Abstract
Aim
The COVID-19 pandemic led to widespread disruption of colorectal cancer services during 2020. Established cancer referral pathways were modified in response to reduced diagnostic availability. The aim of this paper is to assess the impact of COVID-19 on colorectal cancer referral, presentation and stage.Methods
This was a single centre, retrospective cohort study performed at a tertiary referral centre. Patients diagnosed and managed with colorectal adenocarcinoma between January and December 2020 were compared with patients from 2018 and 2019 in terms of demographics, mode of presentation and pathological cancer staging.Results
In all, 272 patients were diagnosed with colorectal adenocarcinoma during 2020 compared with 282 in 2019 and 257 in 2018. Patients in all years were comparable for age, gender and tumour location (P > 0.05). There was a significant decrease in urgent suspected cancer referrals, diagnostic colonoscopy and radiological imaging performed between March and June 2020 compared with previous years. More patients presented as emergencies (P = 0.03) with increased rates of large bowel obstruction in 2020 compared with 2018-2019 (P = 0.01). The distribution of TNM grade was similar across the 3 years but more T4 cancers were diagnosed in 2020 versus 2018-2019 (P = 0.03).Conclusion
This study demonstrates that a relatively short-term impact on the colorectal cancer referral pathway can have significant consequences on patient presentation leading to higher risk emergency presentation and surgery at a more advanced stage. It is therefore critical that efforts are made to make this pathway more robust to minimize the impact of other future adverse events and to consolidate the benefits of earlier diagnosis and treatment.Free full text
COVID‐19 and the emergency presentation of colorectal cancer
Abstract
Aim
The COVID‐19 pandemic led to widespread disruption of colorectal cancer services during 2020. Established cancer referral pathways were modified in response to reduced diagnostic availability. The aim of this paper is to assess the impact of COVID‐19 on colorectal cancer referral, presentation and stage.
Methods
This was a single centre, retrospective cohort study performed at a tertiary referral centre. Patients diagnosed and managed with colorectal adenocarcinoma between January and December 2020 were compared with patients from 2018 and 2019 in terms of demographics, mode of presentation and pathological cancer staging.
Results
In all, 272 patients were diagnosed with colorectal adenocarcinoma during 2020 compared with 282 in 2019 and 257 in 2018. Patients in all years were comparable for age, gender and tumour location (P > 0.05). There was a significant decrease in urgent suspected cancer referrals, diagnostic colonoscopy and radiological imaging performed between March and June 2020 compared with previous years. More patients presented as emergencies (P = 0.03) with increased rates of large bowel obstruction in 2020 compared with 2018–2019 (P = 0.01). The distribution of TNM grade was similar across the 3 years but more T4 cancers were diagnosed in 2020 versus 2018–2019 (P = 0.03).
Conclusion
This study demonstrates that a relatively short‐term impact on the colorectal cancer referral pathway can have significant consequences on patient presentation leading to higher risk emergency presentation and surgery at a more advanced stage. It is therefore critical that efforts are made to make this pathway more robust to minimize the impact of other future adverse events and to consolidate the benefits of earlier diagnosis and treatment.
INTRODUCTION
In March 2020, the UK began a nationwide lockdown in response to the exponential rise in the number of COVID‐19 (SARS‐CoV‐2) cases [1, 2, 3, 4]. To mitigate against the significant risk that the NHS would be overwhelmed, all non‐urgent care was temporarily suspended. An estimated 30 000 UK cancer operations were cancelled, diagnostic capacity was reduced and the number of urgent cancer referrals fell by approximately 25% [5].
In April 2020, a joint position statement was released by the Association of Coloproctology of Great Britain and Ireland, the British Society of Gastroenterology and the British Society of Gastrointestinal and Abdominal Radiology. This proposed adaptation to the conventional rapid access colorectal cancer (CRC) pathway was due to the concern over aerosol generating procedures [6, 7]. Traditional evidence‐based models of care were adjusted in an attempt to treat the growing CRC backlog alongside the increasing burden of emergency COVID admissions.
Delay in urgent referral or diagnostic testing often leads to CRC being treated at a more advanced stage [8, 9]. At our institution, there was a perceived notion of more patients presenting with bowel obstruction/perforation from CRC following the peak of the COVID‐19 first wave. The literature further demonstrates that emergency surgery for CRC is associated with a higher postoperative morbidity and mortality compared with the elective setting [10, 11, 12, 13]. Emergency surgery for CRC also carries a significantly increased risk of anastomotic leak (8.9% vs. 2.6%) and stoma formation [14].
The aim of this paper is to assess the impact of the COVID‐19 pandemic on CRC referral and diagnostics. We further aimed to analyse the effect of any adjustment in the standard urgent suspected cancer (USC) referral pathway on the presentation and stage of CRC during 2020 compared with previous years at our institution.
METHODS
Study design and setting
This was a single centre retrospective cohort study performed at a tertiary referral centre for CRC. Patients diagnosed and managed with colorectal adenocarcinoma during the calendar year 2020 were compared with patients from 2018 and 2019. Two previous years’ data were selected to provide a comparison of results achieved in 2020 with our standard of care. These comparative years were grouped to avoid any discrepancy from inter‐group variation. Patients were grouped according to month of first presentation to the multidisciplinary team (MDT).
Inclusion and exclusion criteria
All patients with a new diagnosis of small/large bowel adenocarcinoma between January and December for three distinct year groups, 2018, 2019 and 2020, were included. Patients were identified from a prospectively collected database and by reviewing the minutes of our colorectal multidisciplinary team. Those who underwent emergency or elective surgery were included based on their date of operation. Any patients with dysplasia, squamous cell carcinoma, neuroendocrine tumours and sarcomas were excluded. An emergency presentation was defined as any patient requiring assessment by the on‐call general surgical team. An emergency intervention was classed as any of these patients proceeding to emergency laparotomy/laparoscopy or endoscopic stent.
Primary and secondary outcomes
The primary outcome was the number of patients requiring an emergency admission and intervention for CRC. Secondary outcomes were patient demographics, TNM classification, tumour location, referral route and diagnostic activity.
Data collection
Medical records were reviewed to establish both primary and secondary outcomes. Radiological activity was reviewed using local IT systems (SYNAPSE® and SYNAPSE CLM®, Fujifilm). Referral and endoscopic activity were obtained using Welsh Clinical Portal and the Cardiff and Vale Clinical Portal (NHS Wales Informatics Service).
Statistical analysis
Descriptive statistics were reported as percentages. Continuous variables were compared using the Student's t test, categorical variables through the Wilcoxon (chi squared) test. Chi‐squared tests were used to assess TNM classification, tumour location, emergency presentations, referral routes and MDT decision. A P value of <0.05 was considered statistically significant. Data analysis was performed with the Statistical Software for the Social Sciences SPSS Advanced Statistics 22 (IBM Software Group).
RESULTS
There were 267 patients diagnosed with colorectal adenocarcinoma at our institution during 2020, 282 in 2019 and 257 in 2018 (Table (Table1).1). Patient demographics were comparable between 2020 and 2018–2019 (P > 0.05; Table Table11).
TABLE 1
Patient demographics, TNM grade, tumour location, presentation and referral route for colorectal cancer for 2018–2020, where an asterisk denotes a statistically significant result
| Characteristic |
2018/2019 n = 539 |
2020 n = 267 | P value |
|---|---|---|---|
| Age (years), mean (SD) | 70 (12.5) | 70 (14.0) | 0.72 |
| Female gender, n (%) | 231 (42.9) | 116 (43.4) | 0.87 |
| T stage n (%) | – | 0.02* | |
| T1 | 31 (5.8) | 17 (6.4) | 0.72 |
| T2 | 82 (15.2) | 29 (10.9) | 0.10 |
| T3 | 269 (49.9) | 116 (43.4) | 0.09 |
| T4 | 146 (27.1) | 92 (34.5) | 0.03* |
| TX | 11 (2.0) | 12 (4.5) | 0.05 |
| N1 or higher, n (%) | 292 (54.2) | 152 (56.9) | 0.46 |
| M1 or higher, n (%) | 145 (26.9) | 85 (31.8) | 0.14 |
| Tumour location, n (%) | |||
| Small bowel | 3 (0.06) | 2 (0.8) | 0.08 |
| Colon | 350 (64.9) | 193 (72.8) | |
| Rectum | 186 (34.5) | 70 (26.4) | |
| Emergency presentation, n (%) | 154 (28.6) | 96 (36.0) | 0.03* |
| Large bowel obstruction, n (%) | 23 (4.3) | 23 (8.6) | 0.01* |
| Small bowel obstruction, n (%) | 20 (3.7) | 6 (2.2) | |
| Perforation, n (%) | 18 (3.3) | 11 | |
| Urgency of surgery, n (%) | |||
| Elective | 298 (80.5) | 115 (71.9) | 0.03* |
| Emergency | 72 (19.5) | 45 (28.1) | |
Primary outcome
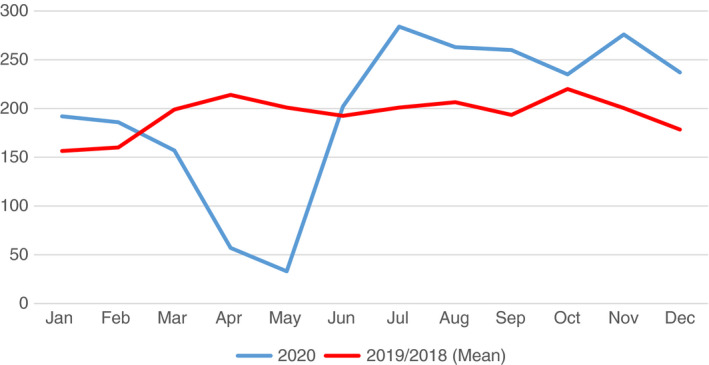
There was a two‐fold increase in the percentage of patients who presented with large bowel obstruction in 2020 compared with 2018–2019 (P = 0.01) (Table (Table1,1, Figure Figure1).1). This trend became apparent in the second half of the year (from June to December 2020; Figure Figure1).1). This resulted in an increase in the number of emergency operations for CRC during 2020 than previously observed (P = 0.03) (Table (Table11).
Secondary outcomes
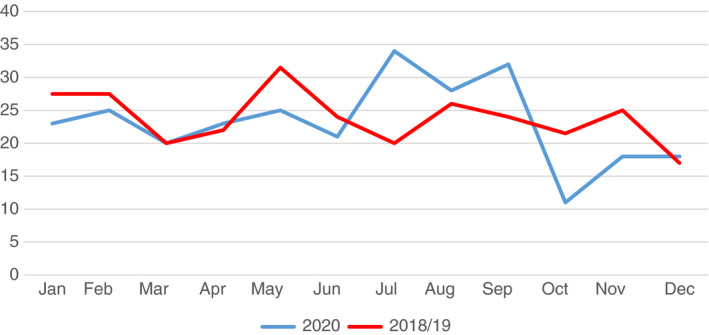
A decrease in USC referrals was demonstrated between March and April 2020 compared with previous years with a subsequent recovery and peak in July 2020 (P = 0.02) (Figure (Figure2).2). There was a decrease in cancer diagnostic activity during 2020 (Figures (Figures33 and and4)4) compared with 2018–2019. There was steep reduction in the overall number of diagnostic colonoscopies performed from February 2020 (coinciding with the national lockdown). This has yet to recover to numbers observed in previous years (Figure (Figure3).3). The number of diagnostic CT scans (colonography and minimal preparation) was also observed to reduce significantly from February 2020 with a subsequent rebound seen from June to September 2020 (Figure (Figure4).4). The number of emergency presentations for CRC increased in 2020 (P = 0.03, Table Table1).1). There was a significant difference in the TNM tumour distribution between 2020 and 2018–2019 (P = 0.02) (Table (Table1).1). There were more T4 cancers found during 2020 than for 2018–2019 (34.5% vs. 27.1%, P = 0.03). Node positive disease and metastases were equivalent in 2020 versus 2018–2019 (P = 0.46, 0.14 respectively).

Mean number of diagnostic endoscopic procedures (colonoscopy and flexible sigmoidoscopy) performed per month for 2020 versus 2018–2019
DISCUSSION
This study aimed to assess the impact of the COVID‐19 pandemic on CRC referral and diagnostics at our institution (Figure (Figure5).5). We further aimed to analyse the effect of these USC pathway delays on the presentation and stage of CRC during 2020 compared with previous years.
The key findings from our study were as follows. (1) There was a decrease in the number of USC elective referrals and the number of diagnostic tests performed during the first wave of the pandemic. (2) There was an increase in the number of patients presenting as CRC emergencies between June and December 2020 compared with the previous 2 years. (3) There was a significant increase in the number of T4 cancers diagnosed during 2020 compared with previous experience.
This paper demonstrates several factors which need to be considered when planning strategies to manage future COVID‐19 outbreaks. Our results show that only a short delay (4 months) in referral and diagnosis is required before an increase in patients presenting with large bowel obstruction becomes evident. Whilst our data do not provide direct evidence for poorer cancer outcomes, several previous publications have shown that emergency surgery in CRC does carry a worse prognosis [14, 15, 16]. Morbidity and mortality for emergent colorectal surgery are between 15%–50% and 6%–15% compared with elective surgery rates of 4%–14% and 1%–7% respectively [10, 11, 12, 13, 14]. Postoperative complications are higher for emergency CRC surgery (91.1%) than in elective groups (23.9%) [10, 11, 12, 13, 14]. The risk of anastomotic leakage is consistently higher in emergency surgery which often leads to an increased rate of permanent stoma formation. Emergency surgery is also an independent prognostic factor for cancer‐related survival (relative risk 1.6) and distant metastases (relative risk 1.8) [14, 15, 16]. Local invasion and distal disease are significantly higher in obstructing versus non‐obstructing tumours [14, 15, 16].
An interesting trend in our data is that the overall number of CRCs diagnosed was similar between 2020 and 2018–2019. This would imply that we were able to address the initial delay in diagnosis during the first 6 months of 2020 by increasing activity towards the latter part of the year. Despite an increase in the number of CRC emergency presentations in 2020, the overall distribution of T1–3 grade, nodal disease and metastases was comparable to previous years. The number of T4 cancers, however, was significantly higher in 2020 (P = 0.03). In previous years, this group may have avoided emergency surgery by having a large tumour resected electively with a specialist colorectal surgeon. Only time will allow us to assess whether oncological outcomes have been affected.
Our study outlines several positive findings associated with the 2020 pandemic. We have been able to demonstrate analogous total numbers of CRC surgeries during 2020 compared with previous experience. Although our capacity to diagnose CRC was affected during the first wave of the pandemic, it is encouraging to find good recovery to reach the pre‐COVID standards by the end of 2020. It is difficult to appreciate if the delay in presentation of CRC was due to the reduction of USC referrals or diagnostic capacity. Although our diagnostic services did recover more rapidly, it is likely that both factors contributed to this finding.
When interpreting the results of this study, the following limitations should be considered. First, the retrospective collection of data relies on several individuals for accurate records and thus we cannot exclude inherent bias. Second, this is a single institution's experience and must be interpreted accordingly. It is unclear yet as to whether these results will be reproducible across other UK hospitals as we were fortunate to establish an early green hospital site within the private sector for elective resection. In addition, we fast‐tracked the use of qFIT10 as a triage tool to focus the use of limited diagnostics. Our referral pathway also includes the widespread utilization of virtual consultations to engage patients without the need for physical attendance. Public Health campaigns have been launched in Wales to widen awareness of cancer‐related symptoms. Approximately 50% of patients ignored cancer type symptoms during the first wave of the pandemic [17]. Focused targeting of these groups will be an important part of ensuring a robust USC CRC pathway in the coming years.
This paper demonstrates the impact of the COVID‐19 pandemic on CRC services at our institution during 2020. Short‐term reduction in bowel cancer referrals and rationing of diagnostic services can change the mode of presentation for CRC patients and influence overall quality of care. This paper underlines the importance of prompt referral and early diagnosis of CRC to reduce cancer stage and the need for emergency intervention with known poorer outcomes. A robust system for CRC management is needed which can function through the future peaks and troughs of the COVID‐19 prevalence. Future work will evaluate the long‐term oncological outcomes of this cohort against previous benchmarked standards.
CONFLICT OF INTERESTS
There are no relevant disclosures or conflicts of interest to declare related to this project, and no sources of funding or financial relationships.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. 10.1001/jama.2020.2648 [online ahead of print] [Abstract] [CrossRef] [Google Scholar]
314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. 10.1001/jama.2020.2648 [online ahead of print] [Abstract] [CrossRef] [Google Scholar]Full text links
Read article at publisher's site: https://doi.org/10.1111/codi.15662
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8250723
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/103161013
Article citations
Decreased Positive Fecal Occult Blood Tests and Delayed Medical Presentation for Colorectal Cancer during the Initial COVID-19 Pandemic Period: A Single-center Experience.
J Anus Rectum Colon, 8(3):188-194, 30 Jul 2024
Cited by: 0 articles | PMID: 39086876 | PMCID: PMC11286375
Impact of COVID-19 Pandemic on the Clinical and Pathologic Characteristics of Colorectal Cancer: A Retrospective Multicenter Study in South Korea.
Cancer Manag Res, 16:1131-1139, 04 Sep 2024
Cited by: 0 articles | PMID: 39247180 | PMCID: PMC11380852
The impact of COVID-19 on colorectal cancer in regional Northern Australia and changes to treatment related to distance to care: a retrospective cohort study.
Ann Med Surg (Lond), 86(9):5017-5023, 23 Jul 2024
Cited by: 0 articles | PMID: 39238998 | PMCID: PMC11374236
Impact of COVID-19 pandemic on surgical volume and outcomes in a terciary care center in Brazil.
Rev Col Bras Cir, 51:e20243678, 06 May 2024
Cited by: 0 articles | PMID: 38716917 | PMCID: PMC11185064
Impact of the Sars-Cov-2 outbreak on the initial clinical presentation of new solid cancer diagnoses: a systematic review and meta-analysis.
BMC Cancer, 24(1):143, 29 Jan 2024
Cited by: 0 articles | PMID: 38287348 | PMCID: PMC10823607
Review Free full text in Europe PMC
Go to all (35) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Clinical outcomes of obstructive colorectal cancer patients during the coronavirus disease 2019 pandemic.
Ulus Travma Acil Cerrahi Derg, 29(6):663-668, 01 Jun 2023
Cited by: 0 articles | PMID: 37278080 | PMCID: PMC10315929
Colorectal Cancer Stage at Diagnosis Before vs During the COVID-19 Pandemic in Italy.
JAMA Netw Open, 5(11):e2243119, 01 Nov 2022
Cited by: 25 articles | PMID: 36409496 | PMCID: PMC9679872
Impact of the COVID-19 Pandemic on Colorectal Cancer Diagnosis and Treatment: a Systematic Review.
J Gastrointest Cancer, 54(1):171-187, 29 Nov 2021
Cited by: 43 articles | PMID: 34843058 | PMCID: PMC8628028
Review Free full text in Europe PMC
COVID-19 pandemic and its impact on emergency surgery in colorectal cancer: A single centre experience.
Med J Malaysia, 78(1):32-34, 01 Jan 2023
Cited by: 1 article | PMID: 36715188

 1
1