Abstract
Free full text

Acquired intra abdominal testis due to adhesions after necrotizing enterocolitis
Abstract
Undescendent testis happens usually due to the stagnation during testicular descends. Stagnation of a testicle in the abdomen may be the target of adhesions with intestinal segments. Our case report a very rare variant of acquired intra-abdominal cryptorchidism due to adhesions after necrotizing enterocolitis. Newborn baby after NEC has a significant risk of developing intraperitoneal adhesions. In this report we will describe a case of previously palpable testis in the inguinal canal at neonatal age which was pulled inside the abdomen at seventh month of age through adhesions between test and the segment of sigmoid colon after NEC.
1. Introduction
Undescendent testis (UDT) refers to the absence of the testicle in the hemiscrotum. In most cases stagnation occurs in the inguinal canal and very rarely in the abdomen where, in addition to the histopathological damage, it can become target of adhesions with intestinal segments. There have been documented some very rare reports of intestinal obstruction due to adhesions between an intra abdominal testis and the intestinal segment. In newborns, the most common cause of adhesions is necrotizing enterocolitis (NEC). Same mechanism that causes obstructive ileus as a consequence of adhesions between bowel segments, have been reported to cause obstructive ileus due to adhesions between testicular structures and bowel segments even rarely reported. Our case documents an etiological factor of acquired intra-abdominal cryptorchidism due to adhesions after NEC. We have reviewed the literature and to our knowledge this is first case reporting adhesions due to NEC causing acquired intra-abdominal testis.
2. Case
Here we describe a case of a testis previously palpated in the inguinal canal at neonatal age which had retracted in the abdomen after seven months of age due to adhesions between the testis and the sigmoid colon segment after NEC. He was operated at neonatal age because of complicated NEC. An ileostomy was performed, which was closed three months later. At the time of the first operation when the ileostomy was performed as well as three months later when the ileostomy was closed, the presence of the testis was noted in the inguinal canal, while many adhesions between intestinal segments were released. After closure of the ileostomy, he was followed in our outpatient clinic every 2 months, for the left UDT with ultrasound and physical examination. At the first outpatient visit at five months of age, the left hemiscrotum showed the absence of testicle which was slightly smaller than the right testicle and was evident in the inguinal canal. At the second visit, two months later, it was evidenced that the left testis has retrieved into the internal inguinal orifice and it was not able to pull it near the neck of the left hemiscrotum, as it was possible in the previous visit. At the third visit when the child was nine months old, we could not palpate the testis in the inguinal canal. On ultrasound it was found to be close to the internal inguinal orifice what also was confirmed with pelvic MRI (Fig. 1).
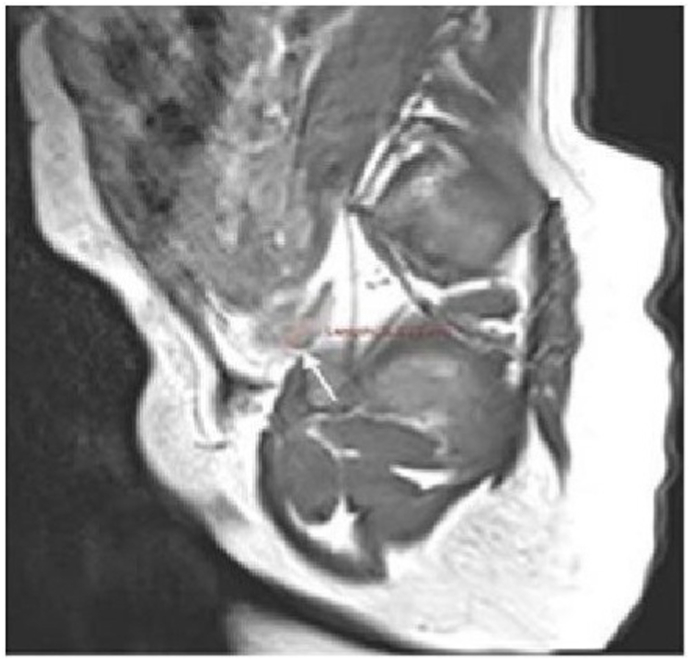
MRI of the pelvic demonstrated the presence of left testis in the pelvis, near the left inguinal canal.
The child was scheduled two months later for laparoscopic exploration. Lower pol of testis was found to be attached by adhesions to the loop of the sigmoid colon (Fig. 2).

Intra operative picture during laparoscopy demonstrates in the upper part of the picture the presence of testis attached with adhesions in the sigmoid loop shown on the lower part of the picture.
Adhesions and peritoneal attachments were released to gain length and the testis was brought to the neck of the hemiscrotum with slight tension where it was attached. Patient was discharged the following day. Five months after laparoscopic orchiopexy, the testis remains in the neck of the left hemiscrotum with good vascularization but with very small progressive development (10 × 6 millimeters) compared to the contra lateral testis (11.5 × 7.1 mm) (Fig. 3).
3. Discussion
NEC is often source of adhesions which usually occur between bowel segments and with surrounding intra peritoneal structures also. UDT can be target of these adhesions while still intra abdominally but adhesions have not been prescribed to because of acquired intra-abdominal testis as occurred in our case. Referring our case, testis while being near to internal ring when is still in the inguinal canal it can become a target of adhesions. On the other hand, UDT is associated with increased risk for torsion, trauma, infertility, malignancy and has the psychological impact of an absent testis later on adulthood also.1,2 Also, acquired cryptorchidism as well as congenital UDT is at risk for developing the same adverse histological changes seen in primary cryptorchid testes requiring surgical correction.3 Bowel obstruction has been documented to occur from adhesions between the intra-abdominal testis and bowel.4 In our case retraction of testis was due to adhesions in the sigmoid segment and clearly shows the correlation provoked by NEC and acquired intra abdominal testis. The case we have described here was positioned in the inguinal canal in the first five months, and then ascended into the abdomen due to retraction from adhesions attached to the sigmoid colon ending in the intra abdominal testis. This case highlights the importance of measures that need to be taken during adhesiolysis when a testis is in inguinal canal and can easily slide back inside the abdominal cavity and potentially becoming adherent in bowel segment due to adhesions thus potentially causing acquired intra abdominal testis. Cryptorchid testes undergo parenchymal changes if surgical correction is delayed beyond 2 years of age. Our case showed slow development and was noticed to be slightly hypo trophic. Imaging exploration of the pelvic cavity in case of unpalpable testis is mandatory especially when one was previously evidenced to be in inguinal canal since it can become torqued and atrophied or even retract intra abdominally like it happened in our case. Any neonate requiring a laparotomy has a significant risk for developing adhesions. Our case emphasizes a very rare presentation of acquired intra-abdominal testis. Further, delineates the importance of thorough intraoperative exploration of internal inguinal ring during laparotomies especially when pathologies like NEC are followed with adhesions and when a testis is in inguinal canal or even absent. However, few cases have been reported showing correlation between cryptorchidism and intestinal obstruction in children.5 Reviewing the literature, to our knowledge acquired intra abdominal testis in children caused after NEC adhesions has not been reported previously.
4. Conclusion
We think that this etiologic factor of acquired intra-abdominal testis need to be estimated and should be reported in literature in context of etiopathology of UDT. Pediatric surgeons should consider as risk factor for acquired intra-abdominal testis when a neonate or infant with inguinal testis undergoes pathologies with potentially adhesions production such as NEC and should take measures for preventing adhesions near inguinal canal as a potentially risk factor for acquired intra-abdominal testis.
References
Articles from Urology Case Reports are provided here courtesy of Elsevier
Citations & impact
Impact metrics
Article citations
Diagnoses and Treatment of Acquired Undescended Testes: A Review.
Medicine (Baltimore), 103(27):e38812, 01 Jul 2024
Cited by: 0 articles | PMID: 38968470 | PMCID: PMC11224853
Review Free full text in Europe PMC
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Avoidance of inguinal incision in laparoscopically confirmed vanishing testis syndrome.
J Urol, 166(4):1421-1424, 01 Oct 2001
Cited by: 20 articles | PMID: 11547102
Inguinal approach for the management of unilateral non-palpable testis: is diagnostic laparoscopy necessary?
J Pediatr Urol, 10(2):233-236, 16 Oct 2013
Cited by: 7 articles | PMID: 24206784
A case of peeping testis moving from the inguinal position into the abdomen.
J Surg Case Rep, 2020(3):rjaa027, 06 Mar 2020
Cited by: 0 articles | PMID: 32161639 | PMCID: PMC7059888
The role of intra-abdominal pressure in human testicular migration.
Int Braz J Urol, 47(1):36-44, 01 Jan 2021
Cited by: 5 articles | PMID: 32758302 | PMCID: PMC7712702
Review Free full text in Europe PMC





