Abstract
Background
A retrospective cohort study was performed to evaluate the immediate effect on the oropharynx dimensions from different mandibular advancements in patients undergone counterclockwise rotation (CCW) of the maxillomandibular complex.Material and methods
138 CBCT images of patients, who had undergone orthognathic surgery, were identified from Dolphin Imaging archive according to pre- (T0) and post-operative (T1) times. Each pre-operative CBCT image was selected considering retrognathic mandible. Superimpositions of CBCT images were performed to measure mandibular advancement at B point in millimeters (mm) and divided into three groups: G1 (< 5 mm), G2 (between 5 and 10 mm) and G3 (> 10 mm). For evaluating oropharynx dimension at T0 and T1 for each group, medial sagittal area (MSA), volume, and minimum cross-sectional axial area (CSA) were measured on Dolphin Imaging. Pearson correlation verified reliability of method. Paired t-test were applied to compare values of measurements between T0 and T1 (p ≤ 0.05).Results
88 CBCT images were included. Method was reliable (r ≥ 0.93). According to MSA, volume and CSA values from G1, there was no significant difference between T0 and T1. CSA values presented significant difference comparing T0 and T1 in G2 (p ≤ 0.05). In subjects of G3, measurements increased in T1 significantly affecting oropharynx dimension.Conclusions
MSA, volume and CSA values showed a significant increase affecting upper airway in advancements higher than 10 mm. Mandibular advancement range showed different effects in the airway space and should be considered to achieve favorable post-operative results in the oropharynx dimensions. Key words:Retrognathia, orthognathic surgery, three-dimensional imaging, oropharynx, airway.Free full text
Immediate three-dimensional changes in the oropharynx after different mandibular advancements in counterclockwise rotation orthognathic planning
Abstract
Background
A retrospective cohort study was performed to evaluate the immediate effect on the oropharynx dimensions from different mandibular advancements in patients undergone counterclockwise rotation (CCW) of the maxillomandibular complex.
Material and Methods
138 CBCT images of patients, who had undergone orthognathic surgery, were identified from Dolphin Imaging archive according to pre- (T0) and post-operative (T1) times. Each pre-operative CBCT image was selected considering retrognathic mandible. Superimpositions of CBCT images were performed to measure mandibular advancement at B point in millimeters (mm) and divided into three groups: G1 (< 5 mm), G2 (between 5 and 10 mm) and G3 (> 10 mm). For evaluating oropharynx dimension at T0 and T1 for each group, medial sagittal area (MSA), volume, and minimum cross-sectional axial area (CSA) were measured on Dolphin Imaging. Pearson correlation verified reliability of method. Paired t-test were applied to compare values of measurements between T0 and T1 (p ≤ 0.05).
Results
88 CBCT images were included. Method was reliable (r ≥ 0.93). According to MSA, volume and CSA values from G1, there was no significant difference between T0 and T1. CSA values presented significant difference comparing T0 and T1 in G2 (p ≤ 0.05). In subjects of G3, measurements increased in T1 significantly affecting oropharynx dimension.
Conclusions
MSA, volume and CSA values showed a significant increase affecting upper airway in advancements higher than 10 mm. Mandibular advancement range showed different effects in the airway space and should be considered to achieve favorable post-operative results in the oropharynx dimensions.
Key words:Retrognathia, orthognathic surgery, three-dimensional imaging, oropharynx, airway.
Introduction
Class II dentofacial deformities or mandibular retrognathic patients tend to show a narrow oropharynx dimensions or upper airway (UA). Other factors commonly found in class II patients, such as increased vertical length of the UA, high occlusal plane and retrusion of pogonion may increase airflow resistance (1). Decreased airway space and increased resistance to airflow may lead to a severe narrowing or to a transitory obstruction in the minimal axial area resulting in one of the predisposing factors for obstructive sleep apnea (2-3).
Orthognathic surgery is performed to correct bone deformities and facial soft tissue discrepancies (4). Commonly, bimaxillary advancements cause major skeleton modifications increasing UA area and volume (3). As usual, bimaxillary advancements equal to or higher than 10 millimeters (mm) were reported as favorable changes to the UA dimensions (3,5-7). In this sense, mandibular movements seem to be more important than maxillary advancement (8). Since mandibular advancement stretches the pharynx and the suprahyoid muscles, airway gain may be enhanced with a counterclockwise (CCW) maxillomandibular rotation. The occlusal plane rotation was able to provide pogonion and B point move forward farther than the lower teeth maximizing the advancement of the hyoid bone, base of the tongue, genioglossus, and geniohyoid muscles (9).
Traditionally, lateral cephalograms have been used to evaluate airway parameters (10). However, bidimensional images have presented limitations for evaluating a three-dimensional structure (11-13). Three-dimensional images can be used to reconstruct and evaluate airway spaces from computed tomography scans (1-2,5-6). Furthermore, cone beam computed tomography (CBCT) has shown an appropriated image method to verify UA dimensions in patients undergone orthognathic surgery (8,14-15).
Three-dimensional assessments were developed to measure UA changes using CBCT images to compare pre- and postoperative of CCW rotation in a patient sample of maxillomandibular advancements higher than 10 mm (16-18). However, if their single groups of mandibular advancement were only considered to CCW rotation and guaranteed a significant increase of the UA dimensions, this magnitude of surgical movement could not aesthetically be accepTable planning to all patients. Therefore, our aim was to evaluate the immediate effect on the oropharynx dimensions from different mandibular advancements in patients undergone Orthognathic surgery by CCW maxillomandibular rotation planning.
Material and Methods
This retrospective cohort study was performed by using 138 pre- and postoperative CBCT scans of patients who had undergone orthognathic surgery at the University Hospital of Pedro Ernesto, State University of Rio de Janeiro (Rio de Janeiro, Brazil) between January 2012 and January 2016.
All subjects were scanned in the same I-CAT scanner (Imaging Sciences International, Hatfield, Pennsylvania, USA), operating at 120 kV, 5 mA, FOV of 22 x 13 cm, isotropic voxel of 0.3 mm, and 14-bit grey scale. The CBCT scans were taken according to previous protocol developed at our Oral and Maxillofacial Surgery Division, patients were instructed to sit upright with a natural head position and asked to breathe slowly and not to swallow. The mandible was positioned in a centric relation with manual manipulation and no use of interocclusal device (15). For all CBCT acquisitions, two time points were considered pre-operative (T0), and immediately up to 15 days after surgery (T2). The DICOM images were imported and archived into Dolphin Imaging 11.7 (Dolphin Imaging and Management Solutions, Chatsworth, Calif., USA), which was carried out the same workflow of orthognathic surgery planning. All orthognathic surgeries were conducted by the same Oral and Maxillofacial Surgeon team. The study was approved by the Research Ethics Committee of the Federal University of Juiz de Fora and State University of Rio de Janeiro regarding the use of data and performed according to the ethical principles and Declaration of Helsinki.
From each patient and clinical records, subjects were selected according to the following inclusion criteria: (I) availability of pre- and post-operative CBCT data imported into Dolphin Imaging software; (II) patients with retrognathic mandible from Steiner’s cephalometric analysis (angle between Sella point-nasion-B point, SNB < 78º); (III) bi-maxillary orthognathic surgery by CCW maxillomandibular complex rotation as planned. Exclusion criteria were: (I) patients with asymmetric mandible; (II) growing patients (III) history of adjuvant surgery in the soft tissues of the head and neck region; (IV) trans-surgical or post-operative complications; and (V) incomplete records.
-Cranial base superimposition and B point measurements in mandibular advancements
From subjects available at Dolphin Imaging software, three-dimensional soft and hard tissue had been segmented from each pre-operative DICOM image and patient’s heads were positioned in an estimated natural position (15) before performing planning workflow. Thereupon, each post-operative DICOM image was superimposed over pre-operative CBCT volume by an operator (C.B.L), who used Superimpose Tool. Axial, sagittal, and coronal slices of the CBCT volumes were used to select the anatomical structures of the skull base supporting alignment between post-operative CBCT images in relation to pre-operative one by using a voxel-based superimposition. This superimposition method was used to keep on the same pre- and post-operative head position considering cranial base with no changes after surgical procedures (19-20).
After performing the superimpositions, the same operator (C.B.L) selected Measure tool following as reference the sagittal plane at Dolphin Imaging software to determine linear measurement of the anterior nasal spine (ANS), upper central incisor (UCI), lower central incisor (LCI), and B point. From linear measurements in mm, CCW maxillomandibular rotations were confirmed by verifying comparisons between linear measurements either B points were higher than LCI or UCI advanced more than ANS (Fig. (Fig.1).1). According to mandibular advancement measurements in B point, subjects were allocated to three groups: G1 (advancement < 5 mm), G2 (advancement between 5 and 10 mm) and G3 (advancement > 10 mm).
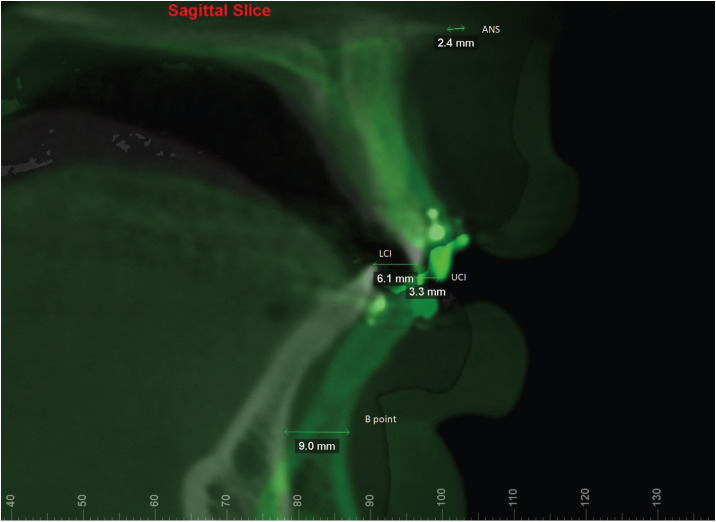
Superimposition of T0 and T1 and measurements of the advancements at anterior nasal spine (ANS), upper central incisor (UCI), lower central incisor (LCI) and B point.
-Oropharynx dimensions evaluation
The Sinus/Airway Evaluation Tool in the Dolphin Imaging software was used for reconstruction and evaluation of the oropharynx (12,15-18,21). At First, the oropharynx anatomical references were delimited in the medial sagittal reconstruction and described such as: anterior, lateral and posterior limits were defined by soft tissue contour of pharyngeal walls; upper limit, retropalatal region delimited by a parallel line to the horizontal plane from posterior nasal spine extending to the posterior wall of the pharynx; lower limit, a parallel line to the horizontal plane crossing at the height of the base of the epiglottis to posterior wall of hypopharynx.
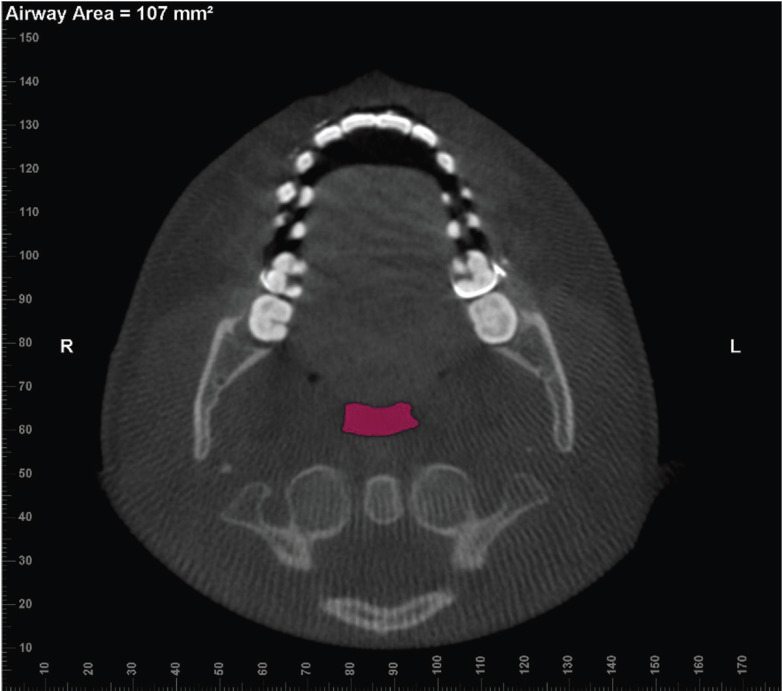
Next, the Add Seed Points Tool was used to insert seed points inside this area. The detection sensitivity of the airway space was standardized at 25%, and the Update Volume Tool was used to calculate the medial sagittal area in mm2 (MSA) and the Volume in the airway space of oropharynx in mm3, as previously delimited (Fig. (Fig.2)2) (13). The minimum cross-sectional axial area in mm2 (CSA) was measured using the option Enable Minimum Axial Area in the axial view (Fig. (Fig.3).3). All analysis was performed by the same evaluator (C.B.L) limiting a maximum of 5 subject CBCT images at 1-week intervals. All workflow of oropharynx dimension evaluations was measured twice considering abovementioned interval of times.
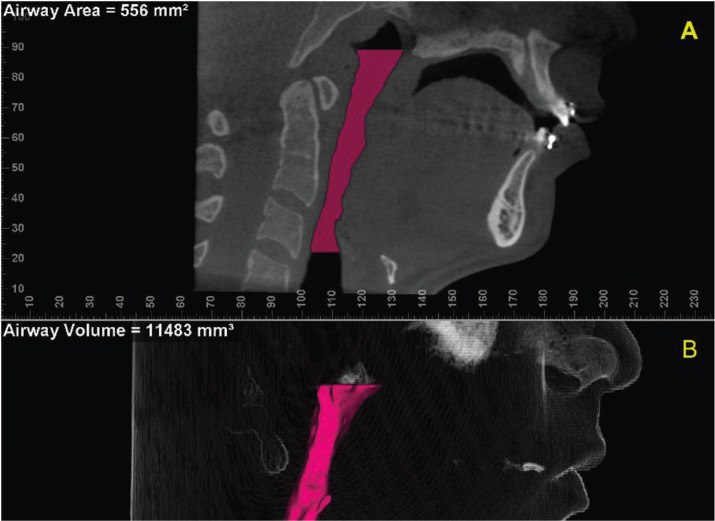
Oropharynx delimited in the CBCT: (A) Sagittal reconstruction indicating the medial sagittal area (MSA); (B) Three-dimensional reconstruction indicating the volume of oropharynx.
-Statistical analysis
Statistical analysis was performed with SPSS software (Statistics IBM software version 15.0; IBM Corp, Armonk, NY). Pearson’s correlation coefficients (r) were calculated to assess reliability of the intra-rater method.
Descriptive analysis was able to show the minimum, maximum, means and standard deviation (SD) for linear measurements ANS, UCI, LCI and B point between pre- and post-operative images superimposed, according to G1, G2 and G3. Paired t-tests were used to compare oropharynx dimensions (MSA, volume and minimal CSA) between T0 and T1 in each group (G1, G2 and G3). Statistical significance was set at p ≤ 0.05.
Results
From 138 CBCT pre- and post-operative images assessed, 88 CBCT images were selected according to inclusion criteria. Hence, forty-four skeletal class II patients were analyzed for the study sample, 33 females and 11 males, and range in age from 18 to 40 years.
Pearson’s correlation coefficient was excellent (r ≥ 0.93) showing intra-rater agreement, and the method was reliable. The patients were assigned to 13 subjects in G1 (B point measurement < 5 mm), 19 in G2 (5 mm < B point measurement < 10 mm), and 12 in G3 (B point measurement ≥ 10 mm). Table 1 presents mean B point measurement and descriptive results of linear measurements between others cephalometric references from pre- and postoperative CBCT image superimpositions.
Table 1
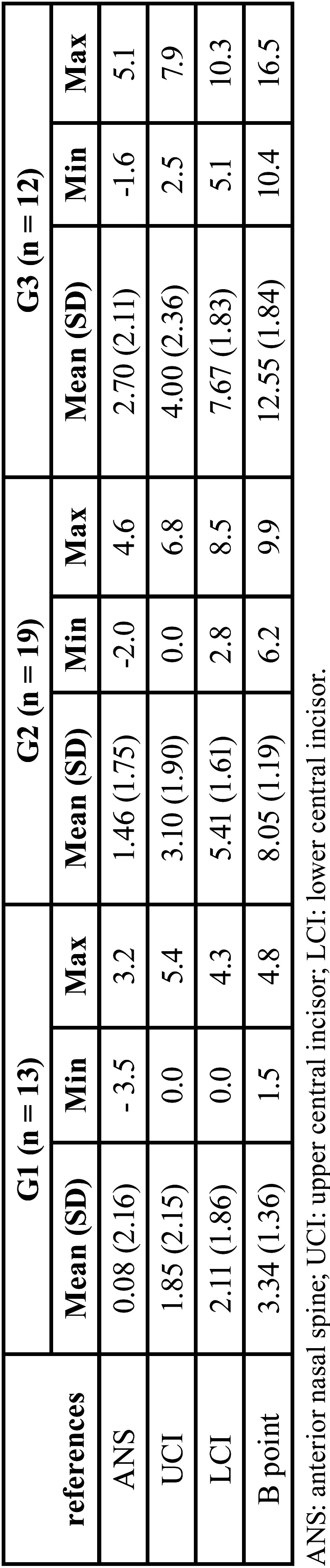
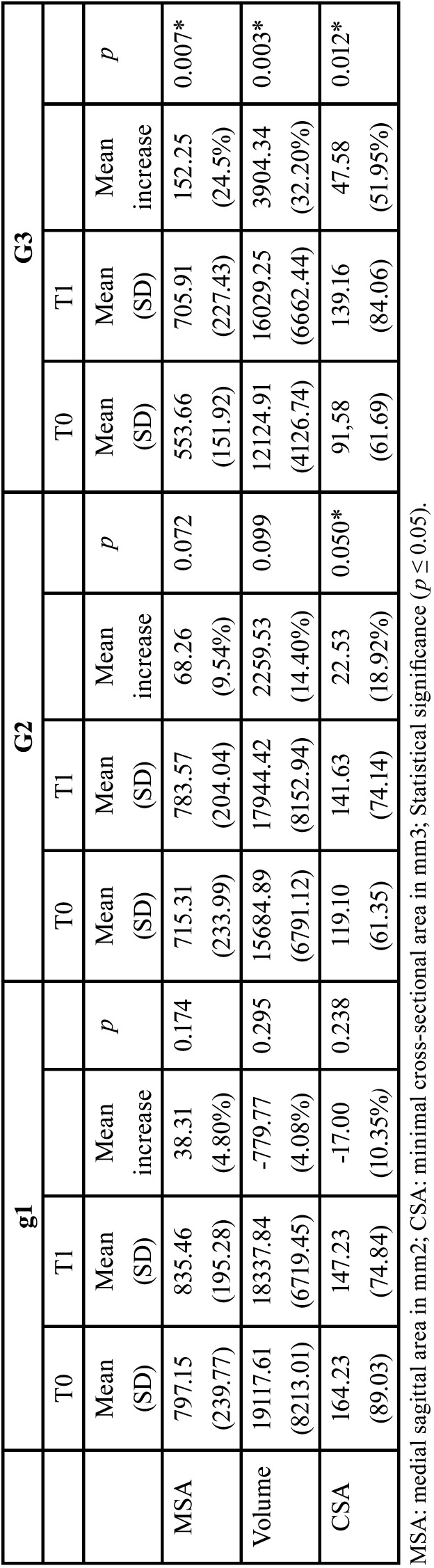
Table 2 presents Paired t-test results, which were statistically significant (p ≤ 0.05) for G3 when values of the MSA, volume and CSA were compared between pre-(T0) and postoperative (T1). For G3 subjects, Table 2 shows that there was a mean higher than 20% increase in the oropharynx dimension considering MSA, Volume and CSA measured.
Table 2
Discussion
Oropharynx dimensions has been selected for assessment in retrognathic patients since they can present constriction areas in the UA (6). Afterward orthognathic surgery, mandibular movements can be more susceptible to provide effects in the oropharynx region than nasopharynx and hypopharynx (1,5,13). And, mandibular advancements presented more favorable impact than maxillary movements in the oropharynx dimensions (8). Hence, our method categorized each subject (pre-operative CBCT image) regarding at different mandibular advancement (G1, G2 and G3), and then, evaluated the effects in the oropharynx dimension comparing pre- (T0) and postoperative (T1) CBCT images.
From assessment of UA comparing between lateral cephalometric radiographs and CBCT images, Aboudara et al. (2009) established that CBCT scan is a simple and effective method to provide an accurately analysis of the airway area and volumetric measurement. As CBCT segmentations in software became possible, several methods have been developed to measure UA after orthognathic surgery, providing the accurate morphology by means of the measurements of MSA, minimal CSA, and volume (1). Commonly, volume and minimal CSA were considered the most important parameters for showing the total gain capacity of the oropharynx dimension (1,6,22). Our results indicated higher effects in the oropharynx dimensions after CCW maxillomandibular complex rotation from increasing the volume and minimal CSA measurements means, regardless group or statistically significant difference.
In accordance with each category of the subjects (G1, G2 and G3), mandibular advancements lower than 5 mm (G1) did not produce significant changes in the oropharynx dimensions in any of the variables. The lack of change may be related to the small amount of advancement, which may have been insufficient to stretch the suprahyoid musculature (17). Nevertheless, a significant increase in UA space with similar advancements has been reported. Ristow et al. (2018) found a significant difference in oropharynx volume and minimal CSA, with a mean value of mandibular advancement of 4.77 mm measured at three different points (left and right mental foramen and pogonion). These authors used two different programs to evaluate mandibular advancement and the airways, instead of using Dolphin Imaging. Hence, different software for assessing UA may generate differences among the results (24).
Previous studies have presented significant improvements in minimal CSA and volume with mandibular advancements between 5 and 10 mm (13,17,21). This is partially in accordance with the present study since G2 presented significant improvements in minimal CSA, but no statistically significant difference was observed when the oropharynx volume was evaluated. This difference in volume can be explained by stipulating different anatomical limits for oropharynx, patient position during computerized tomography acquisition, planning of different surgical advancements, and the time elapsed for evaluation. Based on method of anatomical delimits, Brunetto et al. (2014) included part of the nasopharynx in their analysis and performed higher maxillary advancements (mean 4.71 mm), whereas our method was restricted to oropharynx and mean of maxillary advancement was 1.46 mm at ANS and 3.10 mm at UCI (G2). In addition to using different anatomical limits, Kochar et al. (2016) evaluated the oropharynx dimensions after isolated mandibular surgeries by using multislice computerized tomography. Hence, differences between results may be related to patient position during scans images because our protocol of CBCT scans were performed in sitting position, whereas supine position in computerized tomography. Thus, we suppose that patient position may alter the UA due to the gravitational forces that displace the tongue and soft palate posteriorly (25). Kochar et al. (2016) and Brunetto et al. (2014) evaluated the UA at least 5 months of postoperatively, which may be different from an evaluation conducted during the immediate postoperative period (12).
Advancements higher than 10 mm are commonly related to an enlargement of the airways with linear bimaxillary advancement (3,5-7). However, these linear maxillary advancements are not always possible from an esthetic point of view, creating a biprotuse profile with an acute naso-labial angle (1). Thus, the CCW rotation, in addition to improving the airway, as shown in the present study (G3), enhances the esthetic profile of class II patients by optimizing the advancement of the pogonion and avoiding the unpleasant protrusion of the maxilla in the patient (4).
CCW rotation with mandibular advancements higher than 10 mm has been related to significant increases in MSA, volume and minimal CSA in the oropharynx (1,12,16,18). Raffaini and Pisani (2012) evaluated 10 patients with mandibular advancements ranging from 10 to 18 mm and showed gains in the oropharynx dimension of 34% in MSA, 56% in volume, and 112% in minimal CSA. Besides finding gains of 178 mm2 in surface area, 10.118 mm3 in volume, and 76.67 mm2 in CSA, Miranda et al. (2015) evaluated 23 patients with a mean advancement of 14 mm and did not report the sensitivity parameter of the airway used on Dolphin Imaging. Comparatively with our results, their values detected higher impact in the oropharynx dimensions because it may be related to sample size, amount of mandibular advancement, assessment of method, patient’s overweight, and individual differences in muscle tone around the pharyngeal airways (26).
Despite the present study did not consider long-term postoperative outcomes, previous study reported long-term stability of the skeletal movement after counterclockwise rotation using rigid fixation (27). And long-term stability of oropharyngeal airway space has also kept on sTable after postsurgical follow-up of 34 months (28). On the other hand, a long-term follow-up of the maintenance of the dimension of the UA after CCW rotation would require a strict control of all of the different variables which may predispose changes, such as an increase of the body mass index, muscle tone analysis, connective tissue flaccidity, and adipose tissue distribution (15).
There was limitation of our study because some important clinical evaluation should have been considered, such as body mass index, the Berlin questionnaire, the Epworth Sleepiness Scale, and polysomnography. And, we recognize that prospective study including different CCW advancements and evaluating three-dimensional changes with a strict control of the external factors that influences the changes in the UA would be conducted.
Conclusions
In subjects with mandibular advancements between 5 and 10 mm, only minimal CSA was significantly affected from comparing pre- and post-operative. Values of MSA, volume and CSA showed a significant increase in the oropharynx dimension of the subjects with mandibular advancements higher than 10 mm. Therefore, range of mandibular advancements showed different effects in the upper airway space, and it should be considered in CCW rotation planning to look forward to favorable post-operative results in the oropharynx.
Acknowledgments
Ackcnowledgements This work was supported by the Department of Oral and Maxillofacial Surgery, Rio de Janeiro State University, Rio de Janeiro, Brazil.
${Availability of data and materials} None declared.
Authors contributions None declared.
Ethics Anonymous data from cone beam computed tomography of patients that had undergone orthognathic surgery were analyzed after approval by human’s research Committee in Brazil (ethical standards applicable in 1964 Helsinki Declaration). The data were analyzed without personal identifying details. Ethical approval was supported by Ethics Committee of the Juiz de Fora Federal University, Minas Gerais, Brazil (Number: 2.195.162) and Pedro Ernesto University Hospital (Number: 2.450.559).
Conflicts of interest The authors declare that they have no conflict of interest.
Funding There was no funding for this study.
References
Articles from Journal of Clinical and Experimental Dentistry are provided here courtesy of Medicina Oral S.L
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Airway space changes after maxillomandibular counterclockwise rotation and mandibular advancement with TMJ Concepts® total joint prostheses: three-dimensional assessment.
Int J Oral Maxillofac Surg, 42(8):1014-1022, 29 May 2013
Cited by: 13 articles | PMID: 23726273
Three-dimensional comparison between the effects of mandibular advancement device and maxillomandibular advancement surgery on upper airway.
BMC Oral Health, 23(1):436, 30 Jun 2023
Cited by: 1 article | PMID: 37391785 | PMCID: PMC10314553
Pharyngeal airway changes in Class III patients treated with double jaw orthognathic surgery--maxillary advancement and mandibular setback.
J Oral Maxillofac Surg, 70(11):e639-47, 01 Nov 2012
Cited by: 15 articles | PMID: 23078826
Three-dimensional changes to the upper airway after maxillomandibular advancement with counterclockwise rotation: a systematic review and meta-analysis.
Int J Oral Maxillofac Surg, 47(5):622-629, 26 Nov 2017
Cited by: 7 articles | PMID: 29183699
Review

 2
2