (12%) | 1 | |
| Haemoptysis | 3 (4%) | 0 | 0.09 | |
| Dyspnea | 59 (87%) | 51 (62%) | 0.001 | |
| Respiratory failure | 58 (85%) | 13 (16%) | <0.001 | |
| ARDS | 55 (81%) | 7 (9%) | <0.001 | |
| Acute kidney injury | 21 (31%) | 2 (2%) | <0.001 | |
| Infection | 11 (16%) | 1 (1%) | 0.002 | |
| Treatments | ||||
| ICU admission | 30 (44%) | 11 (13%) | <0.001 | |
| High flow nasal cannula | 31 (46%) | 10 (12%) | <0.001 | |
| Non-invasive mechanical ventilation | 46 (68%) | 5 (6%) | <0.001 | |
| Invasive mechanical ventilation | 25 (37%) | 0 | <0.001 | |
| ECMO | 7 (10%) | 0 | 0.003 | |
| CRRT | 5 (7%) | 0 | 0.02 | |
| Prone position mechanical ventilation | 3 (4%) | 0 | 0.09 | |
| Antiviral treatment | 33 (49%) | 55 (67%) | 0.05 | |
| Antibiotic treatment | 63 (93%) | 80 (98%) | 0.66 | |
| Antifungal treatment | 12 (18%) | 5 (6%) | 0.04 | |
| Glucocorticoid treatment | 31 (46%) | 22 (27%) | 0.02 | |
| Time from onset of symptom to start of Glucocorticoid treatment, days | 11.7 (6.9) | 11.4 (4.4) | 0.89 | |
| Time from hospital admission to start of Glucocorticoid treatment, days | 1.5 (1.2) | 3.2 (2.7) | 0.01 | |
| Glucocorticoid treatment duration, days | 7.2 (6.7) | 7.0 (5.0) | 0.92 | |
| Supportive therapy | 45 (66%) | 18 (22%) | <0.001 | |
| Length of stay, days | 7.4 (5.5) | 12.3 (4.4) | <0.001 | |
| Laboratory Findings | ||||
| Time from onset of symptom to test, days | 11.6 (6.8) | 9.8 (4.3) | 0.07 | |
White blood cell count, × × 109/L 109/L | 3.50-9.50 | 10.62 (4.76) | 6.76 (3.49) | <0.001 |
Lymphocyte count, × × 109/L 109/L | 1.10-3.20 | 0.60 (0.32) | 1.42 (2.14) | <0.001 |
| Haemoglobin, g/L | 130.0-175.0 | 127.0 (16.7) | 127.6 (16.3) | 0.82 |
Platelet count, × × 109/L 109/L | 125.0-350.0 | 173.6 (67.7) | 222.1 (78.0) | <0.001 |
| Albumin, g/L | 35.0-52.0 | 28.8 (3.8) | 32.7 (3.8) | <0.001 |
| Alanine aminotransferase, U/L | 9.0-50.0 | 170.8 (991.6) | 48.68 (83.1) | 0.35 |
| Aspartate aminotransferase, U/L | 15.0-40.0 | 288.9 (1875.5) | 40.7 (57.8) | 0.31 |
| Total bilirubin, μmol/L | 0.0-26.0 | 18.1 (10.7) | 12.8 (6.8) | 0.001 |
| Blood urea nitrogen, mmol/L | 3.1-8.0 | 8.65 (4.5) | 5.11 (2.1) | <0.001 |
| Creatinine, umol/L | 59.0-104.0 | 91.2 (56.2) | 72.1 (22.2) | 0.02 |
| Creatine kinase, U/L | 50.0-310.0 | 319.4 (838.5) | 231.7 (862.3) | 0.56 |
| Lactate dehydrogenase, U/L | 120.0-250.0 | 905.8 (2619.1) | 297.9 (110.4) | 0.08 |
| Cardiac troponin, pg/mL | 2.0-28.0 | 30.3 (151.0) | 3.5 (6.2) | <0.001 |
| Myoglobin, ng/mL | 0.0-146.9 | 258.9 (307.6) | 77.7 (136.1) | <0.001 |
| C-reactive protein, mg/L | 0.0-5.0 | 126.6 (106.3) | 34.1 (54.5) | <0.001 |
| Interleukin-6, pg/mL | 0.0-7.0 | 11.4 (8.5) | 6.8 (3.61) | <0.001 |
| Serum ferritin, ng/mL | 21.8-274.7 | 1297.6 (1030.9) | 614.0 (752.2) | <0.001 |
Data are n (%), n/N (%), mean (SD), and median (IQR). When the data were normally distributed, continuous variables were then described using median and interquartile range (IQR) values.
ARDS =
= acute respiratory distress syndrome. ECMO
acute respiratory distress syndrome. ECMO =
= extracorporeal membrane oxygenation. ICU
extracorporeal membrane oxygenation. ICU =
= intensive care unit. CRRT
intensive care unit. CRRT =
= continuous renal replacement therapy.
continuous renal replacement therapy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Full text links
Read article at publisher's site: https://doi.org/10.1007/s00134-020-06028-z
Read article for free, from open access legal sources, via Unpaywall:
https://link.springer.com/content/pdf/10.1007/s00134-020-06028-z.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1007/s00134-020-06028-z
Article citations
Inactivated vaccine dosage and serum IgG levels correlate with persistent COVID-19 infections in hematologic malignancy patients during the Omicron Surge in China.
BMC Infect Dis, 24(1):1141, 11 Oct 2024
Cited by: 0 articles | PMID: 39394593 | PMCID: PMC11468290
Postorotracheal intubation dysphagia in patients with COVID-19: A retrospective study.
Sao Paulo Med J, 142(6):e2022608, 24 May 2024
Cited by: 0 articles | PMID: 38808794 | PMCID: PMC11126317
Precision nutrition to reset virus-induced human metabolic reprogramming and dysregulation (HMRD) in long-COVID.
NPJ Sci Food, 8(1):19, 30 Mar 2024
Cited by: 2 articles | PMID: 38555403 | PMCID: PMC10981760
Review Free full text in Europe PMC
COVID-19 Associated Cardiovascular Disease-Risks, Prevention and Management: Heart at Risk Due to COVID-19.
Curr Issues Mol Biol, 46(3):1904-1920, 29 Feb 2024
Cited by: 1 article | PMID: 38534740 | PMCID: PMC10969474
Review Free full text in Europe PMC
Characteristics of Suspected COVID-19 Discharged Emergency Department Patients Who Returned During the First Wave.
West J Emerg Med, 24(3):405-415, 03 Apr 2023
Cited by: 0 articles | PMID: 37278789 | PMCID: PMC10284524
Go to all (119) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
The Clinical Manifestations and Chest Computed Tomography Findings of Coronavirus Disease 2019 (COVID-19) Patients in China: A Proportion Meta-Analysis.
Clin Exp Otorhinolaryngol, 13(2):95-105, 01 May 2020
Cited by: 24 articles | PMID: 32434310 | PMCID: PMC7248616
Clinical outcomes of COVID-19 in Wuhan, China: a large cohort study.
Ann Intensive Care, 10(1):99, 31 Jul 2020
Cited by: 69 articles | PMID: 32737627 | PMCID: PMC7393341
Strongly Heterogeneous Transmission of COVID-19 in Mainland China: Local and Regional Variation.
Front Med (Lausanne), 7:329, 19 Jun 2020
Cited by: 17 articles | PMID: 32637423 | PMCID: PMC7317008
Epidemiological and clinical characteristics of COVID-19 patients in Hengyang, Hunan Province, China.
World J Clin Cases, 8(12):2554-2565, 01 Jun 2020
Cited by: 20 articles | PMID: 32607332 | PMCID: PMC7322431

 4
4



