Abstract
Free full text
A Comparative Analysis of Health-Related Quality of Life 1 Year Following Myomectomy or Uterine Artery Embolization: Findings from the COMPARE-UF Registry
Associated Data
Abstract
Objective:
To compare 12-month post-treatment health-related quality of life (HR-QoL) and symptom severity (SS) changes among patients with symptomatic uterine fibroids (SUF) not seeking fertility and undergo a hysterectomy, abdominal myomectomy (AM), or uterine artery embolization (UAE).
Materials and Methods:
The Comparing Options for Management: Patient-Centered Results for Uterine Fibroids (COMPARE-UF) Registry is a multi-institutional prospective observational cohort study of patients treated for SUF. A subset of 1465 women 31–45 years of age, who underwent either hysterectomy (n =
= 741), AM (n
741), AM (n =
= 446), or UAE (n
446), or UAE (n =
= 155) were included in this analysis. Demographics, fibroid history, and symptoms were obtained by baseline questionnaires and at 1 year post-treatment. Results were stratified by all treatments and propensity score weighting to adjust for differences in baseline characteristics.
155) were included in this analysis. Demographics, fibroid history, and symptoms were obtained by baseline questionnaires and at 1 year post-treatment. Results were stratified by all treatments and propensity score weighting to adjust for differences in baseline characteristics.
Results:
Women undergoing UAE reported the lowest baseline HR-QoL and highest SS scores (mean =
= 40.6 [standard deviation (SD)
40.6 [standard deviation (SD) =
= 23.8]; 62.3 [SD
23.8]; 62.3 [SD =
= 24.2]) followed by hysterectomy (44.3 [24.3]; 59.8 [SD
24.2]) followed by hysterectomy (44.3 [24.3]; 59.8 [SD =
= 24.1]). At 12 months, women who underwent a hysterectomy experienced the largest change in both HR-QoL (48.7 [26.2]) and SS (51.9 [25.6]) followed by other uterine-sparing treatments. Propensity score weighting revealed all treatments produced substantial improvement, with hysterectomy patients reporting the highest HR-QoL score (92.0 [17.8]) compared with myomectomy (86.7 [17.2]) and UAE (82.6 [21.5]) (p
24.1]). At 12 months, women who underwent a hysterectomy experienced the largest change in both HR-QoL (48.7 [26.2]) and SS (51.9 [25.6]) followed by other uterine-sparing treatments. Propensity score weighting revealed all treatments produced substantial improvement, with hysterectomy patients reporting the highest HR-QoL score (92.0 [17.8]) compared with myomectomy (86.7 [17.2]) and UAE (82.6 [21.5]) (p <
< 0.0001). Similarly, hysterectomy patients reported the lowest SS scores (8.2 [15.1]) compared with myomectomy (16.5 [15.1]) and UAE (19.6 [17.5]) (p
0.0001). Similarly, hysterectomy patients reported the lowest SS scores (8.2 [15.1]) compared with myomectomy (16.5 [15.1]) and UAE (19.6 [17.5]) (p <
< 0.0001).
0.0001).
Conclusion:
All procedures showed improvement in HR-QoL and reduction in SS score at 12 months, hysterectomy showing maximum improvement. Of importance, at 12 months, patients who underwent either a myomectomy or UAE reported comparable symptom relief and HR-QoL.
Clinicaltrials.Gov Identifier: NCT02260752.
Introduction
Uterine leiomyomas affect nearly 70% of self-reported white women and more than 80% of self-reported black/African American women by the age of 50.1 Women with fibroids experience a range of symptoms, including excessive uterine bleeding that can lead to anemia, urinary problems, pelvic pressure and pain, sexual dysfunction, and infertility, all of which can influence quality of life.2–6 While some women can be treated medically, many patients with symptomatic fibroids require procedures that include myomectomy, hysterectomy, and uterine artery embolization (UAE). Each procedure has been shown to have its own risks, benefits, and applicability for different patients with a range of clinical outcomes.7–10 Despite the development of newer procedures such as UAE, hysterectomy and myomectomy still comprise about 90%–95% of all uterine fibroid procedures in the United States of America.11,12
The efficacy and outcome of each treatment modality is impacted, in part, by each woman's symptoms, patient-specific factors (i.e., age, body mass index, and size, location, and number of fibroids), and patient treatment goals and expectations, which have rarely been examined. Prior studies have compared outcomes between surgical procedures (myomectomy vs. hysterectomy)13 or compared surgical versus nonsurgical approaches (<1 year),14–16 while others have evaluated long-term outcomes (>1 year), across the most common procedures for fibroid-associated symptoms.17–20
The Comparing Options for Management: Patient-Centered Results for Uterine Fibroids (COMPARE-UF) registry is a prospective cohort study of women who planned treatment for uterine fibroids (UF). COMPARE-UF was designed to provide women and clinicians with insights on the short- (6–12 weeks postprocedure) and long-term (≥1 year post procedure) outcomes of fibroid treatments. Recently, we reported on the short-term21 and long-term17 quality of life of after surgical interventions for UF (myomectomy vs. hysterectomy), showing better health-related quality of life (HR-QoL) at 1 year for those treated with hysterectomy; however, outcomes for women undergoing nonsurgical procedures have not been reported from this cohort. To address this evidence gap, we compared 1-year HR-QoL and symptom severity (SS) scores using the validated Uterine Fibroids Symptom and Quality of Life (UFS-QoL) questionnaire completed by women enrolled in COMPARE-UF registry, who had a hysterectomy, abdominal myomectomy (AM), or UAE, through any approach.
Materials and Methods
Study population
COMPARE-UF (NCT02260752, clinical trials.gov) is a registry of women with symptomatic uterine fibroids (SUF), designed to inform women and clinicians about treatment outcomes in response to priorities identified by patient stakeholders. Details of the study design have been described previously.22 Between November 11, 2015, and April 18, 2019, 2857 premenopausal (defined as having a menstrual period in the last 3 months) women with symptomatic fibroids were enrolled. These participants were between 18 and 54 years of age; had at least one uterine fibroid documented by ultrasound, magnetic resonance imaging, or pathology report; and were presenting for an elective fibroid treatment procedure at one of nine clinical sites.22 There was no requirement related to whether or not the woman had a prior UF treatment. All participants completed a questionnaire before their treatment and the information collected included 2857 participants (Fig. 1 and Supplementary Table S1).
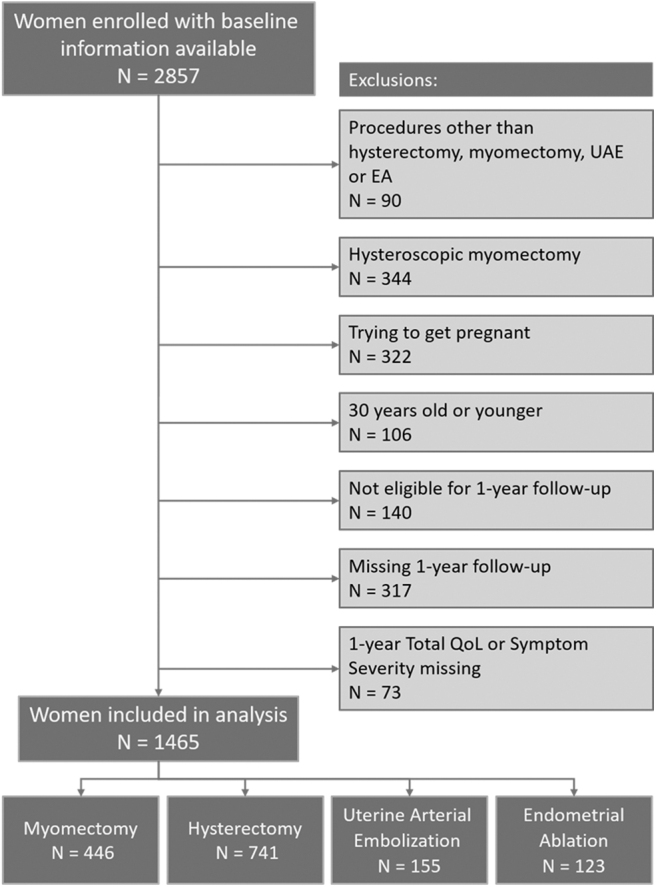
CONSORT diagram, including exclusion criteria for analytic data on comparative outcomes at 1-year follow-up for different procedure types.
Participants younger than 30 years were not analyzed due to the low number of definitive surgical procedures such as hysterectomy. These analyses included women 31 years of age or older, undergoing a hysterectomy, AM, UAE, or endometrial ablation. We excluded participants who had a hysteroscopic myomectomy, those attempting to conceive (self-reported intent), and those who had not yet been followed for at least one year postprocedure, and patients with missing UFS-QoL information or those lost to follow-up. Endometrial ablation was also excluded from the comparative analysis due to the lack of overlapping in the baseline characteristics with the other three treatments, particularly uterine volumes. See Figure 1 for CONSORT Flow Diagram. Institutional Review Boards at Duke University (the data coordinating center) and each individual study site reviewed and approved the study. Informed consent was obtained from each participant.
Exposure and covariate assessment
Participants' data were collected by phone interviews and self-administered questionnaires. All operative and procedural notes were provided to the central data abstraction center at Henry Ford Health System. Sociodemographic, reproductive (contraceptive use, menstrual characteristics, and parity), and clinical (age at fibroid diagnosis, fibroid/uterine volume, number of fibroids, prior treatment, history of anemia, and other medical conditions) data were collected from baseline questionnaires that were administered before the fibroid procedure.22
Outcome assessment
As described previously, symptoms and health-related quality-of-life data were collected utilizing the UFS-QoL questionnaire to assess short-term outcomes (6 months after the procedure) and long-term outcomes assessed annually (at 1, 2, and 3 years after the procedure date) online through a password-protected study portal, on paper, or by phone interview.17 The UFS-QoL is a validated fibroid-specific symptom and quality-of-life questionnaire consisting of 37 questions, 8 symptom questions and 29 quality of life questions, on a 5-point Likert scale across 6 domains, including concern, activities, energy/mood, control, self-consciousness, and sexual function.23 UFS-QoL yields two scores: a symptom score and an HR-QoL score, each based on responses that are summed and transformed to a 100-point scale, with lower SS scores correlating with fewer symptoms and higher HR-QoL scores indicating better quality of life and functioning.
Statistical analysis
Baseline characteristics, including demographics, medical history, and fibroid-specific history, were summarized by treatment with continuous variables presented as means and standard deviations (SD) or medians and quartiles and categorical variables as frequencies and percentages. Overall, HR-QoL and its components, as well as SS in the four treatment groups at baseline and change from baseline to 1 year were summarized with means and SD.
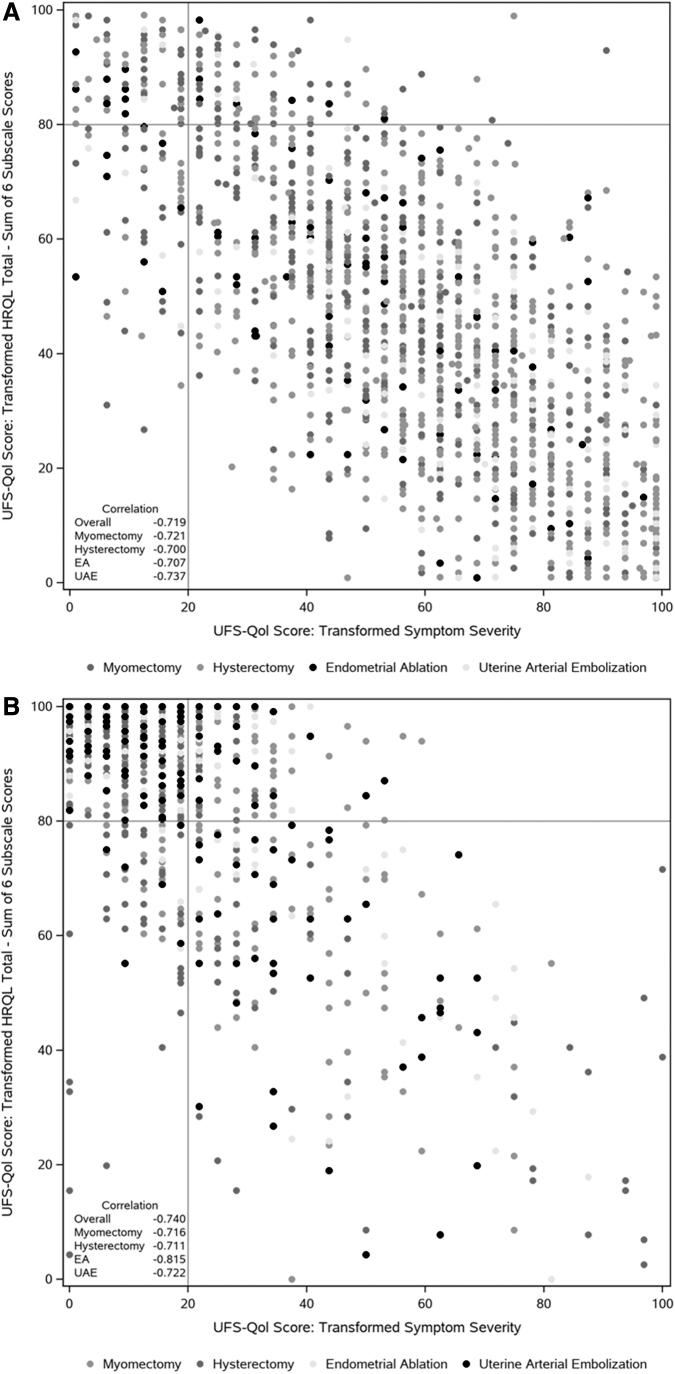
For descriptive purposes, scatter plots comparing symptom severity scores and overall UFS-QoL at baseline and 1 year by treatment are presented. Quadrants are defined using a cutpoint of 20 for SS and 80 for overall UFS-QoL. By way of reference, prior research has determined that the mean symptom score for a normal premenopausal woman without fibroids was 15.3 and the HR-QoL score was a mean of 92.8.24
Propensity score weighting was used to account for differences in baseline characteristics among the women who received each procedure.25,26 To calculate propensity scores, a multinomial logistic regression model was derived with procedure type as the outcome and baseline participant characteristics or symptoms as the independent variables, as described previously.17 Two different analyses are presented for each outcome: one considering the change in outcome (HR-QoL or SS score) as a continuous variable and a second analysis based on categories for the change in outcome. These categories were based on clinically meaningful changes (≥10-unit change), as an estimate of the degree of change.24,27 Weighted linear regression models and cross-tabulations were used to compare treatments.
The weights were derived from the propensity score model described above. Endometrial ablation was excluded from the comparative analysis due to the lack of overlapping in baseline characteristics with the other three treatments, particularly uterine volumes. Missingness for the variables included in the propensity score model was low and missing values were imputed using single imputation. All statistical analyses were performed with SAS System v9.4 (TS1M6) and with the PSweight package in R at Duke Clinical Research Institute.
Results
In total, 1465 patients were included for analysis. The most common fibroid treatment was hysterectomy (n =
= 741), followed by myomectomy (n
741), followed by myomectomy (n =
= 446), UAE (n
446), UAE (n =
= 155), and endometrial ablation (EA) (n
155), and endometrial ablation (EA) (n =
= 123; not included in our analysis). Baseline characteristics are displayed in Table 1. Notably, women undergoing myomectomy were younger (mean
123; not included in our analysis). Baseline characteristics are displayed in Table 1. Notably, women undergoing myomectomy were younger (mean =
= 38.5 years old [SD
38.5 years old [SD =
= 5.3 years]) than those undergoing hysterectomy (44.9 [4.8]), EA (44.6 [4.6]), and UAE (46.5 [5.0]). In addition, while black women comprised 40.7% of the total study population (596/1465), black women were found to be overrepresented in the group undergoing UAE (71%) compared with other treatment modalities. The majority of women (54%) undergoing myomectomy reported no previous pregnancy before treatment. Comorbid conditions, such as depression and anxiety, were commonly reported among women undergoing endometrial ablation, whereas alcohol and marijuana use were similarly distributed across all treatment modalities.
5.3 years]) than those undergoing hysterectomy (44.9 [4.8]), EA (44.6 [4.6]), and UAE (46.5 [5.0]). In addition, while black women comprised 40.7% of the total study population (596/1465), black women were found to be overrepresented in the group undergoing UAE (71%) compared with other treatment modalities. The majority of women (54%) undergoing myomectomy reported no previous pregnancy before treatment. Comorbid conditions, such as depression and anxiety, were commonly reported among women undergoing endometrial ablation, whereas alcohol and marijuana use were similarly distributed across all treatment modalities.
Table 1.
Baseline Characteristics of Participants by Elective Procedure Type
Myomectomy, N = = 446 (30.4%) 446 (30.4%) | Hysterectomy, N = = 741 (50.6%) 741 (50.6%) | Endometrial ablation, N = = 123 (8.4%) 123 (8.4%) | Uterine artery embolization, N = = 155 (10.6%) 155 (10.6%) | |
|---|---|---|---|---|
| Age (years), mean (SD) | 38.5 (5.3) | 44.9 (4.8) | 44.6 (4.6) | 44.6 (5.0) |
| Age group, years, n (%) | ||||
 31–39 31–39 | 265 (59.4) | 96 (13.0) | 19 (15.4) | 25 (16.1) |
 40–44 40–44 | 120 (26.9) | 235 (31.7) | 38 (30.9) | 39 (25.2) |
 45+ 45+ | 61 (13.7) | 410 (55.3) | 66 (53.7) | 91 (58.7) |
| Race, n (%) | ||||
 White White | 173 (38.8) | 393 (53.0) | 67 (54.5) | 34 (21.9) |
 Black Black | 184 (41.3) | 256 (34.5) | 47 (38.2) | 109 (70.3) |
 Other Other | 89 (20.0) | 92 (12.4) | 9 (7.3) | 12 (7.7) |
 Hispanic, n (%) Hispanic, n (%) | 28 (6.3) | 50 (6.7) | 9 (7.3) | 6 (3.9) |
| Insurance, n (%) | ||||
 Private Private | 380 (85.2) | 614 (82.9) | 107 (87.0) | 128 (82.6) |
 Active military Active military | 5 (1.1) | 3 (0.4) | 0 (0.0) | 1 (0.6) |
 Other Other | 61 (13.7) | 124 (16.7) | 16 (13.0) | 26 (16.8) |
 BMI (kg/m2), mean (SD) BMI (kg/m2), mean (SD) | 27.9 (7.0) | 31.1 (8.0) | 32.4 (7.9) | 32.4 (9.1) |
 Ever pregnant, n (%) Ever pregnant, n (%) | 205 (46.0) | 579 (78.1) | 113 (91.9) | 117 (75.5) |
 2 or more pregnancies 2 or more pregnancies | 105 (23.5) | 471 (63.6) | 100 (81.3) | 95 (61.3) |
 Other medical condition, n (%) Other medical condition, n (%) | 164 (36.8) | 396 (53.4) | 79 (64.2) | 93 (60.0) |
 Depression Depression | 105 (23.5) | 203 (27.4) | 46 (37.4) | 43 (27.7) |
 Anxiety Anxiety | 119 (26.7) | 188 (25.4) | 43 (35.0) | 39 (25.2) |
 Endometriosis Endometriosis | 34 (7.6) | 78 (10.5) | 17 (13.8) | 12 (7.7) |
 Adenomyosis Adenomyosis | 5 (1.1) | 32 (4.3) | 1 (0.8) | 8 (5.2) |
| Lifestyle factors | ||||
 Tobacco Tobacco | 19 (4.3) | 57 (7.7) | 13 (10.6) | 10 (6.5) |
 Alcohola Alcohola | 402 (90.1) | 624 (84.2) | 101 (82.1) | 134 (86.5) |
 Marijuanaa Marijuanaa | 37 (8.3) | 44 (5.9) | 6 (4.9) | 5 (3.2) |
BMI, body mass index; SD, standard deviation.
Fibroid-specific history is displayed in Table 2. When evaluating fibroid-specific symptom and treatment history, several relationships were identified. Women undergoing hysterectomy reported longer symptom duration (7.3 years, mean SD [8.0]) and more intermenstrual bleeding (52.1%) than women undergoing other procedures. In addition, nearly one in five women undergoing hysterectomy had undergone previous treatment for UF, the most common of which was AM (6.6%) followed by endometrial ablation (4.3%). Women undergoing UAE reported similar duration of symptoms (7.5 years mean SD [7.9]) as those who had a planned hysterectomy. However, women undergoing UAE more commonly reported a history of anemia (72.3%) with one in seven requiring a blood transfusion.
Table 2.
Fibroid-Specific History
Myomectomy, N = = 446 (30.4%) 446 (30.4%) | Hysterectomy, N = = 741 (50.6%) 741 (50.6%) | Endometrial ablation, N = = 123 (8.4%) 123 (8.4%) | Uterine artery embolization, N = = 155, (10.6%) 155, (10.6%) | |
|---|---|---|---|---|
| Age first told have fibroids (years), mean (SD) | 33.9 (6.5) | 38.6 (8.2) | 40.4 (6.7) | 37.8 (8.0) |
| Age first have fibroid symptoms (years), mean (SD) | 33.4 (7.4) | 37.6 (8.9) | 38.2 (8.6) | 37.1 (9.0) |
| Duration of symptoms (years), mean (SD) | 5.1 (6.0) | 7.3 (8.0) | 6.4 (7.8) | 7.5 (7.9) |
| Family history of fibroids, n (%) | 258 (57.8) | 376 (50.7) | 59 (48.0) | 82 (52.9) |
| Current contraception, n (%) | 278 (62.3) | 502 (67.7) | 97 (78.9) | 96 (61.9) |
| Regular, predictable menses, n (%) | 338 (75.8) | 419 (56.5) | 66 (53.7) | 89 (57.4) |
| History of anemia, n (%) | 201 (45.1) | 412 (55.6) | 60 (48.8) | 112 (72.3) |
| Requiring transfusion, n (%) | 37 (8.3) | 77 (10.4) | 13 (10.6) | 24 (15.5) |
| Total fibroid volume (cm3), median (Q1, Q3)a | 293 (120–552) | 132 (33–310) | 5 (1–18) | 154 (74–339) |
| Uterine volume (cm3), median (Q1, Q3)a | 586 (300–1024) | 415 (218–786) | 174 (118–256) | 538 (293–949) |
| Number of fibroids measured, median (Q1, Q3)a | 2 (1–4) | 2 (1–3) | 1 (1–1) | 2 (1–3) |
| Any fibroid symptoms, n (%) | 419 (93.9) | 701 (94.6) | 119 (96.7) | 150 (96.8) |
| Bleeding symptoms | 342 (76.7) | 629 (84.9) | 118 (95.9) | 135 (87.1) |
| Menses ≥7 days | 204 (45.7) | 448 (60.5) | 92 (74.8) | 95 (61.3) |
| Heavy menses | 314 (70.4) | 580 (78.3) | 113 (91.9) | 122 (78.7) |
| Bleeding between periods | 182 (40.8) | 386 (52.1) | 59 (48.0) | 76 (49.0) |
| Frequent urination | 278 (62.3) | 428 (57.8) | 63 (51.2) | 111 (71.6) |
| Nocturia | 250 (56.1) | 440 (59.4) | 68 (55.3) | 105 (67.7) |
| Abdominal bloating | 322 (72.2) | 535 (72.2) | 96 (78.0) | 129 (83.2) |
| Abdominal/pelvic pressure | 326 (73.1) | 545 (73.5) | 83 (67.5) | 122 (78.7) |
| Appear pregnant | 198 (44.4) | 314 (42.4) | 43 (35.0) | 66 (42.6) |
| Discomfort during intercourse | 186 (41.7) | 325 (43.9) | 53 (43.1) | 65 (41.9) |
| Pelvic pain requiring meds | 161 (36.1) | 358 (48.3) | 57 (46.3) | 73 (47.1) |
| Subfertility | 62 (13.9) | 84 (11.3) | 19 (15.4) | 17 (11.0) |
| Multiple miscarriages | 15 (3.4) | 37 (5.0) | 13 (10.6) | 10 (6.5) |
| Nonmenstrual pain | 40 (9.0) | 104 (14.0) | 30 (24.4) | 19 (12.3) |
| Any prior treatment, n (%) | 68 (15.2) | 155 (20.9) | 10 (8.1) | 24 (15.5) |
| Abdominal myomectomy | 28 (6.3) | 49 (6.6) | 2 (1.6) | 7 (4.5) |
| Hysteroscopic myomectomy | 18 (4.0) | 25 (3.4) | 2 (1.6) | 5 (3.2) |
| Laparoscopic/robotic myomectomy | 14 (3.1) | 31 (4.2) | 2 (1.6) | 4 (2.6) |
| Vaginal myomectomy | 9 (2.0) | 17 (2.3) | 1 (0.8) | 3 (1.9) |
| Focused ultrasound | 2 (0.4) | 6 (0.8) | 0 (0.0) | 0 (0.0) |
| Endometrial ablation | 5 (1.1) | 32 (4.3) | 1 (0.8) | 6 (3.9) |
| Radiofrequency ablation | 0 (0.0) | 1 (0.1) | 0 (0.0) | 0 (0.0) |
| Uterine artery embolization | 3 (0.7) | 23 (3.1) | 1 (0.8) | 1 (0.6) |
Baseline and 1 year post-treatment change (1-year HR-QoL minus baseline HR-QoL) in HR-QoL and SS scores from the UFS-QoL questionnaire are displayed in Table 3 and Supplementary Figure S1. Women undergoing UAE reported the lowest baseline HR-QoL score (40.6 [23.8]) followed by women who planned to undergo hysterectomy (44.3 [24.3]). A similar relationship was seen with baseline SS scores, with worse symptom scores for UAE patients, and uniformly, women undergoing UAE reported the lowest baseline scores across all UFS-QoL domains. At 1 year post-treatment, women undergoing hysterectomy experienced the largest improved change in HR-QoL (48.7 [26.2]) and decrease in SS scores (51.9 [25.6]) followed by the other fertility-sparing treatment options.
Table 3.
Baseline and 1 Year Post-Treatment Change in Health-Related Quality of Life and Symptom Severity
Myomectomy, N = = 446 (30.4%) 446 (30.4%) | Hysterectomy, N = = 741 (50.6%) 741 (50.6%) | Endometrial ablation, N = = 123 (8.4%) 123 (8.4%) | Uterine artery embolization, N = = 155 (10.6%) 155 (10.6%) | |
|---|---|---|---|---|
| Quality of life at baseline mean (SD) | ||||
 HR-QoL score HR-QoL score | 51.0 (25.4) | 44.3 (24.3) | 52.1 (23.2) | 40.6 (23.8) |
 Symptom severity Symptom severity | 50.3 (24.6) | 59.8 (24.1) | 47.4 (24.1) | 62.3 (24.4) |
| UFS-QOL domains | ||||
 Concern Concern | 49.7 (33.4) | 38.3 (29.6) | 39.5 (27.8) | 35.0 (30.7) |
 Activity Activity | 53.3 (28.8) | 45.5 (27.8) | 54.8 (27.3) | 43.3 (26.9) |
 Energy Energy | 52.0 (27.8) | 45.6 (26.6) | 49.4 (24.4) | 41.0 (24.8) |
 Control Control | 50.8 (27.3) | 48.4 (26.9) | 60.3 (25.5) | 45.1 (27.4) |
 Self-conscious Self-conscious | 45.5 (31.5) | 42.2 (31.0) | 55.4 (31.4) | 35.2 (27.6) |
 Sexual function Sexual function | 53.3 (34.0) | 44.8 (32.3) | 54.0 (33.8) | 42.8 (34.0) |
| Change in quality of life from baseline to 1 year mean (SD) | ||||
 Change in HR-QoL score improvement (+) ↑ Change in HR-QoL score improvement (+) ↑ | +36.6 (26.9) | +48.7 (26.2) | +32.6 (25.9) | +41.7 (27.4) |
 Change in symptom severity improvement (–) ↓ Change in symptom severity improvement (–) ↓ | –33.5 (25.6) | –51.9 (25.6) | –26.0 (30.1) | –42.2 (26.7) |
| Changes in UFS-QOL domains | ||||
 Concern Concern | –37.0 (35.4) | –58.0 (31.9) | –45.4 (35.8) | –46.9 (34.4) |
 Activity Activity | +37.2 (30.0) | +48.5 (30.1) | +32.2 (31.7) | +41.6 (31.3) |
 Energy Energy | +35.1 (29.1) | +46.3 (28.8) | +32.7 (27.8) | +41.0 (28.8) |
 Control Control | +37.9 (29.0) | +45.3 (28.7) | +27.9 (26.2) | +40.5 (29.9) |
 Self-conscious Self-conscious | –36.7 (33.9) | –48.1 (32.4) | –24.8 (32.1) | –40.8 (32.5) |
 Sexual function Sexual function | +33.7 (36.1) | +43.6 (36.0) | +28.0 (35.0) | +34.0 (37.5) |
Data are mean ±
± SD or % (n) unless otherwise specified.
SD or % (n) unless otherwise specified.
HRQOL, health-related quality of life; UFS-QOL, uterine fibroid symptom quality of life.
Following propensity score weighting, total and changes in HR-QoL scores 1 year post-treatment were evaluated and are displayed in Table 4. Patients who underwent hysterectomy reported the highest HR-QoL score (92.0 [17.8]) at 1-year follow-up, compared with women who underwent myomectomy (86.7 [17.2]) or UAE (82.6 [21.5]) (p <
< 0.0001). Specifically, nearly 55.2% reported a maximum HR-QoL score of 100 at 1 year post-treatment, compared with 25.6% for myomectomy and 26.1% for UAE (p-value for trend <0.0001).
0.0001). Specifically, nearly 55.2% reported a maximum HR-QoL score of 100 at 1 year post-treatment, compared with 25.6% for myomectomy and 26.1% for UAE (p-value for trend <0.0001).
Table 4.
Change in Health-Related Quality of Life at 1-Year Follow-Up and Absolute Values of Health-Related Quality of Life at 1-Year Follow-Upa
| Unweighted | Weighted | |||||
|---|---|---|---|---|---|---|
| Myomectomy | Hysterectomy | UAE | Myomectomy | Hysterectomy | UAE | |
| Change in HR-QOL score from baseline to 1-year follow-up | ||||||
 <−10 points of change <−10 points of change | 3.4 | 1.6 | 1.3 | 3.2 | 2.4 | 0.8 |
 –10 to 0 points of change –10 to 0 points of change | 3.4 | 2.0 | 4.5 | 2.3 | 2.6 | 5.7 |
 0–10 points of change 0–10 points of change | 9.6 | 5.3 | 12.3 | 7.5 | 5.7 | 15.9 |
 10–20 points of change 10–20 points of change | 15.5 | 7.4 | 6.5 | 10.3 | 7.8 | 4.9 |
 ≥20 points of change ≥20 points of change | 68.2 | 83.7 | 75.5 | 76.8 | 81.5 | 72.7 |
 p-value trend p-value trend | <0.0001 | 0.0969 | ||||
| Total HR-QoL score at 1-year follow-up | ||||||
 <80 <80 | 23.1 | 10.5 | 32.3 | 27.0 | 12.7 | 31.8 |
 80–89 80–89 | 12.6 | 6.3 | 15.5 | 12.2 | 6.6 | 15.7 |
 90–99 90–99 | 36.5 | 25.8 | 28.4 | 35.1 | 25.5 | 26.5 |
 100 100 | 27.8 | 57.4 | 23.9 | 25.6 | 55.2 | 26.1 |
 p-value trend p-value trend | <0.0001 | <0.0001 | ||||
| Total HR-QoL score at 1-year follow-up, mean (SD) | 87.6 (17.3) | 93.1 (16.5) | 82.3 (21.4) | 86.7 (17.2) | 92.0 (17.8) | 82.6 (21.5) |
| p | <0.0001 | <0.0001 | ||||
UAE, uterine artery embolization.
Propensity score weighted SS scores at 1 year post treatment are displayed in Table 5. Again, women who underwent hysterectomy reported the lowest SS scores (8.2 [15.1]) compared with myomectomy (16.5 [15.1]) and UAE (19.6 [17.5]) (p <
< 0.0001). Nearly half of all patients who underwent hysterectomy (46.8%) reported a minimum SS score of “0” (p-value for trend <0.0001).
0.0001). Nearly half of all patients who underwent hysterectomy (46.8%) reported a minimum SS score of “0” (p-value for trend <0.0001).
Table 5.
Change in Symptom Severity at 1-Year Follow-Up and Absolute Values of Symptom Severity at 1-Year Follow-Up
| Unweighted | Weighted | |||||
|---|---|---|---|---|---|---|
| Myomectomy | Hysterectomy | UAE | Myomectomy | Hysterectomy | UAE | |
| Change in symptom severity score from baseline to 1-year follow-up | ||||||
 <−10 points of change <−10 points of change | 4.5 | 1.2 | 1.3 | 2.7 | 1.2 | 1.7 |
 –10 to 0 points of change –10 to 0 points of change | 4.0 | 0.8 | 1.3 | 1.7 | 1.0 | 1.1 |
 0–10 points of change 0–10 points of change | 11.0 | 5.8 | 9.7 | 6.1 | 6.9 | 10.4 |
 10–20 points of change 10–20 points of change | 12.3 | 4.7 | 11.6 | 9.9 | 5.9 | 12.2 |
 ≥20 points of change ≥20 points of change | 68.2 | 87.4 | 76.1 | 79.6 | 85.0 | 74.7 |
 p-value trend p-value trend | <0.0001 | 0.0405 | ||||
| Total symptom severity score at 1-year follow-up | ||||||
 >20 >20 | 32.5 | 8.9 | 40.6 | 32.8 | 9.3 | 41.9 |
 11–20 11–20 | 21.7 | 13.6 | 22.6 | 24.6 | 14.9 | 22.2 |
 1–10 1–10 | 29.1 | 31.2 | 19.4 | 24.4 | 29.0 | 17.9 |
 0 0 | 16.6 | 46.3 | 17.4 | 18.3 | 46.8 | 18.0 |
| p-value trend | <0.0001 | <0.0001 | ||||
| Symptom severity score at 1-year follow-up mean (SD) | 16.8 (15.9) | 7.8 (14.4) | 20.1 (18.0) | 16.5 (15.1) | 8.2 (15.1) | 19.6 (17.5) |
| p | <0.0001 | <0.0001 | ||||
Figure 2 demonstrates the distribution of HR-QoL by SS at both baseline and at 1 year post-treatment. It is notable that the majority of patients, regardless of treatment type, cluster in the right lower quadrant (high SS and low HR-QoL), but transition to the left upper quadrant at 1 year (low SS and high HR-QoL). (Correlation coefficients: overall, −0.719; myomectomy, −0.721; hysterectomy, −0.700; EA, −0.707; and UAE, −0.737).
Discussion
For all procedure types, we observed substantial improvement in HR-QoL and SS 1 year after treatment. By both metrics (HR-QoL and SS), we observed the most improvement for women who received a hysterectomy, followed by participants who had myomectomy, and then by those who had UAE. The smallest improvement was observed for women who received EA to treat their fibroids. While hysterectomy is clearly the most definitive treatment, hysterectomy is also the most invasive, and therefore, the subtle differences between the nonhysterectomy procedures warrant further investigation.
To date, studies have compared long-term outcomes for fibroid procedures such as UAE, myomectomy, and hysterectomy. A few studies report that UAEs and myomectomies yield comparable long-term outcomes for patient satisfaction, total symptomatic relief, and quality of life.15,20 While long-term studies have looked at comparative outcomes for UAE or myomectomy for women with UF and UAE versus hysterectomy at 428 and 10 years,29 outcomes with the UFS-QoL have not been reported.
Although UAE is a less invasive procedure, there is a significantly higher rate of reintervention compared to those who had surgical management (myomectomy or hysterectomy) (32% compared to 4%).19 When this risk of reintervention is examined over 5 years, estimates ranged from 17% to 33% for 5 years after myomectomy, EA, and UAE, with myomectomy showing the lowest 12-month reintervention rate (4.2%), followed by UAE (7.0%), and then EA (12.4%; both p <
< 0.001 relative to myomectomy.30 While Moss et al. saw no significant difference in long-term outcomes for symptomatic relief and quality of life between UAE, myomectomy, and hysterectomy, Broder et al. found comparable results in long-term outcomes for UAE and myomectomy only for those patients who did not require reintervention.18,19
0.001 relative to myomectomy.30 While Moss et al. saw no significant difference in long-term outcomes for symptomatic relief and quality of life between UAE, myomectomy, and hysterectomy, Broder et al. found comparable results in long-term outcomes for UAE and myomectomy only for those patients who did not require reintervention.18,19
More recently, the FEMME trial (treating fibroids with either embolization or myomectomy to measure the effect on quality of life among women wishing to avoid hysterectomy), demonstrated that, while the perioperative complications are greater following a myomectomy relative to UAE (29% vs. 24%), at 2 years, the fibroid-related quality of life was marginally better in women who had a myomectomy relative to those who underwent UAE.31 Mara et al. also noted that UAEs were associated with a higher incidence of reintervention, but because many of those were per protocol rather than symptoms, it is difficult to assess. Also 13% of UAE patients in that single study were unilateral only, with a technical failure rate much higher than most other studies. Regardless, at 2 years, there was no difference in symptom and quality-of-life outcomes.15
Our observations are consistent with other studies that found, although there was consistent improvement in long-term HR-QoL scores and symptomatic severity scores regardless of treatment type, women who had a hysterectomy experienced the greatest improvement compared with patients who had received UAE and myomectomy.13,16,32,33 Wallace et al. investigated the comparison between the surgical approaches (hysterectomy and myomectomy) and concluded that, despite the improvements for both procedures, hysterectomy was associated with a higher quality of life than myomectomy, specifically those performed through the minimally invasive route.17
Interestingly, 9.9% of our sample at baseline had an SS score of ≤20 and 11.9% had an HR-QoL score >80, yet all these participants elected to receive procedures for their fibroids (Table 1). Furthermore, a considerable number of participants who elected to receive a procedure for their fibroids reported both a low SS score and a high HR-QoL at baseline (Fig. 2A, B, see upper left quadrant).
While these participants reported improvements in HR-QoL and SS after their procedures, these improvements were marginal, especially compared to participants in low HR-QoL and high SS groups. This can be attributed to the fact that these participants did not have much room for improvement to begin with, as they were already close to having an optimal QoL and SS scores. Furthermore, this observation of patients with a low SS and relatively high HR-QoL electing treatment for fibroids suggests that fibroid-associated symptoms and related quality-of-life impact may not be the only fibroid-related concerns for women choosing to proceed with treatment.
These data raise questions regarding the rationale for treating this group of patients and the type of procedure elected. This observation may highlight the complexity of decision making for patients with UF. A variety of clinical and nonclinical considerations impact a patient's decision to move forward with treatment, including family history, long-term concerns, and economic factors. For example, if a patient's family history includes women with advanced disease requiring a hysterectomy, patients may opt for early intervention to preclude this and facilitate uterine preservation.
While we excluded those patients actively seeking fertility from this analysis, patients with future fertility interests may be included into this group. It is especially interesting to note the racial distribution in treatment choices. While a comparable number of white and black women chose myomectomy (38% vs. 41%), a greater percentage of black women underwent UAE than white women (70% vs. 22%). This decision does not appear to be related to the number of fibroids or median fibroid volume and may again reflect other nonclinical considerations, such as potentially a shorter recovery time after UAE and thus shorter time needed to take off work.
Health insurance coverage can impact patient treatment course since loss or change in insurance, and annual out-of-pocket deductibles may influence patients to be proactive in the management of their fibroids and procedure choices. Furthermore, it is important to consider how a statistically significant, but clinically marginal degree of relief may benefit an individual's quality of life. These are important questions to address, to justify the risks of these procedures and the costs not only for individual patients and their families but also for the health care system as a whole. Answering these questions was beyond the scope of our data and analysis.
However, one possibility is that lower risk options such as medication were already attempted with little to no success. We also speculated that, for these women, their selected fibroid procedures represented a safe means of alleviating minor symptoms, optimizing quality of life, and preventing future discomfort if they were informed that fibroids continue to grow over time. More research is needed to understand better the necessity, as well as the cost/benefit analysis of fibroid procedures for women with high QoL and low SS.
The strengths of this study include its large sample size, which provides greater precision to compare less common procedures, and the inclusion of a diverse patient population from across the United States, thereby increasing generalizability of results. The study population has a similar distribution of patient characteristics when compared with national data.11 Furthermore, the longitudinal design of our study provides prospective assessment of postsurgical quality of life and symptoms, minimizing potential for recall bias. The limitations of this nonrandomized, prospective cohort observational study include unmeasured confounding factors, specifically the lack of information on factors that may contribute to fibroid procedure choice that is not captured by the variables we collected in this study, which likely introduced bias.
Patients self-select type of treatment based on a multitude of parameters, which are largely unknown. Propensity score matching was used to attempt to alleviate this bias. Additional consideration is a significant variability in the degree of improvement across all study arms. This indicates a significant overlap in the degree of improvement across different study arms. Therefore, even if, on average, hysterectomy provides largest degree of improvement in symptoms, this may or may not be true for the individual patient. Therefore, future prospective randomized trials may answer the question how to provide a tailored treatment for the individual patient.
Conclusion
In this comparative analysis study of one-year follow-up HR-QoL and SS scores, we showed that all treatment modalities investigated (hysterectomy, myomectomy, UAE, and endometrial ablation) appeared to benefit women with SUF. The improvements in HR-QoL are reflected by clinical improvement in symptoms directly influenced by the fibroids, as well as emotional aspects of the disease, including depression and anxiety. The degree of improvement is impacted by uterine volume, a metric of fibroid bulk, as well as irregular bleeding and pelvic pressure.
However, uterine volume was significantly lower for patients who underwent endometrial ablation (Table 2), consistent with the notion that this treatment is performed for patients with irregular bleeding. This is of importance as it may cofound interpretation of results pertaining to fibroid symptoms. Of note, nearly 20% of all patients with higher SS (>20) and lower HR-QoL (<80) had prior treatment, with the most significant recurrence of symptoms in patients who previously had an AM. Interestingly, a high number of patients seeking treatment reported a low SS and high HR-QoL, despite which they proceeded to elect to undergo a surgical procedure.
Women who had a hysterectomy appeared to provide the greatest improvement in both SS and HR-QoL, followed by comparable improvement in patients who had either an AM or uterine embolization, consistent with previous studies. It is important to note that 1 year after treatment, patients who underwent either a myomectomy or UAE reported comparable symptom relief and health-related quality-of-life scores.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the enrolling clinical centers and collaborators: Atlanta Fibroid Center of Atlanta Interventional Institute: John C. Lipman, MD, Principal Investigator; Brigham and Women's and Affiliated Hospitals: Raymond M. Anchan, MD, PhD, Principal Investigator, Serene S. Srouji, MD, Antonio R. Gargiulo, MD, James Greenberg, MD (Massachusetts General Hospital), John C. Petrozza, MD (Beth Israel Deaconess Medical Center) and Olga Brooks, MD; University of California Fibroid Network: Vanessa Jacoby, MD, Principal Investigator (UC-San Francisco), Ram Parvataneni, MD, MPH (UC-Los Angeles), Erica Oberman, MD (UC-Los Angeles), Naghmeh Salamat Saberi, MD (UC-Irvine), Shira Varon, MD (UC-San Diego), and L. Elaine Waetjen, MD (UC-Davis); Henry Ford Health System: Ganesa Wegienka, PhD, Principal Investigator; Inova Health: George L. Maxwell, MD, Principal Investigator, and Abbas Shoberi, MD; Mayo Clinic: Elizabeth A. Stewart, MD, Principal Investigator, Shannon Laughlin-Tommaso, MD, Bijan Borah, PhD, and Joyce Balls-Berry, PhD; Satellite Site Investigators: Jennifer Bantz, MD, Paul Matigbay, MD, Gokhan Anil, MD, and Jason Dewitt, MD; Michigan Medicine (University of Michigan): Erica E. Marsh, MD, Principal Investigator; University of Mississippi Medical Center: Kedra Wallace, PhD, Principal Investigator, and J. Preston Parry, MD; UNC Health Care (The University of North Carolina at Chapel Hill): Wanda Nicholson, MD, Principal Investigator, Andrea Knittel, MD, Anissa Vines, PhD, Lauren Schiff, MD, and Stephen Loehr, MD.
The authors would also like to thank Maya Seshan and Anne Lindholm for editorial assistance with the article.
Authors' Contributions
R.M.A., P.B., K.T., E.D., A.M., A.G., J.P., O.B., S.S., C.C.M., J.G., G.W., E.A.S., W.K.N., S.L.-T., M.P.D, L.M., E.E.M., E.R.M., V.J., and J.B.S. were involved in conducting the study at their respective sites, patient recruitment, data analysis, and article preparation. D.W., L.T., S.V., A.I.V., L.W., and K.W. were involved in conducting the study at their respective sites, data analysis, and article preparation.
Disclaimer
The content of this article is solely the responsibility of the authors, and readers should not interpret any statement in this product as an official position or the views of AHRQ, the U.S. Department of Health and Human Services, or PCORI.
Author Disclosure Statement
R.M.A., D.W., P.B., K.T., E.D., A.M., O.B., S.S., C.C.M., J.G., G.R.W., W.K.N., S.Z., F.L., L.T., J.B.S., S.V., G.L.M., A.I.V., L.A.W, and K.W. have nothing to disclose related to this topic of research.
A.R.G. reports consulting for Medicaroid Inc., and Lumenis, Inc.
J.P. reports consulting for Hologic and is on the Myriad Speakers Bureau.
E.A.S. reports personal fees from Bayer, AbbVie, Allergan, Myovant, UpToDate, Med Learning Group, PeerView, and Welltwigs outside the submitted work and an issued patent “Methods and Compounds for Treatment of Abnormal Uterine Bleeding” 6440445.
S.L.-T. reports grants from Bayer and personal fees from Allergan Pharma and UpToDate outside the submitted work.
M.P.D. reports grants from AbbVie, Bayer, and ObsEva outside the submitted work.
E.E.M. reports consultant work for Allergan and Myovant Sciences outside the submitted work.
E.R.M. reports personal fees from AbbVie, Merck, Allergan, and Bayer outside the submitted work.
V.L.J. reports grants from Acessa Health outside the submitted work.
Funding Information
This study was supported by grant no. P50HS023418 from the Agency for Health care Research and Quality (AHRQ) with funding provided by the Patient-Centered Outcomes Research Institute (PCORI) under Memorandum of Understanding no. 2013-001.
References
Articles from Journal of Women's Health are provided here courtesy of Mary Ann Liebert, Inc.
Citations & impact
Impact metrics
Citations of article over time
Article citations
Systematic review and meta-analysis of current evidence in uterine artery embolization vs myomectomy for symptomatic uterine fibroids.
Sci Rep, 14(1):19252, 20 Aug 2024
Cited by: 0 articles | PMID: 39164326 | PMCID: PMC11336172
Review Free full text in Europe PMC
Current opinion on large-scale prospective myomectomy databases toward evidence-based preconception and antenatal counselling utilising a standardised myomectomy operation note.
Facts Views Vis Obgyn, 16(1):59-65, 01 Mar 2024
Cited by: 0 articles | PMID: 38551475 | PMCID: PMC11198879
The impact of fibroid treatments on quality of life and mental health: a systematic review.
Fertil Steril, 121(3):400-425, 19 Jan 2024
Cited by: 0 articles | PMID: 38246400 | PMCID: PMC11140829
Review Free full text in Europe PMC
New treatment options for nonsurgical management of uterine fibroids.
Curr Opin Obstet Gynecol, 35(4):288-293, 03 May 2023
Cited by: 2 articles | PMID: 37144584 | PMCID: PMC10330353
Review Free full text in Europe PMC
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Clinical Trials
- (1 citation) ClinicalTrials.gov - NCT02260752
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Long-term health-related quality of life and symptom severity following hysterectomy, myomectomy, or uterine artery embolization for the treatment of symptomatic uterine fibroids.
Am J Obstet Gynecol, 229(3):275.e1-275.e17, 26 May 2023
Cited by: 3 articles | PMID: 37244458
The Comparing Options for Management: PAtient-centered REsults for Uterine Fibroids (COMPARE-UF) registry: rationale and design.
Am J Obstet Gynecol, 219(1):95.e1-95.e10, 08 May 2018
Cited by: 21 articles | PMID: 29750955 | PMCID: PMC8889489
Short-term quality of life after myomectomy for uterine fibroids from the COMPARE-UF Fibroid Registry.
Am J Obstet Gynecol, 222(4):345.e1-345.e22, 31 Oct 2019
Cited by: 8 articles | PMID: 31678093
Uterine artery embolization as a treatment option for uterine myomas.
Obstet Gynecol Clin North Am, 33(1):125-144, 01 Mar 2006
Cited by: 33 articles | PMID: 16504811
Review
 1
1