Abstract
Importance
In late December 2019, an outbreak caused by a novel severe acute respiratory syndrome coronavirus 2 emerged in Wuhan, China. Data on the clinical characteristics and outcomes of infected patients in urban communities in the US are limited.Objectives
To describe the clinical characteristics and outcomes of patients with coronavirus disease 2019 (COVID-19) and to perform a comparative analysis of hospitalized and ambulatory patient populations.Design, setting, and participants
This study is a case series of 463 consecutive patients with COVID-19 evaluated at Henry Ford Health System in metropolitan Detroit, Michigan, from March 9 to March 27, 2020. Data analysis was performed from March to April 2020.Exposure
Laboratory-confirmed severe acute respiratory syndrome coronavirus 2 infection.Main outcomes and measures
Demographic data, underlying comorbidities, clinical presentation, complications, treatment, and outcomes were collected.Results
Of 463 patients with COVID-19 (mean [SD] age, 57.5 [16.8] years), 259 (55.9%) were female, and 334 (72.1%) were African American. Most patients (435 [94.0%]) had at least 1 comorbidity, including hypertension (295 patients [63.7%]), chronic kidney disease (182 patients [39.3%]), and diabetes (178 patients [38.4%]). Common symptoms at presentation were cough (347 patients [74.9%]), fever (315 patients [68.0%]), and dyspnea (282 patients [60.9%]). Three hundred fifty-five patients (76.7%) were hospitalized; 141 (39.7%) required intensive care unit management and 114 (80.8%) of those patients required invasive mechanical ventilation. Male sex (odds ratio [OR], 2.0; 95% CI, 1.3-3.2; P = .001), severe obesity (OR, 2.0; 95% CI, 1.4-3.6; P = .02), and chronic kidney disease (OR, 2.0; 95% CI, 1.3-3.3; P = .006) were independently associated with intensive care unit admission. Patients admitted to the intensive care unit had longer length of stay and higher incidence of respiratory failure and acute respiratory distress syndrome requiring invasive mechanical ventilation, acute kidney injury requiring dialysis, shock, and mortality (57 patients [40.4%] vs 15 patients [7.0%]) compared with patients in the general practice unit. Twenty-nine (11.2%) of those discharged from the hospital were readmitted and, overall, 20.0% died within 30 days. Male sex (OR, 1.8; 95% CI, 1.1-3.1; P = .03) and age older than 60 years (OR, 5.3; 95% CI, 2.9-9.7; P < .001) were significantly associated with mortality, whereas African American race was not (OR, 0.98; 95% CI, 0.54-1.8; P = .86).Conclusions and relevance
In this review of urban metropolitan patients with COVID-19, most were African American with a high prevalence of comorbid conditions and high rates of hospitalization, intensive care unit admission, complications, and mortality due to COVID-19.Free full text

Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit
Key Points
Question
What are the clinical characteristics and outcomes of patients with coronavirus disease 2019 evaluated at Henry Ford Health System in Southeast Michigan during the early phase of the outbreak?
Findings
In this case series involving 463 consecutive patients with confirmed coronavirus disease 2019 evaluated at a 5-hospital system serving metropolitan Detroit, 72.1% of patients were African American and 94.0% had at least 1 comorbidity. Among the 355 patients who were hospitalized, 39.7% required intensive care unit admission, of whom 80.8% underwent invasive mechanical ventilation and 40.4% died within 30 days.
Meaning
In this series of patients with coronavirus disease 2019 in metropolitan Detroit, a high proportion were admitted and required intensive care unit admission and invasive mechanical ventilation with a mortality rate of 40.4% among patients in the intensive care unit.
Abstract
Importance
In late December 2019, an outbreak caused by a novel severe acute respiratory syndrome coronavirus 2 emerged in Wuhan, China. Data on the clinical characteristics and outcomes of infected patients in urban communities in the US are limited.
Objectives
To describe the clinical characteristics and outcomes of patients with coronavirus disease 2019 (COVID-19) and to perform a comparative analysis of hospitalized and ambulatory patient populations.
Design, Setting, and Participants
This study is a case series of 463 consecutive patients with COVID-19 evaluated at Henry Ford Health System in metropolitan Detroit, Michigan, from March 9 to March 27, 2020. Data analysis was performed from March to April 2020.
Exposure
Laboratory-confirmed severe acute respiratory syndrome coronavirus 2 infection.
Main Outcomes and Measures
Demographic data, underlying comorbidities, clinical presentation, complications, treatment, and outcomes were collected.
Results
Of 463 patients with COVID-19 (mean [SD] age, 57.5 [16.8] years), 259 (55.9%) were female, and 334 (72.1%) were African American. Most patients (435 [94.0%]) had at least 1 comorbidity, including hypertension (295 patients [63.7%]), chronic kidney disease (182 patients [39.3%]), and diabetes (178 patients [38.4%]). Common symptoms at presentation were cough (347 patients [74.9%]), fever (315 patients [68.0%]), and dyspnea (282 patients [60.9%]). Three hundred fifty-five patients (76.7%) were hospitalized; 141 (39.7%) required intensive care unit management and 114 (80.8%) of those patients required invasive mechanical ventilation. Male sex (odds ratio [OR], 2.0; 95% CI, 1.3-3.2; P
2.0; 95% CI, 1.3-3.2; P =
= .001), severe obesity (OR,
.001), severe obesity (OR, 2.0; 95% CI, 1.4-3.6; P
2.0; 95% CI, 1.4-3.6; P =
= .02), and chronic kidney disease (OR,
.02), and chronic kidney disease (OR, 2.0; 95% CI, 1.3-3.3; P
2.0; 95% CI, 1.3-3.3; P =
= .006) were independently associated with intensive care unit admission. Patients admitted to the intensive care unit had longer length of stay and higher incidence of respiratory failure and acute respiratory distress syndrome requiring invasive mechanical ventilation, acute kidney injury requiring dialysis, shock, and mortality (57 patients [40.4%] vs 15 patients [7.0%]) compared with patients in the general practice unit. Twenty-nine (11.2%) of those discharged from the hospital were readmitted and, overall, 20.0% died within 30 days. Male sex (OR,
.006) were independently associated with intensive care unit admission. Patients admitted to the intensive care unit had longer length of stay and higher incidence of respiratory failure and acute respiratory distress syndrome requiring invasive mechanical ventilation, acute kidney injury requiring dialysis, shock, and mortality (57 patients [40.4%] vs 15 patients [7.0%]) compared with patients in the general practice unit. Twenty-nine (11.2%) of those discharged from the hospital were readmitted and, overall, 20.0% died within 30 days. Male sex (OR, 1.8; 95% CI, 1.1-3.1; P
1.8; 95% CI, 1.1-3.1; P =
= .03) and age older than 60 years (OR,
.03) and age older than 60 years (OR, 5.3; 95% CI, 2.9-9.7; P
5.3; 95% CI, 2.9-9.7; P <
< .001) were significantly associated with mortality, whereas African American race was not (OR,
.001) were significantly associated with mortality, whereas African American race was not (OR, 0.98; 95% CI, 0.54-1.8; P
0.98; 95% CI, 0.54-1.8; P =
= .86).
.86).
Conclusions and Relevance
In this review of urban metropolitan patients with COVID-19, most were African American with a high prevalence of comorbid conditions and high rates of hospitalization, intensive care unit admission, complications, and mortality due to COVID-19.
Introduction
An outbreak caused by a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported in Wuhan, China in late December 2019.1 Three months later, coronavirus disease 2019 (COVID-19), the disease caused by SARS-CoV-2, was declared a pandemic by World Health Organization, and as of May 14, 2020, more than 4.3 million cases of COVID-19 and 297 000 deaths were reported.2 Since it was first detected in Washington State on January 20, 2020, the US now leads the world with more than 1.39 million confirmed COVID-19 cases and 84
000 deaths were reported.2 Since it was first detected in Washington State on January 20, 2020, the US now leads the world with more than 1.39 million confirmed COVID-19 cases and 84 000 deaths. All 50 states have reported cases of COVID-19, with most states reporting community spread.3
000 deaths. All 50 states have reported cases of COVID-19, with most states reporting community spread.3
Early reports have suggested an incubation period of 2 to 14 days, with clinical presentations ranging from mild infection to severe disease to fatal illness.3,4,5 The most commonly reported symptoms are cough, fever, and dyspnea.6,7,8,9 Myalgia and gastrointestinal symptoms, including diarrhea and nausea or vomiting, are also common.8 Recent reports6,9,10,11 suggest that approximately 14% to 29% of hospitalized patients with COVID-19 pneumonia require intensive care, primarily for respiratory support in the setting of hypoxic respiratory failure, with acute respiratory distress syndrome (ARDS) developing in 33% of hospitalized patients at a median time from symptom onset of 8 days.9 In these reports,6,8 critically ill patients were older, more likely to be male, and to have underlying comorbidities. The mortality rate ranged from 8.7% to 21% among those patients admitted with pneumonia.6,9,10,11
On March 10, 2020, the state of Michigan confirmed its first 2 cases of COVID-19, and in the days since, the case number has increased to 49 582 with 4787 (10%) deaths, amounting to the highest case fatality rate in the nation.3 Metropolitan Detroit, which includes Oakland, Macomb, and Wayne counties, was at the epicenter of the outbreak, accounting for 80% of cases and 86% of deaths statewide. The city of Detroit accounted for almost one-third of all confirmed cases and deaths.12 The objective of this study is to describe the clinical characteristics and outcomes of the first 463 patients with COVID-19 evaluated at the Henry Ford Health System (HFHS), a 5-hospital system that serves metropolitan Detroit, and to perform a comparative analysis of hospitalized and ambulatory patient populations.
582 with 4787 (10%) deaths, amounting to the highest case fatality rate in the nation.3 Metropolitan Detroit, which includes Oakland, Macomb, and Wayne counties, was at the epicenter of the outbreak, accounting for 80% of cases and 86% of deaths statewide. The city of Detroit accounted for almost one-third of all confirmed cases and deaths.12 The objective of this study is to describe the clinical characteristics and outcomes of the first 463 patients with COVID-19 evaluated at the Henry Ford Health System (HFHS), a 5-hospital system that serves metropolitan Detroit, and to perform a comparative analysis of hospitalized and ambulatory patient populations.
Methods
Study Design and Participants
The HFHS institutional review board approved patient data review with waiver of consent because the data were deidentified. This is a case series that includes consecutive adult patients evaluated in HFHS from March 9, 2020 (date of first specimen tested), to March 27, 2020, and diagnosed with COVID-19. The HFHS is a comprehensive, integrated, health care organization that includes 5 hospitals and 9 emergency departments (EDs) in Southeast Michigan. Its 877-bed flagship hospital, Henry Ford Hospital, serves a large urban, mostly African American population in metropolitan Detroit. Patients were triaged on the basis of clinician judgment. All patients included in the study had SARS-CoV-2 infection confirmed by positive polymerase chain reaction testing of nasopharyngeal specimens. All clinical outcomes were monitored for 30 days.
Data Collection and Definitions
A trained team of physicians and research associates performed a retrospective review of the electronic health records to obtain data on a standardized data collection form. Demographic data, underlying comorbidities, symptoms and signs at presentation, complications, treatment, and outcomes were collected and evaluated. Race/ethnicity data were collected in electronic health records by self-report using standard classification.13 Severe obesity (defined as body mass index [BMI] ≥40; BMI is calculated as weight in kilograms divided by height in meters squared) and ARDS were defined in accordance with the definition established by National Institute of Health14 and Berlin Definition,15 respectively. Acute kidney injury was diagnosed according to the Kidney Disease: Improving Global Outcomes definition.16 Cardiac injury was characterized by the presence of serum levels of high-sensitivity cardiac troponin I above the 99th percentile upper reference limit.
Complications and treatment included acute kidney injury requiring renal replacement therapy, hypoxic respiratory failure and/or ARDS requiring invasive mechanical ventilation (IMV), and shock requiring vasopressor treatment. Outcomes included discharge from the ED, length of stay, discharge disposition, and 30-day readmission and mortality rates.
Laboratory and Radiographic Studies
Methods for laboratory confirmation of SARS-CoV-2 infection have been described elsewhere.17 Influenza polymerase chain reaction testing was also performed for all patients. Routine blood examinations included daily complete blood count with differential, basic metabolic panel, liver function tests, ferritin, magnesium, C-reactive protein, lactate dehydrogenase, and creatine phosphokinase, in addition to high-sensitivity cardiac troponin I and D-dimer every 48 hours. Furthermore, routine laboratory evaluation included interleukin-6 and disseminated intravascular coagulation panel when available for patients admitted to the intensive care unit (ICU). A chest radiograph and subsequent radiographs were obtained at baseline and as determined clinically by health care practitioners on case-by-case basis.
Statistical Analysis
Continuous variables were described as median (interquartile range [IQR]) or mean (SD), and categorical variables were described as frequency rates and percentages. The U test or t test was used for continuous variables, whereas the χ2 or Fisher exact test was used for categorical variables. Comparisons between cohorts were analyzed using univariable analysis. Multivariable logistic regression was performed to model the association of demographic characteristics and comorbidities with ventilator-dependent respiratory failure. Multivariable regression was also performed to model the association of demographic characteristics and comorbidities with the need for ICU care at any time during the hospitalization. Race (African American or non–African American) was included in these models because of the high proportion of African American patients in Detroit. Demographic characteristics or comorbidities in which univariable analysis yielded P <
< .10 were included. Finally, multivariable logistic regression analysis of the associations of age older than 60 years, African American race, and sex with mortality was performed. At the time of analysis, mortality data were complete to 30 days after the initial encounter. We did not perform a formal sample size calculation for the study because the primary objective was to describe the characteristics of the initial surge of patients positive for SARS-CoV-2 within our health system. A 2-sided α
.10 were included. Finally, multivariable logistic regression analysis of the associations of age older than 60 years, African American race, and sex with mortality was performed. At the time of analysis, mortality data were complete to 30 days after the initial encounter. We did not perform a formal sample size calculation for the study because the primary objective was to describe the characteristics of the initial surge of patients positive for SARS-CoV-2 within our health system. A 2-sided α <
< .05 was considered statistically significant. Odds ratios (ORs) with 95% CIs were reported for all models. Statistical analyses were performed using SAS statistical software version 9.4 (SAS Institute). Data analysis was performed from March to April 2020.
.05 was considered statistically significant. Odds ratios (ORs) with 95% CIs were reported for all models. Statistical analyses were performed using SAS statistical software version 9.4 (SAS Institute). Data analysis was performed from March to April 2020.
Results
During the study period, 477 of 1459 patients (32.7%) tested positive for SARS-CoV-2 at HFHS. The first 2 reported cases at HFHS were on March 11, 2020. Of the 477 patients, 14 were excluded from the study because of a lack of demographic and baseline data. Most patients were African American (334 patients [72.1%]) and female (259 patients [55.9%]) with mean (SD) age of 57.5 (16.8) years. Most patients (435 [94.0%]) had at least 1 comorbidity, including hypertension (295 patients [63.7%]), chronic kidney disease (182 patients [39.3%]), and diabetes (178 patients [38.4%]). The mean (SD) number of comorbidities of admitted patients was 3.2 (1.8) compared with 1.9 (1.7) in patients discharged from the ED (difference, 1.3; 95% CI, 0.96-1.72; P <
< .001). Eighty-one admitted patients (22.8%) had prior ED visits for their symptoms compared with none of those who did not require hospitalization; more than one-fourth of all patients (124 patients [26.8%]) had known exposure to someone with COVID-19. Of note, there were no coinfections in patients who were not admitted; among hospitalized patients, 1 case of respiratory syncytial virus in the general practice unit (GPU) and 4 cases of influenza (2 in the GPU and 2 in the ICU [<1% of coinfections]) were detected. Table 1 summarizes the baseline clinical characteristics of the overall cohort.
.001). Eighty-one admitted patients (22.8%) had prior ED visits for their symptoms compared with none of those who did not require hospitalization; more than one-fourth of all patients (124 patients [26.8%]) had known exposure to someone with COVID-19. Of note, there were no coinfections in patients who were not admitted; among hospitalized patients, 1 case of respiratory syncytial virus in the general practice unit (GPU) and 4 cases of influenza (2 in the GPU and 2 in the ICU [<1% of coinfections]) were detected. Table 1 summarizes the baseline clinical characteristics of the overall cohort.
Table 1.
| Characteristic | Patients, No. (%) | P value | ||
|---|---|---|---|---|
All (N = = 463) 463) | Discharged home (n = = 108) 108) | Hospital admission (n = = 355) 355) | ||
| Demographic characteristics | ||||
| Age, mean (SD), y | 57.5 (16.8) | 44.8 (15.1) | 61.4 (15.4) | .005 |
| Age >60 y | 218 (47.1) | 16 (14.8) | 202 (56.9) | <.001 |
| African American race | 334 (72.1) | 74 (68.5) | 260 (73.2) | .34 |
| Female | 259 (55.9) | 69 (63.9) | 190 (53.5) | .06 |
| Known exposure | 124 (26.8) | 31 (28.7) | 93 (26.2) | .61 |
| Prior emergency department visit in past 7 d | 81 (17.5) | 0 | 81 (22.8) | <.001 |
| Symptoms | ||||
| Cough | 347 (74.9) | 87 (80.6) | 260 (73.2) | .14 |
| Nasal congestion | 113 (24.5) | 38 (35.2) | 75 (21.2) | .003 |
| Dyspnea | 282 (60.9) | 40 (37.0) | 242 (68.2) | <.001 |
| Fever | 315 (68.0) | 75 (69.4) | 240 (67.6) | .72 |
| Headache | 74 (16.0) | 28 (25.9) | 46 (13.0) | .001 |
| Myalgias | 194 (42.0) | 46 (42.6) | 148 (41.8) | .89 |
| Anorexia | 100 (21.7) | 10 (9.3) | 90 (25.4) | <.001 |
| Nausea | 94 (20.4) | 12 (11.1) | 82 (23.2) | .007 |
| Vomiting | 53 (11.5) | 8 (7.4) | 45 (12.7) | .13 |
| Diarrhea | 100 (21.7) | 14 (13.1) | 86 (24.3) | .01 |
| Comorbidities | ||||
| Asthma | 73 (15.8) | 20 (18.5) | 53 (14.9) | .37 |
| Chronic obstructive pulmonary disease | 49 (10.6) | 8 (7.4) | 41 (11.6) | .22 |
| Obstructive sleep apnea | 57 (12.3) | 8 (7.4) | 49 (13.8) | .08 |
| Diabetes | 178 (38.4) | 22 (20.4) | 156 (43.4) | <.001 |
| Hypertension | 295 (63.7) | 37 (34.3) | 258 (72.7) | <.001 |
| Coronary artery disease | 59 (12.7) | 3 (2.7) | 56 (15.8) | <.001 |
| Congestive heart failure | 49 (10.6) | 3 (2.8) | 46 (13.3) | .001 |
| Chronic kidney disease | 182 (39.3) | 21 (19.4) | 161 (45.4) | <.001 |
| End-stage renal disease | 26 (5.6) | 2 (1.9) | 24 (6.8) | .06 |
| Cancer | 49 (10.6) | 6 (5.6) | 43 (12.3) | .05 |
| Rheumatologic disease | 10 (2.2) | 1 (0.9) | 9 (2.5) | .47 |
| Solid organ transplant | 11 (2.4) | 3 (2.8) | 8 (2.3) | .72 |
| Body mass index, mean (SD)a | 33.0 (8.5) | 31.0 (7.3) | 33.6 (8.7) | .01 |
| Any obesity | 262 (57.6) | 52 (48.2) | 210 (59.2) | .04 |
| Severe obesity | 89 (19.2) | 14 (13.0) | 75 (21.3) | .06 |
| Tobacco use | 160 (34.8) | 23 (21.9) | 137 (38.6) | .002 |
| Vital signs, median (interquartile range) | ||||
| Lowest emergency department oxygen saturation as measured by pulse oximetry, % | 94 (90-96) | 98 (96-99) | 93 (88-95) | <.001 |
| Heart rate, beats/min | 96 (84-109) | 96 (84-106) | 96 (83-109) | .71 |
| Temperature, °F | 99.0 (98.0-100.0) | 99.0 (98.0-99.5) | 99.0 (98.0-100.0) | .97 |
| Respiratory rate, breaths/min | 19 (18-22) | 18 (17-18) | 20 (18-22) | .02 |
| Baseline chest radiograph findings | ||||
| Unilateral infiltrate | 62 (13.4) | 7 (11.9) | 55 (16.5) | <.001 |
| Bilateral infiltrate | 187 (40.3) | 5 (8.5) | 182 (54.7) | |
| Normal | 105 (22.7) | 41 (69.5) | 63 (18.9) | |
| Baseline laboratory values, median (interquartile range) | ||||
| White blood cell count, cells/μL | 5.8 (4.2-7.5) | 6.1 (3.8-8.6) | 5.8 (4.3-7.5) | .03 |
| Absolute lymphocyte count, cells/μL | 0.8 (0.6-1.2) | 1.0 (0.7-1.6) | 0.8 (0.6-1.1) | .03 |
| Creatinine, mg/dL | 1.1 (0.84-1.54) | 0.85 (0.69-1.18) | 1.12 (0.85-1.61) | .001 |
| Aspartate aminotransferase, IU/L | 30 (26-55) | 26 (24-58) | 35 (27-55) | <.001 |
| High-sensitivity cardiac troponin I >99th percentile | 107 (23.1) | 2 (1.9) | 105 (29.6) | <.001 |
SI conversion factors: To convert degrees Fahrenheit to degrees Celsius, subtract 32 and multiply by .5556; white blood cell count to ×109/L, multiply by .001; lymphocytes to ×109/L, multiply by .001; creatinine to micromoles per liter, multiply by 88.4; aspartate aminotransferase to microkatals per liter, multiply by 0.0167.
Among all patients, 355 (76.7%) required hospital admission (Figure). Common symptoms at presentation were cough (347 patients [74.9%]), fever (315 patients [68.0%]), and dyspnea (282 patients [60.9%]). Symptoms of dyspnea (242 patients [68.1%] vs 40 patients [37.0%]), anorexia (90 patients [25.4%] vs 10 patients [9.3%]), nausea (82 patients [23.1%] vs 12 patients [11.1%]), and diarrhea (86 patients [24.2%] vs 14 patients [12.9%]) were more common among admitted patients than among patients who were discharged home. Furthermore, age older than 60 years (202 patients [56.9%] vs 16 patients [14.8%]), severe obesity (75 patients [21.3%] vs 14 patients [12.9%]), diabetes (156 patients [43.9%] vs 22 patients [20.4%]), hypertension (258 patients [72.7%] vs 37 patients [34.3%]), coronary artery disease (56 patients [15.8%] vs 3 patients [2.7%]), chronic kidney disease (CKD) (161 patients [45.4%] vs 21 patients [19.4%]), and cancer (43 patients [12.1%] vs 6 patients [5.6%]) were more common among admitted patients than among patients who were discharged home. The mean (SD) BMI of hospitalized patients was 33.6 (8.7), with 26% of severely obese patients requiring ICU. Patients requiring hospital admission also had a higher incidence of bilateral infiltrates on chest radiographs (182 patients [54.7%] vs 5 patients [8.5%]), more pronounced lymphopenia (median lymphocyte count, 0.8 cells/μL [IQR, 0.6-1.1 cells/μL] vs 1.0 cells/μL [IQR, 0.7-1.6 cells/μL]; to convert to ×109/L, multiply by .001), and elevated liver enzyme levels (median aspartate aminotransferase level, 35 IU/L [IQR, 27-55 IU/L] vs 26 IU/L [IQR, 24-58 IU/L]); to convert to microkatals per liter, multiply by 0.0167) (Table 1).
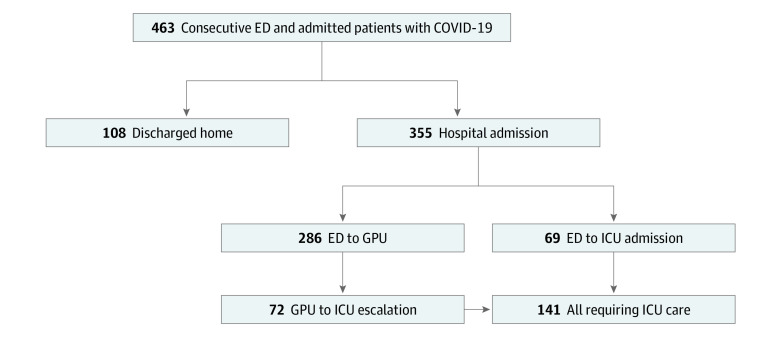
ED indicates emergency department; GPU, general practice unit; and ICU, intensive care unit.
One hundred forty-one patients (39.7%) required ICU level care during their stay. On univariable analyses, those requiring ICU level care were more likely than patients in the GPU to be older than 60 years (92 patients [65.3%] vs 110 patients [51.4%]), male (80 patients [56.7%] vs 85 patients [39.7%]), and have comorbidities, including severe obesity (37 patients [26.2%] vs 38 patients [17.8%]), diabetes (73 patients [51.8%] vs 83 patients [38.8%]), hypertension (111 patients [78.7%] vs 147 patients [68.7%]), and CKD (83 patients [58.9%] vs 78 patients [36.5%]) (Table 2).
Table 2.
| Characteristic | Patients, No. (%) | P value | |
|---|---|---|---|
General practice unit (n = = 214) 214) | Intensive care unit (n = = 141) 141) | ||
| Demographic characteristics | |||
| Male | 85 (39.7) | 80 (56.7) | .002 |
| African American race | 156 (72.9) | 104 (73.8) | .67 |
| Age, mean (SD) y | 59.8 (15.2) | 63.8 (15.4) | .02 |
| Age >60 y | 110 (51.4) | 92 (65.3) | .01 |
| Prior emergency department visit | 42 (19.6) | 39 (27.7) | <.001 |
| Symptoms | |||
| Onset <7 d before admission | 170 (79.4) | 121 (85.8) | .65 |
| Fever | 155 (72.4) | 95 (67.4) | .09 |
| Dyspnea | 140 (65.4) | 111 (78.7) | .04 |
| Headache | 36 (16.7) | 12 (8.5) | .02 |
| Diarrhea | 56 (26.2) | 33 (23.4) | .43 |
| Comorbid conditions | |||
| Asthma | 34 (15.9) | 19 (13.5) | .53 |
| Chronic obstructive pulmonary disease | 23 (10.8) | 18 (12.8) | .56 |
| Obstructive sleep apnea | 27 (12.6) | 22 (15.6) | .43 |
| Body mass index, mean (SD)a | 33.0 (8.1) | 34.4 (9.5) | .22 |
| Any obesity | 123 (57.6) | 87 (61.7) | .43 |
| Severe obesity | 38 (17.8) | 37 (26.2) | .06 |
| Diabetes | 83 (38.8) | 73 (51.8) | .02 |
| Hypertension | 147 (68.7) | 111 (78.7) | .04 |
| Chronic kidney disease | 78 (36.5) | 83 (58.9) | <.001 |
| End-stage renal disease | 15 (7.0) | 9 (6.4) | .99 |
| Solid organ transplant | 5 (2.3) | 3 (2.1) | .99 |
| Coronary artery disease | 30 (14.0) | 26 (18.4) | .26 |
| Congestive heart failure | 23 (10.8) | 23 (16.6) | .11 |
| Cancer | 20 (9.4) | 23 (16.6) | .04 |
| Tobacco use | 79 (36.9) | 58 (41.1) | .42 |
| Baseline respiratory vital signs | |||
| Oxygen saturation as measured by pulse oximetry, median (interquartile range), % | 94 (92-96) | 89 (85-93) | <.001 |
| Respiratory rate ≥22 breaths/min | 47 (22.0) | 47 (33.3) | .02 |
| Bilateral infiltrate on chest radiograph | 93 (43.5) | 89 (63.1) | <.001 |
| Baseline laboratory values, median (interquartile range) | |||
| White blood cell, cells/μL | 5.6 (4.1-7.2) | 6.2 (4.5-7.8) | .05 |
| Absolute lymphocyte count, cells/μL | 0.9 (0.7-1.2) | 0.8 (0.6-1.0) | .007 |
| Creatinine, mg/dL | 1.02 (0.82-1.40) | 1.32 (0.98-1.92) | <.001 |
| Aspartate aminotransferase, IU/L | 31 (25-44) | 44 (30-67) | <.001 |
| Lactate dehydrogenase, IU/L | 283 (235-375) | 395 (296-526) | <.001 |
| Ferritin, ng/mL | 350 (171-718) | 735 (347-1330) | <.001 |
| D-dimer, μg/mL | 0.95 (0.57-1.57) | 1.43 (0.81-3.22) | <.001 |
| Procalcitonin >0.5 ng/mL | 20 (9.4) | 31 (22.0) | <.001 |
| High-sensitivity cardiac troponin I >99th percentile | 47 (22.0) | 58 (41.1) | <.001 |
| Complications | |||
| Acute respiratory distress syndrome | 7 (3.3) | 104 (73.8) | <.001 |
| Acute kidney injury | 61 (28.5) | 98 (69.5) | <.001 |
| Treatments | |||
| Antibiotics | 148 (69.2) | 116 (82.3) | .01 |
| Mechanical ventilation for respiratory failure | 0 | 114 (80.8) | <.001 |
| Vasopressors for shock | 0 | 64 (45.4) | <.001 |
| Renal replacement therapy | 1 (0.5) | 24 (17.0) | <.001 |
| Length of stay, median (interquartile range), d | 5 (3-7) | 15 (9-23) | <.001 |
| Outcomes | |||
| Discharge disposition | |||
| Home | 183 (85.5) | 49 (34.8) | <.001 |
| In-house mortality | 11 (5.1) | 55 (39.0) | <.001 |
| Placement in rehabilitation center | 8 (3.7) | 13 (9.2) | .66 |
| Other | 6 (2.8) | 3 (2.1) | .75 |
| 30-d hospital readmission | 27 (8.9) | 2 (2.3) | <.001 |
| 30-d mortality | 15 (7.0) | 57 (40.4) | <.001 |
SI conversion factors: To convert white blood cell count to ×109/L, multiply by .001; lymphocytes to ×109/L, multiply by .001; creatinine to micromoles per liter, multiply by 88.4; aspartate aminotransferase to microkatals per liter, multiply by 0.0167; lactate dehydrogenase to microkatals per liter, multiply by 0.0167; ferritin to micrograms per liter, multiply by 1.0; D-dimer to nanomoles per liter, multiply by 5.476.
Signs and symptoms associated with the need for ICU care were dyspnea (111 patients in the ICU [78.7%] vs 140 patients in the GPU [65.4%]), tachypnea (47 patients in the ICU [33.3%] vs 47 patients in the GPU [22.0%]), and hypoxia (median oxygen saturation as measured by pulse oximetry, 89% [IQR, 85%-93%] for patients in the ICU vs 94% [IQR, 92%-96%] for patients in the GPU). On univariable analysis, symptoms of fever (155 patients [72.4%] vs 95 patients [67.4%]) and headache (36 patients [16.8%] vs 12 patients [8.5%]) at presentation were more common among patients in the GPU than patients in the ICU. Inflammatory marker and cardiac biomarkers were all higher in the ICU population than in the GPU population. Rates of complications were higher among patients in the ICU compared with patients in the GPU, including respiratory failure (114 patients [80.8%] vs 0 patients), acute kidney injury (98 patients [69.5%] vs 61 patients [28.5%]), ARDS (104 patients [73.8%] vs 7 patients [3.3%]), and shock (64 patients [45.4%] vs 0 patients). After adjusting for significant factors and race, male sex (OR, 2.0; 95% CI, 1.3-3.2; P
2.0; 95% CI, 1.3-3.2; P =
= .001), severe obesity (OR,
.001), severe obesity (OR, 2.0; 95% CI, 1.4-3.6; P
2.0; 95% CI, 1.4-3.6; P =
= .02), and CKD (OR,
.02), and CKD (OR, 2.0; 95% CI, 1.3-3.3; P
2.0; 95% CI, 1.3-3.3; P =
= .006) remained significantly associated with the need for ICU care (Table 3).
.006) remained significantly associated with the need for ICU care (Table 3).
Table 3.
| Characteristic | Odds ratio (95% CI) | P value |
|---|---|---|
| Male | 2.0 (1.3-3.2) | .004 |
| Age >60 y | 1.6 (1.0-2.7) | .07 |
| African American race | 0.9 (0.5-1.6) | .78 |
| Severe obesity | 2.0 (1.4-3.6) | .02 |
| Chronic kidney disease | 2.0 (1.3-3.3) | .006 |
| Cancer | 1.9 (1.0-3.9) | .06 |
| Diabetes | 1.3 (0.8-2.2) | .25 |
| Hypertension | 1.0 (0.5-1.8) | .92 |
| Coronary artery disease | 1.1 (0.6-2.0) | .88 |
One-hundred four patients in the ICU (73.8%) developed ARDS and 114 (80.8%) required IMV for respiratory failure. The median time from symptom onset to need for IMV was 8 days (IQR, 6-10 days), and the median time to IMV after admission was 1 day (IQR, 0-3 days). Among the 286 patients initially admitted to the GPU, 72 (25.2%) were transferred to the ICU for escalation of care (Figure). The median time to ICU transfer from the time of admission was 2 days (IQR, 1-4 days). In a multivariable analysis, male sex (OR, 2.9; 95% CI, 1.7 to 4.8; P
2.9; 95% CI, 1.7 to 4.8; P <
< .001), age older than 60 years (OR,
.001), age older than 60 years (OR, 3.5; 95% CI, 1.9 to 6.4; P
3.5; 95% CI, 1.9 to 6.4; P <
< .001), severe obesity (OR,
.001), severe obesity (OR, 3.2; 95% CI, 1.7 to 6.0; P
3.2; 95% CI, 1.7 to 6.0; P <
< .001), CKD (OR,
.001), CKD (OR, 2.4; 95% CI, 1.4 to 4.2; P
2.4; 95% CI, 1.4 to 4.2; P <
< .001), and cancer (OR,
.001), and cancer (OR, 2.5; 95% CI, 1.2 to 5.0; P
2.5; 95% CI, 1.2 to 5.0; P =
= .01) were independently associated with the need for IMV (Table 4). There were 35 patients admitted younger than 40 years, 8 of whom required IMV. Of those requiring IMV, 5 (62.5%) had severe obesity compared with 7 (25.9%) of those who did not require IMV (difference, 36.6%; 95% CI, −5.5% to 67.2%; P
.01) were independently associated with the need for IMV (Table 4). There were 35 patients admitted younger than 40 years, 8 of whom required IMV. Of those requiring IMV, 5 (62.5%) had severe obesity compared with 7 (25.9%) of those who did not require IMV (difference, 36.6%; 95% CI, −5.5% to 67.2%; P =
= .09). Race was not associated with ICU admission or need for IMV.
.09). Race was not associated with ICU admission or need for IMV.
Table 4.
| Characteristic | Odds ratio (95% CI) | P value |
|---|---|---|
| Male | 2.9 (1.7-4.8) | <.001 |
| Age >60 y | 3.5 (1.9-6.4) | <.001 |
| African American race | 0.7 (0.4-1.3) | .29 |
| Severe obesity | 3.2 (1.7-6.0) | <.001 |
| Chronic kidney disease | 2.4 (1.4-4.2) | .001 |
| Cancer | 2.5 (1.2-5.0) | .01 |
| Diabetes | 1.2 (0.7-2.0) | .58 |
| Hypertension | 0.9 (0.5-1.8) | .81 |
| Coronary artery disease | 1.3 (0.7-2.6) | .45 |
| Congestive heart failure | 0.7 (0.3-1.5) | .38 |
| Tobacco use | 1.1 (0.7-1.9) | .66 |
There was a difference in the length of stay between the 2 groups (median, 15 days [IQR, 9-23 days] for patients in the ICU vs 5 days [IQR, 3-7 days] for patients in the GPU). Overall, 262 (73.8%) hospitalized patients were discharged with median length of stay of 8.5 days (IQR, 4-11 days). In-house mortality was higher in the ICU (55 patients [39.0%]) than GPU (11 patients [5.1%]). Of the 11 patients in the GPU with in-hospital mortality, 2 died of pulseless electrical activity arrest, and 9 died of hypoxic respiratory failure because their code status was switched to “comfort care” at admission. (Table 2). More patients in the GPU (183 patients [85.5%]) than in the ICU (49 patients [34.8%]) were discharged to home (difference, 50.7%; 95% CI, 40.6%-59.6%; P <
< .001). Among patients initially discharged home from the ED, 4 (3.7%) were readmitted within 30 days and none died. Twenty-nine (11.2%) of those discharged from the hospital were readmitted within 30 days and 4 died. The overall 30-day mortality rate was 16.0% for the entire cohort and 20.0% for hospitalized patients; another patient died in the ED. Mortality in the ICU (57 patients [40.4%]) was significantly higher than in the GPU (15 patients [7.0%]) (difference, 33.4%; 95% CI, 24.3%-42.5%; P
.001). Among patients initially discharged home from the ED, 4 (3.7%) were readmitted within 30 days and none died. Twenty-nine (11.2%) of those discharged from the hospital were readmitted within 30 days and 4 died. The overall 30-day mortality rate was 16.0% for the entire cohort and 20.0% for hospitalized patients; another patient died in the ED. Mortality in the ICU (57 patients [40.4%]) was significantly higher than in the GPU (15 patients [7.0%]) (difference, 33.4%; 95% CI, 24.3%-42.5%; P <
< .001); 52 patients requiring IMV (45.6%) died. Male sex (OR,
.001); 52 patients requiring IMV (45.6%) died. Male sex (OR, 1.8; 95% CI, 1.1-3.1; P
1.8; 95% CI, 1.1-3.1; P =
= .03) and age older than 60 years (OR,
.03) and age older than 60 years (OR, 5.3; 95% CI, 2.9-9.7; P
5.3; 95% CI, 2.9-9.7; P <
< .001) were significantly associated with mortality, whereas African American race was not (OR,
.001) were significantly associated with mortality, whereas African American race was not (OR, 0.98; 95% CI, 0.54-1.8; P
0.98; 95% CI, 0.54-1.8; P =
= .86).
.86).
Discussion
This study describes the demographic characteristics and clinical presentation of the initial 463 patients with COVID-19 evaluated in the HFHS, a multicenter academic institution in metropolitan Detroit. This study provides additional insight into the clinical presentation and outcomes of COVID-19 in an urban setting.
Compared with previous reports, most of our patients were African American and required hospitalization.6,8,10 However, our findings support the observations of earlier studies, which found a high percentage of hospitalized patients of advanced age with preexisting conditions, hypertension being the most common.6,8,9,18 COVID-19 rapidly spread throughout the state of Michigan and has disproportionately affected the African American population, who have high rates of comorbid conditions and mean BMI of 30.19,20 As of May 14, 2020, African American patients accounted for 32% of cases and 41% of deaths despite composing only 14% of the state’s population.12,21 This is in line with what has been described in other states.22 For example, in Louisiana, African American residents make up 32% of the state population, but accounted for more than 56% of COVID-19 deaths as of May 14, 2020.23
Factors such as lower wage positions and employment in critical infrastructure jobs, higher rates of poverty, lack of access to a personal vehicle and reliance on public transportation, and unstable or crowded housing conditions make preventive strategies such as social distancing and self-isolation or quarantine difficult to maintain.24 In Michigan, 27% of African American residents lived in poverty compared with 11% of white residents in 2019.25 These social determinants of health result in lack of health insurance and access to care, which may put patients at a disproportionately greater risk of acquiring infection and higher rates of complications from COVID-19.
Interestingly, more than one-half of cases and hospitalizations occurred among women, in contrast to previous reports.6,8,9,18 Women represent 51% and 53% of the Michigan and Detroit populations, respectively.21,26 In addition, they have a lower labor force participation rate (55%) and higher poverty rate (15% vs 12%) compared with their male counterparts (70%), according to the most recent data.25 Poverty can negatively affect family structure and increase health risks, all of which may have contributed to the higher infection rates in women.
The spectrum of disease described in our study is similar to those from the Centers for Disease Control and Prevention’s COVID-19–Associated Hospitalization Surveillance Network, the New York City area, and China.5,7,9,27 In the initial reports from Wuhan, China, during the early stages of the pandemic,24 shortness of breath was reported in 54% of patients and was associated with composite end point of admission to an ICU, use of mechanical ventilation, and death. A similar prevalence of dyspnea was reported in 21 critically ill patients in Washington State and in the COVID-19–Associated Hospitalization Surveillance Network database.7,8 In our series, dyspnea at presentation was associated with hospitalization and the need for ICU management. However, symptoms of fever and headache at presentation were more common among patients in the GPU than patients in the ICU on univariable analysis. A substantial proportion of patients presenting with gastrointestinal symptoms, including anorexia, nausea, and diarrhea, required hospitalization, similar to the data reported in the COVID-19–Associated Hospitalization Surveillance Network. Although we were testing for influenza, coinfection was very rare (<1%).
Compared with previous reports, a larger proportion of our hospitalized patients required ICU admission; 39.7% required ICU care compared with 14% in New York City area, 24% across the US, and up to 20% in reports from China.6,9,11,24 In the multivariable analysis, race was not associated with ICU admission or the need for IMV; however, male sex, severe obesity, and CKD were associated with need for ICU level care and IMV. A notable characteristic in our cohort was the prevalence of obesity; the mean BMI of hospitalized patients was 33.6, with 26% of severely obese patients requiring ICU. Severe obesity was independently associated with the need for mechanical ventilation (OR, 3.2; 95% CI, 1.7-6.0; P
3.2; 95% CI, 1.7-6.0; P <
< .001). The association between obesity and need for IMV has been previously reported in patients with COVID-19.25 In a retrospective analysis28 of 124 patients in the ICU, almost one-half had BMI greater than 30, including 15% with BMI greater than or equal to 40. The mean BMI was 31 (range, 27.3-37.5) in patients requiring IMV compared with 27 (range, 25.3-30.8) in those who did not (P
.001). The association between obesity and need for IMV has been previously reported in patients with COVID-19.25 In a retrospective analysis28 of 124 patients in the ICU, almost one-half had BMI greater than 30, including 15% with BMI greater than or equal to 40. The mean BMI was 31 (range, 27.3-37.5) in patients requiring IMV compared with 27 (range, 25.3-30.8) in those who did not (P <
< .001).28 Moreover, in that study, BMI greater than 35 was independently associated with the need for IMV (OR,
.001).28 Moreover, in that study, BMI greater than 35 was independently associated with the need for IMV (OR, 7.36; 95% CI, 1.63-33.14; P
7.36; 95% CI, 1.63-33.14; P =
= .02).28
.02).28
The rate of complications, including acute kidney injury, hypoxic respiratory failure, and need for IMV, was higher and the length of stay was longer in our patient population than what was recently reported in New York City6; however, the rate of readmission was less than 10% in both cohorts. Overall mortality was in line with what has been reported in the US.6,8,10 Similarly, ICU mortality was higher than GPU mortality.10 Male sex and age older than 60 years were significantly associated with mortality but race was not.
Limitations
This study has a few limitations. It was conducted a single large health system in Southeast Michigan. In addition, this case series has no control group, and the findings may not be generalizable to other populations.
Conclusions
In this study of patients infected with SARS-CoV-2 in the metropolitan Detroit area, 76.7% of the patients who were infected were hospitalized and most of these patients were African American. The high prevalence of comorbidities and severe obesity in the population likely contributed to the disparities in morbidity associated with COVID-19.
References
 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. 10.1001/jama.2020.2648 [Abstract] [CrossRef] [Google Scholar]
314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. 10.1001/jama.2020.2648 [Abstract] [CrossRef] [Google Scholar]Full text links
Read article at publisher's site: https://doi.org/10.1001/jamanetworkopen.2020.12270
Read article for free, from open access legal sources, via Unpaywall:
https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2767216/suleyman_2020_oi_200467.pdf
Citations & impact
Impact metrics
Article citations
Neuroinflammation in Severe COVID-19: The Dynamics of Inflammatory and Brain Injury Markers During Hospitalization.
Mol Neurobiol, 21 Oct 2024
Cited by: 0 articles | PMID: 39433647
Efficacy of High Flow Nasal Cannula in the Treatment of Patients with COVID-19 with Acute Respiratory Distress Syndrome: Results of Single Centre Study in Vietnam.
Pulm Ther, 10(4):451-468, 18 Oct 2024
Cited by: 0 articles | PMID: 39422832
COVID-19 Related Knowledge, Attitudes, and Behaviors Among Black Men with Chronic Health Conditions: A Latent Profile Analysis.
Soc Work Public Health, 39(7):734-749, 28 Jul 2024
Cited by: 0 articles | PMID: 39068542
Evaluation of the Effect of Influenza Vaccine on the Development of Symptoms in SARS-CoV-2 Infection and Outcome in Patients Hospitalized due to COVID-19.
Vaccines (Basel), 12(7):765, 12 Jul 2024
Cited by: 0 articles | PMID: 39066403 | PMCID: PMC11281370
Exploring the impact of cognitive dysfunction, fatigue, and shortness of breath on activities of daily life after COVID-19 infection, until 1-year follow-up.
J Rehabil Med, 56:jrm35403, 25 Jun 2024
Cited by: 0 articles | PMID: 38915292 | PMCID: PMC11218676
Go to all (384) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series.
BMJ, 369:m1996, 29 May 2020
Cited by: 486 articles | PMID: 32471884 | PMCID: PMC7256651
Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy.
JAMA, 323(16):1574-1581, 01 Apr 2020
Cited by: 3263 articles | PMID: 32250385 | PMCID: PMC7136855
Risk Factors for Hospitalization, Mechanical Ventilation, or Death Among 10 131 US Veterans With SARS-CoV-2 Infection.
JAMA Netw Open, 3(9):e2022310, 01 Sep 2020
Cited by: 241 articles | PMID: 32965502 | PMCID: PMC7512055
Maternal and infant outcomes of full-term pregnancy combined with COVID-2019 in Wuhan, China: retrospective case series.
Arch Gynecol Obstet, 302(3):545-551, 21 Jul 2020
Cited by: 16 articles | PMID: 32696241 | PMCID: PMC7372542
Review Free full text in Europe PMC

 1
1 



