Abstract
Purpose
To evaluate clinical-functional and radiologic outcomes of elderly patients with an unstable intertrochanteric femur fracture treated with a wedge wing in the lag screw.Materials and methods
Forty-eight patients treated with the Dyna Locking Trochanteric nail (DLT nail) to resolve an unstable intertrochanteric femur fracture were reviewed retrospectively. Based on AO/OTA classification, Fracture 31-A2 (34 cases) and 31-A3 (14 cases) were included in the analysis. We measured the femoral neck-shaft angle, tip-apex distance (TAD), Cleveland index, sliding distance of the lag screw, and time to the fracture union. The Harris Hip Score and Paker and Palmer's mobility score for clinical evaluation were used.Results
The mean follow-up period was 21.4 months (range, 12-34 months). The postoperative state of reduction was good in 28 cases and acceptable in 20 cases. The mean TAD was 20.5 mm. The position of the lag screw was center-center in 30 cases and center-inferior in 18 cases. The mean sliding distance of the lag screw was 3.4 mm at the last follow-up. The mean union time was 4.5 months. Two cases had complications which included a cut-out (1 case) and non-union (1 case). The mean Harris Hip Score was 86.5±8.3 (range, 76-90). Walking ability in 34 of the cases (70.8%) at last follow-up was similar to that prior to fracture.Conclusion
Functional and radiological outcomes are satisfactory using the DLT nail in the treatment of elderly patients with unstable intertrochanteric fractures; however, wedge wing in the lag screw does not prevent implant-related complications.Free full text

Outcomes of Wedge Wing in the Lag Screw for Unstable Intertrochanteric Fractures in Elderly Patients
Abstract
Purpose
To evaluate clinical-functional and radiologic outcomes of elderly patients with an unstable intertrochanteric femur fracture treated with a wedge wing in the lag screw.
Materials and Methods
Forty-eight patients treated with the Dyna Locking Trochanteric nail (DLT nail) to resolve an unstable intertrochanteric femur fracture were reviewed retrospectively. Based on AO/OTA classification, Fracture 31-A2 (34 cases) and 31-A3 (14 cases) were included in the analysis. We measured the femoral neck-shaft angle, tip-apex distance (TAD), Cleveland index, sliding distance of the lag screw, and time to the fracture union. The Harris Hip Score and Paker and Palmer's mobility score for clinical evaluation were used.
Results
The mean follow-up period was 21.4 months (range, 12–34 months). The postoperative state of reduction was good in 28 cases and acceptable in 20 cases. The mean TAD was 20.5 mm. The position of the lag screw was center-center in 30 cases and center-inferior in 18 cases. The mean sliding distance of the lag screw was 3.4 mm at the last follow-up. The mean union time was 4.5 months. Two cases had complications which included a cut-out (1 case) and non-union (1 case). The mean Harris Hip Score was 86.5±8.3 (range, 76–90). Walking ability in 34 of the cases (70.8%) at last follow-up was similar to that prior to fracture.
Conclusion
Functional and radiological outcomes are satisfactory using the DLT nail in the treatment of elderly patients with unstable intertrochanteric fractures; however, wedge wing in the lag screw does not prevent implant-related complications.
INTRODUCTION
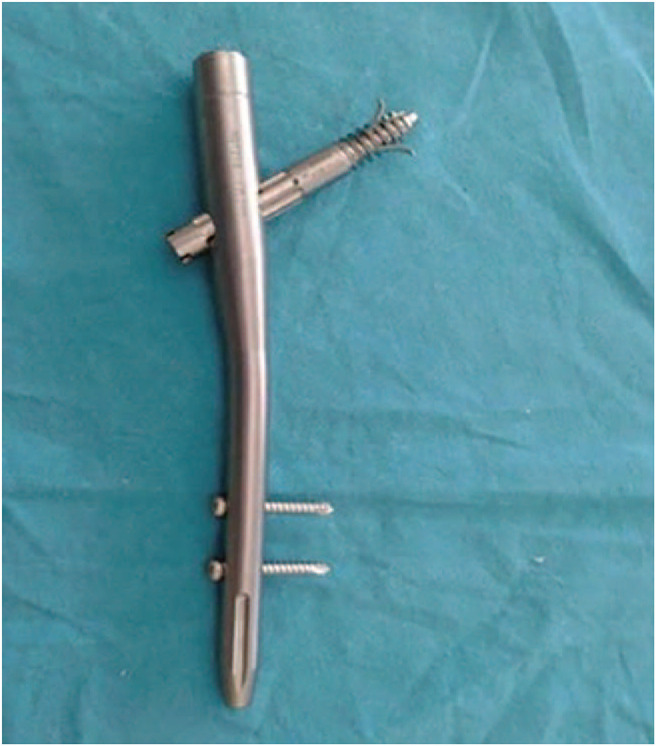
There are many available devices or implants to treat unstable intertrochanteric femur fractures. The type of implant used for the fixation of an intertrochanteric fracture can be broadly divided into intramedullary devices and extramedullary devices. An intramedullary nail (IMN) consists of a dynamic lag screw that passes through a short IMN. It confers a short-term advantage of full weight-bearing capacity shortly after implantation. A dynamic hip screw (DHS) with a side plate assembly is the most commonly used device for fixation of an intertrochanteric fracture. It is a non-collapsible fixation device that permits the proximal fragment to collapse or settle on the fixation device seeking its own position of stability1). Drawbacks to the DHS include complications such as varus deformity and lag screw cut-out. Alternatively, the wedge wing type screw (Dyna Locking Trochanter®[DLT]; U&I Corporation, Seoul, Korea) has the advantage of improving the fixation force by protruding the wing from the lag screw in patients with an unstable intertrochanteric fracture2,3).
There are limited studies regarding clinical outcomes of the DLT nail used for intertrochanteric femur fractures. Therefore, in the current study, we report the radiological and clinical results of unstable intertrochanteric fractures repaired using the DLT nail with wedge wing of the lag screw (Fig. 1).
MATERIALS AND METHODS
This study was approved by the Institutional Review Board (IRB) of Wonkwang University Hospital (No. WKUHIRB-2020-04-020) and the informed consent was waived by the IRB.
1. Patients
Among the 58 patients with an intertrochanteric fracture who underwent surgery using a lag screw with a wedge wing between January 2013 and January 2017 in the Wonkwang University Hospital, 48 patients who were followed-up for more than 12 months were included in the study. This study included patients with an unstable intertrochanteric fracture (AO/OTA 31-A2, A3) and osteoporosis on bone mineral density performed before surgery of −2.5 or less. Patients with osteopenia greater than −2.5 were excluded. The 10 excluded cases consisted of three cases of death, two cases with another orthopedic surgery performed simultaneously on the lower extremity, and five cases with a follow-up of less than a year. The fractures were classified as 31-A2 in 34 cases and 31-A3 in 14 cases according to the AO/OTA classification (Table 1). The patients consisted of 18 males (37.5%) and 30 females (62.5%) with a mean age of 77.1 ±5.3 years (range, 75–95 years). Bone density was measured by Dual Energy X-ray Absorptionmetry (DEXA), and the scores were normalized to the T-score at the femoral neck. The mean score was −3.56±1.1 (−2.6 to −4.9). The mean follow-up period was 21.4±9.6 months (range, 12–34 months). The most common comorbidity was hypertension (24 cases), followed by diabetes, cardiovascular diseases, stroke, and chronic kidney disease in 17, 9, 7, and 5 cases, respectively (Table 1). The American Society for Anesthesiologist (ASA) score4), an assessment of preoperative health status, was graded as stage 2 in 27 cases and stage 3 in 21 cases. For those patients on anticoagulants, medication was stopped for 4 to 5 days prior to surgery in order to minimize bleeding during and after surgery and to prevent aggravation of underlying diseases.
Table 1
| Demographic data | Value | |
|---|---|---|
| AO/OTA classification | ||
| 31-A2 | 34 | |
| 31-A3 | 14 | |
| Sex | ||
| Male | 18 (37.5) | |
| Female | 30 (62.5) | |
| Mean age (yr) | 77.1±5.3 (75-95) | |
| Mean F/U period (mo) | 21.4±9.6 (12-34) | |
| Underlying disease | ||
| Hypertension | 24 | |
| Diabetes mellitus | 17 | |
| Cardiovascular disease | 9 | |
| Cerebrovascular disease | 7 | |
| Chronic kidney disease | 5 | |
Values are presented as number only, number (%), or mean±standard deviation (range).
F/U: follow-up.
2. Surgical Technique & Postoperative Rehabilitation
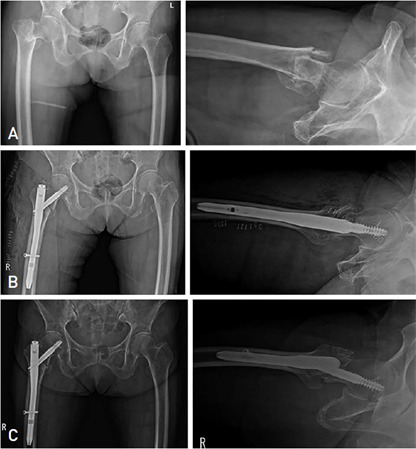
Operations were performed using an image amplifier on the fracture operating table. If radiographic findings showed that the proximal bone fragment was displaced outward from the distal fragment, the fractured portion of the bone was towed, and the distal fragment was displaced outward using a Steinmann pin. The proximal bone fragment was displaced inward to overlap the distal bone fragment or displaced 5 mm further inward to reduce the valgus. When the proximal fragment was displaced posteriorly, a Hohmann retractor was inserted between the fractures. After the proximal fragment spanned the anterior cortical bone, the proximal fragment was reduced interiorly in the first half in the form of levers and overlapped the distal fragments. If the proximal bone fragment was displaced inward, the lag screw was fixed after pulling and holding it toward the distal bone fragment using a retractor. On the anteroposterior view of the image amplifier, it is observed in the form of the valgus within 5°. On the lateral view of the image amplifier, the proximal bone fragment was observed 1 cm ahead of the distal bone fragment (Fig. 2). A guide pin was fixed to the acetabulum to prevent the deformation of the femoral head and the varus during the fixation of the lag screw. A Steinman pin was used to prevent external rotation of the proximal bone fragment. The lag screw inserted into the femoral head was positioned center-center or center-inferior when possible. In all cases, a 200-mm-long nail with a distal diameter of 10 mm or 11 mm and a lag screw angle of 130°was used. Active joint exercises were allowed as early as the day after the surgery. Seated and quadriceps muscle exercises were allowed from the first postoperative day, and ambulation with a wheelchair along with caregiver assistance was started on the 3rd to 5th day postoperative. Tolerable weight-bearing was instructed 7 days postoperative depending on the degree of reduction, systemic condition, and pain. Full weight-bearing ambulation with a walker was allowed 10 to 14 days postoperative.
3. Radiologic and Clinical Evaluation
Radiographic follow-up was performed immediately, 1 week, 3 months, 6 months, and 1 year after the surgery. The adequacy of the fracture reduction was evaluated using the modified Baumgaertner criteria suggested by Fogagnolo et al.5) (Table 2). The Cleveland index, which divides anteroposterior and lateral radiographs of the hip joint into nine zones, was used to classify the position of the lag screws in the femoral head6) (Fig. 3). Moreover, the tip-apex distance (TAD)7), which is the distance between the tip of the substitute and the cortex of the femoral head, was measured using the anteroposterior and lateral radiographs of the hip joint. The TAD and the femoral neck-shaft angle were measured immediately after the surgery and at the last follow-up. The femoral neck-shaft angle was the difference in the actual anatomical neck-shaft angle of the fused femur, not the metal that was inserted. This serves as an index for indirect evaluation of the degree of reduction after surgery. Cases with 10°or more of angular deformation were classified as varus deformity. If the bone union was not observed in the anteroposterior and lateral radiographs of the hip joint after 6 months, it was classified as non-union. The distance between the outer end of the lag screw and the outer cortical bone of the femur in the anteroposterior radiographs were measured. The degree of sliding was then calculated by measuring the difference between the measured distance and the bone union image at the last follow-up session. Surgical time, bleeding volume, and transfusion volume were evaluated retrospectively. The Harris Hip Score was used for clinical evaluation. In addition, recovery of walking ability and daily activity were used to evaluate recovery measured against the preoperative level8,9). A Mann–Whitney U-test was performed for statistical analysis.
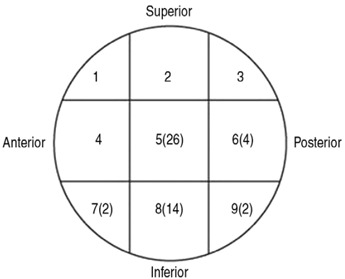
Table 2
| Radiologic evaluation | Value | |
|---|---|---|
| Postoperative reduction state | ||
| Good | 28 | |
| Acceptable | 20 | |
| Bone union | 40 | |
| Mean union period (wk) | 16.7±4.7 (14-27) | |
| Tip-apex distance (mm) | ||
| Postoperative | 17.1±3.8 (13-23) | |
| Last F/U | 20.5±4.1 (16-25) | |
| Neck-Shaft angle (。) | ||
| Postoperative | 135 | |
| Last F/U | 127 | |
| Sliding distance (mm) | 3.4 | |
| Cleveland index | ||
| 5 | 26 | |
| 6 | 4 | |
| 7 | 2 | |
| 8 | 14 | |
| 9 | 2 | |
Values are presented as number only or mean±standard deviation (range).
F/U: follow-up.
RESULTS
1. Radiologic Evaluation
Twenty-eight satisfactory cases and 20 acceptable cases of reduction were reported after surgery. Bone union was achieved in 40 (83.3%) of the 48 cases, and the mean union time was 16.7±4.7 weeks (range, 14–27 weeks). The mean postoperative TAD and TAD at the last follow-up was 17.1±3.8 mm (range, 13–23 mm) and 20.5±4.1 mm (range, 16–25 mm), respectively. The femoral neck-shaft angle was 135°after the operation and 127°at the last follow-up. Furthermore, the mean sliding distance of the lag screw was 3.4 mm. According to the Cleveland index, 26, 4, 2, 14, and 2 cases were observed in zones 5, 6, 7, 8, and 9, respectively. No cases were observed in zones 1, 2, 3, and 4.
2. Clinical Evaluation
The mean operation time was 41.0±10.8 minutes (range, 30–60 minutes) from skin incision to suture. The mean bleeding volume was 170.0±43.4 mL (range, 100–220 mL), and 13 patients were transfused when the hemoglobin level was 7 or lower after the surgery. The mean Harris Hip Score on the last follow-up was 86.5±8.3 (range, 76–90). Walking was started with partial weight loading using a walker. The mean gait period was 2.5±1.3 days (range, 3–7 days). Gait was delayed in two patients with long-term pneumonia treatment and in four patients with preoperative dementia. Walking ability was restored to pre-fracture level in 34 cases (70.8%), and in the remaining 14 cases (29.2%), subjects were able to walk with a cane or wheelchair, though they had not been used previously. Daily basic and instrumental activities were achieved in 34 cases and 14 cases, respectively (Table 3).
Table 3
| Clinical evaluation | Value | |
|---|---|---|
| Operating time (min) | 41.0±10.8 (30-60) | |
| Blood loss (mL) | 170.0±43.4 (100-220) | |
| Blood transfusion | 13 | |
| Harris Hip Score | 86.5±8.3 (76-90) | |
| Mean ambulation period (day) | 2.5±1.3 (3-7) | |
| Ambulatory ability | ||
| Pretrauma gait | 34 | |
| Cane or wheelchair | 14 | |
| Activity of daily living | ||
| Basic activity of daily living | 34 | |
| Instrumental activity of daily living | 14 | |
Values are presented as mean±standard deviation (range) or number only.
F/U: follow-up.
3. Complications
Systemic complications included two cases of pneumonia, three cases of urinary tract infection, and eight cases of delirium. Radiologically, there was one case of cut-through of the lag screw with a perforation of the femoral head (Fig. 2). Thus, a total of one case (2.1%) of fixation failure occurred; however, reoperation could not be performed due to worsening of the general condition of the patient.
DISCUSSION
The incidence rate of intertrochanteric fracture is gradually increasing in accordance with the growing elderly population. For unstable intertrochanteric fractures in the elderly, stable fixation is important to restore activity to the preoperative level and reduce the risk of reoperation, complications, and death10,11,12,13,14).
The IMN has a theoretical advantage as a load-sharing implant and can reduce the surgical time and amount of bleeding by using an obstructive technique. In order to increase the compression and stability of the fracture in the lag screw type, a groove was made in the lag screw, and the compression screw was fixed to induce sliding of the lag screw in a certain direction. However, biomechanical compression was not significantly different from the screw metal plate and complications such as cut-out could not be prevented15,16,17,18,19,20,21). Thus, variations of implants have been developed to prevent such issues. The blade type nail (PFNA; Synthes, Raynham, MA, USA) is an alternative characterized by inserting a spiral-shaped blade, which results in less bone loss in the femoral head and excellent fixation power, providing resistance to varus and rotational deformation. Another method utilizes a screw with u-blade type nail (Gamma-3; Stryker, Kalamazoo, MI, USA) which consists of one distal locking screw that has a flexible curved instrument shape to prevent compression of soft tissues and collision of iliac ridges. Another option includes integrated interlocking screws (Intertan; Smith & Nephew, London, UK) where the mechanism of the two screws directed to the femoral head enables linear compression during surgery and improves the rotational stability of the femoral head and neck bone fragments. Recently, the use of blade type and screw with u-blade type lag screws have been reported promising results. In the current study, the authors used a DLT nail with a wedge wing type lag screw that can achieve rotational stability in the femoral head while preserving the advantages of the existing lag screw in elderly patients with unstable intertrochanteric fracture. The use of the wedge wing of the DLT nail strengthens the fixation power in the femoral head, preventing cut-out and loss of reduction of the lag screw in patients with severe osteoporosis. Compared to other implants, dynamization of the distal occlusal screw fracture has the advantage of reducing the rate of fixation failure or reoperation.
The position of the lag screw (TAD<25 mm) is considered to be a critical factor in reducing the failure rate of internal fixation of a femoral head perforation10). Ruecker et al.13) reported disagreement in the ideal position of the lag screw in the femoral head. However, many authors state that it is ideal to position the lag screw in the center inferior location on the anteroposterior view and in the center on the lateral view17,18). Kuzyk et al.22) reported that the inferior position on the anteroposterior view maximizes biomechanical stiffness and that the center position on the lateral view helps to achieve maximum load-to-failure and minimum TAD. In the current study, the lag screws in the head were positioned in the center and inferior end on the anteroposterior view and in the center on the lateral view. The mean TAD was 18.5 mm (range, 14–25 mm). Perforation occurred in one case with a TAD of 25 mm and non-union occurred in one case with a thickness of 22 mm. The mean TAD was increased as it was difficult to locate within 10 mm of the femoral cartilage head to extend the wedge wing after the fixation of the lag screw. Kim et al.2) reported that DLT nails were a good option for intertrochanteric fractures for the first time in Korea. However, stable fractures and unstable fractures were observed in 22 cases and 14 cases, respectively, and the benefit of the wedge wing lag screw could not be confirmed in unstable fractures.
Temiz et al.23) reported zero cases of implant failure and cut-out, five cases of greater trochanter fracture, and three cases of varus deformity as a result of DLT treatment in 32 geriatric patients with unstable intertrochanteric fractures. However, Gunay et al.24) reported that 13 out of 51 elderly patients with intertrochanteric fractures over 80 years of age who were treated with DLT nails experienced cut-out complications. Thus, the authors reported that wedge wing lag screws do not function properly in unstable intertrochanteric fractures and that the reduction quality was the most important factor. In addition, Kim et al.2) stated that in a comparison of the three different types of lag screws, which included screw type, blade type, and wedge wing type, there were no differences in complications such as cut-out and that precise reduction of fracture site and surgical technique is fundamental. In the current study, it was observed that adequate reduction led to only one case of a cut-out. In particular, cutout may occur in the elderly when an unstable femoral intertrochanteric fracture is anatomically reduced. Thus, we attempted to reduce the proximal fragment to an extramedullary type instead of the distal fragment and reduce in the form of valgus within 5°to decrease the chance of complications. Notably, though implants cannot prevent complications, the quality of reduction and lag screw position is critical for the prevention of complications.
Fogagnolo et al.5) reported that the degree of reduction after surgery should be the normal femoral neck-shaft angle or slightly valgus on the anteroposterior view and within 20°on the lateral view. Andruszkow et al.25) stated that in order to prevent perforation of the femoral head, the femoral neck-shaft angle should be valgus at 5–10°compared to the contralateral side. In the current study, the proximal and distal fragments were displaced inward and outward, respectively, and the valgus was reduced. The proximal fragment was then displaced in the anterior direction and the lag screw was fixed. The mean postoperative femoral neck-shaft angle measured immediately after surgery was 135°on the anteroposterior view.
In our study, there was only one case of fixation failure, though we believe we used adequate lag screws for the types of fractures presented. The limitations of the current study include a small sample size and a short follow-up period. Moreover, factors related to fixation failure were not considered in this study and there were no selection criteria for the patient group as it is not a comparative study. Further follow-up studies will be needed to support the current findings.
CONCLUSION
Functional and radiological results obtained in this study using DLT nails in elderly patients with unstable intertrochanteric fractures were satisfactory.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
Articles from Hip & Pelvis are provided here courtesy of Korean Hip Society
Citations & impact
Impact metrics
Article citations
Comparative analysis of radiological outcomes among cephalomedullary nails: helical, screw and winged screw.
PeerJ, 12:e18020, 19 Sep 2024
Cited by: 0 articles | PMID: 39308830 | PMCID: PMC11416753
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Unstable intertrochanteric femur fractures in geriatric patients treated with the DLT trochanteric nail.
Injury, 46 Suppl 2:S41-6, 26 May 2015
Cited by: 15 articles | PMID: 26021665
Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures.
Injury, 48 Suppl 2:S72-S77, 01 Aug 2017
Cited by: 11 articles | PMID: 28802425
Radiographic and functional results of osteosynthesis using the proximal femoral nail antirotation (PFNA) in the treatment of unstable intertrochanteric femoral fractures.
Acta Orthop Traumatol Turc, 44(2):127-134, 01 Jan 2010
Cited by: 21 articles | PMID: 20676015
U-blade gamma 3 vs. gamma 3 nails for intertrochanteric hip fracture: Meta-analysis.
Front Surg, 9:1015554, 23 Nov 2022
Cited by: 1 article | PMID: 36504573 | PMCID: PMC9727099
Review Free full text in Europe PMC
Funding
Funders who supported this work.