Abstract
Importance
Distal radius fractures are common and are managed with or without surgery. Current evidence indicates surgical treatment is not superior to nonsurgical treatment at 12 months.Objective
Does surgical treatment for displaced distal radius fractures in patients 60 years or older provide better patient-reported wrist pain and function outcomes than nonsurgical treatment at 24 months?Design, setting, and participants
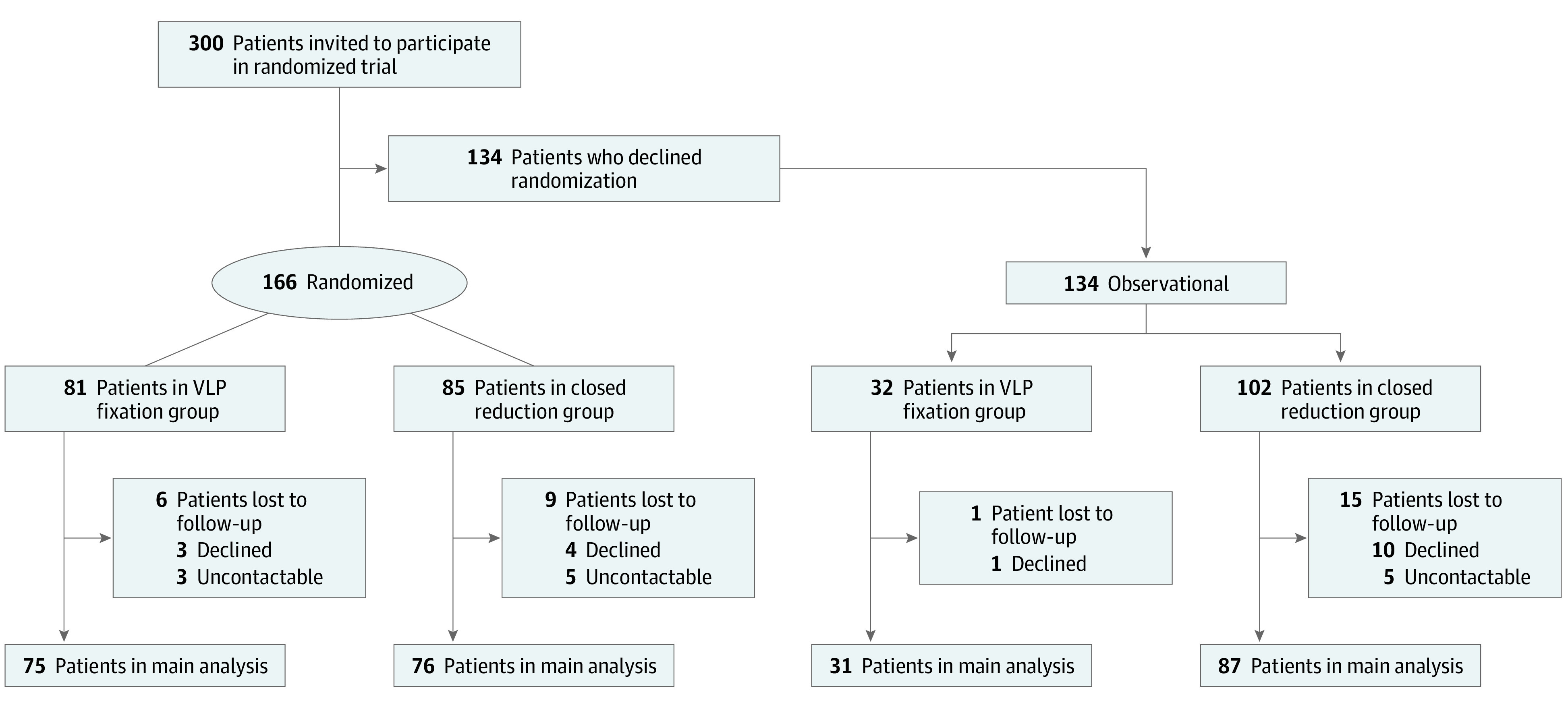
In this secondary analysis of a combined multicenter randomized clinical trial (RCT) and a parallel observational study, 300 patients were screened from 19 centers in Australia and New Zealand. Of these, 166 participants were randomized to surgical or nonsurgical treatment. Participants who declined randomization (n = 134) were included in the parallel observational group with the same treatment options and follow-up. Participants were followed up at 3, 12, and 24 months by a blinded assessor. The 24-month outcomes are reported herein. Data were collected from December 1, 2016, to December 31, 2020, and analyzed from February 4 to October 21, 2021.Interventions
Surgical treatment consisting of open reduction and internal fixation using a volar-locking plate (VLP group) and nonsurgical treatment consisting of closed reduction and cast immobilization (CR group).Main outcomes and measures
The primary outcome was patient-reported function using the Patient-Rated Wrist Evaluation (PRWE) questionnaire. Secondary outcomes included health-related quality of life, wrist pain, patient-reported treatment success, patient-rated bother with appearance, and posttreatment complications.Results
Among the 166 randomized and 134 observational participants (300 participants; mean [SD] age, 71.2 [7.5] years; 269 women [89.7%]), 151 (91.0%) randomized and 118 (88.1%) observational participants were followed up at 24 months. In the RCT, no clinically important difference occurred in mean PRWE scores at 24 months (13.6 [95% CI, 9.1-18.1] points for VLP fixation vs 15.8 [95% CI, 11.3-20.2] points for CR; mean difference, 2.1 [95% CI, -4.2 to 8.5]; P = .50). There were no between-group differences in all other outcomes except for patient-reported treatment success, which favored VLP fixation (33 of 74 [44.6%] in the CR group vs 54 of 72 [75.0%] in the VLP fixation group reported very successful treatment; P = .002). Rates of posttreatment complications were generally low and similar between treatment groups, including deep infection (1 of 76 [1.3%] in the CR group vs 0 of 75 in the VLP fixation group) and complex regional pain syndrome (2 of 76 [2.6%] in the CR group vs 1 of 75 [1.3%] in the VLP fixation group). The 24-month trial outcomes were consistent with 12-month outcomes and with outcomes from the observational group.Conclusions and relevance
Consistent with previous reports, these findings suggest that VLP fixation may not be superior to CR for displaced distal radius fractures for patient-rated wrist function in persons 60 years or older during a 2-year period. Significantly higher patient-reported treatment success at 2 years in the VLP group may be attributable to other treatment outcomes not captured in this study.Trial registration
ANZCTR.org Identifier: ACTRN12616000969460.Free full text

Plating vs Closed Reduction for Fractures in the Distal Radius in Older Patients
Key Points
Question
Does surgical treatment of wrist fractures with volar-locking plates in patients 60 years and older yield superior patient-reported wrist pain and function at 24 months after treatment compared with nonsurgical treatment?
Findings
In this secondary analysis of a randomized clinical trial and parallel observational study of 300 participants (166 who were randomized to surgical or nonsurgical treatment and 134 who declined randomization), no clinically important difference between treatment groups was found in wrist pain and function at 12 and 24 months, despite higher patient-reported treatment success in the surgical treatment group.
Meaning
These findings suggest that in patients 60 years and older, surgical treatment with volar-locking plates does not provide any important functional advantages over nonsurgical treatment at 12 and 24 months.
Abstract
Importance
Distal radius fractures are common and are managed with or without surgery. Current evidence indicates surgical treatment is not superior to nonsurgical treatment at 12 months.
Objective
Does surgical treatment for displaced distal radius fractures in patients 60 years or older provide better patient-reported wrist pain and function outcomes than nonsurgical treatment at 24 months?
Design, Setting, and Participants
In this secondary analysis of a combined multicenter randomized clinical trial (RCT) and a parallel observational study, 300 patients were screened from 19 centers in Australia and New Zealand. Of these, 166 participants were randomized to surgical or nonsurgical treatment. Participants who declined randomization (n = 134) were included in the parallel observational group with the same treatment options and follow-up. Participants were followed up at 3, 12, and 24 months by a blinded assessor. The 24-month outcomes are reported herein. Data were collected from December 1, 2016, to December 31, 2020, and analyzed from February 4 to October 21, 2021.
Interventions
Surgical treatment consisting of open reduction and internal fixation using a volar-locking plate (VLP group) and nonsurgical treatment consisting of closed reduction and cast immobilization (CR group).
Main Outcomes and Measures
The primary outcome was patient-reported function using the Patient-Rated Wrist Evaluation (PRWE) questionnaire. Secondary outcomes included health-related quality of life, wrist pain, patient-reported treatment success, patient-rated bother with appearance, and posttreatment complications.
Results
Among the 166 randomized and 134 observational participants (300 participants; mean [SD] age, 71.2 [7.5] years; 269 women [89.7%]), 151 (91.0%) randomized and 118 (88.1%) observational participants were followed up at 24 months. In the RCT, no clinically important difference occurred in mean PRWE scores at 24 months (13.6 [95% CI, 9.1-18.1] points for VLP fixation vs 15.8 [95% CI, 11.3-20.2] points for CR; mean difference, 2.1 [95% CI, −4.2 to 8.5]; P =
= .50). There were no between-group differences in all other outcomes except for patient-reported treatment success, which favored VLP fixation (33 of 74 [44.6%] in the CR group vs 54 of 72 [75.0%] in the VLP fixation group reported very successful treatment; P
.50). There were no between-group differences in all other outcomes except for patient-reported treatment success, which favored VLP fixation (33 of 74 [44.6%] in the CR group vs 54 of 72 [75.0%] in the VLP fixation group reported very successful treatment; P =
= .002). Rates of posttreatment complications were generally low and similar between treatment groups, including deep infection (1 of 76 [1.3%] in the CR group vs 0 of 75 in the VLP fixation group) and complex regional pain syndrome (2 of 76 [2.6%] in the CR group vs 1 of 75 [1.3%] in the VLP fixation group). The 24-month trial outcomes were consistent with 12-month outcomes and with outcomes from the observational group.
.002). Rates of posttreatment complications were generally low and similar between treatment groups, including deep infection (1 of 76 [1.3%] in the CR group vs 0 of 75 in the VLP fixation group) and complex regional pain syndrome (2 of 76 [2.6%] in the CR group vs 1 of 75 [1.3%] in the VLP fixation group). The 24-month trial outcomes were consistent with 12-month outcomes and with outcomes from the observational group.
Conclusions and Relevance
Consistent with previous reports, these findings suggest that VLP fixation may not be superior to CR for displaced distal radius fractures for patient-rated wrist function in persons 60 years or older during a 2-year period. Significantly higher patient-reported treatment success at 2 years in the VLP group may be attributable to other treatment outcomes not captured in this study.
Trial Registration
ANZCTR.org Identifier: ACTRN12616000969460
Introduction
Wrist fractures are the most common type of upper limb fractures.1,2 They are particularly common in older people owing to their increased risk of falls and osteoporosis, and incidence appears to be increasing.3,4 Disability from wrist fractures in older people can significantly impact independence.5 Direct treatment costs are forecast to rise substantially given the aging population and increasing incidence of wrist fractures.6
The 2 most common treatments for wrist fracture are nonsurgical treatment by closed reduction and cast immobilization (CR) and surgical treatment by open reduction and fracture fixation using a volar-locking plate (VLP).7 Surgical treatment, including VLP fixation, has been shown to produce better fracture alignment than CR.8,9,10,11,12,13,14 However, in older patients, VLP fixation has also been shown to offer no clinically important benefit in patient-reported pain and function over CR at 12 months.9,11,12,13,14,15,16,17 There has also been shown to be little if any association between radiographic and functional outcomes (A.L., J.N., W.X., R.M., M.K., and I.A.H., unpublished data, 2022).18,19,20,21 The synthesized evidence comparing posttreatment complications for these 2 types of treatment is less clear. Although 2 systematic reviews14,15 found higher rates of overall complications and reoperation with CR, another13 found no difference, and other reviews9,10,12 found significantly lower rates of major complications with CR.
In an effort to clarify both the short- and long-term results for VLP fixation compared with CR, we conducted a randomized clinical trial (RCT) testing the superiority of VLP fixation vs CR for the treatment of displaced distal radius fractures in patients 60 years and older: the CROSSFIRE (Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly) trial.16 At 1 year, VLP was not superior to CR for patient-reported wrist function, quality of life, wrist pain, bother with appearance, and posttreatment complications; however, patient-reported treatment success significantly favored VLP fixation. The present report described the 24-month patient-reported outcomes and complications of the CROSSFIRE trial.
Methods
CROSSFIRE was a multicenter combined RCT and parallel observational study comparing outcomes of VLP fixation with CR in the treatment of displaced distal radius fractures in patients 60 years and older. CROSSFIRE was approved by the Hunter New England Local Health District human research ethics committee. All study participants provided written informed consent. Methods for the CROSSFIRE study have been described in the published protocol22 and the statistical analysis plan23; the trial protocol is available in Supplement 1. Participants were followed up at 3, 12, and 24 months by a blinded investigator via telephone. The 3- and 12-month outcomes have been reported previously.16 This secondary analysis reports the 24-month outcomes, although some previously reported data are also presented to provide context. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Outcomes
Data for this analysis were collected from December 1, 2016, to December 31, 2020. The primary outcome was the total score on the Patient-Rated Wrist Evaluation (PRWE) questionnaire administered at the 24-month (within 1 month) follow-up. The PRWE consists of a pain component (50 points) and a function component (50 points) producing a total score of 100, with higher scores indicating poorer outcomes. We considered 14 points on the PRWE to be the minimal clinically important difference (MCID) necessary to justify the additional costs and risks of surgery compared with nonsurgical treatment.24 The pain and function domain scores of the PRWE underwent a separate sensitivity analysis.
Secondary outcomes were utility-based quality of life at 24 months based on the EuroQol (EQ) 5-dimension 5-level score (MCIDs, 0.074 for EQ utility index scores and 10.8 points for EQ visual analog scale scores25); wrist pain using a numeric rating scale of 0 to 10 points, with 0 indicating no pain and 10 indicating maximal pain (MCID, 1.7 points based on the median of a systematic review of MCIDs for pain scales26); patient-reported treatment success at 3 and 12 months measured on a Likert scale, ranging from very successful to very unsuccessful; patient-rated bother with appearance at 12 months (the bother question has been assessed for reliability in wrist fractures27); and complications, including deep infection, reoperation, neuropathy, tendon irritation that required treatment, tendon rupture, fracture nonunion at 6 months, implant failure, complex regional pain syndrome, and death.
Statistical Analysis
Data were analyzed from February 4 to October 21, 2021. Data were analyzed based on intention to treat at 3 time points. We used SAS statistical software, version 9.4 (SAS Institute Inc), and R statistical computing software, version 3.4.4 (R Foundation for Statistical Computing). Continuous outcomes were reported as means and SDs. The mean differences (MDs) between treatment groups were tested using 2-sample t tests. Categorical and binary outcomes were reported as frequency and incidence with risk ratios (RRs) calculated between treatment groups. Repeated measures were analyzed using analysis of variance.
If a participant provided data at 24 months, they were included in the analysis. Participants were lost to follow-up if they could not be contacted or declined to participate in follow-up. We did not impute missing data for the analysis of 24-month outcomes, consistent with the analysis of 12-month outcomes. To investigate the influence of missing data, we compared the baseline characteristics of those participants who were included in the final analysis with those who were lost to follow-up. Further details are provided in the statistical analysis plan.23
To investigate effects of potential confounders, we performed a regression analysis on 12- and 24-month PRWE scores. We used generalized linear modeling to analyze the effect of treatment, adjusting for covariates including age, sex, fracture type (AO/Orthopaedic Trauma Association classification type 23A [extra-articular] and 23C [intra-articular]), patient preference, and health-related quality of life (EQ visual analog scale). Race and ethnicity data were not considered relevant to the study and were not collected. Two-sided P < .05 indicated statistical significance.
Results
A total of 300 patients were included (mean [SD] age, 71.2 [7.5] years; 269 women [89.7%] and 31 men [10.3%]). From the original 166 randomized participants, 151 (91.0%; 75 of 81 [92.6%] from the VLP fixation group and 76 of 85 [89.4%] from the CR group) were followed up at 24 months. From 134 observational participants, 118 (88.1%; 31 of 32 [96.9%] from the VLP group and 87 of 102 [85.3%] from the CR group) were followed up at 24 months (269 of 300 [89.7%] combined) (Figure 1). Among the 300 RCT and observational participants, 18 declined participation and 13 could not be contacted at 24 months. Baseline (presurgical) characteristics for patients in the RCT are compared in Table 1. The characteristics of those included in the analysis were similar to characteristics of those who were lost to follow-up, apart from smoking prevalence, which was significantly higher in the group lost to follow-up (4 of 166 [2.4%] vs 2 of 15 [13.3%]; P = .003) (eTable 1 in Supplement 2).
Table 1.
| Baseline measure | Treatment group | |
|---|---|---|
CR (n = = 85) 85) | VLP fixation (n = = 81) 81) | |
| Age, mean (range), y | 71.3 (60-90) | 70.5 (60-86) |
| Sex | ||
| Women | 75 (88.2) | 70 (86.4) |
| Men | 10 (11.8) | 11 (13.6) |
| Fracture type | ||
| 23A | 49 (58.3) | 55 (67.9) |
| 23C | 35 (41.7) | 26 (32.1) |
| Comorbidities | ||
| Diabetes | 9 (10.6) | 10 (12.3) |
| Smoker | 3 (3.5) | 1 (1.2) |
| Glucocorticoid treatment | 10 (11.8) | 10 (12.3) |
| Osteoporosis treatment | 10 (11.8) | 10 (12.3) |
| Treatment preference | ||
| Surgery | 5 (5.9) | 10 (12.6) |
| Closed reduction | 24 (28.2) | 25 (31.6) |
| No preference | 56 (65.9) | 44 (55.7) |
| EQ-5D-5L score, mean (SD)b | ||
| Index | 0.89 (0.14) | 0.85 (0.19) |
| Visual analog scale | 83.6 (14.4) | 81.1 (17.4) |
Abbreviations: CR, closed reduction and cast immobilization; EQ-5D-5L, EuroQol 5-dimension 5-level; VLP, volar-locking plate.
Patient-Reported Outcomes
For participants in the RCT, mean PRWE scores were 13.6 (95% CI, 9.1-18.1) for the VLP fixation group compared with 15.8 (95% CI, 11.3-20.2) for the CR group (MD, 2.1 [95% CI, −4.2 to 8.5]; P =
= .50) at 24 months. Repeated-measures analysis indicated a significant change in the between-group MDs over time (P
.50) at 24 months. Repeated-measures analysis indicated a significant change in the between-group MDs over time (P =
= .03) (Figure 2), with a larger early difference favoring VLP fixation that decreased over time (MD of 9.0 for 3 months, 28.1 [95% CI, 23.0-33.2] vs 37.1 [95% CI, 32.1-42.1]; MD of 1.7 for 12 months, 19.8 [95% CI, 14.7-24.9] vs 21.5 [16.5-26.5]). There was no difference between groups in mean PRWE pain domain scores (MD,
.03) (Figure 2), with a larger early difference favoring VLP fixation that decreased over time (MD of 9.0 for 3 months, 28.1 [95% CI, 23.0-33.2] vs 37.1 [95% CI, 32.1-42.1]; MD of 1.7 for 12 months, 19.8 [95% CI, 14.7-24.9] vs 21.5 [16.5-26.5]). There was no difference between groups in mean PRWE pain domain scores (MD, 0.03 [95% CI, −3.30 to 3.35]; P
0.03 [95% CI, −3.30 to 3.35]; P =
= .99) and function domain scores (MD,
.99) and function domain scores (MD, 2.1 favoring VLP fixation [95% CI, −1.2 to 5.4]; P
2.1 favoring VLP fixation [95% CI, −1.2 to 5.4]; P =
= .21) (eTable 2 in Supplement 2). No between-group differences were found in pain (MD, 0.1 [95% CI, −0.5 to 0.7]; P
.21) (eTable 2 in Supplement 2). No between-group differences were found in pain (MD, 0.1 [95% CI, −0.5 to 0.7]; P =
= .69) or health-related quality of life measured by the EQ index score (MD, 0.04 [95% CI, −0.03 to 0.11]; P
.69) or health-related quality of life measured by the EQ index score (MD, 0.04 [95% CI, −0.03 to 0.11]; P =
= .24) and the EQ visual analog scale score (MD, 2.1 [95% CI, −4.5 to 8.7]; P
.24) and the EQ visual analog scale score (MD, 2.1 [95% CI, −4.5 to 8.7]; P =
= .53) (Table 2).
.53) (Table 2).
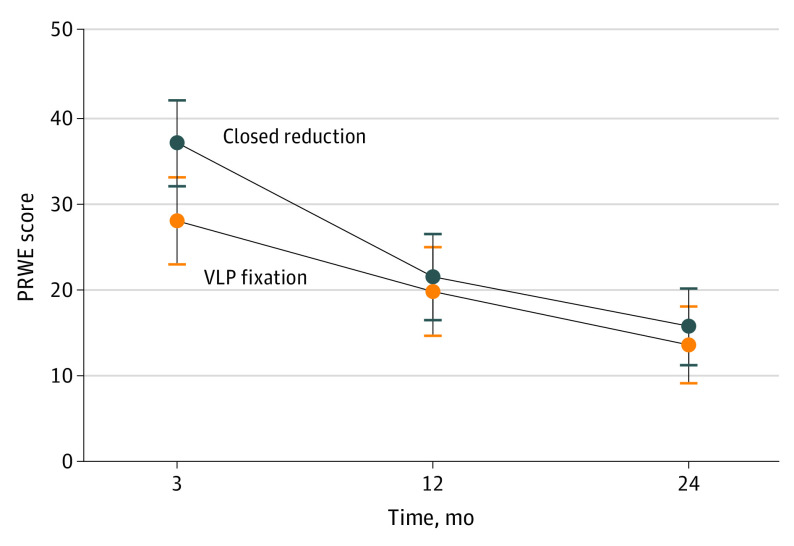
Error bars indicate 95% CIs. Changes in between-group mean differences over time were significant (P =
= .03). VLP indicates volar-locking plate.
.03). VLP indicates volar-locking plate.
Table 2.
| Outcome | Follow-up time, mo | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 3 | 12 | 24 | |||||||
| CR group (n = 85) | VLP fixation group (n = 79) | MD (95% CI) or RR (95% CI)a | CR group (n = 85) | VLP fixation group (n = 79) | MD (95% CI) or RR (95% CI) | CR group (n = 74) | VLP fixation group (n = 74) | MD (95% CI) or RR (95% CI)a | |
| PRWE score, mean (SD)b | 37.1 (22.3) | 28.1 (23.1) | 9 (1.8 to 16.2) | 21.5 (24.3) | 19.8 (21.1) | 1.7 (−5.4 to 8.8) | 15.8 (20.8) | 13.6 (18.1) | 2.1 (−4.2 to 8.5) |
| P value | NA | NA | NA | NA | NA | NA | NA | NA | .50 |
| DASH score, mean (SD) | NA | NA | NA | 19.6 (21) | 18.7 (20.1) | 0.9 (−5.6 to 7.4) | NA | NA | NA |
| EQ-5D-5L score, mean (SD) | |||||||||
| Index | 0.70 (0.24) | 0.74 (0.24) | −0.03 (−0.10 to 0.04) | 0.70 (0.23) | 0.69 (0.22) | 0.01 (−0.06 to 0.08) | 0.75 (0.21) | 0.75 (0.25) | 0.04 (−0.03 to 0.11) |
| P value | NA | NA | NA | NA | NA | NA | NA | NA | 0.24 |
| Visual analog scale | 76.0 (17.7) | 74.2 (21.2) | 1.8 (−4.3 to 7.9) | 73.9 (21.5) | 72.6 (19.3) | 1.4 (−5.0 to 7.7) | 76.4 (18.0) | 74.3 (22.4) | 2.1 (−4.5 to 8.7) |
| P value | NA | NA | NA | NA | NA | NA | NA | NA | .53 |
| Pain on NRS, mean (SD)c | 1.5 (2.5) | 1.1 (1.9) | 0.5 (−0.2 to 1.1) | 1.0 (2.1) | 1.1 (2.2) | −0.1 (−0.8 to 0.6) | 0.8 (2.1) | 0.6 (1.6) | 0.1 (−0.5 to 0.7) |
| P value | NA | NA | NA | NA | NA | NA | NA | NA | .69 |
| Patient-reported treatment success, No./total No. (%) | |||||||||
| Very successful | 21/80 (26.3) | 33/75 (44.0) | NA | 27/81 (33.3) | 42/79 (53.2) | NA | 33/74 (44.6) | 54/72 (75.0) | NA |
| Successful | 33.80 (41.3) | 28/75 (37.3) | NA | 30/81 (37.0) | 28/79 (35.4) | NA | 27/74 (36.5) | 15/72 (20.8) | NA |
| Neutral | 14.80 (17.5) | 5 (6.7) | NA | 9/81 (11.1) | 4/79 (5.1) | NA | 8/74 (10.8) | 1 (1.4) | NA |
| Unsuccessful | 6/80 (7.5) | 5 (6.7) | NA | 12 (14.8) | 5/79 (6.3) | NA | 4/74 (5.4) | 2 (2.8) | NA |
| Very unsuccessful | 6/80 (7.5) | 4 (5.3) | NA | 3 (3.7) | 0 | NA | 2/74 (2.7) | 0 | NA |
| P value | NA | NA | .10 | NA | NA | .03 | NA | NA | .002 |
| Patient-reported bother with appearance, No./total No. (%) | |||||||||
| Not at all | NA | NA | NA | 64/81 (79.0) | 69/77 (89.6) | NA | 64/74 (86.5) | 69/73 (94.5) | NA |
| Bothered a little | NA | NA | NA | 10/81 (12.3) | 7/77 (9.1) | NA | 7/74 (9.5) | 3/73 (4.1) | NA |
| Bothered moderately | NA | NA | NA | 6/81 (7.4) | 1/77 (1.4) | NA | 3/74 (4.1) | 1/73 (1.4) | NA |
| Very bothered | NA | NA | NA | 1/81 (1.2) | 0 | NA | 0 | 0 | NA |
| Extremely bothered | NA | NA | NA | 0 | 0 | NA | 0 | 0 | NA |
| P value | NA | NA | NA | NA | NA | .16 | NA | NA | .25 |
| Therapy use, No. (%) | |||||||||
| To 3 mo | 44 (54) | 56 (72) | 1.32 (1.04 to 1.69) | NA | NA | NA | NA | NA | NA |
| At 3 mo | 26 (59) | 22 (39) | 0.65 (0.43 to 0.98) | NA | NA | NA | NA | NA | NA |
Abbreviations: CR, closed reduction and cast immobilization; DASH, Disabilities of the Arm, Shoulder, and Hand questionnaire; EQ-5D-5L, EuroQol 5-dimension 5-level; MD, mean difference; NA, not applicable; NRS, Numeric Rating Scale; PRWE, Patient-Rated Wrist Evaluation; RR, risk ratio; VLP, volar-locking plate.
Patient-reported treatment success favored VLP fixation at 24 months, with 33 of 74 participants (44.6%) in the CR group vs 54 of 72 (75.0%) in the VLP fixation group reporting that their treatment was very successful (P =
= .002) (Table 2). Overall treatment success (very successful or successful) was significantly higher in the VLP fixation group (RR, 1.18 [95% CI, 1.05-1.33]; P
.002) (Table 2). Overall treatment success (very successful or successful) was significantly higher in the VLP fixation group (RR, 1.18 [95% CI, 1.05-1.33]; P =
= .006) (eTable 3 in Supplement 2). There was no significant between-group difference in patient-reported bother with appearance (Table 2).
.006) (eTable 3 in Supplement 2). There was no significant between-group difference in patient-reported bother with appearance (Table 2).
Complications
At 24 months, a total of 14 of 76 participants (18.4%) had complications in the CR group compared with 7 of 75 (9.3%) in the VLP fixation group (RR, 0.51 [95% CI, 0.22-1.18]) (Table 3). Complications led to additional operations in 8 participants, 6 in the CR group and 2 in the VLP fixation group (RR, 0.34 [95% CI, 0.07-1.62]). The incidence of fracture nonunion at 6 months was higher in the CR group (4 cases, 3 of which required further surgery, compared with none in the VLP fixation group). Incidence of other complications was very low and favored VLP fixation (deep infection, 1 [1.3%] vs 0; complex regional pain syndrome, 2 [2.6%] vs 1 [1.3%]) or was equivocal (tendon rupture, 1 [1.3%] vs 1 [1.3%]; implant failure, 1 [1.3%] vs 1 [1.3%]; and death, 1 [1.3%] vs 1 [1.3%]). Notably, deep infection (n =
= 1) and implant failure (n
1) and implant failure (n =
= 1) complications occurred in patients allocated to the CR group who crossed over to VLP fixation (2 of 75 [2.7%]). From 12 to 24 months, new complications occurred: tendon irritation (1 in each treatment group), implant failure (1 in the VLP fixation group), and death (1 in each treatment group).
1) complications occurred in patients allocated to the CR group who crossed over to VLP fixation (2 of 75 [2.7%]). From 12 to 24 months, new complications occurred: tendon irritation (1 in each treatment group), implant failure (1 in the VLP fixation group), and death (1 in each treatment group).
Table 3.
| Complication | Follow-up time, mo | |||||
|---|---|---|---|---|---|---|
| 12 | 24 | |||||
| RCT group, No. (%) | RR (95% CI)a | RCT group, No. (%) | RR (95% CI)a | |||
| CR (n = 84) | VLP fixation (n = 80) | CR (n = 76) | VLP fixation (n = 75) | |||
| Any complications | 12 (14.3) | 6 (7.5) | 0.53 (0.21-1.33) | 14 (18.4) | 7 (9.3) | 0.51 (0.22-1.18) |
| Deep infection | 1 (1.2)b | 0 | NA | 1 (1.3) | 0 | NA |
| Reoperation | 6 (7.1)c | 2 (2.5)d | 0.35 (0.07-1.68) | 6 (7.9) | 2 (2.7)e | 0.34 (0.07-1.62) |
| Neuropathy | 3 (3.6) | 3 (3.7) | 1.05 (0.22-5.05) | 3 (3.9) | 2 (2.7)e | 0.68 (0.12-3.93) |
| Tendon irritation requiring treatment | 0 | 1 (1.3) | NA | 1 (1.3)f | 2 (2.7)f | 2.03 (0.19-21.88) |
| Tendon rupture | 1 (1.2) | 1 (1.3) | 1.05 (0.07-16.50) | 1 (1.3) | 1 (1.3) | 1.01 (0.06-15.91) |
| Fracture nonunion at 6 mo | 4 (4.8) | 0 | NA | 4 (5.3) | 0 | NA |
| Implant failure | 1 (1.2)b | 0 | NA | 1 (1.3) | 1 (1.3)f | 1.01 (0.06-15.91) |
| Complex regional pain syndrome | 2 (2.4) | 1 (1.3) | 0.53 (0.05-5.68) | 2 (2.6) | 1 (1.3) | 0.51 (0.05-5.47) |
| Death | 0 | 0 | NA | 1 (1.3)f | 1 (1.3)f | 1.01 (0.06-15.91) |
Abbreviations: CR, closed reduction and cast immobilization; NA, not applicable; RCT, randomized clinical trial; RR, risk ratio; VLP, volar-locking plate.
 =
= 1), fracture nonunion requiring plating (n
1), fracture nonunion requiring plating (n =
= 1), hardware failure after early crossover to surgery (n
1), hardware failure after early crossover to surgery (n =
= 1), postoperative infection requiring surgical washout after crossing over to surgery (n
1), postoperative infection requiring surgical washout after crossing over to surgery (n =
= 1), and osteotomy at 6 months after initial treatment (n
1), and osteotomy at 6 months after initial treatment (n =
= 2).
2). =
= 1) and removal of hardware after tendon irritation at 3 months after initial treatment.
1) and removal of hardware after tendon irritation at 3 months after initial treatment.Observational Cohort
Findings in the observational group at 24 months were similar to findings in the RCT at 24 months. There were no clinically important between-treatment group differences. Mean (SD) PRWE scores were 4.9 (10.3) for VLP fixation compared with 6.8 (13.2) for CR (MD, 1.9 [95% CI, −3.3 to 7.1]). There were no between-group differences in other patient-reported outcomes, including treatment success (eTable 5 in Supplement 2). No between-group differences were found in the rate of complications at 24 months (eTable 5 in Supplement 2). In the regression analysis, the treatment effect was not different when it was adjusted for age, sex, fracture type, patient preference, and baseline health-related quality of life (EQ visual analog scale) at 12 months (MD, 2.2 [95% CI, 4.9-9.3]; P =
= .55) and at 24 months (MD, 1.9 [95% CI, −4.7 to 8.5]; P
.55) and at 24 months (MD, 1.9 [95% CI, −4.7 to 8.5]; P =
= .58) (eTable 4 in Supplement 2).
.58) (eTable 4 in Supplement 2).
Discussion
Main Findings
In this RCT, we found no clinically important difference in patient-reported wrist pain and function at 24 months after treatment for wrist fracture between the VLP fixation and CR groups (Table 2). Repeated-measures analysis revealed a significant change in patient-reported function with a large early mean change, decreasing to a negligible mean difference over time (Figure 2). We detected no clinically important between-group differences in quality of life, pain, or bother with appearance at all time points. However, there was a significant difference in patient-reported treatment success at 24 months favoring VLP fixation. These findings were consistent with the 12-month outcomes. The rates of posttreatment complications were generally low and similar between treatment groups, and there were few new complications reported from 12 to 24 months. The study was underpowered to detect significant between-group differences in complication rates. Given that 2 participants with known complications at 12 months were lost to follow-up at 24 months in the VLP group, it is possible that we underreported complications in the VLP group at final follow-up (Table 3).
Findings in the observational group were similar to those in the RCT. Regression analysis indicated that treatment outcome was not modified by age, sex, or other potentially important characteristics at 12 and 24 months after treatment.
We found that participants in the VLP fixation group reported significantly higher treatment success than participants in the CR group at both 12 and 24 months, despite there being no between-group difference in patient-reported wrist pain, function, health-related quality of life, and bother with appearance. Similarly, Hassellund et al17 found that patients undergoing VLP fixation were more satisfied than those undergoing CR at all time points. The between-group difference in reported treatment success may be attributed to an outcome associated with earlier recovery after VLP fixation or some other outcome that was not captured here but may be important to the patient nonetheless.28 Alternatively, given that participants were not blinded to treatment type, the difference may be due to patient expectations and beliefs that surgery is superior.29,30
Comparison With Similar Studies
Recent clinical practice guidelines on the treatment of wrist fractures31,32 were based largely on the evidence of 2 RCTs33,34 and offer uncertain and contradictory recommendations for treatment of wrist fractures in older patients. However, since 2018, several RCTs16,17,19,35,36,37,38 and at least 5 reviews11,12,13,14,15 have been published. Importantly, few studies comparing VLP fixation with CR have reported 24-month outcomes. One systematic review14 comparing the outcomes of VLP fixation with CR in adult patients reported no clinically important between-group difference in patient-reported function at 24 months, based on low-certainty evidence from 3 RCTs19,37,39 (241 participants) and an MD of 8.9 points (95% CI, 5.8-12.1 points; P <
< .001) on the Disabilities of the Arm, Shoulder, and Hand questionnaire, which is marginally lower than the MCID of 10 points.24 Only the RCTs by Martinez-Mendez et al19 reported PRWE scores at 24 months; of 97 participants 60 years and older, there was an MD of 13 points (95% CI, 5-21 points) points on the PRWE favoring the VLP group, marginally less than the MCID of 14 points.24 In comparison, at the same time point, we reported a between-group MD of 2.1 points (95% CI, −4.2 to 8.5 points) on the PRWE. However, Martinez-Mendez et al19 included only type 23C fractures, whereas our study included type 23A and 23C fractures. Although they did not report a crossover rate, Martinez-Mendez et al19 reported a 26% unacceptable loss of reduction in the CR group that might help explain the difference in functional outcomes at 24 months.
.001) on the Disabilities of the Arm, Shoulder, and Hand questionnaire, which is marginally lower than the MCID of 10 points.24 Only the RCTs by Martinez-Mendez et al19 reported PRWE scores at 24 months; of 97 participants 60 years and older, there was an MD of 13 points (95% CI, 5-21 points) points on the PRWE favoring the VLP group, marginally less than the MCID of 14 points.24 In comparison, at the same time point, we reported a between-group MD of 2.1 points (95% CI, −4.2 to 8.5 points) on the PRWE. However, Martinez-Mendez et al19 included only type 23C fractures, whereas our study included type 23A and 23C fractures. Although they did not report a crossover rate, Martinez-Mendez et al19 reported a 26% unacceptable loss of reduction in the CR group that might help explain the difference in functional outcomes at 24 months.
Another systematic review13 compared outcomes of VLP fixation with CR in the treatment of distal radius fractures in 561 older participants drawn from 6 studies.19,33,34,35,36,37 However, in that review, 12-month Disabilities of the Arm, Shoulder, and Hand questionnaire scores from certain studies33,34,35,36 were meta-analyzed with 24-month scores from other studies.19,37 The authors of the systematic review13 concluded that there was no clinically important between-group difference at final follow-up. A recent trial of 304 older participants38 compared the outcomes of CR with various forms of surgical treatment and reported no clinically important between-group difference in patient-reported function at 12 months and little change from 12 to 24 months despite a high rate of malunion in the CR group (59%).
CROSSFIRE was performed to clarify uncertainty in the evidence. Comparison RCTs had lower rates of follow-up,33,34 differential loss to follow-up,33,34,36,37 high rates of crossover between treatment groups,34 or high rates of reoperation.19,35 One review12 and 1 RCT19 based their conclusions on statistical significance rather than on clinical importance. In comparison, our study had high follow-up rates, low crossover rates, and low rates of revision, and our conclusions were based on comparison with prespecified MCIDs.
There is now enough certainty in the evidence comparing VLP fixation with CR in older patients to make strong as opposed to conditional treatment recommendations. Volar-locking plate fixation produces significantly better radiographic alignment than CR and enables earlier return to function. Although patient-reported treatment success is higher with VLP fixation, there is no difference in patient-reported function at 12 and 24 months, and the rate of major complications is not different. Given that there is no clear benefit to VLP fixation from 3 months after treatment, at the 2-year follow-up CR remains the preferred treatment option for most patients 60 years and older. The importance of early functional recovery and reasons for higher patient-reported treatment success with VLP fixation require further investigation.
Strengths and Limitations
Strengths of this study include the high rate of follow-up (89.7% combined, 91.0% for the RCT and 88.1% for the observational group) at 24 months and low rate of crossover (2.7% in the RCT) together with the inclusion of an observational (real-world) arm. There was little difference in baseline characteristics between participants from the RCT and the observational group, and findings from the RCT were similar to findings from the observational group, indicating that study findings were likely generalizable to individuals who did not participate in the RCT.
The main limitation of this study, as with many surgical trials, was that participants and surgeons could not be blinded to treatment allocation, creating the potential for performance and detection bias. Performance bias may explain the discrepancy between patient-reported treatment success and other patient-reported outcomes; however, any bias from unblinding is likely to favor the surgical group.29,30 We minimized this bias by using a blinded investigator to gather outcomes by telephone at all time points. Another limitation was that no screening log was used during recruitment, creating the potential for sampling bias.
Conclusions
The findings of this secondary analysis of an RCT suggest that VLP fixation of displaced type 23A and 23C distal radius fractures for patients 60 years and older may not lead to better wrist pain and functional outcomes at 24 months compared with CR. Significantly higher patient-reported treatment success at 24 months with VLP fixation may be attributable to performance bias or a treatment outcome not captured in this study. These findings are consistent with findings from the parallel observational study and from other RCTs.
Notes
Supplement 2.
eTable 1. Baseline Characteristics of Retained Participants vs Those Lost to Follow-up
eTable 2. PRWE Domain Scores
eTable 3. Treatment Success as a Binary Variable
eTable 4. Regression Analysis of Primary Outcome, Adjusting for Age, Sex, Fracture Type, Patient Preference, and Baseline Quality of Life (EQ-VAS Score)
eTable 5. Observational Group
References
Full text links
Read article at publisher's site: https://doi.org/10.1001/jamasurg.2022.0809
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9047748
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/127389294
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1001/jamasurg.2022.0809
Article citations
Non-surgical vs. surgical treatment of distal radius fractures: a meta-analysis of randomized controlled trials.
BMC Surg, 24(1):205, 10 Jul 2024
Cited by: 0 articles | PMID: 38987723
Review
Intra-Articular Corrective Osteotomy for Distal Radial Intra-Articular Malunion Using Patient-Matched Instruments: A Prospective, Multicenter, Open-Label, Single-Arm Trial.
JB JS Open Access, 9(3):e24.00026, 01 Jul 2024
Cited by: 0 articles | PMID: 39161933 | PMCID: PMC11328987
Complications after volar plate synthesis for distal radius fractures.
EFORT Open Rev, 9(6):567-580, 03 Jun 2024
Cited by: 1 article | PMID: 38828969 | PMCID: PMC11195338
Review Free full text in Europe PMC
Current Management and Volar Locking Plate Fixation with Bone Cement Augmentation for Elderly Distal Radius Fractures-An Updated Narrative Review.
J Clin Med, 12(21):6801, 27 Oct 2023
Cited by: 1 article | PMID: 37959267 | PMCID: PMC10648218
Review Free full text in Europe PMC
Surgical options for distal radius fractures of type C in elderly patients over 65 years old: a comparison of external fixation with Kirschner wires and volar locking plate.
J Orthop Surg Res, 18(1):669, 09 Sep 2023
Cited by: 1 article | PMID: 37689739 | PMCID: PMC10493013
Go to all (6) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Surgical Plating vs Closed Reduction for Fractures in the Distal Radius in Older Patients: A Randomized Clinical Trial.
JAMA Surg, 156(3):229-237, 01 Mar 2021
Cited by: 27 articles | PMID: 33439250 | PMCID: PMC7807386
Surgical plating versus closed reduction for fractures in the distal radius in older patients: a cost-effectiveness analysis from the hospital perspective.
ANZ J Surg, 92(12):3311-3318, 05 Nov 2022
Cited by: 1 article | PMID: 36333993 | PMCID: PMC10947348
Non-operative treatment or volar locking plate fixation for dorsally displaced distal radius fractures in patients over 70 years - a three year follow-up of a randomized controlled trial.
BMC Musculoskelet Disord, 23(1):447, 12 May 2022
Cited by: 8 articles | PMID: 35549696 | PMCID: PMC9097389
Are Volar Locking Plates Superior to Percutaneous K-wires for Distal Radius Fractures? A Meta-analysis.
Clin Orthop Relat Res, 473(9):3017-3027, 16 May 2015
Cited by: 39 articles | PMID: 25981715 | PMCID: PMC4523532
Review Free full text in Europe PMC
 1,2
1,2