Abstract
Purpose
To describe a case of a combined procedure including autokeratoplasty, pars plana vitrectomy (PPV), and scleral intraocular lens (IOL) fixation.Methods
Case report.Results
We describe a case of an 85-year-old patient presenting a right, blind eye with a clear cornea and a left eye with acceptable visual potential but affected by bullous keratopathy, aphakia, and a posteriorly dislocated nucleus. The patient underwent a contralateral autokeratoplasty, PPV, and flanged intrascleral IOL fixation with double needle technique. After 24 months of follow-up, the graft remained clear, and the IOL was stable.Conclusions
Complex cases comprising anterior and posterior segments pathology sometimes require combined procedures. A shortage of corneal tissue in developing countries is common. In strictly selected cases, autokeratoplasty may be an option and is associated with fewer complications than allograft corneal transplantation. Sutureless novel techniques for intrascleral fixation of IOL have shown good results and reliable lens stability.Free full text

Contralateral Autokeratoplasty, Pars Plana Vitrectomy for Luxated Cataract, and Flanged Intrascleral Intraocular Lens Fixation
Abstract
Purpose:
To describe a case of a combined procedure including autokeratoplasty, pars plana vitrectomy (PPV), and scleral intraocular lens (IOL) fixation.
Methods:
Case report.
Results:
We describe a case of an 85-year-old patient presenting a right, blind eye with a clear cornea and a left eye with acceptable visual potential but affected by bullous keratopathy, aphakia, and a posteriorly dislocated nucleus. The patient underwent a contralateral autokeratoplasty, PPV, and flanged intrascleral IOL fixation with double needle technique. After 24 months of follow-up, the graft remained clear, and the IOL was stable.
Conclusions:
Complex cases comprising anterior and posterior segments pathology sometimes require combined procedures. A shortage of corneal tissue in developing countries is common. In strictly selected cases, autokeratoplasty may be an option and is associated with fewer complications than allograft corneal transplantation. Sutureless novel techniques for intrascleral fixation of IOL have shown good results and reliable lens stability.
INTRODUCTION
Penetrating autokeratoplasty for unilateral corneal opacity has been described as a valid treatment for patients with a clear cornea in a contralateral blind eye. Frequent complications such as steroid-induced glaucoma and graft rejection would be avoided with this procedure,1,2 and it might be useful in developing countries as well where donor tissue could be scarce.3 When combined with pars plana vitrectomy (PPV) for mixed anterior and posterior segment disease, a temporary keratoprosthesis might be needed.4,5 In complex cases with cataract, aphakia, or a severely damaged anterior segment, placing an intraocular lens (IOL) in the capsular bag or the ciliary sulcus might not be feasible. Recently, new techniques of intrascleral implantation were developed with good outcomes.6 Combined procedures of allograft corneal transplantation, PPV, and scleral IOL fixation have been reported.7 We present a case of autokeratoplasty, PPV for posterior nucleus dislocation, and flanged intrascleral IOL fixation.
CASE REPORT
An 85-year-old diabetic male was admitted to our hospital for corneal opacity. He presented with a history of glaucoma, uneventful cataract surgery in his right eye, and a dislocated nucleus due to a complication during cataract extraction in his left eye. The right eye had no light perception, and the left eye had visual acuity of counting fingers. Slit-lamp biomicroscopy showed pseudoexfoliation, a clear cornea in his right eye, and a bullous keratopathy with an anterior chamber IOL in his left eye. Ultrasonography revealed a dense nucleus dislocated in the vitreous cavity of the left eye. A combined procedure of penetrating keratoplasty (PK), PPV, and flanged intrascleral IOL fixation was indicated. Due to the shortage of corneal tissue in our country, an autokeratoplasty was performed. The procedure was made under general anesthesia. First, the left cornea was trephined, the anterior chamber IOL was removed, and an Eckardt temporary keratoprosthesis was sutured. The opaque cornea was placed in balanced salt solution (BSS). Iris retractors were needed for pupil dilation. 23-gauge PPV was performed, with nucleus levitation and expression through an anterior opening, by releasing one of the sutures of the keratoprosthesis [Figure [Figure1a1a--f].f]. Then, the right eye cornea was trephined and placed in BSS. The left, opaque cornea was rapidly sutured in the right eye with eight interrupted nylon 10.0 sutures, leaving a formed anterior chamber without leakage. In the left eye, two scleral angled incisions were made parallel to the limbus with 27-gauge needles. The Eckardt keratoprosthesis was removed. An open-sky IOL Tecnis ZA9003 (Abbott Medical Optics, Santa Ana, CA) insertion in the posterior chamber was performed, the haptics were externalized through the scleral tunnels, and they were cauterized to make a flange. The right, transparent cornea was placed in the left eye with 16 interrupted nylon 10.0 sutures. Finally, eight additional sutures were placed in the right eye. Postoperatively, both eyes were started on topical prednisolone acetate 1% QID and moxifloxacin 0.5% QID. One week after the surgical procedure, the left eye presented a transparent graft [Figure [Figure2a2a--f].f]. Considering there was no risk of immune rejection, corticosteroids were tapered and discontinued after a month, along with the antibiotics. The right eye eventually developed an infectious ulcer and required a Gundersen flap. During 24 months of follow-up, the left eye graft remained clear, and the patient had a best corrected visual acuity of 20/200.
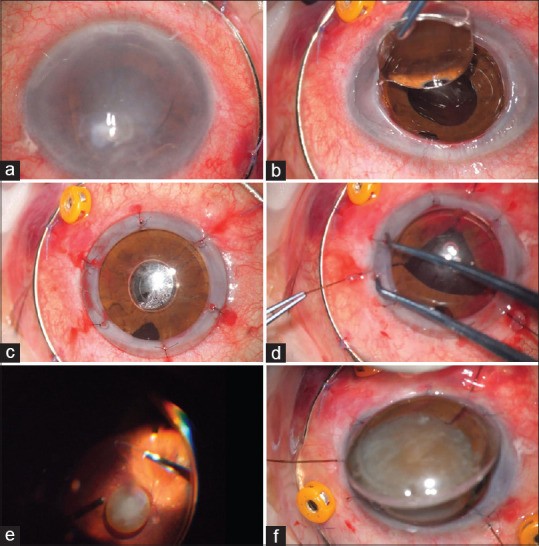
Intraoperative photographs. (a) Left eye. Bullous keratopathy. (b) Anterior chamber intraocular lens explantation after trephination. (c) Eckardt temporary keratoprosthesis. (d) Iris retractors. (e) Dislocated nucleus levitation. (f) Nucleus expression
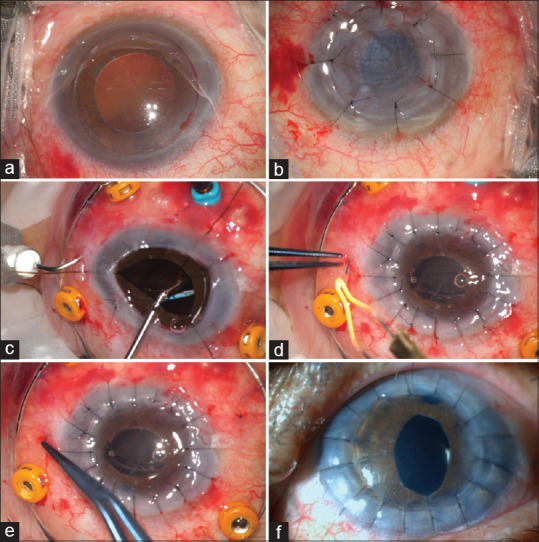
Intraoperative photographs. (a) Right eye. Transparent cornea trephination. (b) Opaque cornea transplantation. (c) Left eye. Angled sclerotomy 2 mm from the limbus with a 27-gauge needle, followed by open-sky intraocular lens haptic threading into the lumen of the needle. (d) After penetrating keratoplasty, cauterization of the externalized haptics to make flanges. (e) Flanges pushed back and fixed into the scleral tunnels. (f) Slit-lamp biomicroscopy. 7-day postoperative showing a clear graft in the left eye
DISCUSSION
Complex cases affecting anterior and posterior segments require the combination of various techniques. Even though there are reports on surgical procedures comprising keratoplasty, vitrectomy, and scleral fixation IOL,7 none of these includes an autokeratoplasty. Autokeratoplasty can be ipsilateral rotational, for a paracentral corneal scar,8 or contralateral, when the patient has an opaque cornea in an otherwise healthy eye, and a transparent cornea in a fellow blind eye.1,3 Sanjuán et al. reported the largest case series of contralateral autokeratoplasty, with 31 eyes. Anatomical success was obtained in 74% and functional success in 58% of the eyes at the end of the follow-up (mean: 11.3 years). They found progression of previous glaucoma to be the most relevant factor for graft failure and low visual acuity in the long-term.2 In our patient, the low visual acuity in the left eye could be explained by a dislocated nucleus and a cloudy cornea. That is the reason why, even though we were not able to thoroughly examine the retina and the optic nerve, we believed the eye had an acceptable visual potential.
For combined anterior and posterior segment procedures, a temporary keratoprosthesis is needed during the vitrectomy to avoid possible endothelial loss of a newly grafted corneal tissue. According to some authors, corneal graft clarity maintenance could range from 49% to 79% of the eyes after using a temporary keratoprosthesis and subsequent keratoplasty.5,9 However, other case series report a corneal graft survival of only 27.3% that would mostly depend on the presence of preoperative active corneal inflammation.4
In complex cases, capsular bag support might be inadequate. To overcome this situation, anterior chamber IOL, iris-fixed IOL, and a transscleral sutured IOL were commonly used. In 2017, Yamane et al. described a novel technique for performing a transconjunctival sutureless intrascleral fixation of IOL. Two angled incisions were made with 30-gauge thin-wall needles, parallel to the limbus. Afterward, haptics of an IOL were externalized through the incisions and cauterized to make a flange, which was then fixed into the scleral tunnel. Proper IOL fixation was achieved with this technique.6 In our case, a 30-gauge thin-wall needle was not available. The technique described by Yamane had to be slightly modified by using a regular 27-gauge needle.
Recently, a new scleral-fixated, sutureless, posterior chamber IOL (Soleko, Carlevale) has been designed and combined with PK in an aphakic patient presenting corneal scarring, with positive results.10
Combined procedures including keratoplasty, PPV, and scleral IOL fixation have been reported. Yokogawa et al. reported 13 cases of combined procedures. Eight cases underwent keratoplasty, PPV, and flanged intrascleral IOL fixation; five of these eyes underwent PK, and three were treated with Descemet-stripping automated endothelial keratoplasty. An Eckardt temporary keratoprosthesis was used in PK cases. Bullous keratopathy was the cause of corneal opacity in all 8 cases. Posterior segment pathology included rhegmatogenous retinal detachment, diabetic retinopathy, and dislocated hypermature cataract. Postsurgical follow-up showed clear grafts, well-fixed IOLs, attached retinas, and improvement in visual acuity.7
We present a case of combined anterior and posterior segment procedures with good results. Only for thoroughly evaluated patients, autokeratoplasty could be a valid option, especially in developing countries where a shortage of corneal tissue could be a problem. In cases of severe anterior segment pathology, where a keratoplasty has to be performed and aphakia presents without a capsular bag to give support to an IOL, flanged intrascleral IOL fixation is a reliable technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
Articles from Journal of Current Ophthalmology are provided here courtesy of Wolters Kluwer -- Medknow Publications
Citations & impact
Impact metrics
Article citations
Concomitant sutureless scleral fixation of intraocular lens with keratoplasty: Review of surgical techniques.
Indian J Ophthalmol, 71(5):1718-1732, 01 May 2023
Cited by: 0 articles | PMID: 37203023 | PMCID: PMC10391482
Review Free full text in Europe PMC
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Combined Keratoplasty, Pars Plana Vitrectomy, and Flanged Intrascleral Intraocular Lens Fixation to Restore Vision in Complex Eyes With Coexisting Anterior and Posterior Segment Problems.
Cornea, 37 Suppl 1:S78-S85, 01 Nov 2018
Cited by: 11 articles | PMID: 30216334
Outcomes of four-point suture fixated and two-point sutureless posterior chamber IOLs combined with pars plana vitrectomy.
BMC Ophthalmol, 22(1):57, 05 Feb 2022
Cited by: 6 articles | PMID: 35123431 | PMCID: PMC8818229
Combined flanged intrascleral intraocular lens fixation with corneal transplant.
Am J Ophthalmol Case Rep, 13:1-5, 10 Nov 2018
Cited by: 6 articles | PMID: 30505976 | PMCID: PMC6247402
[Sutureless scleral intraocular lens fixation: report of nine cases and literature review].
J Fr Ophtalmol, 36(8):658-668, 25 Jul 2013
Cited by: 2 articles | PMID: 23891322
Review



