Abstract
Free full text
A point mutation in recC associated with subclonal replacement of carbapenem-resistant Klebsiella pneumoniae ST11 in China
Abstract
Adaptation to selective pressures is crucial for clinically important pathogens to establish epidemics, but the underlying evolutionary drivers remain poorly understood. The current epidemic of carbapenem-resistant Klebsiella pneumoniae (CRKP) poses a significant threat to public health. In this study we analyzed the genome sequences of 794 CRKP bloodstream isolates collected in 40 hospitals in China between 2014 and 2019. We uncovered a subclonal replacement in the predominant clone ST11, where the previously prevalent subclone OL101:KL47 was replaced by O2v1:KL64 over time in a stepwise manner. O2v1:KL64 carried a higher load of mobile genetic elements, and a point mutation exclusively detected in the recC of O2v1:KL64 significantly promotes recombination proficiency. The epidemic success of O2v1:KL64 was further associated with a hypervirulent sublineage with enhanced resistance to phagocytosis, sulfamethoxazole-trimethoprim, and tetracycline. The phenotypic alterations were linked to the overrepresentation of hypervirulence determinants and antibiotic genes conferred by the acquisition of an rmpA-positive pLVPK-like virulence plasmid and an IncFII-type multidrug-resistant plasmid, respectively. The dissemination of the sublineage was further promoted by more frequent inter-hospital transmission. The results collectively demonstrate that the expansion of O2v1:KL64 is correlated to a repertoire of genomic alterations convergent in a subpopulation with evolutionary advantages.
Introduction
Klebsiella pneumoniae is a significant nosocomial pathogen worldwide, and its remarkable ability to acquire antibiotic resistance largely facilitates its widespread dissemination. In the last decade, the rate of multidrug-resistant (MDR) K. pneumoniae, particularly carbapenem-resistant K. pneumoniae (CRKP), is trending upwards globally, and is associated with an enormous global public health burden1–3. In particular, bloodstream infections (BSI) caused by CRKP highly challenges clinical treatments, resulting in a high mortality rate of up to over 50% in nosocomial settings4,5. The World Health Organization has included CRKP in a list of antimicrobial-resistant priority pathogens for which new antibiotics are urgently needed.
The rapid expansion of CRKP has been attributed to the acquisition of carbapenemases as well as the establishment of successful clones (i.e., high-risk clones). The population structure of CRKP varies geographically6. In Asia, especially China, KPC-2-producing sequence type (ST) 11 is predominant, accounting for up to 60–70% of CRKP3. ST258, a supposed descendent of ST11, has become the most prevalent KPC-2/KPC-3 producing clone in North America, Latin America, and Europe2,6,7. Although these clones have remained at high prevalence in certain regions for decades, intra-clonal segregations have been observed. More than two subclones have been identified in the ST11 and ST258 population, and recombinations involving the capsule polysaccharide synthesis (CPS) locus are supposed to be primarily responsible for genetic diversification4,8,9. We recently revealed a subclonal switch among CRKP-ST11 bloodstream isolates collected in a single center in China between 2013 and 2017, where ST11-KL47 had been displaced by ST11-KL64 as the predominant subclone4. Of greater concern, ST11-KL64 has evolved enhanced pathogenicity, resulting in significantly higher 30-day mortality compared to ST11-KL47. However, the spatiotemporal dynamics and underlying driving forces of the population structure remain poorly understood.
In this work, we investigate the genomic evolution of 794 CRKP isolates collected in the framework of national surveillance for bloodstream isolates between 2014 and 2019 across China to elucidate the spatial and temporal dynamic population structure of CRKP-ST11 and to dissect the genetic and phenotypic drivers of the intra-clonal diversification. The genomic alterations correlating with subclonal switch and phenotypical variations in the dominant ST11 population are characterized and linked to evolutionary drivers.
Results
Population structure of CRKP bloodstream (CRKP-BS) isolates in China
Between 2014 and 2019, 4635 K. pneumoniae species complex bloodstream isolates were collected from 45 sentinel hospitals distributed across 19 provinces covering 75.7% population of China (ca. 1.06 billion) (Fig. 1a). A total of 794 non-repetitive CRKP isolates were identified in 40 hospitals of 16 provinces, including 772 K. pneumoniae sensu stricto, 10 K. variicola, 11 K. quasipneumoniae, and 1 K. michiganensis (not belonging to K. pneumoniae species complex but was included in the analysis) (Supplementary Fig. 1 and Supplementary Dataset 1). The proportion of CRKP had increased from 11.2% to 17.7% over the study period (Fig. 1b). The population structure of CRKP-BS was highly complex, and 72 STs were detected (Supplementary Dataset 1). ST11 was the predominant clone (81.4%; 646/794), followed by ST15 (55/794; 6.93%).
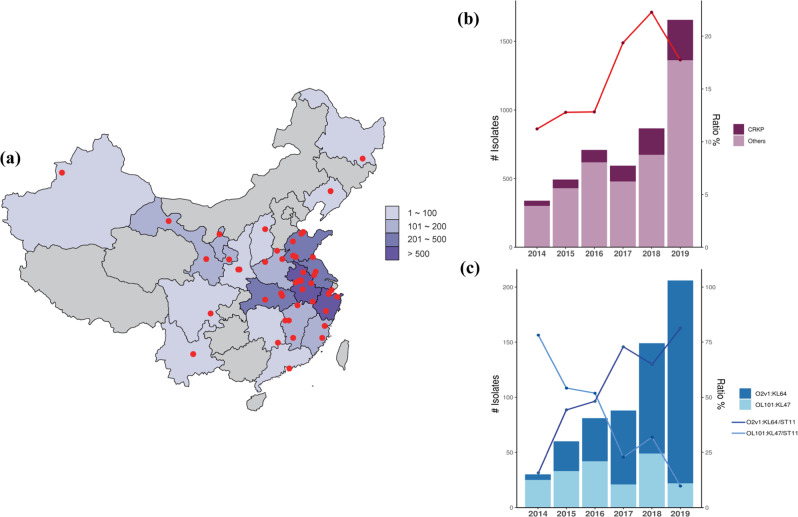
a Geographical distribution of 45 sentinel hospitals participating in this study. The number of isolates collected in each province is shown by color gradients at the right. b The graph shows the number (dark red bars) and the ratio of CRKP (red line) detected each year during the surveillance. c The graph shows the number of O2v1:KL64 and OL101:KL47 detected in CRKP (blue bars) each year, and the ratio of O2v1:KL64 to CRKP-ST11 (purple line) and OL101:KL47 to CRKP-ST11 (blue line). Source data are provided as a Source Data file.
One or more carbapenemase genes were detected in 771 of 794 isolates (97.1%), and 753 belonged to K. pneumoniae sensu stricto, which encoded blaKPC-like (n =
= 712; including 709 blaKPC-2 and 3 blaKPC-3), blaNDM-like (n
712; including 709 blaKPC-2 and 3 blaKPC-3), blaNDM-like (n =
= 36), blaIMP-like (n
36), blaIMP-like (n =
= 4), and blaOXA-48-like (n
4), and blaOXA-48-like (n =
= 5) genes (Supplementary Dataset 1). The majority of blaKPC-like-positive K. pneumoniae sensu stricto isolates (686/712; 96.3%) belong to ST11 and ST15, suggesting clonal dissemination of blaKPC-like genes in China.
5) genes (Supplementary Dataset 1). The majority of blaKPC-like-positive K. pneumoniae sensu stricto isolates (686/712; 96.3%) belong to ST11 and ST15, suggesting clonal dissemination of blaKPC-like genes in China.
Occurrence of subclonal switch in CRKP-ST11 within a 6-year period
We identified 55 K-loci (KLs, capsule synthesis loci) and ten O-loci (OLs, outer lipopolysaccharide synthesis loci) in the CRKP-BS population (Supplementary Dataset 1). ST11 comprised 13 KLs and 8 OLs, of which KL64 (422/646; 65.3%) and O2v1 (418/646; 64.8%) was the most prevalent, followed by KL47 (192/646; 29.7%) and OL101 (an O12 derivative) (193/646; 29.9%). ST15 included 5 KLs and 5 OLs, and KL19 (43/56; 76.8%) and O2v1 (42/56; 75%) were predominant. The proportion of OL101:KL47 among CRKP-ST11 dropped from 78.1% (25/32) in 2014 to 9.7% (22/226) in 2019, whereas that of O2v1:KL64 (4 OL102:KL64 isolates were included to simplify the analysis through the study) increased from 15.6% (5/32) in 2014 to 81.4% (184/226) in 2019 (Fig. 1c). The findings demonstrate that subclonal replacement has occurred from OL101:KL47 to O2v1:KL64 within the ST11 population in China. The subclone O2v1:KL19 was constantly prevalent in ST15 during the study period (66.7%-87%).
O2v1:KL64 is derived from OL101:KL47
To determine the phylogenetic relationship of these ST11 subclones, a maximum-likelihood tree was derived from 4460 recombination-free SNPs. A clade comprising isolates of O2v1:KL103, O2v2:KL105, O3b:KL111, and O4:KL15 was basal in the tree (Fig. 2), presenting the ancestral clade of the ST11 isolates. All O2v1:KL64 isolates clustered together to form the deepest branching clade and also clustered with one sublineage of OL101:KL47, indicating that O2v1:KL64 was derived from OL101:KL47. This is consistent with our previous conclusion from single-center data4. The other serotypes clustered either with OL101:KL47 (O3/O3a:KL10 and O5:KL25) or with O2v1:KL64 (O2v1:KL21, O2v1:KL28, O2v1:KL31, O2v1:KL103, O2v1:KL107, and O3/O3a:KL58), supporting the notion that they evolved from the two major subclones.
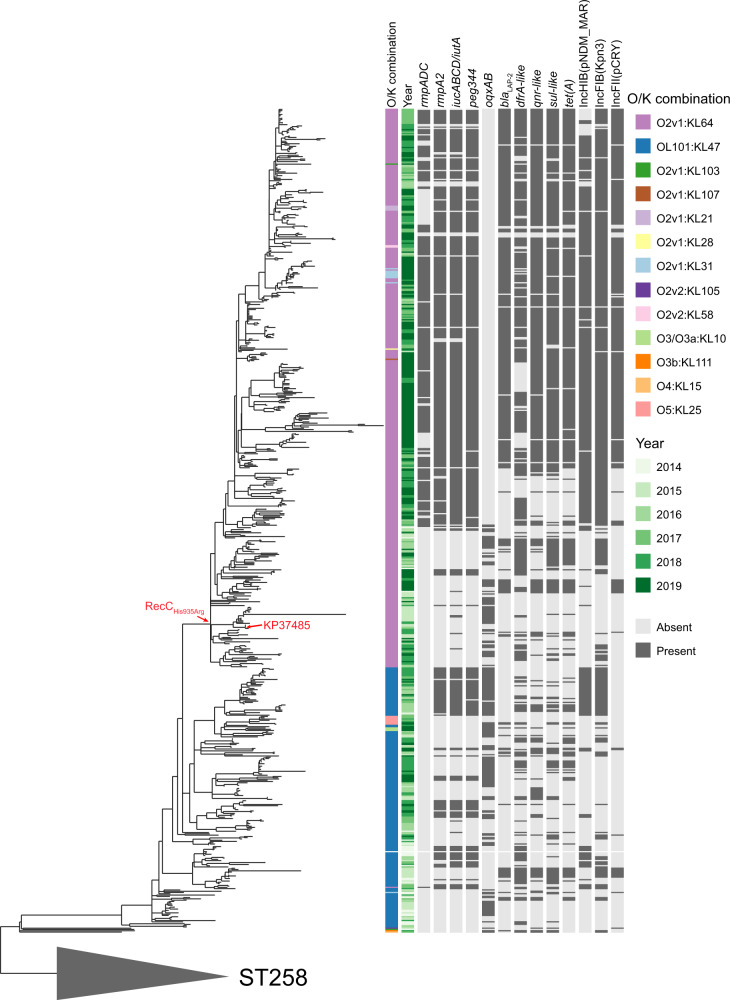
The phylogenetic tree was obtained by mapping all sequence reads to the hybrid assembly of an ST11-OL101:KL47 isolate (KP16932) and removing the recombined regions from the alignment. The tree was rooted using the ST258 outgroup isolates (gray triangle). Thirteen O/K combinations were detected in our ST11 collection, which are indicated in different colors, as shown in the legend. The hypervirulence biomarkers detected (except for iro due to its rarity in our collection) are shown here. The ARGs [blaLAP-2, dfrA-like, qnr-like, sul-like, tet(A), and oqxAB] detected with significantly different abundance between OL101:K47 and O2v1:KL64 are shown. The replicon types corresponding to the prevalent virulence [IncHI1B(pNDM-MAR) and IncFIB(Kpn3)] and MDR plasmid [IncFII(pCRY)] carrying these ARGs (except for oqxAB) are shown here. The RecC allele (RecCHis935Arg) was detected exclusively in O2v1:KL64, as shown on the branch, and the reference (KP37485) used in the recombination assay is indicated on the tree. Source data are provided as a Source Data file.
Recombination contributes significantly to the intra-clonal diversification of CRKP-ST11
We identified 42,824 core-genome SNPs prior to and 4460 SNPs after the removal of recombination regions, suggesting that recombination has contributed heavily to the population diversity. These include a 96.1-kb and 12.1-kb region encompassing the CPS and lipopolysaccharide (LPS) locus that introduced 1182 and 261 SNPs, respectively, thereby accounting for the switch from OL101:KL47 to O2v1:KL64 (Supplementary Fig. 2). There were additional recombination events spanning the CPS and/or LPS region that were detected in the OL101:KL47/O2v1:KL64-derived subclones and these also conferred switches in O/K-types.
To further estimate the role of recombination in the genetic variations of O2v1:KL64 and OL101:KL47, we calculated nucleotide divergence for all pairs of genomes within the two subclones before and after the removal of recombinant sequence regions. Less nucleotide divergence was detected in O2v1:KL64 than in OL101:KL47 before (median pairwise divergence: 4.2 ×
× 10−5 vs 1.5
10−5 vs 1.5 ×
× 10−4; p
10−4; p <
< 2.2
2.2 ×
× 10−16 by Wilcoxon rank-sum test) and after the removal of recombination regions (1.3
10−16 by Wilcoxon rank-sum test) and after the removal of recombination regions (1.3 ×
× 10−5 vs 2.1
10−5 vs 2.1 ×
× 10−5; p
10−5; p <
< 2.2
2.2 ×
× 10−16) (Supplementary Fig. 3). This is probably due to the fact that O2v1:KL64 emerged later than OL101:KL47 and has had less time to accumulate genetic diversity. The r/m value of O2v1:KL64 was approximately 2.5-fold higher than that of OL101:KL47 (17.68 vs 7.28), suggesting that the contribution of recombination to the genetic variations was higher in O2v1:KL64 than in OL101:KL47.
10−16) (Supplementary Fig. 3). This is probably due to the fact that O2v1:KL64 emerged later than OL101:KL47 and has had less time to accumulate genetic diversity. The r/m value of O2v1:KL64 was approximately 2.5-fold higher than that of OL101:KL47 (17.68 vs 7.28), suggesting that the contribution of recombination to the genetic variations was higher in O2v1:KL64 than in OL101:KL47.
Point mutation in RecC confers a higher recombination frequency to O2v1:KL64
Given the higher r/m value detected in O2v1:KL64 compared with OL101:KL47, and more serotypes derived from O2v1:KL64 (n =
= 7) than from OL101:KL47 (n
7) than from OL101:KL47 (n =
= 2), we supposed that O2v1:KL64 might have evolved with higher recombination proficiency. To test the hypothesis, we examined subclone-specific SNPs associated with recombination, and a single missense mutation in the recC gene (2804
2), we supposed that O2v1:KL64 might have evolved with higher recombination proficiency. To test the hypothesis, we examined subclone-specific SNPs associated with recombination, and a single missense mutation in the recC gene (2804 A
A >
> G; His935Arg) was exclusively found in O2v1:KL64 compared with the sequence of OL101:KL47. It is known that functional recC is required for genetic recombination in Escherichia coli, and mutations in recC can affect recombination proficiency10. We engineered an O2v1:KL64 mutant (KP37485ΔrecC), and confirmed that deletion of recC indeed abolished recombination proficiency reflected by the resistance to the DNA-damaging agent mitomycin C11, which could be restored by complementation with recCO2v1:KL64 or recCOL101:KL47 (Fig. 3), demonstrating that recC is involved in recombination in K. pneumoniae as that in E. coli.
G; His935Arg) was exclusively found in O2v1:KL64 compared with the sequence of OL101:KL47. It is known that functional recC is required for genetic recombination in Escherichia coli, and mutations in recC can affect recombination proficiency10. We engineered an O2v1:KL64 mutant (KP37485ΔrecC), and confirmed that deletion of recC indeed abolished recombination proficiency reflected by the resistance to the DNA-damaging agent mitomycin C11, which could be restored by complementation with recCO2v1:KL64 or recCOL101:KL47 (Fig. 3), demonstrating that recC is involved in recombination in K. pneumoniae as that in E. coli.
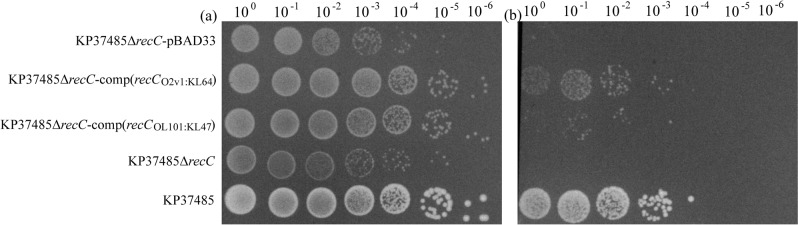
Late logarithmic phase cells grown in LB broth with 0.2% (w/v) l-arabinose and 25 mg/L chloramphenicol were harvested and resuspended in PBS to obtain 5
mg/L chloramphenicol were harvested and resuspended in PBS to obtain 5 ×
× 108 cfu/ml, followed by being treated with PBS (a) or mitomycin C at 8
108 cfu/ml, followed by being treated with PBS (a) or mitomycin C at 8 mg/L (b) for 1
mg/L (b) for 1 h. Cultures were serially diluted tenfold, spotted at 10
h. Cultures were serially diluted tenfold, spotted at 10 ul in rows on LB plates, and incubated overnight at 37
ul in rows on LB plates, and incubated overnight at 37 °C. Source data are provided as a Source Data file.
°C. Source data are provided as a Source Data file.
To validate whether the single missense mutation of recC could affect recombination proficiency, we engineered an isogenic mutant KP37485-recCOL101:KL47 by replacing the recCO2v1:KL64 with recCOL101:KL47. Apart from 2804 A
A >
> G, no other SNPs were found in the genome of KP37485-recCOL101:KL47 confirmed by sequencing. Compared with that of KP37485, a threefold reduction of resistance to mitomycin C was observed for KP37485-recCOL101:KL47 [survival ratio: (1.85
G, no other SNPs were found in the genome of KP37485-recCOL101:KL47 confirmed by sequencing. Compared with that of KP37485, a threefold reduction of resistance to mitomycin C was observed for KP37485-recCOL101:KL47 [survival ratio: (1.85 ±
± 0.38)
0.38) ×
× 10−6 vs (0.62
10−6 vs (0.62 ±
± 0.05)
0.05) ×
× 10−6); p
10−6); p =
= 0.0295 by t-test], indicating that the single mutation in recC gene has an effect on recombination proficiency. We further designed a transduction experiment to validate the impact of the two recC alleles on recombination frequency (Supplementary Fig. 4). KP37485 showed a 245-fold higher recombination frequency than KP37485-recCOL101:KL47 [mean (1.38
0.0295 by t-test], indicating that the single mutation in recC gene has an effect on recombination proficiency. We further designed a transduction experiment to validate the impact of the two recC alleles on recombination frequency (Supplementary Fig. 4). KP37485 showed a 245-fold higher recombination frequency than KP37485-recCOL101:KL47 [mean (1.38 ±
± 0.48)
0.48) ×
× 10−8 vs (5.62
10−8 vs (5.62 ±
± 0.44)
0.44) ×
× 10−11; p
10−11; p =
= 0.0388 by t-test], while homologous recombination was undetectable in KP37485ΔrecC. The results demonstrate that the single missense mutation in the recC gene can significantly enhance recombination proficiency.
0.0388 by t-test], while homologous recombination was undetectable in KP37485ΔrecC. The results demonstrate that the single missense mutation in the recC gene can significantly enhance recombination proficiency.
We further analyzed 14,407 K. pneumoniae genomes retrieved from the NCBI RefSeq database as of November 2022 to determine the distribution of recCHis935Arg, and the allele was exclusively found in 763 of 823 ST11 O2v1:KL64 isolates (Supplementary Dataset 2). All but one of the recCHis935Arg-positive isolates were collected in China, indicating that recCHis935Arg was specific to Chinese ST11 O2v1:KL64 isolates.
O2v1:KL64 encodes a higher load of mobile genetic elements (MGEs)
Recombination and horizontal gene transfer are known to be vital in shaping bacteria genome structures by affecting the exchange of genetic materials, e.g., MGEs12. We here analyzed MGEs in the 646 ST11 genomes, including integrons, insertion sequences (ISs), prophages, and plasmids (approximated by replicons), to identify additional mechanisms involved in the diversification of CRKP-ST11. A significantly higher load of prophages, replicons, and ISs was found in O2v1:KL64 compared to OL101:KL47 (median 9 vs 8; 6 vs 4; and 22 vs 18, respectively) (Wilcoxon rank-sum test: p =
= 2.2
2.2 ×
× 10−16; 2.2
10−16; 2.2 ×
× 10−16; 1.87
10−16; 1.87 ×
× 10−8) (Supplementary Fig. 5a–d), while the number of integrons was comparable in the two subclones with a significantly different distribution (median 2 vs 2; p
10−8) (Supplementary Fig. 5a–d), while the number of integrons was comparable in the two subclones with a significantly different distribution (median 2 vs 2; p =
= 6.88
6.88 ×
× 10−9) (Supplementary Fig. 5e). A similar trend was found between ST11 and no-ST11 (Supplementary Fig. 6). To better understand whether the differences in prophages, plasmids, and ISs between the two subclones were due to vertical or horizontal transfer, we reconstructed the ancestral states of these MGEs. Our results indicate that the large-scale expansion of plasmids and ISs within O2v1:KL64 was likely caused by a single acquisition event (Fig. 4a, b), supporting the vertical model. In contrast, we found that differences in prophages were likely due to multiple acquisition and loss events within O2v1:KL64 (Fig. 4c), suggesting a more complex pattern of horizontal transfer. These findings support the critical role of MGEs, especially of prophages and plasmids, in shaping the population structure of CRKP-ST11.
10−9) (Supplementary Fig. 5e). A similar trend was found between ST11 and no-ST11 (Supplementary Fig. 6). To better understand whether the differences in prophages, plasmids, and ISs between the two subclones were due to vertical or horizontal transfer, we reconstructed the ancestral states of these MGEs. Our results indicate that the large-scale expansion of plasmids and ISs within O2v1:KL64 was likely caused by a single acquisition event (Fig. 4a, b), supporting the vertical model. In contrast, we found that differences in prophages were likely due to multiple acquisition and loss events within O2v1:KL64 (Fig. 4c), suggesting a more complex pattern of horizontal transfer. These findings support the critical role of MGEs, especially of prophages and plasmids, in shaping the population structure of CRKP-ST11.
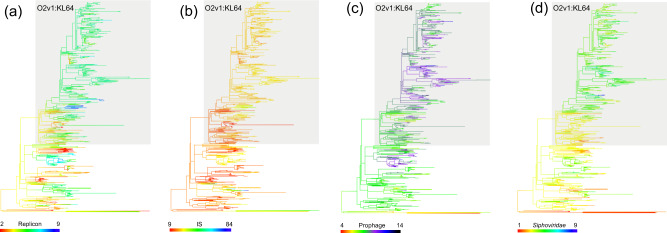
MGE was mapped as a continuous character onto the phylogenetic tree calculated by the 646 ST11 genomes. Evolution reconstructed with the R package phytools on the dataset, including the number of plasmid replicons (a), IS copies (b), prophages (c), and Siphoviridae prophages (d) identified per genome. Colors are assigned based on the number of MGEs detected per genome, as indicated by the bars. The O2v1:KL64 subclone is highlighted by a gray box. Source data are provided as a Source Data file.
It is known that phage-induced selective pressures play a critical role in driving the serotype switch of K. pneomoniae13. We, therefore, examined whether the presence and type of phages were possibly involved in the intra-clonal diversification of CRKP-ST11. Most of the prophages detected (95.03%) were classified into three families, namely Myoviridae, Podoviridae, and Siphoviridae. A load of Myoviridae and Podoviridae prophages was comparable between the two subclones (median 92 kb; 19.8
kb; 19.8 kb), while that of Siphoviridae prophages was significantly higher in O2v1:KL64 than in OL101:KL47 (median 95
kb), while that of Siphoviridae prophages was significantly higher in O2v1:KL64 than in OL101:KL47 (median 95 kb vs 60.3
kb vs 60.3 kb) (p
kb) (p =
= 2.2
2.2 ×
× 10−16 by Wilcoxon rank-sum test) (Supplementary Fig. 5f–h). As with plasmids and ISs, the widespread expansion of Siphoviridae prophages probably resulted from a single acquisition event within O2v1:KL64 (Fig. 4d).
10−16 by Wilcoxon rank-sum test) (Supplementary Fig. 5f–h). As with plasmids and ISs, the widespread expansion of Siphoviridae prophages probably resulted from a single acquisition event within O2v1:KL64 (Fig. 4d).
Emergence of a hypervirulent population by exclusively obtaining rmpA-positive virulence plasmids drives the expansion of O2v1:KL64
To evaluate the potential pathogenesis of O2v1:KL64 and OL101:KL47, 154 experimentally validated virulence factors (VFs) of K. pneumoniae were analyzed (see methods). O2v1:KL64 carried significantly more virulence determinants than OL101:KL47 (median 97 vs 85) (p =
= 2.2
2.2 ×
× 10−16 by Wilcoxon rank-sum test) (Supplementary Fig. 7). A set of key VFs (i.e., iucABCD, terABCDEZ, peg-344, rmpADC, and rmpA2) associated with hypervirulence and typically mobilized by virulence plasmids8,14 mainly contributed to the inter-subclonal differences (Supplementary Dataset 3), and their proportions were significantly higher in O2v1:KL64 (56.9–71.1%) than in OL101:KL47 (0–41.1%) (p
10−16 by Wilcoxon rank-sum test) (Supplementary Fig. 7). A set of key VFs (i.e., iucABCD, terABCDEZ, peg-344, rmpADC, and rmpA2) associated with hypervirulence and typically mobilized by virulence plasmids8,14 mainly contributed to the inter-subclonal differences (Supplementary Dataset 3), and their proportions were significantly higher in O2v1:KL64 (56.9–71.1%) than in OL101:KL47 (0–41.1%) (p ≤
≤ 2.82
2.82 ×
× 10−9 by Chi-square test for each pairwise comparison). Notably, rmpADC was exclusively carried by O2v1:KL64 with a rate of 56.9% (240/422). Frame-shifted rmpA and incomplete rmpADC were detected in 21.3% (51/240) and 9.2% (22/240) rmpADC-positive O2v1:KL64 isolates, respectively. While rmpA2 was found in OL101:KL47 (74/192) and O2v1:KL64 (290/422), frame-shifted rmpA2 was detected in 67.6 and 98.6% of rmpA2-positive OL101:KL47 (50/74) and O2v1:KL64 (286/290) isolates, respectively. This is similar to our previous observation from single-center data4. Since rmpA/A2 is frequently used as the indicator of virulence plasmids, we here simply defined the rmpA/A2-positive isolates as hvKP. The O2v1:KL64-hvKP isolates emerged in 2015 and were detected in nine provinces. The proportion of O2v1:KL64-hvKP among O2v1:KL64 and CRKP-ST11 dramatically increased from 0% in 2014 to 85.9% (158/184) and 69.9% (158/226) in 2019 (Supplementary Fig. 8), respectively, suggesting that the expansion of O2v1:KL64 was associated with an increase in the size of the hvKP population.
10−9 by Chi-square test for each pairwise comparison). Notably, rmpADC was exclusively carried by O2v1:KL64 with a rate of 56.9% (240/422). Frame-shifted rmpA and incomplete rmpADC were detected in 21.3% (51/240) and 9.2% (22/240) rmpADC-positive O2v1:KL64 isolates, respectively. While rmpA2 was found in OL101:KL47 (74/192) and O2v1:KL64 (290/422), frame-shifted rmpA2 was detected in 67.6 and 98.6% of rmpA2-positive OL101:KL47 (50/74) and O2v1:KL64 (286/290) isolates, respectively. This is similar to our previous observation from single-center data4. Since rmpA/A2 is frequently used as the indicator of virulence plasmids, we here simply defined the rmpA/A2-positive isolates as hvKP. The O2v1:KL64-hvKP isolates emerged in 2015 and were detected in nine provinces. The proportion of O2v1:KL64-hvKP among O2v1:KL64 and CRKP-ST11 dramatically increased from 0% in 2014 to 85.9% (158/184) and 69.9% (158/226) in 2019 (Supplementary Fig. 8), respectively, suggesting that the expansion of O2v1:KL64 was associated with an increase in the size of the hvKP population.
To confirm the existence of virulence plasmids in ST11, reads of the 646 ST11 genomes were mapped to two representative virulence plasmids pVir-KP16932 (carried by an ST11-OL101:KL47 isolate) and pVir-KP47434 (carried by an ST11 O2v1:KL64 isolate) reported in our previous study4, and the presence of a virulence plasmid was inferred if the coverage was ≥40% of the reference. We identified 400 isolates (61.9%) which might carry a virulence plasmid (Supplementary Dataset 4). Of these, 33 isolates (13 OL101:KL47 and 20 O2v1:KL64) with mapping coverage ranging between 40–100% were randomly selected for long-read sequencing to examine the diversity of virulence plasmids (Supplementary Dataset 5). The rmpA/A2 genes were detected on the chromosome of 3 OL101:KL47 isolates, and on a putative virulence plasmid in each of 30 isolates, ranging in size from 101.5 to 305.5 kb (Supplementary Dataset 6). The 30 putative virulence plasmids were typed as IncFIB-HIB (n
kb (Supplementary Dataset 6). The 30 putative virulence plasmids were typed as IncFIB-HIB (n =
= 25), IncFIB (n
25), IncFIB (n =
= 2), IncFII-FIB-R (n
2), IncFII-FIB-R (n =
= 2), and untypeable (n
2), and untypeable (n =
= 1), and were grouped into four clusters by MOB-suite15 with AA406 as the predominant cluster (Supplementary Dataset 6). Of these, 13 plasmids shared a relatively conserved backbone (75.5–100% coverage), another 10 with a smaller size could be derived from them or vice versa by gain or loss of genes (67.3–100% coverage), and the other seven were resistance-virulence fusion plasmids carrying 1–10 antimicrobial resistance genes (ARGs) with a lower coverage to the virulence plasmid references (≤60%) (Supplementary Dataset 6 and Supplementary Fig. 9). Mapping the short sequence reads of 389 rmpA/A2-positive ST11 isolates to the 30 putative virulence plasmid sequences identified 347 (89.2%) showing ≥90% coverage to a circularized 107.1-kb IncFIB plasmid pVir-KP115906 which yielded the highest number of matches. These data indicate that most rmpA/A2-positive isolates harbored virulence plasmids. Comparing genome phylogenetic positions and plasmid sequence similarities indicated both horizontal and vertical modes of virulence plasmid transmission among OL101:KL47 and O2v1:KL64 (Supplementary Fig. 9).
1), and were grouped into four clusters by MOB-suite15 with AA406 as the predominant cluster (Supplementary Dataset 6). Of these, 13 plasmids shared a relatively conserved backbone (75.5–100% coverage), another 10 with a smaller size could be derived from them or vice versa by gain or loss of genes (67.3–100% coverage), and the other seven were resistance-virulence fusion plasmids carrying 1–10 antimicrobial resistance genes (ARGs) with a lower coverage to the virulence plasmid references (≤60%) (Supplementary Dataset 6 and Supplementary Fig. 9). Mapping the short sequence reads of 389 rmpA/A2-positive ST11 isolates to the 30 putative virulence plasmid sequences identified 347 (89.2%) showing ≥90% coverage to a circularized 107.1-kb IncFIB plasmid pVir-KP115906 which yielded the highest number of matches. These data indicate that most rmpA/A2-positive isolates harbored virulence plasmids. Comparing genome phylogenetic positions and plasmid sequence similarities indicated both horizontal and vertical modes of virulence plasmid transmission among OL101:KL47 and O2v1:KL64 (Supplementary Fig. 9).
Virulence plasmids are associated with significantly enhanced resistance to phagocytosis in O2v1:KL64
It is known that virulence plasmids can promote the pathogenicity of K. pneumoniae; we here measured phagocytosis to evaluate the pathogenicity of isolates w/o virulence plasmids. Isolates of each subclone were grouped by the presence of rmpA/A2 (the indicator of virulence plasmids), and three isolates were randomly selected for each group in the test. Indeed, compared with those without virulence plasmids, rmpA/A2-positive isolates of both subclones showed enhanced resistance to phagocytosis, but it was only significant for O2v1:KL64 (mean phagocytosis 0.017 ±
± 0.023% vs 0.2
0.023% vs 0.2 ±
± 0.049%; p
0.049%; p =
= 0.0043 by two-sided t-test) (Fig. 5a).
0.0043 by two-sided t-test) (Fig. 5a).
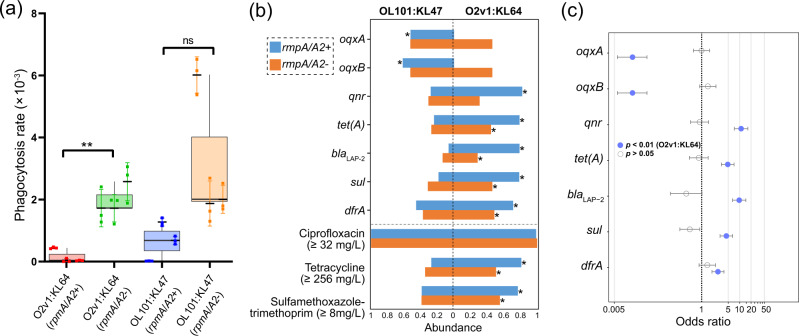
a Comparison of phagocytosis resistance for isolates w/o virulence plasmids (indicated by the presence of rmpA/A2). Three isolates were randomly selected for each group in the test, i.e., O2v1:KL64-rmpA/A2 +
+ (KP33367, KP47434, and KP66639), O2v1:KL64-rmpA/A2- (KP33316, KP37485, and KP39199), OL101:KL47-rmpA/A2
(KP33367, KP47434, and KP66639), O2v1:KL64-rmpA/A2- (KP33316, KP37485, and KP39199), OL101:KL47-rmpA/A2 +
+ (KP16932, KP41051, and 46882), and OL101:KL47-rmpA/A2- (KP30412, KP43350, and KP73269). The assay was triplicated, and the error bars represent standard deviations. Student’s t-tests were used for pairwise group comparisons, and rmpA/A2-positive O2v1:KL64 isolates showed significantly enhanced resistance to phagocytosis than rmpA/A2-negative O2v1:KL64 isolates (p
(KP16932, KP41051, and 46882), and OL101:KL47-rmpA/A2- (KP30412, KP43350, and KP73269). The assay was triplicated, and the error bars represent standard deviations. Student’s t-tests were used for pairwise group comparisons, and rmpA/A2-positive O2v1:KL64 isolates showed significantly enhanced resistance to phagocytosis than rmpA/A2-negative O2v1:KL64 isolates (p =
= 0.0043). Boxplots are displayed using the Tukey method (center line, median; box limits, upper and lower quartiles; whiskers, last point within a 1.5x interquartile range). ns, not significant; *p
0.0043). Boxplots are displayed using the Tukey method (center line, median; box limits, upper and lower quartiles; whiskers, last point within a 1.5x interquartile range). ns, not significant; *p <
< 0.01; b Distribution of ARGs with significant differences between OL101:KL47 and O2v1:KL64 w/o virulence plasmids. The resistance ratio of drugs (ciprofloxacin, tetracycline, and sulfamethoxazole-trimethoprim) associated with these ARGs are compared. Since the breakpoint of tetracycline is not available for K. pneumoniae, we here used MIC
0.01; b Distribution of ARGs with significant differences between OL101:KL47 and O2v1:KL64 w/o virulence plasmids. The resistance ratio of drugs (ciprofloxacin, tetracycline, and sulfamethoxazole-trimethoprim) associated with these ARGs are compared. Since the breakpoint of tetracycline is not available for K. pneumoniae, we here used MIC ≥
≥ 256
256 mg/L to represent high-level resistance. *p
mg/L to represent high-level resistance. *p <
< 0.01 (Chi-squared test). c ARGs associated with virulence plasmids (indicated by the presence of rmpA/A2) in OL101:KL47 (n
0.01 (Chi-squared test). c ARGs associated with virulence plasmids (indicated by the presence of rmpA/A2) in OL101:KL47 (n =
= 192) and O2v1:KL64 (n
192) and O2v1:KL64 (n =
= 422). Circles indicate odds ratios estimated in a single multivariable logistic regression model with all genes; lines indicate 95% confidence intervals for those odds ratios. The median was used as the measure of center for the error bars in panels a and c. All statistical tests carried out were two-sided. Source data are provided as a Source Data file.
422). Circles indicate odds ratios estimated in a single multivariable logistic regression model with all genes; lines indicate 95% confidence intervals for those odds ratios. The median was used as the measure of center for the error bars in panels a and c. All statistical tests carried out were two-sided. Source data are provided as a Source Data file.
Tetracycline and sulfamethoxazole-trimethoprim may have been involved in the selection of O2v1:KL64-hvKP
To explore whether antibiotics were involved in the subclonal selection, we analyzed acquired antibiotic resistance genes (ARGs) for both subclones. The number of acquired ARGs was comparable between O2v1:KL64 (median 11) and OL101:K47 (median 10) (p =
= 0.96 by Wilcoxon rank-sum test) (Supplementary Fig. 10). However, of these with ≥50% proportion in either subclone, the abundance of oqxAB was significantly higher in OL101:KL47 (p
0.96 by Wilcoxon rank-sum test) (Supplementary Fig. 10). However, of these with ≥50% proportion in either subclone, the abundance of oqxAB was significantly higher in OL101:KL47 (p ≤
≤ 5.69
5.69 ×
× 10−12 by Chi-square test), while that of blaLAP-2, dfrA-like, qnr-like, sul-like, and tet(A) was significantly higher in O2v1:KL64 (p
10−12 by Chi-square test), while that of blaLAP-2, dfrA-like, qnr-like, sul-like, and tet(A) was significantly higher in O2v1:KL64 (p ≤
≤ 1.23
1.23 ×
× 10−3 by Chi-square test) (Fig. 5b and Supplementary Dataset 7). A strong correlation was found between the presence of these ARGs and rmpA/A2 in O2v1:KL64 (p
10−3 by Chi-square test) (Fig. 5b and Supplementary Dataset 7). A strong correlation was found between the presence of these ARGs and rmpA/A2 in O2v1:KL64 (p <
< 2.2
2.2 ×
× 10−16), but not in OL101:KL47 (p
10−16), but not in OL101:KL47 (p ≥
≥ 0.05) (Fig. 5c). We further measured MICs of ciprofloxacin, tetracycline, and sulfamethoxazole-trimethoprim for 368 O2v1:KL64 and 140 OL101:K47 isolates. No significant differences were found for ciprofloxacin resistance between O2v1:KL64 and OL101:K47 (p
0.05) (Fig. 5c). We further measured MICs of ciprofloxacin, tetracycline, and sulfamethoxazole-trimethoprim for 368 O2v1:KL64 and 140 OL101:K47 isolates. No significant differences were found for ciprofloxacin resistance between O2v1:KL64 and OL101:K47 (p ≥
≥ 0.95 by Chi-square test) (Fig. 5b), since all isolates harbored a gyrA mutant (Asp87Gly) and a parC mutant (Ser80lle and Asn438Ser). However, the O2v1:KL64-hvKP population displayed the highest resistance rate to tetracycline and sulfamethoxazole-trimethoprim (Fig. 5b).
0.95 by Chi-square test) (Fig. 5b), since all isolates harbored a gyrA mutant (Asp87Gly) and a parC mutant (Ser80lle and Asn438Ser). However, the O2v1:KL64-hvKP population displayed the highest resistance rate to tetracycline and sulfamethoxazole-trimethoprim (Fig. 5b).
To understand how these ARGs were captured, we performed long-read sequencing for 17 isolates (14 O2v1:KL64; 3 OL101:KL47) carrying at least two of blaLAP-2, dfrA-like, qnr-like, sul-like, and tet(A) genes. These ARGs were detected on the replicon-encoding contigs of the 17 genomes, supporting that they were plasmid-borne (Supplementary Dataset 8). These putative plasmids were assigned to three Inc types (IncFII, IncFII-FIB, and IncFII-R) and IncFII was predominant (13/18). Each type of plasmid shared a conserved backbone irrespective of hosts, suggestive of inter-subclonal horizontal transfers (Supplementary Fig. 11a). Mapping the reads of OL101:KL47 and O2v1:KL64 genomes to these putative plasmids revealed that the IncFII-type plasmid was prevalent in O2v1:KL64 (266 genomes showed >90% coverage to pMDR-KP29007), especially in O2v1:KL64-hvKP (241/266), but rare in OL101:KL47 (12 genomes showed >90% coverage to pMDR-KP29007) (Supplementary Fig. 11b).
Detection of successful genotypes in O2v1:KL64
Given that different genotypes were conferred by the genetic diversity of the IncFIB-type virulence plasmids and IncFII-type MDR plasmids in O2v1:KL64 described above, we intended to identify successful genotypes in the context of the associated genes carried by these plasmids (Fig. 6). A total of 48 genotypes was detected based on various combinations of these genes. The most prevalent genotypes (genotypes 1 and 2) encode all genes but dfrA-like and/or oqxAB accounting for 47.9% (202/422) of O2v1:KL64 (Fig. 6a), and the ratio of the two genotypes in each year dramatically increased from 0% to 64.7% (119/184) between 2014 and 2019 (Fig. 6b), suggesting that both could be successful genotypes. In contrast, the third and fourth prevalent genotypes (genotypes 3 and 4) do not carry any target genes or merely encode oqxAB (Fig. 6a), and their proportion in the population decreased from the peak (63%; 17/27) in 2015 to 4.9% (9/184) in 2019 (Fig. 6b).
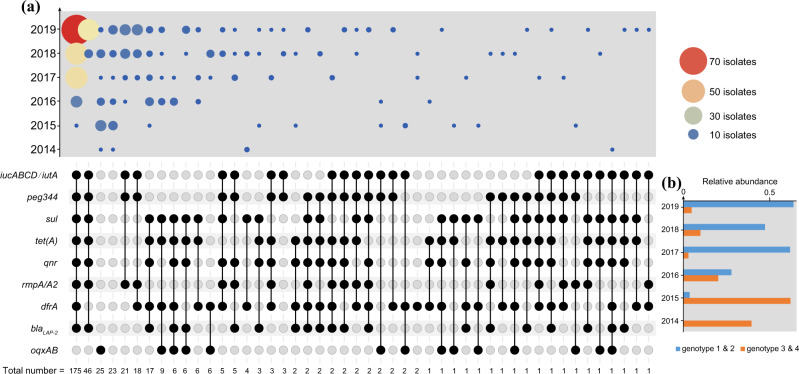
a The combination matrix (bottom) depicts predicted genotypes of O2v1:KL64. Within the combination matrix, black circles indicate the presence of genes and the vertical combination of black circles represents the genotype. The total number of each genotype is indicated below the matrix. The combination matrix was created using the UpSetR package73. The bubble plot (top) depicts the relative number of isolates with each genotype (combination matrix) per year. b The graph shows the relative abundance of genotypes 1 and 2 and genotypes 3 and 4 per year. Source data are provided as a Source Data file.
Enhanced inter-hospital transmission promotes O2v1:KL64-hvKP dissemination
To understand whether the subclonal replacement is associated with an altered transmission pattern, i.e., intra- and inter-hospital transmission, we tried to discriminate likely recent transmission events using pairwise SNP distances by year (2014–2019). We tested a range of SNP thresholds to minimize the bias possibly introduced by a single cutoff. The minimum SNP threshold was set to be 14 SNPs based on the mutation rate of our collection and the reference genome length (see methods), and the maximum was defined to be 25 SNPs based on recent regional epidemiologic studies7,16–18.
A significant transmission pattern shift was observed for O2v1:KL64 from 2015 to 2019 (2014 was excluded in the analysis due to the limited number of isolates obtained) using each threshold of 14–25 SNPs. The fraction of recent transmission within hospitals dramatically decreased from (100–89.7%) to (71.5–40.9%) for O2v1:KL64, while that between hospitals dramatically increased from (0–10.3%) to (28.5–59.1%) (p <
< 0.05 by Mann–Kendall test) (Fig. 7). Similar transmission dynamics were observed for the O2v1:KL64-hvKP population (z
0.05 by Mann–Kendall test) (Fig. 7). Similar transmission dynamics were observed for the O2v1:KL64-hvKP population (z =
= 2.02; p
2.02; p <
< 0.05 by Mann–Kendall test), but not for the rmpA/A2-negative isolates (Fig. 7). This suggests that the hypervirulent subpopulation promoted the dissemination of O2v1:KL64 through enhanced inter-hospital transmissions. Relative stability was observed in the fraction of recent transmission within ([100–98.6%]–[100–83.3%]) and between hospitals ([0–1.4%]–[0–16.7%]) for OL101:K47 from 2014 to 2019 (p
0.05 by Mann–Kendall test), but not for the rmpA/A2-negative isolates (Fig. 7). This suggests that the hypervirulent subpopulation promoted the dissemination of O2v1:KL64 through enhanced inter-hospital transmissions. Relative stability was observed in the fraction of recent transmission within ([100–98.6%]–[100–83.3%]) and between hospitals ([0–1.4%]–[0–16.7%]) for OL101:K47 from 2014 to 2019 (p >
> 0.05 by Mann–Kendall test) (Fig. 7), suggesting that the transmission pattern of OL101:K47 had no significant changes over time.
0.05 by Mann–Kendall test) (Fig. 7), suggesting that the transmission pattern of OL101:K47 had no significant changes over time.
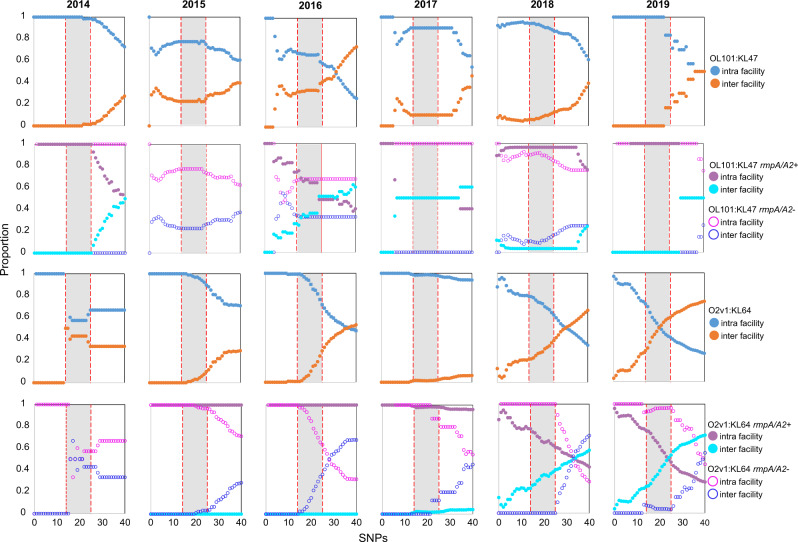
Recent intra- and inter-facility transmission pairs using pairwise single-nucleotide polymorphism (SNP) distances were identified by year. Circles indicate the proportion of pairs (y-axis) calculated by using various pairwise SNP distance thresholds (x-axis). A range of thresholds (14–25 SNPs; a gray area) were used in this study (see methods) to identify recent intra- and inter-facility transmission pairs for OL101:KL47 (the top two rows) or O2v1:KL64 (the bottom two rows). Source data are provided as a Source Data file.
Geographical epidemiology of ST11 subclones
To dissect the geographical epidemiology and evolutionary relationship of the ST11 at the subclonal level, phylogenetic analysis was performed using the 646 ST11 genomes together with 329 publicly available draft genomes of ST11 isolated in 43 countries across four continents (i.e., America, Africa, Asia, and Europe) (Supplementary Dataset 9). All but two Chinese isolates fall into a single clade, with seven isolates obtained from France (supposedly imported from China19), Canada, the United States, and Japan (Supplementary Fig. 12), suggesting that the ST11 clone evolved independently and expanded locally in China. Three O3b:KL13 isolates from the United States clustered with the Chinese clade.
Most of the global ST11 isolates (269/329) were assigned to six major sublineages (Supplementary Fig. 12), including O2v1:KL24 (n =
= 66), O2v1:KL64 (n
66), O2v1:KL64 (n =
= 21), O2v2:KL27 (n
21), O2v2:KL27 (n =
= 36), O2v2:KL105 isolates (n
36), O2v2:KL105 isolates (n =
= 73), O3:KL125 (n
73), O3:KL125 (n =
= 17) and O4:KL15 (n
17) and O4:KL15 (n =
= 56). These sublineages displayed geographic specificity: (i) O4:KL15, O2v1:K24, and O3b:KL125 as international sublineages have spread in multiple countries across ≥3 continents (n
56). These sublineages displayed geographic specificity: (i) O4:KL15, O2v1:K24, and O3b:KL125 as international sublineages have spread in multiple countries across ≥3 continents (n =
= 18 across five continents; n
18 across five continents; n =
= 19 across four continents; n
19 across four continents; n =
= 4 across three continents); (ii) O2v2:KL105 mainly circulated in Europe, especially Eastern Europe (59/73), and O2v2:KL27 isolates were mainly detected in North and South America, suggestive of two continental; (iii) O2v1:KL64 was primarily found in Brazil (18/21) as a local sublineage. Of note, the Brazil O2v1:KL64 isolates were phylogenetically distinct from that of China, indicating an independent evolution for this subclone.
4 across three continents); (ii) O2v2:KL105 mainly circulated in Europe, especially Eastern Europe (59/73), and O2v2:KL27 isolates were mainly detected in North and South America, suggestive of two continental; (iii) O2v1:KL64 was primarily found in Brazil (18/21) as a local sublineage. Of note, the Brazil O2v1:KL64 isolates were phylogenetically distinct from that of China, indicating an independent evolution for this subclone.
BEAST analysis was performed using 147 of the 975 genomes to reduce computation time (see Methods) (Supplementary Fig. 13). The correlation between root-to-tip distances and sampling time indicated a relatively clocklike pattern of molecular evolution (Supplementary Fig. 14). O2v1:KL64 was derived from OL101:KL47 around AD 2006 (95% HPD AD 2004–2009) in China, and OL101:KL47 emerged around AD 2005 (95% HPD AD 2002–2008). The most recent common ancestor (MRCA) of the global and Chinese isolates dated to about AD 1983 (95% HPD AD 1977–1989).
Discussion
The rapid expansion of CRKP globally is largely driven by a number of “highly successful” clones, including ST11. However, the drivers underpinning the successful epidemic spread remain poorly understood. Tracing the genetic and phenotypic variations of isolates spanning a wide range of time and geographies allows us to investigate the evolutionary trajectory and explore the underlying driving forces.
We previously detected a subclonal shift in CRKP-ST11 causing bloodstream infections in a tertiary hospital4. In this study, we further demonstrated the subclonal shift over a 6-year national prevalence survey. CRKP-ST11 has diversified into two major subclones (OL101:KL47 and O2v1:KL64), and OL101:KL47 was replaced in a stepwise manner by O2v1:KL64 over time. The intra-clonal segregation would occur around AD 2006 (Supplementary Fig. 13), and it was primarily due to the recombination of capsule and LPS biosynthesis loci, which have been defined as recombination hot spots subject to strong diversifying selection in K. pneumoniae8,20. From an epidemiological standpoint, it is highly interesting to pinpoint the selective pressures for the prevalence of O2v1:KL64. Consistent with our data that O2 was prevalent in ST11 and ST15, a previous study showed that the O2 serotype was dominant in CRKP (50%) in the last two decades, especially in another epidemic clone ST25821. The prevalence of O2 antigen supposedly correlates with a paucity of anti-O2 antibodies in human B cell repertoires21. Additional studies reported that patients with O2v1:KL64-CRKP BSI had a significantly higher 30-day mortality rate and a higher sepsis/septic shock incidence rate4,22. These suggest that the emergence of O2v1:KL64 is associated with host susceptibility resulting in enhanced pathogenicity by evasion of innate host defense. Hence, the identified subclonal shift within CRKP-ST11 is likely to cause challenges to the current infection control measurements and treatment strategies.
Clonal replacement has been reported in multiple notorious MDR pathogens, and one of the more well-known examples is methicillin-resistant Staphylococcus aureus (MRSA)23,24. Evolved resistance and virulence-associated with a set of genetic alterations have been linked to the clonal replacement of MRSA25–27. In this study, we revealed that the epidemic success of O2v1:KL64 is associated with the expansion of a hypervirulent lineage with the capture of a virulence plasmid. The emergent O2v1:KL64-hvKP isolates have been sporadically reported in several surveillance surveys28,29; however, none of them has systematically investigated the epidemiological and evolutionary characterizations of the lineage. Numerous studies have demonstrated that virulence plasmids can promote the pathogenicity of K. pneumoniae30–32. Indeed, we here found that the O2v1:KL64-hvKP obtained enhanced phagocytosis resistance compared with those isolates without virulence plasmids. Our previous study showed that virulence plasmids promoted pathogen invasion and subsequent clinical infection, and O2v1:KL64-hvKP displayed enhanced resistance to neutrophil killing4. Together, their data confirm that O2v1:KL64-hvKP has evolved to be more virulent through capturing virulence plasmids. The emergence of O2v1:KL64-hvKP is additionally associated with the capture of MDR plasmids. A strong correlation was found between five ARGs [i.e., blaLAP-2, dfrA-like, qnr-like, sul-like, and tet(A)] and O2v1:KL64-hvKP but not OL101:KL47 (Fig. 5c), which is due to the enrichment of an IncFII MDR plasmid. Compared with the other subpopulations, the O2v1:KL64-hvKP displayed the highest resistance to tetracycline and sulfamethoxazole-trimethoprim (Fig. 5b), suggesting that these two drugs might have been involved in the prevalence of O2v1:KL64-hvKP. O2v1:KL64 and OL101:KL47 showed comparable resistance to ciprofloxacin due to mutations in gyrA or parC, while additional loss and gain of oqxAB and qnr-like genes, respectively, was found in O2v1:KL64. Of note, oqxAB have widely been considered to be core genes of K. pneumoniae6, but our results showed that they were lost in most of the O2v1:KL64 isolates, possibly by IS-mediated and/or recombination mechanisms (Supplementary Fig. 15). As a multidrug efflux pump, OqxAB confers low to intermediate resistance to several antibiotics (e.g., quinoxalines, quinolones, tigecycline, and nitrofurantoin), detergents and disinfectants. Loss of OqxAB may affect the drug resistance of O2v1:KL64. Whether such a loss could confer evolutionary advantages to the epidemic success needs to be studied further.
In bacteria, recombination, horizontal gene transfer, and mutations are recognized as major sources of the genetic variations introduced into a population. As found in other prevalent MDR clones (e.g., ST258 and ST15)8, the genomes of ST11 have been shaped by frequent recombination events. In particular, our analysis suggested that the contribution of recombination to the genetic variations was higher in O2v1:KL64 than in OL101:KL47, and we further demonstrated that a point mutation occurring in recC of O2v1:KL64 conferred more recombination proficiency, which was unique to O2v1:KL64 isolated in China. It is known that recC, together with recB and recD, encodes an ATP-dependent nuclease, called RecBCD enzyme, and the RecBCD-dependent pathway is the primary mechanism of homologous recombination and repair of linear double-strand DNA in E. coli. The structure and function of the RecBCD enzyme is regulated by Chi sites (5′-GCTGGTGG-3′) to stimulate recombination33. Current evidence suggests that the RecC subunit recognizes Chi in the 3′ tunnel34, and a 35-kDa C-terminal domain of RecC is required for interaction with the RecD protein, a prerequisite for responsiveness to Chi35. Point mutations in the C-terminal domain of RecC indirectly prevent RecD from associating with RecBC35, resulting in the “double-dagger” phenotype: recombination proficiency that is independent of Chi and the absence of nuclease activities36. Of note, the point mutation (His935Arg) occurring in RecC of O2v1:KL64 is located in the C-terminal domain; we, therefore, infer that it may affect the interaction with the RecD and responsiveness to Chi to stimulate recombination. Further, It was shown that mutations that inactivate the recB or recC gene lead to defects in multiple biological function, including conjugational, transductional, and phage recombination; a loss of SOS induction; sensitivity to DNA-damaging agents that cause DSBs; and low cell viability37. We, therefore, propose that the O2v1:KL64 population carrying the recC mutation had become more diverse through more frequent recombination and by capturing more MGEs as detected in this study, and O2v1:KL64-hvKP was selected for and become prevalent in a short time scale.
In addition, horizontal gene transfer was identified as another driving force for the diversification in ST11, since a significantly higher load of MGEs, including plasmids, ISs, and prophages, was detected in O2v1:KL64 compared to OL101:KL47 (Supplementary Fig. 5a–d). It is known that phage-induced selective pressures play a critical role in the population diversity of bacteria13, and we found that the prophage load was significantly higher in O2v1:KL64 than in OL101:KL47 due to multiple gain and loss events (Fig. 4c). These findings suggest that the two subclones might have been exposed heterogeneously to different types of phages. In particular, our analysis pinpoints that Siphoviridae prophages contributed significantly to the high prophage load in O2v1:KL64, which probably resulted from a single acquisition event through the vertical model (Fig. 4d). Similarly, the large-scale expansion of plasmids and ISs within O2v1:KL64 was also linked to a single acquisition event followed by vertical inheritance (Fig. 4b, c). The vertical transmission of these MGEs suggests that they may have conferred evolutionary advantages to O2v1:KL64, which could be further supported by the identified “successful” genotypes carrying these MGEs (Fig. 6). Given that ST11 genomes harbor more MGEs than non-ST11 in our collection (Supplementary Fig. 6), we propose that accumulation of prophages and plasmids could be one of the vital factors for the epidemic success of successful clones. Despite the benefits that cargo genes (e.g., AMRs) carried by MGEs can provide, the introduction of novel MGEs in a pre-existing, well-tuned genetic background would incur a fitness cost, and the maintenance of MGEs in host cells requires a balance of the costs and benefits to the host38, e.g., minimized over time by selection39. It would be interesting to explore the underlying mechanisms employed by O2v1:KL64 to fine-tune the fitness costs introduced by these MGEs. Additionally, future studies should involve examining the biological function of these genetic elements to understand their role in the population-level success of O2v1:KL64.
Of greater concern, using an SNP-based transmission tracking method, we revealed that the prevalence of O2v1:KL64-hvKP was driven by an altered transmission pattern. The accuracy of SNP-based transmission tracking methods has been recently evidenced by numerous studies using large datasets for various pathogens, like MRSA and CRKP7,16,40. In particular, we here used a range of SNP cutoffs to avoid any bias that could be caused by a single cutoff. Indeed, all SNP cutoffs used in our analysis generated a consistent transmission trend, demonstrating the reliability and validity of our results. The spread of O2v1:KL64-hvKP was mainly driven by an intra-hospital transmission before 2018, which could be attributed to evolutionary advantages conferred by a set of genetic alterations as identified here. With the increasing size of O2v1:KL64-hvKP over time, inter-hospital patient transfers may have further facilitated the spread of the subpopulation across the country, leading to a subsequent switch to inter-hospital transmission. More metadata is needed to uncover the reasons for changes in transmission mode in the future. Our findings highlight the necessity of tailoring the current infection control measures (e.g., active screening of inter-hospital transferred patients with a history of CRKP) to prevent the dissemination of O2v1:KL64-hvKP in China.
In summary, we have shown here that subclonal replacement within CRKP-ST11 has been driven by the expansion of O2v1:KL64 within a 6-year period in China. The epidemic success of O2v1:KL64 is associated with the emergence and dissemination of a subpopulation associated with a repertoire of genetic alterations, and of greater concern, with the enhanced inter-hospital transmission. Collectively, our study highlights that public health efforts should focus on genomic surveillance to identify high-risk clones and subclonal expansions early in the course of an epidemic to potentiate targeted control strategies.
Methods
Dataset
A total of 4635 non-duplicate isolates were collected in the framework of national surveillance for blood isolates (Blood Bacterial Resistant Investigation Collaborative System, BRICS) between January 2014 and December 2019 in China (Fig. 1a). Only the first blood isolate of each species per patient was eligible over the full study period. All participating hospitals sent their isolates to the central laboratory quarterly. Species identification was performed by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF/MS) (Bruker Daltonik GmbH, Bremen, Germany). The increase in the number of isolates over time was partly due to improvements in quality control by participating hospitals during the surveillance period. The sample collection protocol was approved by the institutional review board of the First Affiliated Hospital of Zhejiang University in China.
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was initially performed using a VITEK-2 system (bioMérieux, Lyon, France) in the sentinel hospitals and was further confirmed by the agar dilution and/or broth microdilution method in our laboratory. Results were interpreted according to the Clinical and Laboratory Standards Institute41 and European Committee on Antimicrobial Susceptibility Testing v.10.0 (http://www.eucast.org/clinical_breakpoints/). Carbapenem resistance was defined as a minimum inhibitory concentration (MIC) of ≥4 mg/L for imipenem or meropenem.
mg/L for imipenem or meropenem.
Whole-genome sequencing and quality control analysis
Genomic DNA from 794 CRKP isolates was extracted using Gentra Puregene Yeast/Bact. Kit (Qiagen, San Francisco/Bay Area, CA, USA). The genomes were sequenced using an Illumina Novaseq 6000 system (Illumina, San Diego, United States) with 2 ×
× 150-bp paired-end libraries. Raw reads were trimmed using Trimmomatic v0.3342 and then assembled using SPAdes v3.12.043. We performed long-read sequencing on representative isolates using a Nanopore PromethION platform (Nanopore, Oxford, UK) following a 10-Kbp library protocol. A hybrid assembly was generated by using Unicycler 0.4.044 with short and long reads. QUAST v4.6.045 was used to generate assembly statistics. Species were determined using FastANI v1.33 (https://github.com/ParBLiSS/FastANI), with a cut-off of 95%. The assemblies were annotated using Prokka v1.14.646.
150-bp paired-end libraries. Raw reads were trimmed using Trimmomatic v0.3342 and then assembled using SPAdes v3.12.043. We performed long-read sequencing on representative isolates using a Nanopore PromethION platform (Nanopore, Oxford, UK) following a 10-Kbp library protocol. A hybrid assembly was generated by using Unicycler 0.4.044 with short and long reads. QUAST v4.6.045 was used to generate assembly statistics. Species were determined using FastANI v1.33 (https://github.com/ParBLiSS/FastANI), with a cut-off of 95%. The assemblies were annotated using Prokka v1.14.646.
Identification of STs and K/O-type
The STs were assigned using Kleborate v2.0.147, and the K/O-type was determined using Kaptive v1.048 from the de novo assembly.
Identification of ARGs, VFs, Inc-type, and MGEs
ARGs were detected using Abricate v1.0.1 (https://github.com/tseemann/abricate) with the ARG database ResFinder v4.049. The VFs of K. pneumoniae were downloaded from the K. pneumoniae BIGSdb50 and Virulence Factor Database 2019 (VFDB)51, and the presence of VFs were detected using BLASTp v2.6.0 (identity ≥70%) with the custom VF database containing 154 VF genes (Supplementary Dataset 3). Replicon typing was performed using Abricate v1.0.1 with the PlasmidFinder database52. The presence of integrons was detected using IntegronFinder v1.5.153. IS copy numbers were estimated with the TPM calling function of TPMCalculator v0.0.354 and corrected by the TPM of gapA (a housekeeping gene). The prophages were detected and classified using phigaro v2.2.655. The ancestral state of each MGEs was reconstructed with maximum likelihood using the fastAnc function in the R package phytools v.0.4-9856.
Recombination detection
Recombination analysis was performed using Gubbins v2.257. The Gubbins output files were used to calculate r/m and mean recombination counts per base, calculated over non-overlapping 1000 bp windows. Pairwise nucleotide divergence between subclone-specific core-genome regions was calculated for each pair of genomes within a subclone before and after the removal of putative recombinant regions.
bp windows. Pairwise nucleotide divergence between subclone-specific core-genome regions was calculated for each pair of genomes within a subclone before and after the removal of putative recombinant regions.
Knockout, replacement, and complementation of recC
A representative O2v1:KL64 isolate KP37485 was used for the genetic manipulation. All primers used in this study were listed in Supplementary Dataset 10. For the knockout construction, the recC-spacer DNA fragment was cloned into a pSGKP-apr vector58, and the synthetic oligonucleotide with 45 nt for each homology extension of the target gene was used as a donor template. Both the pSGKP-recC-spacer plasmid and the donor template DNA were transformed into pCasKP-harboring KP37485 by electroporation, and the integration was selected on LB plates containing 5% sucrose at 37
nt for each homology extension of the target gene was used as a donor template. Both the pSGKP-recC-spacer plasmid and the donor template DNA were transformed into pCasKP-harboring KP37485 by electroporation, and the integration was selected on LB plates containing 5% sucrose at 37 °C. For the gene replacement, a linear fragment containing a cat gene with its native promoter from plasmid pKD359 between the 45
°C. For the gene replacement, a linear fragment containing a cat gene with its native promoter from plasmid pKD359 between the 45 nt each homology extension of recC was amplified and used as a donor template, and the resulting KP37485-recC::cat-pCasKP was selected on LB plates containing 5% sucrose plus 25
nt each homology extension of recC was amplified and used as a donor template, and the resulting KP37485-recC::cat-pCasKP was selected on LB plates containing 5% sucrose plus 25 mg/L chloramphenicol and 30
mg/L chloramphenicol and 30 mg/L apramycin at 30
mg/L apramycin at 30 °C. The synthetic oligonucleotide with recCOL101:KL47 as well as its 45
°C. The synthetic oligonucleotide with recCOL101:KL47 as well as its 45 nt each homology extension was used as the donor template and were transformed into KP37485-recC::cat-pCasKP with pSGKP-cat-spacer plasmid. The integration was selected as described in knockout construction, in addition, to being selected by chloramphenicol sensitivity. For the complementation, genes were amplified by PCR and cloned into vector pBAD3360. The resulting plasmids were introduced into kp37485ΔrecC via electroporation. PCR and DNA sequencing were used to confirm the final constructions.
nt each homology extension was used as the donor template and were transformed into KP37485-recC::cat-pCasKP with pSGKP-cat-spacer plasmid. The integration was selected as described in knockout construction, in addition, to being selected by chloramphenicol sensitivity. For the complementation, genes were amplified by PCR and cloned into vector pBAD3360. The resulting plasmids were introduced into kp37485ΔrecC via electroporation. PCR and DNA sequencing were used to confirm the final constructions.
Mitomycin C resistance assay
Recombinational repair of DNA damage mediated by the Rec-dependent pathway is known to be a primary strategy to protect bacteria from DNA-damaging agents (e.g., mitomycin C, ethidium bromide, and UV); therefore, these agents have been used extensively as indicators of recombination proficiency11,35,61. Mitomycin C resistance was assessed as previously described with slight modifications61. K. pneumoniae isolates were grown overnight in LB broth and inoculated into the fresh broth with indicated agents. Strains harboring pBAD33 and its derivative plasmids were grown in LB broth with 0.2% (w/v) l-arabinose and 25 mg/L chloramphenicol. The bacteria were harvested at the late logarithmic phase and suspended in phosphate-buffered saline (PBS), to 5
mg/L chloramphenicol. The bacteria were harvested at the late logarithmic phase and suspended in phosphate-buffered saline (PBS), to 5 ×
× 108 colony-forming units (cfu) per milliliter. Cell suspensions were treated with mitomycin C at indicated concentrations for 1 and 3
108 colony-forming units (cfu) per milliliter. Cell suspensions were treated with mitomycin C at indicated concentrations for 1 and 3 h, serially diluted in PBS, spread on LB plates, and incubated overnight at 37
h, serially diluted in PBS, spread on LB plates, and incubated overnight at 37 °C. Bacterial treated with PBS was used as the negative control. The survival ratio was calculated as follows: (CFU of mitomycin C treatment culture/CFU of PBS-treated culture)
°C. Bacterial treated with PBS was used as the negative control. The survival ratio was calculated as follows: (CFU of mitomycin C treatment culture/CFU of PBS-treated culture) ×
× 100%.
100%.
Recombination assays
The suicide vector pRE118, carrying the upstream and downstream fragment of blaKPC-2 of the KP37485 and an apramycin resistance gene apmR, was generated and electroporated into tested hosts. Recombinants were selected on 50 mg/L apramycin-containing plates and further confirmed by PCR. Recombination frequency was calculated as the number of recombinants/the number of recipients.
mg/L apramycin-containing plates and further confirmed by PCR. Recombination frequency was calculated as the number of recombinants/the number of recipients.
Phagocytosis assay
Phagocytosis assay was performed as previously described in ref. 62. In brief, THP-1 cells were differentiated at 1 ×
× 106 cells/well in a 12-well plate. Bacteria in the mid-log phase were harvested by centrifugation (5
106 cells/well in a 12-well plate. Bacteria in the mid-log phase were harvested by centrifugation (5 min, 6000 rpm, 24
min, 6000 rpm, 24 ˚C), resuspended in 1×PBS, and adjusted to 5
˚C), resuspended in 1×PBS, and adjusted to 5 ×
× 108 CFU/mL. Infections were performed using a multiplicity of infection (MOI) of 50 bacteria per cell. To synchronize the infection, plates were centrifuged at 200×g for 5
108 CFU/mL. Infections were performed using a multiplicity of infection (MOI) of 50 bacteria per cell. To synchronize the infection, plates were centrifuged at 200×g for 5 min and incubated at 37
min and incubated at 37 °C in a humidified 5% CO2 atmosphere. After 1
°C in a humidified 5% CO2 atmosphere. After 1 h of contact, cells were washed twice with PBS and cultured with RPMI 1640 containing 10% FBS and gentamicin (100
h of contact, cells were washed twice with PBS and cultured with RPMI 1640 containing 10% FBS and gentamicin (100 mg/L). To determine the bacterial load in the cell, the cells were washed twice with PBS and lysed with 0.5% saponin in PBS for 10
mg/L). To determine the bacterial load in the cell, the cells were washed twice with PBS and lysed with 0.5% saponin in PBS for 10 min at room temperature. Serial dilutions were plated on LB to quantify the number of intracellular bacteria. All experiments were carried out with triplicate samples on at least three independent occasions.
min at room temperature. Serial dilutions were plated on LB to quantify the number of intracellular bacteria. All experiments were carried out with triplicate samples on at least three independent occasions.
Plasmid analysis
Short-read assemblies were blasted against reference plasmids using BLASTn v2.9.063 to determine the length of the reference plasmid sequence present across isolates. Replicon typing and clustering were performed using MOB-suite15. Representative plasmids were circularized using PCR and Sanger sequencing. The Artemis Comparison Tool v13.0.064 and/or BRIG65 was used to compare and visualize structural variation between two or more sequences. The heatmap showing the percentage of aligned regions between pairs of virulence plasmids was generated using the “pheatmap” package (v1.0.12) in R v4.1.1 (https://www.r-project.org/).
Phylogenetic analysis of Chinese ST11 isolates collected in this study
Trimmed sequencing reads of 646 ST11 isolates collected in this study were mapped to a K. pneumoniae ST11 reference genome KP16932 (accession no. QVAN00000000)4 using BWA mem 62 v0.7.10-r789 (default parameters). Mapped reads were then cleaned and sorted using the SAMtools suite v1.766. Reads were realigned against the reference using GATK v3.767 by creating targets for realignment (RealignerTargetCreator) and performing realignment (IndelRealigner). Removal of optical duplicates was completed using Picard v2.10.1-SNAPSHOT (https://broadinstitute.github.io/picard/). Sequence variants were called using Bcftools v1.9-80 (http://samtools.github.io/bcftools) to generate a reference-based pseudogenome for each genome with greater than 10× depth. High-quality pseudogenomes were concatenated (plasmid sequences excluded) before Gubbins v2.257 was used to remove recombinant regions and invariable sites. Forty ST258 genomes (indicated by the triangle) retrieved from GenBank were included to establish the root of the ST11 tree. The resultant multiple sequence alignment of reference-based pseudogenomes (4460 variant sites) was used to infer a maximum-likelihood phylogeny using RAxML-ng v0.6.068 with 100 bootstrap replicates to assess support.
Phylogenetic and BEAST analysis of a global collection of ST11 isolates
All available genomes of ST11 (n =
= 329) in GenBank retrieved as of March 1, 2021, were included in this analysis (Supplementary Dataset 9). Snippy v4.6.0 (https://github.com/tseemann/snippy) was used to align the 975 genomes to the reference genome KP16932 to generate the alignment of core-genome SNPs. SNPs located in recombination regions were detected by Gubbins v2.257. The resultant recombination-free core-genome SNPs (3027 variant sites) were used to infer a maximum-likelihood phylogeny using RAxML-ng v0.6.068 with a GTR model and gamma correction, and 100 bootstrap replicates were performed to assess support. A chronogram was produced using Bayesian phylogenetic inference. To reduce computation time, 147 genomes, including all KLs, were chosen for the analysis. Analysis of temporal molecular evolutionary signals for the dataset was conducted using TempEst v1.569. A recombination-free core-genome alignment (1995 SNPs) was created using Snippy v4.6.0. BEAST v1.10.470 was used to create and execute three independent chains of length 250,000,000 with 10% burn-in, logging every 25,000 and accounting for invariant sites. We included the prior assumptions of a coalescent Bayesian skyline model for population growth, and a relaxed log normal clock rate to account for rate heterogeneity amongst branches. Convergence of the Markov chain Monte Carlo (MCMC) chain was inspected in Tracer v1.7.271, with all parameter effective sampling sizes being >200. The maximum clade credibility (MCC) tree under each model was generated in TreeAnnotator and plotted in FigTree v1.4.4 (https://github.com/rambaut/figtree).
329) in GenBank retrieved as of March 1, 2021, were included in this analysis (Supplementary Dataset 9). Snippy v4.6.0 (https://github.com/tseemann/snippy) was used to align the 975 genomes to the reference genome KP16932 to generate the alignment of core-genome SNPs. SNPs located in recombination regions were detected by Gubbins v2.257. The resultant recombination-free core-genome SNPs (3027 variant sites) were used to infer a maximum-likelihood phylogeny using RAxML-ng v0.6.068 with a GTR model and gamma correction, and 100 bootstrap replicates were performed to assess support. A chronogram was produced using Bayesian phylogenetic inference. To reduce computation time, 147 genomes, including all KLs, were chosen for the analysis. Analysis of temporal molecular evolutionary signals for the dataset was conducted using TempEst v1.569. A recombination-free core-genome alignment (1995 SNPs) was created using Snippy v4.6.0. BEAST v1.10.470 was used to create and execute three independent chains of length 250,000,000 with 10% burn-in, logging every 25,000 and accounting for invariant sites. We included the prior assumptions of a coalescent Bayesian skyline model for population growth, and a relaxed log normal clock rate to account for rate heterogeneity amongst branches. Convergence of the Markov chain Monte Carlo (MCMC) chain was inspected in Tracer v1.7.271, with all parameter effective sampling sizes being >200. The maximum clade credibility (MCC) tree under each model was generated in TreeAnnotator and plotted in FigTree v1.4.4 (https://github.com/rambaut/figtree).
Intra- and inter-facility transmission analysis
Recombination-filtered core-genome SNPs of each dataset were generated as described above to calculate the pairwise SNP distance matrices. For each pair of unique patient–facility combinations, only the most closely related isolate pair was included as the pairwise genetic distance. A range of thresholds was used here to identify recent intra- and inter-facility transmission pairs using pairwise distances. The minimum threshold was determined as 14 SNPs (2 ×
× 5,716,474
5,716,474 ×
× 1.2256
1.2256 ×
× 10−6) using reference genome length (5,716,474 base pairs) and mutation rate (1.2256
10−6) using reference genome length (5,716,474 base pairs) and mutation rate (1.2256 ×
× 10−6 mutations per base pair per year estimated in this study), and the maximum threshold was defined as 25 SNPs according to recent studies of CRKP transmission7,16–18. This analysis was performed using the regentrans package72 in R v4.1.1.
10−6 mutations per base pair per year estimated in this study), and the maximum threshold was defined as 25 SNPs according to recent studies of CRKP transmission7,16–18. This analysis was performed using the regentrans package72 in R v4.1.1.
Statistical analysis
The Wilcoxon rank-sum tests and Chi-square tests were performed for pairwise group comparisons of MGEs, VFs, ARGs, and Pearson’s Coefficient. The student’s t-tests were used for pairwise group comparisons in phenotypical assays. The Mann–Kendall test was used to test for transmission trends. P values <0.05 were considered significant. All statistical analyses were implemented in R v4.1.1.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Acknowledgements
We thank Jingjie Song and Yang Liu for their technical support of bioinformatics. We also thank Jinru Ji and Chaoqun Ying for preparing the metadata of the collection. This work was funded by the National Key R&D Program of China under award numbers 2021YFC2300300 (to K.Z. and Y.X.) and 2022YFE0103200 (to K.Z.), the National Natural Science Foundation of China under award numbers 81902030 (to T.X.), 81971984 (to Y.X.), and 82172330 (to K.Z.), China Postdoctoral Science Foundation under award number 2022M712187 (to C.-X.X.), Shenzhen Basic Research Key projects under award number JCYJ20200109144220704 (to K.Z.), Shenzhen Basic Research projects under award number JCYJ20190807144409307 (to K.Z.), the Fundamental Research Funds for the Central Universities under award number 2022ZFJH003 (to Y.X.), and Research Project of Jinan Microecological Biomedicine Shandong Laboratory under award number JNL-2022027C (to Y.X.).
Source data
Source Data(370K, xlsx)
Author contributions
K.Z., Y.X., and K.E.H. conceived the project and revised the manuscript. The BRICS Working Group collected the bacterial isolates and epidemiological data and performed preliminary laboratory analyses. K.Z., C.-X.X., P.S., Y.C., K.L.W., and M.M.C.L. performed the data analysis. T.X., S.W., J.L., H.L., and P.S. performed the experiments. K.Z. wrote the manuscript. K.Z. and Y.X. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final version of the manuscript.
Peer review
Peer review information
Nature Communications thanks the other anonymous reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Data availability
All assembled Illumina sequence data have been deposited in GenBank under the BioProject accession number PRJNA778807. Individual accession numbers are also available in Supplementary Dataset 1. Source data are provided with this paper.
Code availability
The custom code used in this study is freely available at https://github.com/xuechunxu/CRKP_ST11_KL64 (10.5281/zenodo.7804081).
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Kai Zhou, Chun-Xu Xue, Tingting Xu, Ping Shen.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Kai Zhou, Email: nc.ude.hcetsus.liam@kuohz.
Yonghong Xiao, Email: nc.ude.ujz@gnohgnoyoaix.
the BRICS Working Group:
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-38061-z.
References
Articles from Nature Communications are provided here courtesy of Nature Publishing Group
Full text links
Read article at publisher's site: https://doi.org/10.1038/s41467-023-38061-z
Read article for free, from open access legal sources, via Unpaywall:
https://www.nature.com/articles/s41467-023-38061-z.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/146827106
Article citations
Emergence of hypervirulent and carbapenem-resistant Klebsiella pneumoniae from 2014 - 2021 in Central and Eastern China: a molecular, biological, and epidemiological study.
BMC Microbiol, 24(1):465, 11 Nov 2024
Cited by: 0 articles | PMID: 39528921 | PMCID: PMC11552131
Genetic characteristics of clinical carbapenem-resistant Klebsiella pneumoniae: epidemic ST11 KPC-2-producing strains and non-negligible NDM-5-producing strains with diverse STs.
Sci Rep, 14(1):24296, 16 Oct 2024
Cited by: 0 articles | PMID: 39414846 | PMCID: PMC11484748
Genomic study substantiates the intensive care unit as a reservoir for carbapenem-resistant <i>Klebsiella pneumoniae</i> in a teaching hospital in China.
Microb Genom, 10(9), 01 Sep 2024
Cited by: 0 articles | PMID: 39325028 | PMCID: PMC11541224
Transmission Dynamics and Novel Treatments of High Risk Carbapenem-Resistant Klebsiella pneumoniae: The Lens of One Health.
Pharmaceuticals (Basel), 17(9):1206, 12 Sep 2024
Cited by: 0 articles | PMID: 39338368 | PMCID: PMC11434721
Review Free full text in Europe PMC
Phage-antibiotic synergy suppresses resistance emergence of <i>Klebsiella pneumoniae</i> by altering the evolutionary fitness.
mBio, 15(10):e0139324, 09 Sep 2024
Cited by: 0 articles | PMID: 39248568 | PMCID: PMC11481518
Go to all (12) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Nucleotide Sequences
- (1 citation) ENA - KP115906
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Recombination Drives Evolution of Carbapenem-Resistant Klebsiella pneumoniae Sequence Type 11 KL47 to KL64 in China.
Microbiol Spectr, 11(1):e0110722, 09 Jan 2023
Cited by: 9 articles | PMID: 36622219 | PMCID: PMC9927301
Characterization difference of typical KL1, KL2 and ST11-KL64 hypervirulent and carbapenem-resistant Klebsiella pneumoniae.
Drug Resist Updat, 67:100918, 03 Jan 2023
Cited by: 10 articles | PMID: 36610180
Novel Subclone of Carbapenem-Resistant Klebsiella pneumoniae Sequence Type 11 with Enhanced Virulence and Transmissibility, China.
Emerg Infect Dis, 26(2):289-297, 01 Feb 2020
Cited by: 95 articles | PMID: 31961299 | PMCID: PMC6986851
Funding
Funders who supported this work.
National Natural Science Foundation of China (3)
Grant ID: 81902030
Grant ID: 82172330
Grant ID: 81971984

 #1
#1 


