Abstract
Background
The suboptimal implementation of guideline-directed medical therapy (GDMT) for heart failure (HF) patients has been linked with poor clinical outcomes. Little is known about the potential role of cardiology residency training programs in improving trainees' (ie, future cardiologists') ability to utilize GDMT.Methods
In this survey-based study, we examined the degree of exposure to ambulatory HF patient management among cardiology trainees in Canada. All cardiology residency program directors (n = 15; 100% response rate) completed our survey.Results
Although 9 programs (60%) mandated ≥ 3 ambulatory cardiology rotations, only 3 (20%) required ≥ 2 ambulatory HF rotations. When HF rotations were provided, only 7 programs (47%) offered moderate or higher exposure to ambulatory nontransplant HF patients (defined as ≥ 5 clinics/rotations). This element was independent of program- and institution-specific characteristics. All institutions had a multidisciplinary HF clinic, and the majority (13 [87%]) had access to an inpatient HF service, a consultative HF service, and/or a specialist pharmacist. Furthermore, 13 program directors (87%) agreed on the importance of adopting HF training curriculum and their program's readiness to implement such a module.Conclusions
The current state of HF training among cardiology residencies is suboptimal and in need of improvement. Most programs have access to a HF clinic, a specialist pharmacist, or an inpatient consultative service, which would facilitate adoption of a HF management curriculum that focuses on practical and experiential aspects of GDMT optimization. This program, which is under development, will be offered to training programs nationwide, to enable trainees to manage this growing and increasingly complex patient population.Free full text
Proposal for an Ambulatory Heart Failure Management Curriculum for Cardiology Residency Training Programs
Abstract
Background
The suboptimal implementation of guideline-directed medical therapy (GDMT) for heart failure (HF) patients has been linked with poor clinical outcomes. Little is known about the potential role of cardiology residency training programs in improving trainees’ (ie, future cardiologists’) ability to utilize GDMT.
Methods
In this survey-based study, we examined the degree of exposure to ambulatory HF patient management among cardiology trainees in Canada. All cardiology residency program directors (n = 15; 100% response rate) completed our survey.
Results
Although 9 programs (60%) mandated ≥ 3 ambulatory cardiology rotations, only 3 (20%) required ≥ 2 ambulatory HF rotations. When HF rotations were provided, only 7 programs (47%) offered moderate or higher exposure to ambulatory nontransplant HF patients (defined as ≥ 5 clinics/rotations). This element was independent of program- and institution-specific characteristics. All institutions had a multidisciplinary HF clinic, and the majority (13 [87%]) had access to an inpatient HF service, a consultative HF service, and/or a specialist pharmacist. Furthermore, 13 program directors (87%) agreed on the importance of adopting HF training curriculum and their program’s readiness to implement such a module.
Conclusions
The current state of HF training among cardiology residencies is suboptimal and in need of improvement. Most programs have access to a HF clinic, a specialist pharmacist, or an inpatient consultative service, which would facilitate adoption of a HF management curriculum that focuses on practical and experiential aspects of GDMT optimization. This program, which is under development, will be offered to training programs nationwide, to enable trainees to manage this growing and increasingly complex patient population.
Résumé
Contexte
Une mise en application sous-optimale des traitements médicaux recommandés dans les lignes directrices (TMRLD) dans les cas de patients atteints d’insuffisance cardiaque (IC) a été associée à des issues cliniques défavorables. On en sait peu sur le rôle éventuel des programmes de résidence en cardiologie sur l’amélioration des capacités des stagiaires (c.-à-d. des futurs cardiologues) à mettre en œuvre les TMRLD.
Méthodologie
Notre étude s’appuyant sur un sondage a permis d’examiner le niveau d’exposition des stagiaires en cardiologie au Canada à la prise en charge des patients ambulatoires atteints d’IC. La direction de tous les programmes de résidence en cardiologie (n = 15; taux de réponse de 100 %) a participé à notre sondage.
Résultats
Alors que neuf programmes (60 %) exigeaient ≥ trois stages en cardiologie ambulatoire, seulement trois d’entre eux (20 %) exigeaient ≥ deux stages en IC ambulatoire. Parmi les programmes offrant des stages en IC, seulement sept (47 %) offraient une exposition modérée à élevée à des patients ambulatoires atteints d’IC et n’ayant pas reçu de greffe (cette exposition était établie à cinq cliniques par stage ou plus); le niveau d’exposition à ces patients ne dépendait pas des caractéristiques du programme ou de l’établissement. Dans tous les établissements, une clinique multidisciplinaire spécialisée en IC était présente, et la majorité d’entre eux (13 [87 %]) bénéficiaient également d’un service pour les patients hospitalisés atteints d’IC, d’un service de consultation en IC et/ou de la présence d’un pharmacien spécialisé. De plus, la direction de 13 programmes (87 %) se disait en accord avec l’importance d’adopter un curriculum de formation portant sur l’IC et considérait que leur programme était prêt à intégrer un tel module.
Conclusions
L’état actuel de la formation en IC dans les programmes de résidence en cardiologie n’est pas optimal, et des améliorations sont nécessaires. La plupart des programmes ont accès à une clinique en IC, un pharmacien spécialisé ou un service de consultation pour les patients hospitalisés, ce qui pourrait faciliter l’adoption d’un curriculum de prise en charge de l’IC portant sur l’expérience concrète de l’optimisation des TMRLD. Ce module, qui est en cours d’élaboration, sera offert à tous les programmes de formation à travers le Canada, pour permettre aux stagiaires de mieux prendre en charge cette population de patients qui gagne en nombre et en complexité.
A multitude of randomized controlled trials have established the efficacy of pharmacologic therapy to improve survival and reduce hospitalizations in patients with heart failure (HF). Despite this established evidence, several studies revealed poor implementation of guideline-directed medical therapy (GDMT) by healthcare providers in Canada and around the world.1 Although the roots of this problem are multifaceted, experts agree that tackling therapeutic inertia constitutes a prime target for effecting improvement in GDMT implementation.1 Therapeutic inertia, defined as the failure to initiate or intensify therapy when treatment goals are not met, has been a pervasive challenge in HF care, with little improvement achieved despite several patient- and provider-level interventions.2 An important contributor to therapeutic inertia is providers’ lack of knowledge and self-confidence in implementing HF guidelines. In a Canada-wide survey of clinicians providing HF care, Gupta and colleagues showed that over 40% of cardiologists misestimated the prevalence and prognosis of HF with preserved ejection fraction.3 Whether this knowledge gap is propagated by insufficient coverage of HF management during cardiology residency training has not yet been investigated.4
Regarding the ambulatory components of general cardiology training in North America, a point of note is that the Accreditation Council for Graduate Medical Education (ACGME) in the US allocates less than 20% of cardiology residency training to the ambulatory experience. Moreover, although the new Royal College of Physicians and Surgeons of Canada (Royal College) requirements do not specify a minimum number of ambulatory clinical rotations, the older guidelines from 2015 (which are currently being followed in most programs) require only 3 months of ambulatory experience during the 3-year-long residency training.5,6 Given this low level of training, and the disproportionate emphasis on in-patient service/procedural skills at the expense of ambulatory practice, we hypothesized that cardiology trainees do not receive sufficient ambulatory exposure to optimize HF patient management and GDMT. This sentiment is supported by the lack of uniformly mandated HF rotations within the Royal College requirements for adult cardiology training.6 Even in the emerging competency-based medical education (CBME) curriculum, HF medication optimization is not considered one of the milestones or entrustable professional activities.
In this survey study of Canadian cardiology training program directors, we aimed to examine the degree of cardiology trainees’ exposure to ambulatory HF practice. Gaining insights into the state of HF training will help identify gaps in the current curricula and guide the design of tailored HF-management curriculum to prepare the next generation of cardiologists to meet the needs of this vulnerable patient population.
Methods
Study population and data collection
We contacted all 15 adult cardiology training program directors in Canada from a previously generated list available at the Royal College Web site. The list is publicly available and includes names and e-mail addresses of every program director in Canada. All participants were contacted by principal investigator A.A. The survey was developed with input from several members of the Canadian Heart Failure Society Research Committee (see Supplemental Appendix S1). Data were collected via a Web-based self-administered survey. The survey contained questions in 3 categories, as follows.
Category 1—Training program-related characteristics
This category includes the following elements: program size (measured as the average number of accepted fellows per year); whether advanced heart failure subspecialty training is offered; the number of mandatory ambulatory cardiology rotations; any current practical GDMT optimization curricula offered within the training program (besides teaching at academic half days); availability of HF rotation during training; whether this HF rotation is mandatory; degree of exposure to ambulatory nontransplant HF patients within the HF rotation; degree of participation in the care of advanced HF patients (transplant/mechanical support/pulmonary hypertension patients); and degree of involvement in remote patient monitoring (working with HF nurses/pharmacists to review patients’ remote monitoring data, including patient-reported weight, blood pressure, heart rate, and laboratory tests when available, and making decisions regarding medication regimen adjustments accordingly).
Category 2—Institution-related characteristics
This category includes the following elements: presence of a multidisciplinary heart function clinic; presence of HF in-patient ward service; HF clinical consultative service; access to a HF specialist pharmacist; presence of internal audit/feedback quality improvement programs for GDMT optimization; and access to remote patient monitoring.
Category 3—Amenability to adopting a dedicated HF management curriculum
This section included the following questions: How strongly do you feel about the need for a dedicated GDMT optimization curriculum during cardiology fellowship training? Would your program be amenable to implementing it? How feasible would it be to arrange an ambulatory HF rotation?
To improve the response rate, we engaged collaborating members from the Canadian Heart Failure Society at each academic institution. The survey was piloted on 2 program directors (13% of the anticipated target population) to ensure readability and clarity of the questions. We distributed the survey via e-mail to all the remaining program directors between May 1st, 2021, and July 24th, 2021. The study cohort was characterized using standard descriptive statistics. Fisher’s exact test was used to compare categorical variables. A 2-tailed P < 0.05 was deemed statistically significant. This project was approved by the University of British Columbia Research Ethics Committee.
Results
General demographics and program-related characteristics
A total of 15 adult cardiology program directors representing all teaching institutions in Canada completed the survey (response rate 100%).
Ambulatory cardiology and heart failure rotation requirements
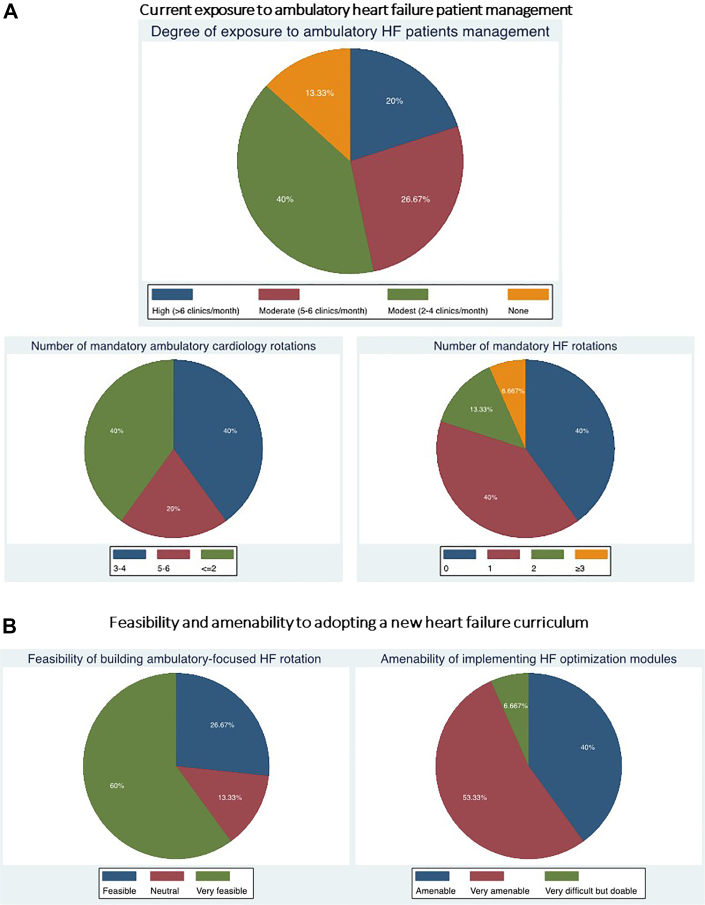
Six programs (40%) required a minimum of 1-2 dedicated ambulatory cardiology rotations (each lasting 4 weeks) during the 3-year residency; another 6 (40%) required 3-4 rotations, and the remaining 3 (20%) required > 4 rotations.(Fig. 1A). Notably, neither the Royal College nor the Accreditation Council for Graduate Medical Education (ACGME) specifies what case mix or subspecialty discipline exposure should be achieved during these ambulatory blocks. Consequently, the structure of ambulatory blocks across cardiology programs is highly variable, with most not mandating any specific involvement at an HF clinic. As for HF rotations, 6 programs (40%) had no mandatory HF rotations, 6 (40%) mandated only one HF rotation, and the remaining 3 (20%) mandated 2 or more rotations. (Fig. 1A). Only one program director planned to increase required ambulatory rotations to accommodate for CBME curriculum implementation.
Degree of exposure to ambulatory nontransplant HF patient management
With regard to ambulatory care during HF rotations, 7 program directors (47%) estimated moderate or high exposure to ambulatory nontransplant HF patients (defined as ≥ 5 clinics/rotations where trainees are involved in GDMT initiation and titration). The remaining 8 program directors (53%) reported modest or no exposure ( ≤ 1 clinic/wk) to nontransplant HF patients (Fig. 1A). None of the program- or institution-related characteristics significantly influenced the degree of exposure to ambulatory HF patient management (P > 0.05 for all). Finally, only 7 programs (47%) had current HF medication optimization modules in place, and the remaining 8 (53%) had no such programs.
Institution-related characteristics
Program directors were asked about available resources/expertise at their institutions that could facilitate ambulatory HF management training. All institutions had a multidisciplinary HF clinic with 10 (67%) having a consultative HF service and 9 (60%) having an inpatient HF admitting service. Furthermore, 9 institutions (60%) had access to a HF specialist pharmacist, and 12 (80%) had remote patient monitoring services. Put together, the majority (13 [87%]) of programs had access to at least one of the following: HF inpatient admitting service; HF consultative service; and HF specialist pharmacists.
Amenability to implementing HF training curriculum
When asked whether a HF medication optimization module should be established to enhance trainees’ readiness to use evidence-based HF medications, the majority (13 [87%]) agreed with this statement. (Fig. 1B). Importantly, 14 directors (93%) believed the structure of their programs to be amenable or very amenable to the adoption of such a module. Similarly, 13 program directors (87%) believed it was feasible or very feasible to establish an ambulatory HF management-focused clinical rotation (Fig. 1B).
Discussion
This is the first study to elucidate HF training practices among cardiology residency programs in Canada to better map the current landscape and identify opportunities for tailored HF management curriculum implementation. The 3 salient findings in our study are as follows: (i) Most Canadian cardiology programs mandate only 1 HF rotation, or none at all, and have no current plans to augment this mandate in the future. (ii) When HF rotations were offered, exposure to ambulatory HF patient management was mostly modest, leaving ample room for improvement. (iii) The majority of Canadian institutions have access to a HF clinic, a specialist pharmacist, or an inpatient HF consultative service. all of which would be helpful in establishing a dedicated HF rotation and HF management training modules.
The lingering poor clinical outcomes among HF patients in spite of remarkable developments in HF pharmacotherapy have been linked to pervasive therapeutic inertia among healthcare providers.1 This inertia, which is linked to providers’ lack of knowledge and self-confidence in HF management, was documented at as early a level as junior cardiology resident, as found by Richardson and colleagues.7 They reported a median 50% score in guideline knowledge and implementation among their cardiology trainees.7 These findings are not surprising in the context of our results, which reveal that 80% of training programs mandated none or only one HF rotation during training, and when HF rotations were offered, less than half the training programs offered moderate/high exposure ( ≥ 5 clinics/rotations) to ambulatory HF patient management.
As individual-level interventions achieved limited success in improving GDMT optimization among cardiologists, our study uncovers an upstream opportunity to enhance cardiologists’ knowledge and HF management skills at the level of a cardiology training program, which may have an even larger and more lasting impact, particularly if implemented as a nationwide curriculum.2
Using the information gleaned from this study, the Canadian Heart Failure Society Research Committee, with trainee representatives, will structure a HF management curriculum aimed at improving ambulatory HF management skills among cardiology trainees. This curriculum will be developed in collaboration with representatives from among Canadian cardiology training program directors and trainees, to ensure that their input is incorporated and that the proposed curriculum addresses areas of deficiency while minimizing redundancy and unnecessary consumption of time and resources. In this way, the program will capitalize on available infrastructure to minimize the cost and resource burden, particularly in the early stages of implementation. Below, we outline the components of this proposed curriculum, which include didactic teaching during a 3-hour academic half-day slot, and several sessions of experiential learning/practice facilitated by peer and supervisor review of sample trainees’ clinic documentations (Fig. 2).
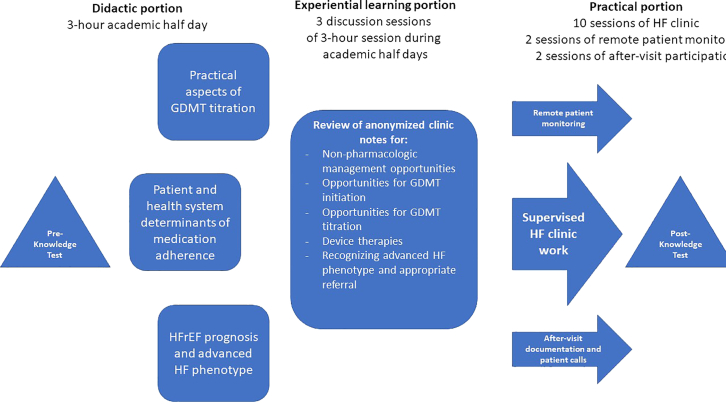
Overview of proposed heart failure (HF) training curriculum. GDMT, guideline-directed medical therapy; HFrEF, heart failure with reduced ejection fraction.
As opposed to traditional curricula that have disproportionate emphasis on theoretical concepts of the pathophysiology and molecular mechanisms of heart failure with reduced ejection fraction, the didactic portion of this module will center on practical aspects of GDMT titration, barriers to reaching target doses, determinants of medication adherence, and understanding of the trajectory of HF patients in the absence of expedient GDMT optimization. The experiential learning portion will include sessions in which learners apply their knowledge and experience of GDMT optimization practices while reviewing anonymized peer clinic notes (Fig. 2). The third element is a practical portion for trainees to apply their learned knowledge in a clinical context. This element includes supervised engagement in multidisciplinary HF clinics, reviewing patients’ medications, identifying opportunities for GDMT optimization, and establishing an effective management plan. When feasible, trainees should also be involved in longitudinal patient follow-up, remote monitoring, and addressing patients’ calls to report symptoms or ask medication-related questions. Important to note is that a standardized HF knowledge test will be administered to participating trainees before and after implementation of the curriculum, to gauge their performance and define areas of improvement (Fig. 2). Finally, the development of this curriculum will be an iterative process with engagement of trainees, training program directors, cardiology scientific bodies, and when possible, the Royal College.
The current technical skill-focused cardiology curriculum may prove less accommodating for a disease-centered learning module like our proposed HF management curriculum. Nonetheless, we are encouraged by the overwhelming buy-in from program directors in this survey and by the available infrastructure in most institutions. Furthermore, experience from the cardiology training program at Vanderbilt University showed that developing an ambulatory cardiology training curriculum (which included HF management) was feasible and resulted in substantial improvement in adherence to guideline-recommended practices.7
We acknowledge several limitations. First, although we acquired valuable information on HF training from surveying program directors, the lack of inclusion of trainees’ perspectives may mean that other opportunities pursued independently by the trainees were overlooked in the survey. Second, although most program directors planned no changes to HF training with CBME curriculum adoption, the CBME rollout is in its early stages, and therefore, unforeseen changes may take place. Third, we did not collect detailed information regarding ambulatory rotations and how much HF care is embedded in them. A possibility is that some HF training is effectively occurring organically within the current curriculum (eg, in ambulatory cardiology rotations, inpatient ward service, and cardiology consultative rotations). Finally, therapeutic inertia is a complex construct that includes, but is not limited to, lack of cardiology providers’ knowledge and confidence in the use of GDMT. Other equally important factors that were not captured in this study include the need for customized training of allied health providers, patient empowerment and education, and restructuring of payer reimbursement processes to incentivize adherence to guideline recommendations.
In sum, the majority of cardiology training programs mandate none or only one ambulatory HF rotation, with insufficient emphasis on nontransplant HF patient management. The rapid expansion of approved HF pharmacotherapy calls for increased exposure of cardiology trainees to ambulatory HF management, which can be accomplished by establishing a tailored curriculum combining didactic, experiential, and practical learning components. Finally, considering that the care of HF patients is often shared among family physicians, internists, cardiology specialists, and nonphysician clinicians, subsequent projects should aim to tailor dedicated HF training modules for internal and family medicine residency programs and allied health professionals.
Acknowledgements
We are grateful to all the program directors who participated in this survey and shared their insight with the research team. The Canadian Heart Failure Society and its research committee members were generous to support this initiative.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: This project was approved by the University of British Columbia Research Ethics Committee.
See page 871 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2022.07.005.
References
Articles from CJC Open are provided here courtesy of Elsevier
Full text links
Read article at publisher's site: https://doi.org/10.1016/j.cjco.2022.07.005
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9568682
Citations & impact
Impact metrics
Article citations
Role of Telemedicine Intervention in the Treatment of Patients with Chronic Heart Failure: A Systematic Review and Meta-analysis.
Anatol J Cardiol, 01 Mar 2024
Cited by: 0 articles | PMID: 38430113 | PMCID: PMC11017678
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Guideline-directed medical therapy in heart failure patients: impact of focused care provided by a heart failure clinic in comparison to general cardiology out-patient department.
Egypt Heart J, 72(1):53, 24 Aug 2020
Cited by: 4 articles | PMID: 32833163 | PMCID: PMC7445219
The Pediatric Heart Failure Workforce: An International, Multicenter Survey.
Pediatr Cardiol, 39(2):307-314, 17 Nov 2017
Cited by: 3 articles | PMID: 29147800
Community-based care for the specialized management of heart failure: an evidence-based analysis.
Ont Health Technol Assess Ser, 9(17):1-42, 01 Nov 2009
Cited by: 6 articles | PMID: 23074521 | PMCID: PMC3377506
The evolving challenge of chronic heart failure management: a call for a new curriculum for training heart failure specialists.
J Am Coll Cardiol, 44(7):1354-1357, 01 Oct 2004
Cited by: 17 articles | PMID: 15464311
Review