Abstract
Background
The eye is an important sensory organ occupationally exposed to ionizing radiation (IR) in healthcare workers (HCWs) engaged in medical imaging (MI). New evidence highlights the possible induction of cataract at IR exposure levels to be much lower than expected in the past.Objective
Conduct an updated review on the current evidence on cataract risk in healthcare workers exposed to IR.Methods
Published scientific studies on cataract risk in IR exposed healthcare workers were collected through a systematic search of two biomedical databases (MEDLINE and Scopus). Data from included studies was extracted and summarized. Study quality was also assessed.Results
All 21 eligible studies reported an increased prevalence of cataract, especially posterior subcapsular cataract, in IR exposed HCWs with a higher prevalence in interventional cardiology staff.Discussion
Our review synthesizes the latest evidence to support the hypothesis of a significantly increased risk of occupational cataract in healthcare workers operating MI and exposed to IR, especially in interventional cardiologists. Data also support a dose-response relationship between IR exposure and the prevalence of opacities, especially posterior subcapsular opacities.Conclusions
Findings highlight the need for effective control measures including appropriate training, adherence to protective procedures, and a constant use of shields and eye personal protective equipment in healthcare workers with optical exposure to IR. Periodic health surveillance programs, possibly including lens evaluation, are also important to monitor cataract risk in these MI operators.Free full text

Risk of cataract in health care workers exposed to ionizing radiation: a systematic review
Abstract
Background:
The eye is an important sensory organ occupationally exposed to ionizing radiation (IR) in healthcare workers (HCWs) engaged in medical imaging (MI). New evidence highlights the possible induction of cataract at IR exposure levels to be much lower than expected in the past.
Objective:
Conduct an updated review on the current evidence on cataract risk in healthcare workers exposed to IR.
Methods:
Published scientific studies on cataract risk in IR exposed healthcare workers were collected through a systematic search of two biomedical databases (MEDLINE and Scopus). Data from included studies was extracted and summarized. Study quality was also assessed.
Results:
All 21 eligible studies reported an increased prevalence of cataract, especially posterior subcapsular cataract, in IR exposed HCWs with a higher prevalence in interventional cardiology staff.
Discussion:
Our review synthesizes the latest evidence to support the hypothesis of a significantly increased risk of occupational cataract in healthcare workers operating MI and exposed to IR, especially in interventional cardiologists. Data also support a dose-response relationship between IR exposure and the prevalence of opacities, especially posterior subcapsular opacities.
Conclusions:
Findings highlight the need for effective control measures including appropriate training, adherence to protective procedures, and a constant use of shields and eye personal protective equipment in healthcare workers with optical exposure to IR. Periodic health surveillance programs, possibly including lens evaluation, are also important to monitor cataract risk in these MI operators.
Abstract
«Revisione sistematica sul rischio di cataratta nel personale sanitario esposto a radiazioni ionizzanti».
Introduzione:
In operatori sanitari addetti a procedure di diagnostica per immagini e di radiologia interventistica possono verificarsi rilevanti esposizioni oculari a radiazioni ionizzanti (RI). Recenti evidenze hanno dimostrato un aumentato rischio di cataratta anche per livelli di esposizione a RI significativamente inferiori alle soglie stabilite in passato.
Obiettivo:
Condurre una revisione sistematica delle evidenze recenti sul rischio di cataratta in operatori sanitari esposti a RI.
Metodi:
Sono stati raccolti studi pubblicati sul rischio di cataratta in operatori sanitari esposti a RI, mediante l’effettuazione di una ricerca sistematica in due database (MEDLINE e Scopus). Sono state effettuate l’estrazione e la sintesi dei dati dagli studi inclusi, ed una valutazione della loro qualità.
Risultati:
Sono stati inclusi nella revisione 21 studi; tutti i lavori riportano un’aumentata prevalenza di cataratta, in particolare di cataratta sottocapsulare posteriore, in operatori sanitari esposti a RI, rilevando prevalenze più elevate nel personale impiegato in attività di cardiologia interventistica.
Discussione:
La revisione della letteratura effettuata ha analizzato le recenti evidenze scientifiche che supportano l’ipotesi di un rischio significativamente aumentato di cataratta occupazionale negli operatori sanitari addetti a procedure di diagnostica per immagini, rilevando un rischio particolarmente elevato per operatori di cardiologia interventistica. I dati supportano anche una relazione dose dipendente tra esposizione a RI e prevalenza di opacità del cristallino, specie sottocapsulari posteriori.
Conclusioni:
I risultati della revisione sistematica evidenziano la necessità di misure di prevenzione efficaci per gli operatori sanitari esposti a RI, che prevedano specifiche attività di informazione e formazione, procedure protettive tecniche e organizzative appropriate ed un uso rigoroso di schermature e DPI, al fine di ridurre al minimo le possibili esposizioni oculari a RI degli operatori. Inoltre, le attività di sorveglianza sanitaria del personale sanitario esposto a RI sono fondamentali ai fini della prevenzione, e debbono includere specificamente la valutazione del cristallino per un efficace monitoraggio del rischio di sviluppo di cataratta.
Introduction
Diagnostic imaging techniques (also called medical imaging; MI) have been in use for over a century, and the existence of relevant health risks for the health care workers (HCWs) dealing with MI, mainly linked to ionizing radiation (IR) exposure, were clear from the beginning (32). The acute effects on the eyes and on the skin were recognized very early, while the existence of long-term effects on various tissues emerged only after some years (32). The eye is one of the most important sensory organs at risk of long-term health effects induced by IR exposure (2, 19, 32). Cataract, an ocular lens opacity associated with visual impairment, has been well documented since the second half of the twentieth century as a major ocular adverse effect associated with IR exposure (1, 9, 32, 38). In fact, the interior capsule of the lens is lined with a transparent layer of epithelial cells which has the purpose of maintaining the function of the lens. Damaged cells tend to lose their transparency due to protein denaturation, resulting in the opacification of the lens (26). While the early stages of such opacification may not cause visual disability, the severity of such changes increases progressively with the IR dose absorbed, with the ultimate stage being visual impairment requiring ophthalmologic intervention (40).
Cataract, or, more generally, lens opacities can be classified into three main types, based on their anatomic location: nuclear (N), cortical (C) and posterior subcapsular (PSC) (28). PSC is the least common among the three major forms of age-related cataract, whereas it is most commonly associated with IR exposure (19).
Over time, radioprotection procedures have led to a general reduction of IR exposure in healthcare workers operating MI, but the development of modern MI techniques have led to the appearance of new modalities of exposure. For example, over the past 30 years, the introduction of interventional cardiologic procedures has resulted in a significant increase in occupational X-ray exposure of interventional cardiologists and other medical, nursing and technical staff involved in radiation-guided interventional procedures, which has led to an elevated risk of radiation injuries (12, 18, 19). The wider use of MI involving X-rays during interventional procedures has led to the steadily increasing exposure of medical staff to ionizing radiation, especially in the field of interventional cardiology with fluoroscopically guided procedures (6, 18, 20, 39). Interventional cardiologists work in close proximity to the source of radiation, and therefore, are potentially at a higher risk of adverse health effects. However, in the case of inadequate protection procedures (e.g. use of protective screens), nurses and technicians who may stand near the patient’s bed for a significant amount of time, are potentially highly exposed (18, 24).
While radiation-induced cataract severity is dose-related with a direct proportionality, its latency period is inversely related to the dose (12). The lowest cataractogenic dose, and the dose-response relation of cataracts in humans are still not well established. For a long time, radiation-related cataract has been considered as a deterministic effect, occurring only after a subject had been exposed to relatively high IR doses, but this view has been challenged by recent studies, which have shown increased risk of lens opacities even after low-dose exposure (9, 30, 35, 36). According to these results, also small cumulative IR doses absorbed by the lens over a long period of time can induce a progressive cataract. The proposed hypothesis is that cataract may be a potentially stochastic phenomena linked to DNA damage, possibly explaining the increased risks at lower radiation exposure levels (5). Recent epidemiology studies yielded new evidence of radiation-induced cataract at lower doses, led the International Commission on Radiological Protection (ICRP) to lower the exposure limit to 0.5 Gy (2, 8, 15, 16, 36, 42).
Nevertheless, data are not completely coherent, and further investigations are still needed, with a particular focus on the exposure of healthcare workers with recent introduction of new procedures releasing relevant occupational IR exposure to the lens (19). Considering these premises, we performed a review of the published scientific papers specifically considering the role of IR as a risk factor for cataract in HCWs, to better understand whether recent technologies and procedures have impacted IR exposure levels and cataract risk in HCW; an additional objective was to study whether specific job categories among HCV have been associated to a particularly increased risk.
Materials and methods
Eligibility criteria, information sources, and search
An electronic search was performed in MEDLINE (through PubMed) and Scopus with limiters set to include original research articles published in peer-reviewed scientific journals in English, French, Italian, Portuguese, or Spanish language, with no time limits for the publication, and up to the 22nd April 2020. Any study design was considered eligible, including cross-sectional studies: only reviews, case reports, comments or letters were excluded. Based on our previous experience (27-29, 33, 37), a specific search string was built: here we report the one for PubMed-MEDLINE: ((Health personnel[mh] health worker*[tw] OR health care worker*[tw] OR Urologists[mh] OR Anesthesiologists[mh] OR anesthetists[mh] OR cardiologists[mh] OR Urologist*[tw] OR Anesthesiologist*[tw] OR anesthetist*[tw] OR cardiologist*[tw] OR radiologic technologist*[tw] OR nuclear medicine personnel[tw] OR dental worker*[tw] OR dentist*[tw] OR dental staff[tw] OR dental staff[mh] OR dental auxiliar*[tw] OR endoscopist*[tw] OR orthopaedic*[tw] OR radiographer*[tw] OR radiologist*[tw] OR surgeon*[tw] OR nurse*[tw] OR radiologists[mh] OR surgeons[mh] OR nurses[mh]) AND (radiology[mh] OR radiation[mh] OR radiology[tw] OR radiation[tw] OR x-rays[tw] OR tomography[tw] OR angiography[tw] OR radiotherapy[tw] ) AND ( aphakia[tw] OR cataract*[tw] OR lens opac*[tw] OR aphakia, postcataract[mh] OR cataract[mh])).
Two main types of studies were considered eligible for inclusion:
a) studies evaluating the presence of cataracts in groups of healthcare workers exposed to IR;
b) studies in groups of patients with cataract, investigated for their occupational exposure to IR as healthcare workers.
Study selection
Study selection was independently performed by two authors:
- the first step was based on the examination of all the titles and abstracts of the studies retrieved from PubMed-MEDLINE and Scopus with the search strings, after duplicates removal;
- the second step was based on the review of the full texts of the articles included after the first step.
For both steps, any disagreements between authors were solved by a third independent author. All the reference lists of included papers were checked to find possible additional relevant research articles, and all the included studies were compared to the list of studies included in a previous systematic review on a similar topic, but not focusing on healthcare workers (19).
Data collection process and quality assessment
Relevant data was extracted from the retrieved studies in order to produce a qualitative synthesis of the results. We also performed quality assessment of the included studies comprising a detailed evaluation of all the potential confounding factors evaluated in the studies, the methodologies applied to assess the exposure and the outcomes, and any other potentially relevant bias. For quality assessment we used an adaptation of the methodology proposed in Jensen, 2011 (21). The quality of the studies, their strengths and weaknesses were evaluated by the authors according to five dimensions, each of them considering a maximum score of 3, for a total possible maximum score of 15. The five dimensions were: a) study design and materials; b) consideration of possible confounders; c) methods for outcome measurements; d) methods for exposure assessment; and e) modalities of data presentation and statistical analysis.
Results
We found 394 potentially relevant articles (260 MEDLINE; 316 Scopus) after duplicates removal, for title and abstract screening (Figure 1). We did not find any additional papers for possible inclusion after a further evaluation of the references from the articles screened and from the ones included in the previously published systematic reviews of Elmaraezy et al. (18) and of Hammer et al. (19). Next, we excluded 251 irrelevant studies at title and abstract screening stage, resulting in 143 papers for full-text screening. At the end, 21 studies satisfied eligibility criteria for inclusion in our review (Figure 1).
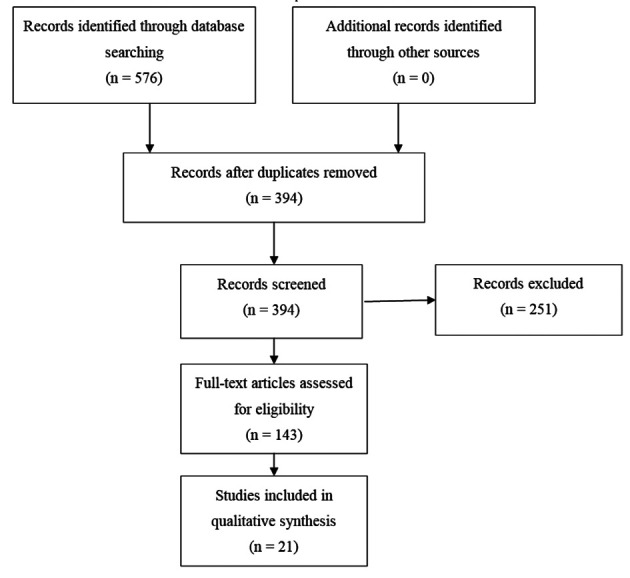
Flow-chart describing the stages of the search process of the literature review on eye lens opacities among health personnel occupationally exposed to Ionizing Radiation
Tables 1 and and22 show the synthesis of the main results of epidemiological studies on cataract in healthcare workers exposed to IR. According to the specific occupational tasks performed, the healthcare workers investigated in the included studies were divided into three groups: radiologists and radiologic technologists (considered in five studies), interventional cardiology staff usually including interventional cardiologists, nurses and technicians (11 studies), and other IR exposed health workers (five studies), including different groups of IR exposed health personnel (often including, within more heterogeneous groups, again some interventional cardiologists and radiologists/technicians) (Table 1).
Table 1
Synthesis of the main results of epidemiological studies on cataract in IR exposed healthcare workers included in this review
| Author, year | Exposed subjects (n.) | Esposure evalaution | Not exposed group | Other risk factors considered | Eye examination using slit lamp in mydriasis | Cataract evaluation method | Lens opacities risk | Type of cataract | Dose-relation |
| Radiologists and radiologic technologists | |||||||||
| Chodick, 2008 | 35705 | Indirect quantitative | - | + | _ | Questionnaire | Increased (not significant) | / | + |
| Bernier, 2017 | 42545 | Indirect quantitative | + (***) | + | - | Questionnaire | Increased | / | + |
| Little, 2018 | 67.247 | Indirect quantitative | - | + | - | Questionnaire | Increased | / | + |
| Velazquez-Kronen, 2019 | 35.751 | Qualitative | - | + | - | Questionnaire | Increased | / | + |
| Little, 2020 | 63.352 | Indirect quantitative | - | + | - | Questionnaire | Increased | / | + |
| Interventional cardiology staff | |||||||||
| Vano, 2010 | 116 | Indirect quantitative | + | +/- | + | Modified Merriam-Focht scoring system | Increased | PSC | + |
| Ciraj-Bjelac, 2010 | 67 | Indirect quantitative | + | - | + | Modified Merriam-Focht scoring system | Increased | PSC | + |
| Yuan, 2010 | 892 | Qualitative | + | - | - | Registry based | Increased (not significant) | / | / |
| Ciraj-Bjelac, 2012 | 52 | Qualitative | + | - | + | Modified Merriam-Focht scoring system | Increased | PSC, C and N | + |
| Jacob, 2013 | 106 | Qualitative | + | + | + | LOCS III | Increased | PSC, C and N | -* |
| Vano, 2013 | 127 | Indirect quantitative | + | +/- | + | Modified Merriam-Focht scoring system | Increased | PSC, C and N | + |
| Auvinen, 2015 | 21 | Direct quantitative | + | + | + | LOCS II | Increased (not significant) | PSC, C and N | - |
| Bitarafan Rajabi, 2015 | 81 | Qualitative/ Indirect quantitative** | + | + | + | LOCS III | Increased | PSC, C and N | + |
| Matsubara, 2017 | 48 | Qualitative/ Indirect quantitative ** | + | + | + | Modified Merriam-Focht scoring system | Increased | PSC | + |
| Barbosa, 2018 | 112 | Qualitative | + | + | + | LOCS III | Increased | PSC, C and N | / |
| Domienik Andrzejewska, 2019 | 69 | Indirect quantitative | + | + | + | LOCS III | Increased (not significant) | PSC, C and N | + |
| Other IR exposed health worker (including also mixed groups, with some participants from the radiology and interventional cardiology units) | |||||||||
| Milacic, 2009 | 115 | Direct quantitative | + | + | + | Retro-illumination method and biomicroscope | Increased | PSC, C and N | +/- |
| Mrena, 2011 | 57 | Indirect quantitative | - | + | + | LOCS II | Increased (not significant) | PSC, C and N | + |
| Negrone, 2016 | 148 | Qualitative** | - | - | - | Questionnaire | Increased | / | + |
| Coppeta, 2018 | 73 | Direct quantitative | - | + | + | LOCS III | Increased | PSC, C and N | + |
| Scheidemann-Wesp, 2019 | 42 | Qualitative | + | + | + | LOCS III | Increased (not significant) | PSC, C and N | + |
Legend: PSC: posterior subcapsular, C: cortical, N: nuclear; *: a clear relationship with workload not observed, but a lower risk in regular users of protective glasses pointed out; **: also data on ocular dose collected, but not used for cataract risk estimates; ***: controls = radiology technologists not engaged in nuclear medicine
Table 2
Evaluation of the risks or prevalence rates of cataract in health personnel exposed to Ionizing Radiation as reported in the studies included in this review.
| Author year | Activity performed | Evaluation of the risk of cataract | Signif. |
| Chodick, 2008 | Radiologic Technologists (exposed to low IR doses) | For workers in the highest exposure category (estimated lens dose, mean, 60 mGy) vs lowest (mean, 5 mGy): adjusted hazard ratio (HR) of cataract= 1.18 (95% CI 0.99-1.40); self-report of >3 x-rays to the face/neck: HR of cataract= 1.25 (95% CI 1.06- 1.47); ERR/Gy = 1.9 (CI 95% -0.69-4.65) | +/- |
| Milacic, 2009 | Health Workers exposed to IR (mainly radiologic technicians and IR exposed physicians) | Significant difference (χ2=65.92;p<0.01) of cataract prevalence between exposed vs unexposed, estimated relative risk=4.6 (CI not reported) | + |
| Ciraj-Bjelac, 2010 | Interventional cardiology staff (IC and nurses) | PSC prevalence= 52% (95% CI: 35–73) for IC; 45% (95% CI 15–100) for nurses; 9% (95% CI 1–33) for controls RR= 5.7 (95% CI 1.5–22) for IC; 5.0 (95% CI 1.2–21) for nurses. Estimated cumulative ocular doses= 0.01 up to 43 Gy, mean 3.4 Strong dose–response relationship found. | + |
| Vano, 2010 | Interventional cardiology staff (IC, nurses, technicians) | Prevalence of PSC in IC vs not exposed= 38% vs 12% (p < 0.005); RR =3.2 (CI 95% 1.7 - 6.1); RR in nurses and technicians (prevalence of PSC= 21%) vs not exposed= 1.7 (0.8–3.7). Cumulative median values of lens doses estimated: 6.0 Sv for IC; 1.5 Sv for nurses and technicians | + |
| Yuan, 2010 | IC | Prevalence exposed vs. unexposed: 1.2% vs. 0.8%, X2 test not significant | - |
| Mrena, 2011 | IR exposed physicians (Radiologists, IC, others) | Any type of lens opacity: adjusted OR = 3.87 CI 95% (0.82 - 18.3) cortical or posterior opacity excluding nuclear opacities: adjusted OR = 1.28 CI 95% (0.08 - 19.38) | - |
| Ciraj-Bjelac, 2012 | Interventional cardiology staff (IC, nurses and technicians) | Prevalence of PSC in IC=53%, in nurses and technicians =45%. RR vs unexposed= 2.6 (95% CI 1.2–5.4) for IC; =2.2 (95% CI 0.98–4.9) for nurses and technicians | + |
| Jacob, 2013 | IC | PSC prevalence= 17% in IC vs 5% in unexposed (p = 0.006); OR = 3.9 (CI 95% 1.3–11.4). Risk increased with duration of activity, no clear relationship with workload observed. For IC regular users of protective glasses: OR= 2.2 (95% CI 0.4–12.8) | + |
| Vano, 2013 | Interventional cardiology staff (IC and IR exposed paramedicals) | Estimated cumulative eye dose (Gy ± SD and range): for IC with opacities 8.3 ± 5.4 (0.7-18.9) compared to 3.0 ± 2.9 (0.1-9.7) for those without opacities; for paramedicals with opacities 2.7 ± 2.0 (0.6-6.3) compared to 1.8 ± 1.9 (0.1-6.8) for those without opacities | + |
| Auvinen 2015 | IC | PSC PR in IC vs unexposed= 2.3% (CI 95% 0.29 - 19.9) PSC ERR per 10 mSv= −0.09 (95% CI (−0.51-0.35) | - |
| Bitarafan Rajabi, 2015 | Interventional cardiology staff (IC and technicians) | Lens opacity incidence in IC staff vs nurses (not exposed)= 79% (95% CI, 69.9-88.1%) vs. 7.1% (95% CI, 2.3-22.6%); attributable risk of 91.0% (95% CI, 40.0-98.6%); increased % of relative risk= 11.06% (95% CI 1.67-73.37%) | + |
| Negrone, 2016 | Health Workers with different working tasks and differnet levels of IR exposure | Highly exposed health workers showed increased cataract prevalence: χ2 = 13.7; p = 0.0001), as well as nurses: χ2 = 14.3 (p = 0.0002) vs other categories; no significantly increased prevalence for workers engaged as physicians and for radiologic technologists | +/- |
| Bernier, 2017 | Radiologic technologists (engaged in nuclear medicine procedures) | Significantly increased cataract risk: Hazard Ratio (HR): =1.08 (95% CI 1.03-1.14) for performance of nuclear medicine (NM) procedures at least once vs never; = 1.07 (95% CI 1.01-1.12) for diagnostic NM procedures; = 1.10 (95% CI 1.04-1.17) for therapeutic NM procedures; = 1.30 (95% CI 1.08-1.58) for diagnostic NM procedures in the 1980s vs. 2000s; = 1.11 (95% CI 1.01-1.23) for therapeutic NM procedures in the 1970s vs early 2000s | + |
| Matsubara, 2017 | Interventional cardiology staff (IC, nurses and technicians) | Prevalence of PSC in IC=28.6%; in nurses & technicians= 19.5%; Increased risk vs. unexposed group: IC 10.6 (CI 95% 1.1 - 101.4); 7.2 (CI 95% 0.9–55.0) for nurses & technicians | + |
| Barbosa, 2018 | Interventional cardiology staff (IC, nurses and technicians) | Significantly increased PSC prevalence in IR exposed vs unexposed: 13% vs 3% | + |
| Coppeta, 2018 | Health Workers classified at high exposure | Lenticular opacity: prevalence = 10.5% in the whole group (95% CI), = 14.3 (4.9-34.6; CI 95%) for comulative dose 10-30mSv/year; =17.8 (CI 95%; 7.8-35.6) for >30mSv/year | + |
| Little, 2018 | Radiologic Technologists | Hazard Ratio (HR) for cataract history compared to subjects with comulative dose at the lens < 10.0mGy: 20-49.9mGy = 1.11 (1.0;1.23) | + |
| Domienik-Andrzejewska, 2019 | IC | Adjusted OR = 1.47 (CI 95% 0.6-3.6) Average cumulative dose: left eye= 224 mSv; right eye= 85 mSv. PSC= 7% in IC vs 6% in unexposed. Considering also other opacities type: adjusted OR for any opacity in IC vs unexposed= 1.47 (95% CI 0.62-3.59); no evidence for increased opacity risk with increasing dose. | - |
| Scheidemann-Wesp, 2019 | Physicians performing fluoroscopy-guided interventional procedures (IC, interventional neuroradiologists and interventional radiologists) | Lens Opacities in IC vs not exposed = 59% vs 28% (difference not significant at the X2 test), mainly in the nuclear region. Results not reported for other interventional physicians | - |
| Velazquez-Kronen, 2019 | Radiologic Technologists | RR vs who never worked in Interventional Fluoroscopy: <1000 procedures = 1.1 (CI 95% 1.0-1.2); 1000-<3000 procedures = 1.2 (CI 95% 1.1-1.4); 3000-<5000 procedures = 1.2 (CI 95% 1.0-1.5); >5000 = 1.3 (CI 95% 1.2-1.5) | + |
| Little, 2020 | Radiologic Technologists | Cumulative occupational IR exposure associated with self-reported cataract: EAR per 104 persons-year Gy= 94.2 (CI 95% 46.7-142.9). No association considering reporting of cataract surgery: EAR per 104 persons-year Gy= 13 (95% CI <0-57. p=0.55) Elevated additive risk observed for estimated occupational lens IR exposure <100mGy (p=0.004), no dose–response relationship | + |
Legend: EAR= excess additive risk; ERR: excessive relative risk; IC: interventional cardiologists; OR: Odds Ratio; PSC: posterior subcapsular cataract; PR: prevalence ratio; RR: relative risk
Most of the studies compared the results obtained in IR exposed healthcare workers operating MI with an unexposed group, but in seven studies no controls were available (9, 14, 22, 23, 30, 31, 43); furthermore Bernier et al. (5) compared radiological technologists engaged in nuclear medicine versus those not engaged in nuclear medicine (Table 1).
IR lens exposure was estimated qualitatively (yes/no) in seven (33%) studies and using indirect quantitative methods in nine (43%) studies, while 2 (20%) studies performed analysis including mixed qualitative and indirect quantitative exposure assessments (Table 1). Direct quantitative measures of occupational IR exposure, in particular at the workers’ lens, have been collected by various studies, but, as representing in the majority of the cases an index of short-term exposure, the data could not be useful for evaluations of the cataract risk in IR exposed operators (Table 1).
Numerous studies adopted different methods to indirectly estimate a quantitative cumulative occupational exposure. Mrena et al. (30) estimated the effective dose as a whole-body dose weighted by a factor indicating the risk of health detriment. In the two studies from Vano et al. (40, 41) the estimation of the lens dose was calculated based on a combination of measured data of scatter radiation doses during several interventional procedures with the reported years of occupational exposure and additional information on eye protection use. Ciraj-Bjelac et al. (12) utilised a retrospective lens dose assessment for each individual, based on a detailed written occupational and medical survey. In Bernier et al. (5), the dose was estimated with the frequency of performing nuclear medicine procedures per week. In the two studies form Little et al. (22, 23) on United States (US) cohorts of radiologic technologists, a reconstruction of the historical dose based on annual reported badge doses (when available) and a specific algorithm including data from a specific work history questionnaire was performed. In 2019, Domienik-Andrzejewska et al. (17) developed another new algorithm for semi-quantitative retrospective exposure assessment (Table 1).
Different methods were applied to evaluate the occurrence of lens opacities, and the localization of opacities. In most of the studies (66%) the lens of exposed operators was directly examined using a slit lamp, usually in mydriasis (3, 4, 7, 12-14, 17, 20, 24, 26, 30, 34, 40, 41), while in six studies the occurrence of opacities was assessed using questionnaires (5, 9, 22, 23, 31, 43), and in one other the cataract cases were recruited from a health insurance database (44) (Table 1).
The specific type of opacities was classified in 13 studies (62%): in some of these studies a modified version of the Merriam-Focht scoring system (25) was applied (12, 13, 24, 40, 41), while in two studies (3, 30) the second version of the Lens Opacities Classification System (LOCS II) (10) was used, and the third version (LOCS III) (11) in another six studies (4, 7, 14, 17, 20, 34) (Table 1).
Overall, the majority of included studies detected a significant increase in the prevalence of cataract, and in particular posterior subcapsular cataract (PSC), in IR exposed health personnel compared to other health personnel not exposed to IR (Table 1 and and2).2). Only six studies (29%) found an elevated risk or increased prevalence of cataract in IR exposed health workers, even if not increased with statistical significance (3, 9, 17, 30, 34, 44) (Table 1 and and2).2). Despite heterogeneous and non-comparable methods applied to evaluate the IR dose to the lens across studies, most authors reported a dose-response relationship between the occupational IR exposure of the lens and cataract risk (Table 1 and and2).2). Most of the studies used cross-sectional designs and compared the prevalence of cataracts between IR exposed healthcare workers and an unexposed group (Table 2). Stronger and more informative evidence was provided by large prospective cohort studies on US radiologic technologists that estimated the increased additive risks for the accumulated lens IR exposure per year (Table 2). Considering different job tasks with varying IR exposure, most of the available evidence was for interventional cardiology staff who were found to have an increased prevalence or higher risk of cataract (Table 2).
With regard to the overall quality assessment of the included studies, it has to be considered that cataract is a multi-factorial age-related disease with quite a high prevalence in the general population. As such, we collected detailed information on all the possible confounding risk factors other than IR exposure evaluated by the studies, even if only a few studies included them in the adjusted models for the risk estimate (Tables 1 and and3).3). Some studies considered only a few potential confounding factors; for example, Yuan et al. (44) only included age in the analysis, while other studies collected a more comprehensive set of potential confounding risk factors including age, gender, family and medical history, concomitant diseases such as hypertension, cardiovascular diseases and arthritis, and other factors such as smoking status, alcohol and drug consumption, and myopia (Table 3).
Table 3
Risk factors other than occupational ionizing radiation exposure possibly related to cataract development considered in the studies included in this review; *: chronic diseases: diabetes, hypertension, cardiovascular diseases and arthritis.
| Author, year | Age | Sex | BMI | Demographic characteristics | Lifestyle | Family history of eye disease | Personal medical history (included eye) | Work history | Chronic diseases* | History of myopia | Steroid use | Smoking status | Alcohol consumption | UV exposure | Non occupational radiation exposure | Other |
| Chodick, 2008 | X | X | X | X | X | X | X | X | X | X | X | |||||
| Milacic, 2009 | X | X | X | X | X | X | X | X | X | X | X | |||||
| Ciraj-bjelac, 2010 | X | X | X | X | X | X | X | X | X | X | ||||||
| Vano, 2010 | X | X | X | X | ||||||||||||
| Yuan, 2010 | X | |||||||||||||||
| Mrena, 2011 | X | X | X | X | X | X | X | X | X | X | ||||||
| Ciraj-bjelac, 2012 | X | X | X | |||||||||||||
| Jacob, 2013 | X | X | X | X | X | X | X | X | X | |||||||
| Vano, 2013 | X | X | X | X | X | X | X | |||||||||
| Auvinen, 2015 | X | X | X | X | ||||||||||||
| Bitarafan Rajabi, 2015 | X | X | X | X | X | X | X | |||||||||
| Negrone, 2016 | X | X | X | X | X | |||||||||||
| Bernier, 2017 | X | X | X | X | X | X | X | X | X | |||||||
| Matsubara, 2017 | X | X | X | X | X | |||||||||||
| Barbosa, 2018 | X | X | X | X | X | X | X | |||||||||
| Coppeta, 2018 | X | X | X | X | X | X | X | |||||||||
| Little, 2018 | X | X | X | X | X | X | X | X | X | X | X | |||||
| Domienik-Andrzejewska, 2019 | X | X | X | X | X | X | X | X | X | X | X | |||||
| Scheidemann-Wesp, 2019 | X | X | X | X | X | X | X | X | X | |||||||
| Velazquez-Kronen, 2019 | X | X | X | X | X | X | X | X | X | X | ||||||
| Little, 2020 | X | X | X | X | X | X | X | X |
We performed the quality assessment based on an adaptation of the Jensen methodology (21), and we found, among 21 studies, eight high quality studies and one with low quality (44), while the remaining studies were classified by the assessors as medium quality (Table 4). The major factors affecting study quality were related to the study design, participant selection, and inadequate adjustment of regression models that did not include all relevant confounders. On the contrary, the IR exposure assessment and cataract outcome ascertainment, with a few exceptions, achieved good quality scores (Table 4).
Table 4
Quality assessment of the studies included in the review
| Authors, year | Design and materials | Consideration of potential confounders | Measurement of outcome | Measurement of exposure | Data presentation and statistical analysis | Quality assessment score | Total score |
| Chodick, 2008 | 2 | 3 | 1 | 2 | 3 | 11 | +++ |
| Milacic, 2009 | 1 | 1 | 3 | 2 | 2 | 9 | ++ |
| Ciraj-bjelac, 2010 | 2 | 1 | 3 | 2 | 2 | 10 | ++ |
| Vano, 2010 | 2 | 1 | 3 | 2 | 2 | 10 | ++ |
| Yuan, 2010 | 1 | 1 | 1 | 1 | 1 | 5 | + |
| Mrena, 2011 | 2 | 3 | 3 | 2 | 2 | 12 | +++ |
| Ciraj-bjelac, 2012 | 2 | 1 | 3 | 2 | 1 | 9 | ++ |
| Jacob, 2013 | 2 | 3 | 3 | 2 | 3 | 13 | +++ |
| Vano, 2013 | 2 | 1 | 3 | 3 | 2 | 11 | +++ |
| Auvinen, 2015 | 2 | 1 | 3 | 2 | 2 | 10 | ++ |
| Bitarafan Rajabi, 2015 | 2 | 1 | 2 | 2 | 2 | 9 | ++ |
| Negrone, 2016 | 1 | 2 | 1 | 3 | 1 | 8 | ++ |
| Bernier, 2017 | 2 | 3 | 1 | 2 | 2 | 10 | ++ |
| Matsubara, 2017 | 2 | 1 | 2 | 2 | 2 | 9 | ++ |
| Barbosa, 2018 | 2 | 2 | 3 | 1 | 2 | 10 | ++ |
| Coppeta, 2018 | 1 | 1 | 3 | 3 | 2 | 10 | ++ |
| Little, 2018 | 3 | 3 | 1 | 2 | 3 | 12 | +++ |
| Domienik-Andrzejewska, 2019 | 2 | 3 | 3 | 2 | 2 | 12 | +++ |
| Scheidemann-Wesp, 2019 | 2 | 1 | 3 | 2 | 2 | 10 | ++ |
| Velazquez-Kronen, 2019 | 3 | 2 | 1 | 2 | 3 | 11 | +++ |
| Little, 2020 | 3 | 3 | 1 | 2 | 3 | 13 | +++ |
Discussion
Overall, 15 (71%) out of 21 studies included in this review found a significantly increased risk or prevalence of cataract in health personnel exposed to IR, while six studies found an increasing risk pattern, even if not statistically significant. A higher risk or greater prevalence of cataract appeared to be positively correlated with an increasing dose of IR absorbed by the healthcare workers’ lenses. In the few cases where a clear dose-response relationship was not observed between exposure levels and cataract risk, there may have been other factors, such as individual-level control measures, influencing the relationship. For example, Jacob et al. (20) reported a lower risk of cataract in regular users of protective glasses.
Six studies did not report a significantly increased risk of cataract amongst IR exposed healthcare workers and this was most likely due to specific characteristics of the study design. For example, Auvinen et al. (3) recruited a small group of 21 physicians exposed to low levels of IR and may have been underpowered to detect a modest increased risk in a low exposure group compared to an unexposed group. Similarly, Chodick et al. (9) used self-reported exposure based on answers to a postal questionnaire and Yuan et al. (44) conducted a qualitative evaluation of IR exposure and both of exposure assessment methods may have led to exposure misclassification.
Regarding the occupational groups investigated in the general category of IR exposed healthcare workers, the majority of the recent studies focused on interventional cardiology staff, including not only interventional cardiologists but in many studies also nurses and technicians. These IR exposed healthcare workers had higher levels of radiation exposure, as well as the highest risks and prevalence of cataract. Another frequently investigated occupational group was that of the radiologists and radiologic technologists, followed by less represented groups, including other physicians as pneumologists, anaesthesiologists, endoscopists, urologists, surgeons and orthopaedics, interventional neurologists and other physicians performing interventional procedures, nuclear medicine personnel, and dental workers.
Studying differences in IR exposure patterns and possible cataract risks in different groups of healthcare workers is extremely important, as the induction of IR-related effects in the lens depends on several aspects involving the specific working tasks and the exposure modalities, first of all the distance and the posture adopted with respect to the IR source. In particular for interventional cardiologists, all studies observed an increased prevalence of cataract compared to non-exposed groups (Table 2), even if in three studies the differences in prevalence estimates were not significant.
Whilst the majority of studies collected data on relevant confounders (Table 3), there were some studies that assessed limited number of confounders (e.g. Yuan only included age) and these models were probably inadequately adjusted. Interestingly, most of the studies examining the relationship between IR exposure and lens opacities applying adjusted models for various factors observed a significant positive association with cataract (Table 1 and and33).
This review confirmed that PSC was the most prevalent type of cataract in the exposed groups.
Approximately 50% of interventional cardiologists and other IR exposed healthcare workers were classified with posterior lens opacities in the majority of included studies (Table 2). However, prevalence data are also variable and difficult to compare between studies, and this variability depends on the different exposures and job tasks, and also on the different methods applied for cataract diagnosis and opacities classification systems adopted. Our data also confirmed previous findings of the systematic review of Elmaraezy et al. (18), reporting a pooled prevalence of overall posterior lens opacities in interventional cardiologists of 33.4% (95% CI [19.6%, 50.9%]), while the overall prevalence of any lens opacity was 36%.
Considering the overall study quality, the high variability in study designs, methods applied, and methodological rigor, this implies difficulties in interpreting the results of the studies, and, unfortunately, precluded any possibility of a meta-analysis and of an overall assessment of the level of evidence considering causality, and in particular dose-response relationships. Different methods have been applied in particular for the sampling and selection of subjects, with different inclusion and exclusion criteria considered in the studies. The exposure levels were estimated using different methods scarcely comparable (or not comparable), and the description of exposure/activity was poor. Among the problems encountered in the evaluation of the results, one of the main was the evaluation of the eye lens dose, measured only in a minority of studies and estimated using different exposure assessment methods. Another limitation was the different lens opacities classification systems used across studies (e.g. LOCS II, LOCS III, modified Merriam-Focht scoring system). All the previously mentioned limitations have been underlined also in the Hammer et al. systematic review (19), which was aimed to evaluate the effect of the occupational exposure to low doses of IR on cataract risk, not limited to HCW: these Authors found that the included studies were heterogeneous and inconclusive regarding the dose–response relationship.
Conclusions
Based on the recent evidence summarised and critiqued in this review, the overall conclusion is that healthcare workers exposed to IR, and especially interventional cardiologists, are at a significantly increased risk of occupational cataract. Data also support a dose-relationship between IR exposure and the prevalence of posterior lens opacities.
Effective procedures for appropriate eye protection are available: comprehensive training, a strict respect of protective procedures, including constant use of shields and eye PPE, a constant wearing of a personal dosimeter, and adequate periodical health surveillance, possibly including lens evaluation, are important for an effective prevention of future cataract occurrence in these operators.
No potential conflict of interest relevant to this article was reported by the authors
References
Articles from La Medicina del Lavoro are provided here courtesy of Mattioli 1885
Citations & impact
Impact metrics
Citations of article over time
Article citations
Deciphering the molecular landscape of ionising radiation-induced eye damage with the help of genomic data mining.
Arh Hig Rada Toksikol, 75(2):91-101, 29 Jun 2024
Cited by: 0 articles | PMID: 38963141 | PMCID: PMC11223508
Central nervous system tumours and occupational ionising radiation exposure: a nested case-control study among the ORICAMs cohort of healthcare workers in France.
BMJ Open, 14(6):e084285, 19 Jun 2024
Cited by: 0 articles | PMID: 38904132 | PMCID: PMC11191795
Occupational Exposure to Solar Radiation and the Eye: A Call to Implement Health Surveillance of Outdoor Workers.
Med Lav, 114(4):e2023032, 02 Aug 2023
Cited by: 0 articles | PMID: 37534422 | PMCID: PMC10415847
The first experience of multi-gripper robot assisted percutaneous coronary intervention in complex coronary lesions.
J Geriatr Cardiol, 20(8):608-611, 01 Aug 2023
Cited by: 2 articles | PMID: 37675265 | PMCID: PMC10477582
Cohort profile: ORICAMs, a French cohort of medical workers exposed to low-dose ionizing radiation.
PLoS One, 18(6):e0286910, 08 Jun 2023
Cited by: 3 articles | PMID: 37289793 | PMCID: PMC10249798
Go to all (10) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Occupational exposure to ionizing radiation and lens opacity in interventional cardiologists.
Int J Occup Med Environ Health, 32(5):663-675, 04 Oct 2019
Cited by: 7 articles | PMID: 31588928
Eye lens opacities and cataracts among physicians and healthcare workers occupationally exposed to radiation: A systematic review and meta-analysis.
Saudi Med J, 43(7):665-677, 01 Jul 2022
Cited by: 1 article | PMID: 35830987 | PMCID: PMC9749701
Review Free full text in Europe PMC
Eye Lens Opacities Among Physicians Occupationally Exposed to Ionizing Radiation.
Ann Occup Hyg, 59(7):945-948, 13 Apr 2015
Cited by: 9 articles | PMID: 25868644
Occupational exposure to low doses of ionizing radiation and cataract development: a systematic literature review and perspectives on future studies.
Radiat Environ Biophys, 52(3):303-319, 27 Jun 2013
Cited by: 41 articles | PMID: 23807741
Review

 1
1 

