Abstract
Free full text

Contraceptive Use and Elective Terminations in Women Enrolled in the Glomerular Disease Collaborative Network
In the United States, nearly half of pregnancies are unintended,1 and unintended pregnancy is associated with preterm birth and low birth weight.2 Glomerular disease and vasculitis increase risk of adverse obstetric outcomes including preeclampsia, preterm delivery, and perinatal death.3 Preventing unintended pregnancy in this high-risk group is imperative, and requires proactive family planning through shared decision making between patient and provider.
Contraception, when used consistently and correctly, helps prevent unintended pregnancy and allows women the opportunity to optimize their health prior to conception. The U.S. Medical Eligibility Criteria for Contraceptive Use (US MEC) published by the Centers for Disease Control and Prevention (CDC) recommends long-acting reversible contraceptives (LARC), including intrauterine devices (IUDs) and contraceptive implants, as first-line choices for women with chronic disease.4 These highly effective agents carry lower venous thromboembolic and cardiovascular risk than estrogen-containing contraception. Contemporary contraceptive methods used by women with glomerular disease and/or vasculitis are unknown. This knowledge may identify gaps in reproductive counseling to be addressed for tailoring family planning discussions between nephrologists and the women for whom they care regularly.
Using the Glomerular Disease Collaborative Network, a longitudinal registry in the southeastern United States, we distributed a women’s health survey to adult women aged 18 to 65 years. Within the broader survey, we assessed women’s comfort discussing contraception with their nephrologist as well as methods chosen by reproductive-aged women (18−50 years old) who had glomerular disease and/or vasculitis. We enquired about pregnancies and their outcomes, including elective terminations (see Supplementary Methods).
Results
A total of 113 women (15.5%) responded, whose mean age at consent was 37.1 ± 8.8 years and whose body mass index (BMI) was 30.7 ± 9.0 kg/m2 (Table 1). Approximately half of the participants (51.3%) had completed college, and an additional 28.3% had completed graduate school. Disease type was self-reported and compatible with registry-verified biopsy diagnosis in 93.8%. The most common diseases were IgA nephropathy and/or vasculitis (29.2%), lupus nephritis (23.9%), focal segmental glomerulosclerosis (FSGS) (19.5%), and antineutrophil cytoplasmic autoantibody (ANCA) glomerulonephritis and/or vasculitis (14.2%). Kidney function was not reported; 13.3% were considered end-stage renal disease (ESRD) because of having received dialysis or having a functioning kidney transplant. Over half (54.9%) had a history of hypertension, 23.0% were past or current smokers, and 12.4% reported prior venous thromboembolism. Nonresponders (n = 614) were of similar mean age (36.6 ± 9.1) to responders but included more African Americans (38.8% vs. 21.2%) and more lupus nephritis patients (34.7%) over IgA (14.7%).
Table 1
Characteristics of participants (n = 113)
| Characteristic | Mean ± SD or n (%) |
|---|---|
| Age, yr | 37.1 ± 8.8 |
| Body mass index | 30.7 ± 9.0 |
| Race/ethnicity | |
| African American | 24 (21) |
| Caucasian | 75 (66) |
| Hispanic | 8 (7) |
| Other | 6 (5) |
| Education completed | |
| High school | 23 (20) |
| College | 58 (51) |
| Graduate school | 32 (28) |
| Disease type | |
| ANCA glomerulonephritis/vasculitis | 16 (14) |
| Focal segmental glomerulosclerosis | 22 (19) |
| IgA nephropathy/vasculitis | 33 (29) |
| Lupus nephritis | 27 (24) |
| Membranous nephropathy | 10 (9) |
| Other | 5 (4) |
| ESRD | |
| Dialysis | 5 (4) |
| Transplantation | 10 (9) |
| Medical history | |
| Blood clot | 14 (12) |
| High blood pressure | 62 (55) |
| Pregnancy | 75 (66) |
| Sexually transmitted infection | 13 (12) |
| Tobacco use (past or current) | 26 (23) |
ANCA, antineutrophil cytoplasmic autoantibody; ESRD, end-stage renal disease.
Participants were asked about their comfort in discussing women’s health issues with their nephrologist. The majority (90.1%) felt “comfortable or very comfortable” discussing contraception. Likewise, 88.3% were “comfortable or very comfortable” discussing desires for pregnancy. Two-thirds (62.5%) believed that kidney disease increases risk for pregnancy complications.
A total of 91.2% reported using any birth control ever to prevent pregnancy. The most common methods reported were birth control pills (66.4%), condoms (64.6%), (41.7%), and withdrawal method (38.1%). In the prior year, 72.6% (n = 82) used some contraceptive method. Women who used contraception were similar in age to those who did not (36.7 vs. 38.0, P = 0.49). The most common methods used in the last year included progesterone intrauterine device (30.5%), condoms (23.2%), birth control pills (22.0%), and withdrawal method (19.5%) (Figure 1). Participants who using LARC were significantly younger (34.5 vs. 38.1, P = 0.05) but did not differ by disease type. Nearly one-third (31.7%) had used 2 or more methods in the prior year. The most common combinations included condoms and withdrawal (9 of 82, 11.0%) and condoms and birth control pills (7 of 82, 8.5%).
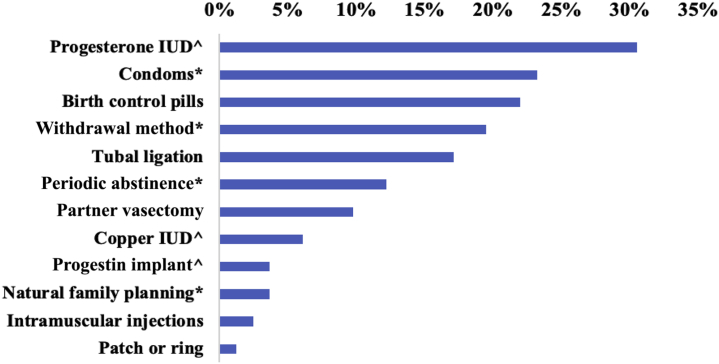
Contraceptive methods used to prevent pregnancy in the past 12 months by reproductive-aged women in the Glomerular Disease Collaborative Network. More than 1 method could be reported. No use of diaphragms or spermicides were reported. IUD, intrauterine device. ^Long-acting reversible contraception.  Typical use associated with >10% failure rate over 1 year of use.
Typical use associated with >10% failure rate over 1 year of use.
Of those participants who reported prior pregnancy (n = 75), 25.3% had at least 1 elective termination (30 elective terminations in 19 women). Women who reported elective termination were older (41.0 vs. 36.2, P = 0.03). One-third (35.0%) with history of pregnancy and lupus nephritis reported an elective termination. Use of LARC in the prior year was lower in women who reported elective termination compared to those who did not (26.7% vs. 41.8%), but the difference was not statistically significant (P = 0.4).
Discussion
Our results provide a window into contraceptive methods in a high-risk population that has not been previously described. By the 2015–2017 US National Survey of Family Growth, 64.9% of women aged 15 to 49 years were currently using contraception.5 It was reassuring to note that our glomerular disease and/or vasculitis population revealed a slightly larger percentage, with 72.6% reporting contraception use in the past 12 months specifically to prevent pregnancy. Use of LARC was remarkably high in this cohort, with 39% of women indicating use within the past 12 months compared to 10% to 14% in the general US population.5,6
Although LARC use in this population is appropriate given the US MEC recommendations, response bias may have influenced our findings. Notably, responders were highly educated and likely represented a group with higher health literacy. College graduates were found to be twice as likely to use an IUD than individuals without a high school diploma6; 79% of our cohort were college graduates. A large number of our nonresponders were diagnosed with lupus, a group with possibly lower LARC use. In a single-center survey of 212 women with lupus, the levenorgestrel IUD was used by only 3%, and 23% of respondents reported unprotected sex “most of the time.”7 Use of an IUD is also reportedly low in kidney transplants recipients, although the efficacy and safety of IUDs in this population have only recently been established.8,9
Respondents in our survey were heterogeneous in regard to underlying disease type and stage of chronic kidney disease. Beyond LARC, other forms may be acceptable based on desire for future pregnancy and consideration of side effect profiles. Our survey did not specifically enquire about concurrent disease activity or medications prescribed, but these likely play a role in both patient and provider preferences. For women who do not desire future pregnancies, laparoscopic, abdominal, and hysteroscopic methods of sterilization are available in the United States, and some of these procedures can be performed in an outpatient setting. For individuals with proteinuria and/or hypertension, progestin-only pills provide a safer cardiovascular profile than those containing estrogen, but are subject to user error given the daily timing of use required.9 It was interesting that about 1 in 3 women endorsed use of 2 or more methods in the past 12 months, which could indicate fragmented or discontinued use. Unfortunately, our survey was not designed to determine whether methods were used together or in succession. Certainly, barrier methods in conjunction with a second form of birth control provides added protection from sexually transmitted infections (of which 11.5% of participants reported a history).
A significant percentage of women were using methods associated with more than 10% failure over 1 year of typical use (e.g., withdrawal), and thus were at risk for unintended pregnancy. In the United States, it has been reported that 24% of women will undergo elective abortion by age 45 years.S1 Our survey found similar results, with 25.3% of women with prior pregnancy reporting at least 1 elective termination. Our survey did not query reasons for termination, such as whether underlying disease played a role, but these remain as questions for future studies. In addition, more data are needed on safety and use of both medical and surgical abortion procedures in this population.
Nephrologists have previously reported lacking confidence in contraception counseling.S2 The majority of respondents here felt comfortable discussing contraception and desires for pregnancy with their nephrologist. However, our small sample size and low response rate caution against the generalizability of our results. Larger studies across a broader demographic are needed to assess these outcomes on both a national and international level. Overall, comprehensive reproductive counseling from nephrologists to women with glomerular disease and/or vasculitis is prudent to help avoid mistimed or unwanted pregnancies. By promoting effective contraception while preserving reproductive autonomy, nephrologists can support women in making informed decisions regarding family planning.
Acknowledgments
MLR was supported by NIDDK/NIH 2T32DK007750-20. VKD, LNB, CJP, SLH and RJF received support from NIH/NIDDK 5P01DK058335-20. Study data were collected and managed using REDCap electronic data capture tools hosted at UNC. REDCap grant support UL1TR002489 from the Clinical and Translational Science Award program of the National Center for Advancing Translational Sciences, National Institutes of Health. This work was presented as an American Society of Nephrology (ASN) abstract (Reynolds M, Poulton C, Blazek L, Nichols A, Hogan S, Falk R, Derebail V. Contraceptive use and elective terminations in women with glomerular disease, TH-PO731) at ASN Kidney Week, November 5–10, 2019, Washington, DC.
References
Articles from Kidney International Reports are provided here courtesy of Elsevier
Full text links
Read article at publisher's site: https://doi.org/10.1016/j.ekir.2020.07.005
Read article for free, from open access legal sources, via Unpaywall:
http://www.kireports.org/article/S246802492031370X/pdf
Citations & impact
Impact metrics
Article citations
Female Reproductive Health and Contraception Use in CKD: An International Mixed-Methods Study.
Kidney Med, 5(10):100713, 13 Aug 2023
Cited by: 3 articles | PMID: 37719717 | PMCID: PMC10502408
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Impact of including elective pregnancy terminations before 20 weeks gestation on birth defect rates.
Teratology, 66 Suppl 1:S32-5, 01 Jan 2002
Cited by: 30 articles | PMID: 12239742
Unemployment, contraceptive behaviour and reproductive outcomes among young Australian women.
Health Policy, 82(1):95-101, 11 Oct 2006
Cited by: 6 articles | PMID: 17045693
Fiscal impact of a potential legislative ban on second trimester elective terminations for prenatally diagnosed abnormalities.
Am J Med Genet, 91(5):359-362, 01 Apr 2000
Cited by: 3 articles | PMID: 10766999
Subdermal contraceptive implants.
J Steroid Biochem Mol Biol, 53(1-6):223-226, 01 Jun 1995
Cited by: 13 articles | PMID: 7626459
Review
Funding
Funders who supported this work.
NCATS NIH HHS (1)
Grant ID: UL1 TR002489
NIDDK NIH HHS (2)
Grant ID: T32 DK007750
Grant ID: P01 DK058335





