Abstract
Objectives
To evaluate the demographic data, ocular and systemic findings, clinical management, and outcomes of patients with ocular cicatricial pemphigoid (OCP).Materials and methods
The medical records of 11 patients diagnosed as having OCP in the ophthalmology department of Ege University between 2008 and 2021 were evaluated retrospectively.Results
The patients' mean follow-up time was 14±5.76 months. All eyes (100%) had conjunctival involvement and 18 (81.81%) had corneal involvement. According to the Tauber staging system, 7 (31.81%), 8 (36.36%), and 7 (31.81%) of the eyes were stage 2, 3, and 4, respectively. The diagnosis was confirmed in 6 (66.66%) of 9 patients who underwent biopsy. Amniotic membrane transplantation was performed in 7 eyes, entropion surgery in 2 eyes, and electrocauterization for trichiasis in 5 eyes. Systemic involvement was observed in 45.45% (5/11) of patients, most commonly oral mucosal involvement (18.18%). Review of medical records showed that alkylating agents, steroids, and dapsone were used in patients treated before 2020. Mycophenolate mofetil was preferred to be used in combination with corticosteroids. Although treatment responses before mycophenolate mofetil usage could not be evaluated well because of loss to follow-up, 4 (66.66%) of 6 patients who received steroid treatment combined with mycophenolate mofetil showed partial or complete clinical remission. No serious side effects and drug withdrawal were observed.Conclusion
OCP is a sight-threatening autoimmune disease that affects older adults. Although positive biopsy results are valuable for diagnosis, negative results do not exclude the diagnosis. The main treatment is systemic immunosuppressives. Disease activity can be suppressed, especially with early initiation of drug therapy. These patients require a multidisciplinary approach. Especially in the presence of isolated ocular findings, ophthalmologists should be able to make the decision to start immunosuppressive treatment, and systemic treatment should not be delayed.Free full text

Clinical Approach to Ocular Cicatricial Pemphigoid
Abstract
Objectives:
To evaluate the demographic data, ocular and systemic findings, clinical management, and outcomes of patients with ocular cicatricial pemphigoid (OCP).
Materials and Methods:
The medical records of 11 patients diagnosed as having OCP in the ophthalmology department of Ege University between 2008 and 2021 were evaluated retrospectively.
Results:
The patients’ mean follow-up time was 14±5.76 months. All eyes (100%) had conjunctival involvement and 18 (81.81%) had corneal involvement. According to the Tauber staging system, 7 (31.81%), 8 (36.36%), and 7 (31.81%) of the eyes were stage 2, 3, and 4, respectively. The diagnosis was confirmed in 6 (66.66%) of 9 patients who underwent biopsy. Amniotic membrane transplantation was performed in 7 eyes, entropion surgery in 2 eyes, and electrocauterization for trichiasis in 5 eyes. Systemic involvement was observed in 45.45% (5/11) of patients, most commonly oral mucosal involvement (18.18%). Review of medical records showed that alkylating agents, steroids, and dapsone were used in patients treated before 2020. Mycophenolate mofetil was preferred to be used in combination with corticosteroids. Although treatment responses before mycophenolate mofetil usage could not be evaluated well because of loss to follow-up, 4 (66.66%) of 6 patients who received steroid treatment combined with mycophenolate mofetil showed partial or complete clinical remission. No serious side effects and drug withdrawal were observed.
Conclusion:
OCP is a sight-threatening autoimmune disease that affects older adults. Although positive biopsy results are valuable for diagnosis, negative results do not exclude the diagnosis. The main treatment is systemic immunosuppressives. Disease activity can be suppressed, especially with early initiation of drug therapy. These patients require a multidisciplinary approach. Especially in the presence of isolated ocular findings, ophthalmologists should be able to make the decision to start immunosuppressive treatment, and systemic treatment should not be delayed.
Introduction
Mucous membrane pemphigoid is an autoimmune disease characterized by accumulation of immunoglobulin (Ig) A, IgG, IgM, and/or complement components along the epithelial basal membrane region of mucosal surfaces such as the oral cavity, nasal cavity, esophagus, larynx, and eye.1 The clinical picture in which mucous membrane pemphigoid primarily affects the eye is called ocular cicatricial pemphigoid (OCP).2 Although ocular involvement may be unilateral at first, bilateral and asymmetrical involvement is observed over time.3 There are multiple assessment algorithms for disease stage and progression. The Tauber staging system enables a multidimensional evaluation, as it combines both fornix depth and conjunctival cicatrization assessment in grading.4 Although the diagnosis can be made clinically, it is supported by biopsy.5 Systemic immunosuppression is the foundation of treatment.
The aim of this study was to retrospectively evaluate the demographic characteristics, ocular and systemic findings, clinical management, and outcomes of patients with OCP who were followed up in the ophthalmology clinic of Ege University Hospital between 2008 and 2021.
Materials and Methods
Medical records pertaining to 22 eyes of 11 patients with OCP who were followed up in the cornea unit of the Ege University Department of Ophthalmology between 2008 and 2021 were evaluated retrospectively. We excluded patients with cicatrizing conjunctivitis due to secondary causes such as chemical injury or drug use and those with conditions that may be associated with cicatrizing conjunctivitis, including oculodermal diseases such as toxic epidermal necrosis/Stevens-Johnson syndrome and bullous pemphigoid, and rheumatological diseases such as systemic lupus erythematosus and Sjögren’s syndrome. The study was approved by the Ege University Faculty of Medicine Ethics Committee and was carried out in accordance with the Declaration of Helsinki.
Demographic data; ocular and systemic findings; Tauber disease stage; conjunctival, skin, or mucosal biopsy results; and treatment preferences and response were evaluated. Best corrected visual acuity (BCVA) in logMAR, lid and eyelash examination to detect pathologies such as entropion, ectropion, trichiasis, and distichiasis, and a slit-lamp examination involving a detailed evaluation of the cornea and conjunctiva were included in the ocular findings. The Tauber staging system for OCP was proposed in 1992 by Tauber et al.4 Stage 1 is subconjunctival scarring and fibrosis; stage 2 consists of fornix foreshortening of 0-25% (stage 2a), 25-50% (2b), 50-75% (2c), or 75-100% (2d) without symblepharon; stage 3 involves horizontal symblepharon of 0-25% (stage 3a), 25-50% (3b), 50-75% (3c), or 75-100% (3d); and stage 4 is ankyloblepharon. The need for surgical intervention and which surgical procedures were performed were recorded. The frequency of systemic involvement was evaluated. In addition, the effectiveness, adverse effect profile, and remission/recurrence rates of systemic mycophenolate mofetil therapy, which is currently the preferred treatment, were evaluated in 6 patients.
Results
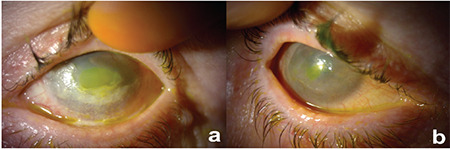
The median age of the patients was 76 years (range: 53-87) and the female:male ratio was 8:3. Mean BCVA was 1.9±0.97 logMAR (range: 0.3-3) before treatment and 1.74±0.95 logMAR (range: 0.2-3) after treatment. The mean follow-up time was 14±5.76 months. The patients’ data are summarized in Table 1.
Table 1
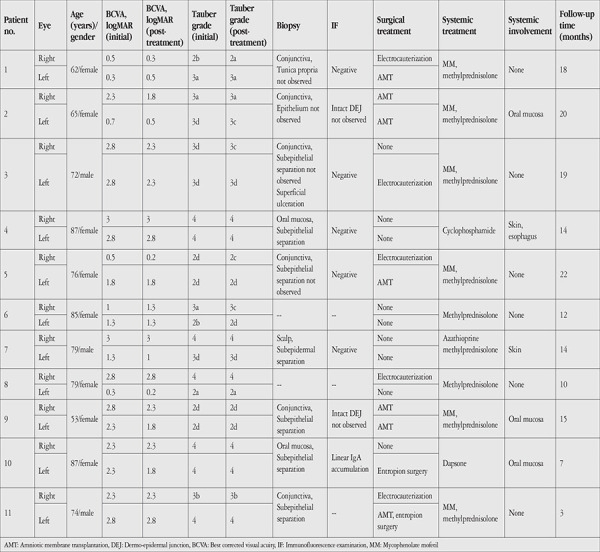
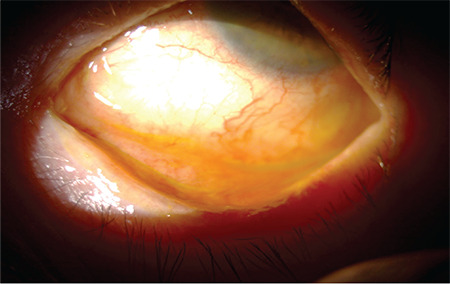
Fourteen (63.63%) of the 22 eyes had lid involvement, which was entropion in 5 eyes (22.72%). Conjunctival involvement was present in all eyes (100%). Figure 1 is an anterior segment photograph showing inferior fornix shortening. Eighteen eyes (81.81%) had corneal involvement, most commonly persistent epithelial defect (n=8). Figure 2 shows anterior segment photographs of a patient with bilateral corneal erosion. Amniotic membrane transplantation was performed in 7 eyes but was not effective in preventing recurrence of corneal erosions in 5 (71.42%) of them. Recurrent corneal erosion was observed at a mean of 28.8±9.88 days (range: 18-42) after amniotic membrane transplantation.
a) Anterior segment photograph showing the recurrence of fluorescein-stained corneal erosion in the left eye of a patient who underwent amniotic membrane transplantation due to recurrent corneal erosion. b) Anterior segment photograph of the same patient’s right eye showing corneal vascularization and fluorescein-stained central erosion
According to the Tauber staging system, 7 (31.81%) of the eyes were stage 2, 8 (36.36%) were stage 3, and 7 (31.81%) were stage 4. Nine of the 11 patients underwent biopsy for histopathologic examination. In 2 patients with data from before 2011, the diagnosis was made clinically and immunosuppressive treatment was initiated urgently because the disease was advanced and there was no suspected differential diagnosis. Conjunctival biopsy was performed in 6 patients, oral mucosa biopsy in 2 patients, and scalp biopsy in 1 patient. In 2 (33.33%) of the conjunctival biopsies, there was no subepithelial separation and no accumulation was detected in immunofluorescence (IF) examination. In the other 4 conjunctival biopsies (66.66%), ulceration and/or subepithelial separation were observed on the surface, but IF examination was inconclusive as an intact dermo-epidermal junction was not observed. Subepithelial/subepidermal separation was observed in 2 non-conjunctiva mucosal biopsies and the scalp biopsy, while linear IgA accumulation at the dermo-epidermal border was observed in one of the oral mucosal biopsies. Although histopathological findings supporting the diagnosis of OCP were observed in 6 (66.66%) of the 9 patients who underwent biopsy, the results of IF examination were not significant. Of the conjunctival biopsies, 2 had no intact dermo-epidermal junction, 2 had subepithelial separation, and 2 had no subepithelial separation and IF accumulation. Figure 3 shows conjunctival biopsy samples stained with hematoxylin and eosin.
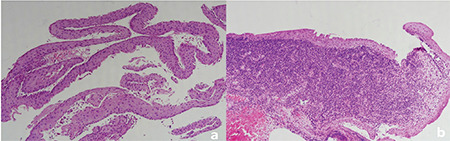
a) Conjunctival biopsy showing only the epithelial area, separated from the subepithelial area (H&E x200). b) Conjunctival biopsy with intense inflammatory cell infiltration in the tunica propria and no subepithelial separation (H&E x100)
Surgery was performed only in the event of complications. Amniotic membrane transplantation was performed in 7 eyes, entropion surgery in 2 eyes, and electrocauterization due to trichiasis in 5 eyes. Amniotic membrane transplantation was performed to treat epithelial erosions and for ocular surface reconstruction in 7 eyes with recurrent epithelial erosions and possible risk of corneal melting despite topical and systemic treatment and inadequate response to bandage contact lens application.
Systemic involvement was observed in 5 (45.45%) of the 11 patients, with oral mucosal involvement being most frequent (18.18%). One patient had a history of dilation for esophageal stenosis.
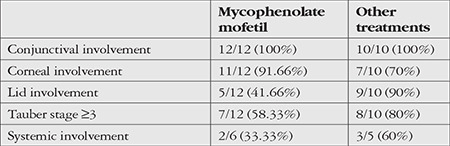
When the general medical records of the patients were examined, it was seen that alkylating agents, steroids, and dapsone were used in patients treated before 2020. We noted that with emerging evidence of its effectiveness in OCP, the use of mycophenolate mofetil in combination with corticosteroids became preferred. Mycophenolate mofetil (CELLCEPT 500 mg, Roche, Milano, Italy) was administered orally at a dose of 1,000 mg/day divided into 2 doses. Patients underwent hemogram and kidney and liver function tests before treatment, once a month for the first 3 months of treatment, and every 3 months thereafter. Treatment responses in the period before mycophenolate mofetil treatment could not be assessed well due to patient loss to follow-up. However, partial or complete clinical remission was observed in 4 (66.66%) of 6 patients who received combined steroid and mycophenolate mofetil therapy. Due to the progressive nature of the disease, we evaluated remission and determined that Tauber disease stage did not progress after treatment and there was no increase or decrease in BCVA values, similar to the literature.6 Systemic involvement was present in 2 (33.33%) of the 6 patients who received this treatment. Treatment responses could not be evaluated in one of the patients who received mycophenolate mofetil therapy because they died as a result of aspiration pneumonia (patient 11) and in another patient who developed concomitant secondary bacterial keratitis (patient 1). No serious adverse effects or drug discontinuation were observed in any of the patients. One patient experienced diarrhea early in treatment and needed only supportive treatment. During follow-up, recurrence in the form of recurrent corneal epithelial defect was observed in 4 (33.33%) of 12 eyes. Comparisons of clinical data between patients using mycophenolate mofetil and other systemic immunosuppressants are summarized in Table 2.
Table 2
Although systemic immunosuppression formed the basis of treatment, all patients used artificial tears containing sodium hyaluronate (Eyestil 0.15%, Sifi, Catania, Italy); cyclosporine drops (RESTASIS® 0.05%, Allergan, Irvine, CA, USA); and topical loteprednol (Lotemax 5 mg/mL, Bausch & Lomb, Tampa, FL, USA) or fluorometholone (Flarex 0.1%, Novartis, Puurs, Belgium), which are surface-active corticosteroids, during exacerbations. Corticosteroid dose was increased in the early postoperative period in patients who underwent surgery.
Discussion
OCP is a rare autoimmune disease that usually affects older adults and is characterized by progressive inflammation and cicatrization of the conjunctiva. Its incidence has been reported at rates varying from 1/20,000 to 1/46,000 in the literature.7 Patients are usually diagnosed in the 7th decade and the condition is more common in women.7,8 In this study, 8 (72.72%) of the 11 patients were women and the median age was 76 (range: 53-87). Thus, the demographic data were consistent with the literature. Similarly, systemic involvement has been reported in approximately 50% in the literature and was observed in 45.45% of the patients in our study.5 The most common extraocular finding is oral mucosal involvement, with desquamative gingivitis usually observed. Patients may present initially to a dentist.9 In our study, oral mucosal involvement was present in 2 of the 5 patients with systemic involvement.
The Tauber staging system for OCP was preferred in this study because it includes both the degree of conjunctival cicatrization in the Foster system and fornix shortening used in the Mondino system.4
The ocular findings of the disease vary. In a cohort study with 34 eyes, the most common clinical finding was conjunctival involvement (100%), followed by corneal involvement (88%) and lid involvement (71%).10 In the present study, the frequency of conjunctival involvement was 100%, but the frequency of corneal (81.81%) and lid (63.63%) involvement was lower compared to the literature. The lower rates of corneal and lid involvement may be explained by the relatively high proportion of patients with early-stage disease.
The diagnosis is generally delayed because initial findings of the disease are non-specific.11 In a retrospective study of 51 patients, it was reported that 83% of patients were at clinical stage 3 or higher at diagnosis.12 In our study, 68.18% of the patients were stage 3 or above. The relatively low number of patients in the advanced stage may be attributed to the high clinical suspicion in our center, which is an important criterion in the early diagnosis of the disease.
The combination of clinical findings and IF confirmation is very valuable in the diagnosis of OCP. Conventional histological examination is insufficient, and demonstrating immune deposit accumulation in the conjunctival basement membrane by direct IF is the gold standard in the diagnosis. Despite adherence to proper sampling techniques, the sensitivity of the direct IF technique in the literature varies widely between 20% and 87%.7,13 In this study, biopsy tissues were collected appropriately and transferred for pathological examination.14 Histopathological findings supporting the diagnosis of OCP were observed in 6 (66.66%) of 9 biopsied patients, while immune accumulation was detected in 1 (20%) of the 5 biopsies in which the dermo-epidermal junction in IF examination of 7 biopsies. IF examination in patients with OCP reveals IgG, complement C3, and to a lesser extent linear IgA accumulation in the epithelial basement membrane zone.15 Differential diagnosis from linear IgA disease cannot be made pathologically but can be made clinically. Although linear IgA disease was considered in the differential diagnosis of the patient with linear IgA accumulation in oral mucosal biopsy, evaluation together with their dermatological and ocular findings was consistent with OCP. Positive biopsy is a valuable finding, but negative biopsy results do not exclude the diagnosis.
Although the prognosis of surgical outcomes is unfavorable in OCP patients, surgery may be required in some cases, such as entropion, which causes ocular surface irritation.16 Cataract surgery can be performed under adequate immunosuppressive therapy to increase vision, but keratoplasty is recommended only for tectonic purposes, as it has a very poor prognosis due to limbal stem cell deficiency, insufficient lid function, and dry eye.17 In this study, cataract surgery was not planned because none of the patients had cataract severe enough to impact visual prognosis. In addition, limbal allograft transplantation can be considered for limbal stem cell deficiency and the associated visual impairment. However, the procedure is not preferred due to the inflammatory nature of the disease and the fact that the 1-year success rate in allograft applications is around 50%.18 In our study, amniotic membrane transplantation was performed in 7 eyes for recurrent corneal erosion and ocular surface reconstruction, 2 eyes underwent entropion surgery, and 5 underwent electrocauterization. Despite performing the surgical interventions after suppressing the inflammatory process, amniotic membrane transplantation failed to prevent the recurrence of corneal ulcerations in 5 eyes (71.42%). Considering that even minor conjunctival traumas can accelerate disease progression in these patients, the 8/0 Vicryl sutures and surgical manipulations made during amniotic membrane transplantation may have triggered inflammation. Barabino et al.19 reported that of 9 eyes with advanced OCP, 6 eyes (66.7%) exhibited goblet cells and restoration of the normal conjunctival epithelium on impression cytology performed 4 weeks after amniotic membrane transplantation. In our study, the patients were only assessed clinically after surgery, and the lack of cytological examination may have resulted in a limited evaluation of response. It has been suggested that during the treatment of corneal ulcerations in OCP patients, amniotic grafting should be performed only on the corneal surface to avoid surgical manipulation of the conjunctiva.20
Systemic immunosuppression is the foundation of treatment. Mild to moderate inflammation can be suppressed with dapsone.8 However, because of the need for close follow-up and some serious side effects such as hemolytic anemia and hepatitis, dapsone therapy is now being replaced by mycophenolate mofetil. Mycophenolate mofetil was preferred as the first-line treatment option in our clinic. In a retrospective study of 23 patients treated with mycophenolate mofetil, clinical remission was reported in 82.6% of patients within 12 months.21 In our study, partial or complete clinical remission was documented in 66.66% of patients receiving mycophenolate mofetil therapy. The lower remission rate in our study may be explained by the small number of patients (one of whom died) and the relatively short follow-up period.
Study Limitations
Limitations of this study include its retrospective study design and the limited sample size. Larger prospective studies on this subject are needed.
Conclusion
OCP is a rare, sight-threatening disease that affects older people. Although positive biopsy results are very valuable in the diagnosis, negative results do not rule out the disease. The main treatment is systemic immunosuppressives, and disease activity can be suppressed with early initiation of therapy. This disease requires a multidisciplinary approach; in patients with isolated ocular findings, ophthalmologists should be able to make immunosuppressive treatment decisions and systemic treatment should not be delayed.
Footnotes
Ethics
Ethics Committee Approval: Ege University Medical Research Ethics Committee, 22-IT/20.
Informed Consent: Obtained.
Peer-review: Internally and externally peer reviewed.
Authorship Contributions
Surgical and Medical Practices: Ö.B.S., M.P., S.E., A.Y., B.Y., Concept: Ö.B.S., M.P., Design: Ö.B.S., Data Collection or Processing: M.D.Ç., Analysis or Interpretation: İ.K., T.A., Literature Search: M.D.Ç., İ.K., Writing: M.D.Ç., İ.K., Ö.B.S., M.P., B.Y.Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
Articles from Turkish Journal of Ophthalmology are provided here courtesy of Galenos Yayinevi
Full text links
Read article at publisher's site: https://doi.org/10.4274/tjo.galenos.2022.34683
Read article for free, from open access legal sources, via Unpaywall:
http://cms.oftalmoloji.org/Uploads/Article_60213/TJO-53-79-En.pdf
Citations & impact
Impact metrics
Article citations
Use of Systemic Mycophenolate Mofetil Therapy in Ocular Surface Inflammatory Pathologies at the Initiative and Responsibility of the Ophthalmologist.
Middle East Afr J Ophthalmol, 29(4):209-215, 01 Oct 2022
Cited by: 0 articles | PMID: 38162558 | PMCID: PMC10754105
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
[Ocular Cicatricial Pemphigoid - a Retrospective Study].
Cesk Slov Oftalmol, 72(1):283-292, 01 Feb 2016
Cited by: 2 articles | PMID: 27041284
[Ocular cicatricial pemphigoid. Retrospective analysis of risk factors and complications].
Ophthalmologe, 97(2):113-120, 01 Feb 2000
Cited by: 11 articles | PMID: 10734737
A nonrandomized comparison of the clinical outcome of ocular involvement in patients with mucous membrane (cicatricial) pemphigoid between conventional immunosuppressive and intravenous immunoglobulin therapies.
Clin Immunol, 111(3):303-310, 01 Jun 2004
Cited by: 50 articles | PMID: 15183151
Clinical Characteristics and Outcomes of Ocular Cicatricial Pemphigoid: A Cohort Study and Literature Review.
Cornea, 38(11):1406-1411, 01 Nov 2019
Cited by: 3 articles | PMID: 31356420
Review

 1,*
1,*