Abstract
Background
Vaccination is an effective strategy to reduce morbidity and mortality from coronavirus disease 2019 (COVID-19). However, the uptake of COVID-19 vaccination has varied across and within countries. Switzerland has had lower levels of COVID-19 vaccination uptake in the general population than many other high-income countries. Understanding the socio-demographic factors associated with vaccination uptake can help to inform future vaccination strategies to increase uptake.Methods
We conducted a longitudinal online survey in the Swiss population, consisting of six survey waves from June to September 2021. Participants provided information on socio-demographic characteristics, history of testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), social contacts, willingness to be vaccinated, and vaccination status. We used a multivariable Poisson regression model to estimate the adjusted rate ratio (aRR) and 95% confidence intervals (CI) of COVID-19 vaccine uptake.Results
We recorded 6,758 observations from 1,884 adults. For the regression analysis, we included 3,513 observations from 1,883 participants. By September 2021, 600 (75%) of 806 study participants had received at least one vaccine dose. Participants who were older, male, and students, had a higher educational level, household income, and number of social contacts, and lived in a household with a medically vulnerable person were more likely to have received at least one vaccine dose. Female participants, those who lived in rural areas and smaller households, and people who perceived COVID-19 measures as being too strict were less likely to be vaccinated. We found no significant association between previous SARS-CoV-2 infections and vaccination uptake.Conclusions
Our results suggest that socio-demographic factors as well as individual behaviours and attitudes played an important role in COVID-19 vaccination uptake in Switzerland. Therefore, appropriate communication with the public is needed to ensure that public health interventions are accepted and implemented by the population. Tailored COVID-19 vaccination strategies in Switzerland that aim to improve uptake should target specific subgroups such as women, people from rural areas or people with lower socio-demographic status.Free full text

Socio-demographic characteristics associated with COVID-19 vaccination uptake in Switzerland: longitudinal analysis of the CoMix study
Abstract
Background
Vaccination is an effective strategy to reduce morbidity and mortality from coronavirus disease 2019 (COVID-19). However, the uptake of COVID-19 vaccination has varied across and within countries. Switzerland has had lower levels of COVID-19 vaccination uptake in the general population than many other high-income countries. Understanding the socio-demographic factors associated with vaccination uptake can help to inform future vaccination strategies to increase uptake.
Methods
We conducted a longitudinal online survey in the Swiss population, consisting of six survey waves from June to September 2021. Participants provided information on socio-demographic characteristics, history of testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), social contacts, willingness to be vaccinated, and vaccination status. We used a multivariable Poisson regression model to estimate the adjusted rate ratio (aRR) and 95% confidence intervals (CI) of COVID-19 vaccine uptake.
Results
We recorded 6,758 observations from 1,884 adults. For the regression analysis, we included 3,513 observations from 1,883 participants. By September 2021, 600 (75%) of 806 study participants had received at least one vaccine dose. Participants who were older, male, and students, had a higher educational level, household income, and number of social contacts, and lived in a household with a medically vulnerable person were more likely to have received at least one vaccine dose. Female participants, those who lived in rural areas and smaller households, and people who perceived COVID-19 measures as being too strict were less likely to be vaccinated. We found no significant association between previous SARS-CoV-2 infections and vaccination uptake.
Conclusions
Our results suggest that socio-demographic factors as well as individual behaviours and attitudes played an important role in COVID-19 vaccination uptake in Switzerland. Therefore, appropriate communication with the public is needed to ensure that public health interventions are accepted and implemented by the population. Tailored COVID-19 vaccination strategies in Switzerland that aim to improve uptake should target specific subgroups such as women, people from rural areas or people with lower socio-demographic status.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-16405-0.
Introduction
Vaccines can prevent symptomatic infections, severe disease, and death from coronavirus disease 2019 (COVID-19). The evidence of vaccine effectiveness comes from randomised clinical trials and real-world data [1, 2]. Although effective vaccines with a favourable safety profile are available against a wide range of pathogens, public confidence in vaccination has declined in some countries, and some population groups are increasingly reluctant to be vaccinated [3]. The World Health Organization (WHO) ranks vaccine hesitancy among the top ten global health threats [4]. Investigating the factors associated with vaccine hesitancy and lower vaccination uptake could help to develop strategies to minimise the impact of COVID-19 and future epidemics.
Several studies have reviewed factors that may be associated with COVID-19 vaccination uptake. A systematic review indicated that socio-demographic factors and perceptions of risk and susceptibility to COVID-19 were associated with the intention to get vaccinated and that vaccine attributes influenced vaccination intention, while receiving negative information about vaccines and working in healthcare resulted in lower intentions to get vaccinated [5]. Switzerland has had lower levels of COVID-19 vaccine uptake in the general population than many other high-income countries [6]. A prospective cohort study in Switzerland found that vaccination uptake was multifactorial and associated with socio-demographic characteristics, health status, trust in institutions, fears of side-effects and expected risk of severe COVID-19 [7]. A further understanding of how socio-demographic and behavioural factors were associated with vaccine uptake, while accounting for the age-dependent roll-out during the COVID-19 vaccination program in Switzerland, will help to improve future vaccination strategies.
The objective of this study was to analyse the association of socio-demographic and other factors with COVID-19 vaccination uptake during the roll-out of the vaccination program in the general population in Switzerland. First, we conducted an online survey with six survey waves from June to September 2021. Second, we studied vaccination uptake in the survey population using a Poisson regression model. Finally, we investigated whether the participants’ characteristics were associated with missed survey waves.
Methods
This study was conducted as part of the CoMix study, which is a longitudinal online survey about social contact patterns during the COVID-19 pandemic in more than 20 countries in Europe and is described in detail elsewhere [8, 9]. The questionnaire included socio-demographic characteristics, attitudes and practices towards public health interventions against COVID-19 and social contact behaviours. Questions about social contacts were based on the POLYMOD survey, conducted in 2008 [10].
In the longitudinal CoMix study design, a sample of the adult (≥ 18 years) Swiss population was invited by the market research company Ipsos MORI to take part in repeated survey waves. We aimed to include 1,000 participants per survey wave, who were representative of the population in Switzerland using quotas on age, gender, and region of residence. We compared the characteristics of the participants with Swiss demographic data as reported by the Federal Statistical Office (FSO) [11] and the vaccination uptake of the participants with the vaccination monitor from the Federal Office of Public Health (FOPH) [12]. We used data from six online surveys from June to September 2021 (B1-B6). Enrolment of new participants continued over the first three waves, primarily due to inconsistent participation and to ensure a sufficient sample size.
18 years) Swiss population was invited by the market research company Ipsos MORI to take part in repeated survey waves. We aimed to include 1,000 participants per survey wave, who were representative of the population in Switzerland using quotas on age, gender, and region of residence. We compared the characteristics of the participants with Swiss demographic data as reported by the Federal Statistical Office (FSO) [11] and the vaccination uptake of the participants with the vaccination monitor from the Federal Office of Public Health (FOPH) [12]. We used data from six online surveys from June to September 2021 (B1-B6). Enrolment of new participants continued over the first three waves, primarily due to inconsistent participation and to ensure a sufficient sample size.
Participants provided sociodemographic information, including age groups (categorised as 18–29, 30–39, 40–49, 50–59, 60–69, and 70 +
+ years), gender (female or male), region (urban or rural), Swiss region of residence (nomenclature of territorial units for statistics (NUTS) regions of Switzerland), country of birth (Switzerland, European Union (EU), or non-EU), educational level (low (obligatory school and vocational education), middle (high school and advanced vocational education), and high (bachelor or higher)), employment level (unemployed, student, homemaker, retired, or unemployed due to health reasons), net household income (<
years), gender (female or male), region (urban or rural), Swiss region of residence (nomenclature of territorial units for statistics (NUTS) regions of Switzerland), country of birth (Switzerland, European Union (EU), or non-EU), educational level (low (obligatory school and vocational education), middle (high school and advanced vocational education), and high (bachelor or higher)), employment level (unemployed, student, homemaker, retired, or unemployed due to health reasons), net household income (< 5,000, 5,001–10,000, or >
5,000, 5,001–10,000, or > 10,000 CHF, preferred not to answer), household size, and whether they were living in a household with a medically vulnerable individual, and testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (tested positive, tested, never tested, preferred not to answer). They also reported social contact behaviours (number of physical contacts per day), vaccination status, willingness to be vaccinated, and attitudes towards COVID-19 measures. Participation in the study was voluntary but each participant received 5 CHF per survey wave. We conducted all analyses using anonymised data in R version 4.2.1 and the code is available on GitHub: https://github.com/ISPMBern/comix. The study was approved by the ethics committee of the Canton of Bern (project number 2020–02926), all methods were performed in accordance with relevant guidelines and regulations, and informed consent of participants was obtained. We followed the STROBE Statement to report this study [13].
10,000 CHF, preferred not to answer), household size, and whether they were living in a household with a medically vulnerable individual, and testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (tested positive, tested, never tested, preferred not to answer). They also reported social contact behaviours (number of physical contacts per day), vaccination status, willingness to be vaccinated, and attitudes towards COVID-19 measures. Participation in the study was voluntary but each participant received 5 CHF per survey wave. We conducted all analyses using anonymised data in R version 4.2.1 and the code is available on GitHub: https://github.com/ISPMBern/comix. The study was approved by the ethics committee of the Canton of Bern (project number 2020–02926), all methods were performed in accordance with relevant guidelines and regulations, and informed consent of participants was obtained. We followed the STROBE Statement to report this study [13].
The primary outcome of the analysis was having received the first dose of the COVID-19 vaccine. In Switzerland, the first COVID-19 vaccine was approved in December 2020 (Swiss Agency for Therapeutic Products, Swissmedic 2020; Supplementary Table 1) and mRNA vaccines (Moderna and Pfizer-BioNTech) were most widely used. In addition, we reported the prevalence of fully vaccinated individuals in Switzerland by the end of our study period in September 2021 (defined as having received at least two doses).
We described vaccination uptake over time. First, we reported the willingness to be vaccinated as reported in the survey. Second, we modelled the primary outcome (vaccination uptake) as a point process using Poisson regression with the logarithm of the observation time (the length of the interval between follow-up surveys per participant, i.e., ti - ti−1) as offset (or denominator) for vaccination uptake [14]. Thus the unadjusted rate ratios (RR) are given as follows: log(E(Yi)/(ti - ti−1)) = 𝛽0+𝛽x. We set time zero to be 1 January 2021, shortly after the administration of the first vaccinations. All participants’ observations were included until they reported having received the first dose, if applicable, and were censored thereafter. We included data recorded on unvaccinated participants at all timepoints. We derived rates from the exponentiated coefficients of the Poisson regression model.
Vaccination status was the dependent variable, and the following factors were covariates: time (survey wave), age, gender, region, residence, country of birth, education level, employment level, net household income, household size, vulnerable group within the household, testing for SARS-CoV-2, number of contacts, and attitude towards COVID-19 measures. The last three covariates could change over time for participants. We performed univariable and multivariable regression models and reported the RR and adjusted RR (aRR) with 95% confidence intervals (CI), controlling for all covariates. We included time by survey waves and modelled an interaction with age to account for the different times at which vaccines became available for different age groups. We calculated the cumulative vaccination uptake for a given interval as one minus the product of all probabilities of not being vaccinated until that interval.
In a sensitivity analysis, we set time zero to be 1 June 2021, which was just before the first survey wave. We performed further sensitivity analyses and compared the results from the Poisson regression model to those derived using Cox proportional hazards regression models. We ran Cox regression models, first with all participants included in the main analysis and second for individuals with an exact date of vaccination (86%) or who had not been vaccinated during the study period, with and without inverse probability weighting cumulatively over time (IPWC) to account for dropouts [15]. We estimated the probability of censoring with each observation or up to the time point of vaccination. Probabilities were then derived with a logistic regression model adjusting for all covariates as described in our main analysis. Further, we subtracted estimated probabilities from 1, which resulted in an estimate of the probability of being uncensored for a given observation. We accumulated these probabilities over time for each participant. Finally, we derived stabilised weights using a logistic regression model without covariates for the nominator. We defined missingness as when a participant was absent in any survey wave after recruitment. To estimate these probabilities, we used logistic regression with all observations and all covariates from the main regression model plus the primary outcome. Further, we use each participant’s last observation to test whether the missingness of a survey wave was associated with covariates that we previously described.
Results
This study included six survey waves from 3 June to 2021 to 9 September 2021, with participants enrolled during the first three waves (Table 1; Supplementary Fig. 1; Supplementary Fig. 2). We followed participants for 55 days on average (range: 0-103 days). The study included 6,758 observations from 1,884 participants. Overall, 918 (49%) were females and 956 (51%) were males. Participants’ age ranged from 18 to 90 years with a median of 47 years. The study population was largely representative of the Swiss population (Supplementary Table 2). For the regression analysis, we included 1,883 participants (one participant had missing data for vaccination status; Table 2). Further, we identified missing data for six observations from three participants (four for vaccination status and two for contact information). We excluded these observations from regression analyses. Of all who participated from June to September 2021, 443 (24%) did not miss any waves, 363 (19%) missed at least one survey wave, and 1,078 (57%) dropped out before the last wave.
Table 1
Overview of survey waves
| Survey wave | Start date, year-month-day | End date, year-month-day | Number of participants | Number of newly enrolled participants | Number of missing participants who had been previously enrolled | Number of returning participants after missing at least one wave | Number of participants with no missing variables |
|---|---|---|---|---|---|---|---|
| B1 | 2021-06-03 | 2021-06-14 | 996 | 996 | 0 | 0 | 996 |
| B2 | 2021-07-02 | 2021-07-19 | 1,559 | 800 | 237 | 0 | 1,558 |
| B3 | 2021-07-20 | 2021-07-29 | 1,324 | 88 | 392 | 69 | 1,322 |
| B4 | 2021-08-10 | 2021-08-16 | 1,120 | 0 | 393 | 189 | 1,119 |
| B5 | 2021-08-26 | 2021-09-01 | 953 | 0 | 354 | 187 | 952 |
| B6 | 2021-09-09 | 2021-09-15 | 806 | 0 | 367 | 220 | 805 |
Table 2
Socio-demographic characteristics, history of testing for SARS-CoV-2, social contact behaviour, and perception of COVID-19 measures in all study participants and in study participants who got vaccinated by the end of the study. * For time-dependent variables, the last observation of the participant is given. Abbreviation: EU, European Union; CHF Swiss Francs
| Category | All participants, N (%) | Vaccinated participants, n (%) |
|---|---|---|
| Total | 1,883 (100%) | 1,321 (100%) |
| Age groups, years | ||
| 18–29 | 358 (19%) | 216 (16%) |
| 30–39 | 358 (19%) | 234 (18%) |
| 40–49 | 308 (16%) | 203 (15%) |
| 50–59 | 363 (19%) | 263 (20%) |
| 60–69 | 289 (15%) | 226 (17%) |
| 70+ | 207 (11%) | 179 (14%) |
| Gender | ||
| Female | 918 (49%) | 613 (46%) |
| Male | 955 (51%) | 699 (53%) |
| Other | 10 (1%) | 9 (1%) |
| Region | ||
| Urban | 1,426 (76%) | 1039 (79%) |
| Rural | 457 (24%) | 282 (21%) |
| Swiss regions | ||
| Espace Mittelland | 406 (22%) | 273 (21%) |
| Zurich | 351 (19%) | 260 (20%) |
| Lake Geneva region | 337 (18%) | 235 (18%) |
| Eastern Switzerland | 263 (14%) | 186 (14%) |
| Northwestern Switzerland | 262 (14%) | 181 (14%) |
| Central Switzerland | 182 (10%) | 129 (10%) |
| Ticino | 82 (4%) | 57 (4%) |
| Country of birth | ||
| Switzerland | 1,331 (71%) | 927 (70%) |
| EU | 249 (13%) | 176 (13%) |
| Non-EU | 156 (8%) | 113 (9%) |
| Unknown | 147 (8%) | 105 (8%) |
| Education level | ||
| Obligatory school and vocational education | 805 (43%) | 531 (40%) |
| Gymnasium and advanced vocational education | 639 (34%) | 439 (33%) |
| Higher education (e.g., Bachelor, Master, or PhD) | 439 (23%) | 351 (27%) |
| Employment status | ||
| Employed | 1,161 (62%) | 789 (60%) |
| Unemployed | 110 (6%) | 67 (5%) |
| Student | 116 (6%) | 83 (6%) |
| Homemaker | 75 (4%) | 43 (3%) |
| Retired | 377 (20%) | 313 (24%) |
| Another unemployed situation | 44 (2%) | 26 (2%) |
| Household income, net | ||
| 0–5,000 CHF | 592 (31%) | 380 (29%) |
| 5,001–10,000 CHF | 762 (40%) | 539 (41%) |
10,000 + + CHF CHF | 248 (13%) | 200 (15%) |
| Preferred not to answer | 281 (15%) | 202 (15%) |
| Household size | ||
| Median (range) | 2 (1–10) | 2 (1–10) |
| Household with medically vulnerability | ||
| No person in a risk group | 1,305 (69%) | 871 (66%) |
| One or more person in a risk group | 578 (31%) | 450 (34%) |
| Testing for SARS-Cov-2* | ||
| Tested positive | 31 (2%) | 25 (2%) |
| Tested | 543 (29%) | 336 (25%) |
| Never tested | 1,277 (68%) | 941 (71%) |
| Preferred not to answer | 32 (2%) | 19 (1%) |
| Number of contacts per day* | ||
| 0–2 | 767 (41%) | 547 (41%) |
| 3–5 | 527 (28%) | 377 (29%) |
| 6+ | 589 (31%) | 397 (30%) |
| Attitudes towards COVID-19 measures* | ||
| About right | 913 (48%) | 737 (56%) |
| Too lenient | 423 (22%) | 356 (27%) |
| Too strict | 501 (27%) | 204 (15%) |
| Don’t know | 46 (2%) | 24 (2%) |
From May 2021 onwards, the COVID-19 vaccination campaign in Switzerland targeted the entire adult population and uptake increased during the study period (Fig. 1A). Vaccination uptake in our study population was higher than in the overall population of Switzerland. In the first survey wave of June 2021, 533 (54%) had at least one vaccine dose compared with 43% of the general Swiss population. This increased to 75% by the sixth survey wave, compared with 70% in the general adult population (Fig. 1A). Participants who had not already been vaccinated indicated their willingness as whether they intended, were hesitating, or had no intention to get vaccinated. The increase in vaccine uptake within the CoMix study occurred mainly amongst those who wanted to get vaccinated (18% in the first wave to 4% in the last wave) rather than those that had no intention (16% in the first wave to 14% in the last wave) or were hesitant (12% in the first wave to 7% in the last wave) (Fig. 1B).
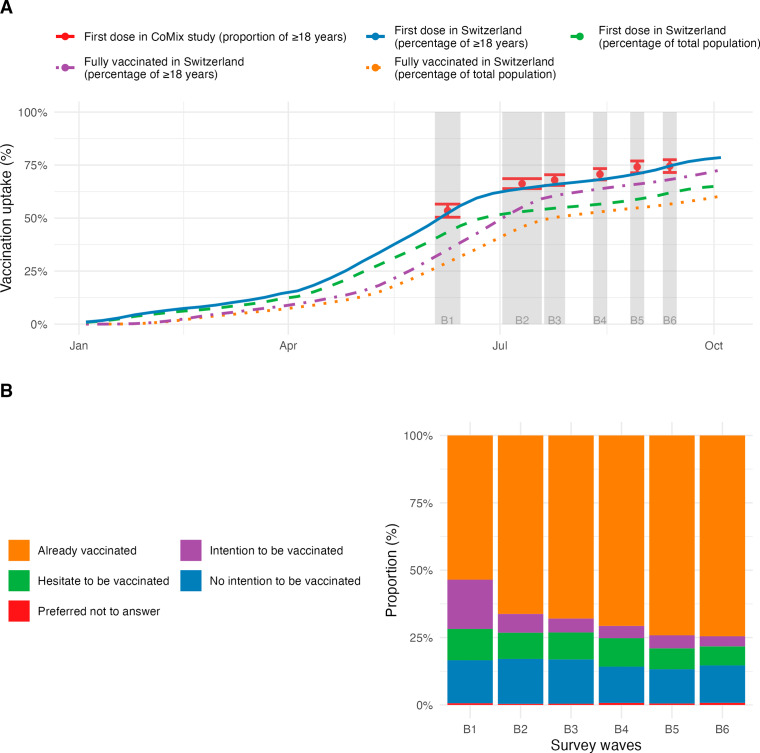
COVID-19 vaccination uptake in Switzerland. A: Comparison of vaccination uptake in the CoMix survey participants (red dots with 95% confidence intervals) and general population of Switzerland. B: Willingness to receive COVID-19 vaccination
In the unadjusted Poisson regression model, we found that people in all older age groups were more likely to get vaccinated than those in the youngest age group (18–29 years; Fig. 2). In the adjusted Poisson regression model, the vaccination uptake per interval in adults 30 years and older was highest before the first survey wave and declined afterwards (Fig. 3). The vaccination uptake per interval in younger adults (18–29 years) peaked at the second survey wave, then declined and increased again at the last survey wave. The modelled cumulative vaccination uptake over the entire study period depended less on age than expected from the crude vaccination uptake in the CoMix study, i.e., the effect of other covariates became more important (Supplementary Fig. 3). Being male was associated with higher vaccination uptake (aRR 1.09, 95% CI: 1.04–1.15) (Fig. 2). We found geographical differences in vaccination uptake. Living in rural areas was associated with lower vaccine uptake than in urban areas (aRR 0.85, 95% CI: 0.80–0.90). Vaccination uptake varied slightly between regions. Most regions were associated with higher vaccine uptake than Espace Mittelland. We did not find statistical evidence of an association between country of birth and vaccination uptake.
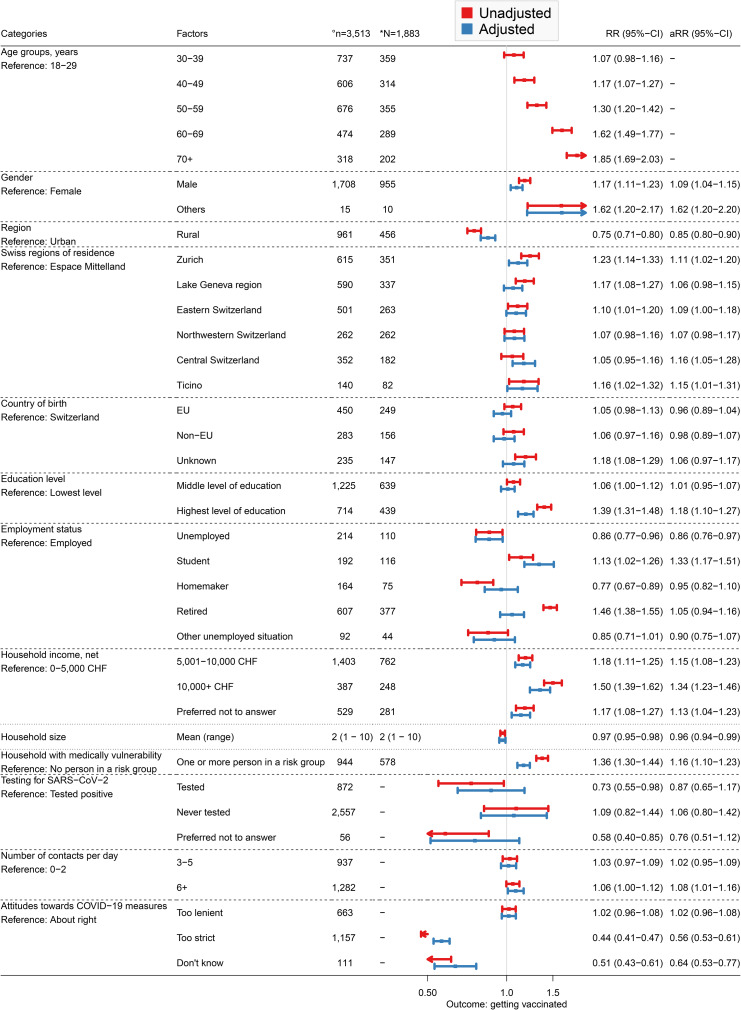
Results of the univariable and multivariable Poisson regression models. The primary outcome of the analysis is having received the first dose of a COVID-19 vaccine. °Number (n) of observations included in the regression analysis. *Number (N) of participants included in the regression analysis. Abbreviations: EU, European Union; CHF, Swiss Francs; CI, confidence interval; RR, rate ratio; aRR, adjusted rate ratio
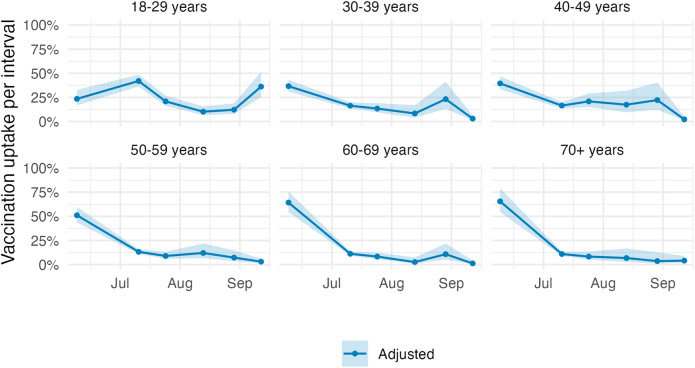
Vaccination uptake per interval by age group. Vaccination uptake corresponds to the percentage receiving the first vaccine dose amongst those who have not already received it. The estimates were adjusted for gender, region, Swiss region of residence, country of birth, education level, employment level, net household income, household size, household with a medically vulnerable individual, testing for SARS-CoV-2, number of contacts per day, and attitude towards COVID-19 measures, with an interaction between age and survey wave. The shaded area indicates the 95% confidence interval
We found that the highest education level (having a Bachelor, Master or PhD), was associated with a higher vaccination uptake (aRR 1.18, 95% CI: 1.10–1.27) than with the lowest education level (completed obligatory school and vocational education only). Unemployed participants were less likely (aRR 0.86, 95% CI: 0.76–0.97) and students were more likely (aRR: 1.33, 95% CI: 1.17–1.51) to get vaccinated than employed participants. In addition, higher income was associated with higher vaccination uptake. A household income between 5,001 CHF and 10,000 CHF compared with less than 5,000 CHF resulted in an aRR of 1.15 (95% CI: 1.08 −
− 1.23) and an income of at least 10,000 CHF resulted in an aRR of 1.34 (95% CI: 1.23
1.23) and an income of at least 10,000 CHF resulted in an aRR of 1.34 (95% CI: 1.23 −
− 1.46). Living in smaller households was associated with lower vaccination uptake (aRR 0.96, 95% CI: 0.94–0.99). In contrast, living with a medically vulnerable individual was associated with a higher aRR of 1.16 (95% CI: 1.10
1.46). Living in smaller households was associated with lower vaccination uptake (aRR 0.96, 95% CI: 0.94–0.99). In contrast, living with a medically vulnerable individual was associated with a higher aRR of 1.16 (95% CI: 1.10 −
− 1.23). We found no association between previous SARS-CoV-2 infections and vaccination uptake. Individuals with six or more contacts per day had higher vaccination uptake than those with fewer than three contacts (aRR 1.08, 95% CI: 1.01
1.23). We found no association between previous SARS-CoV-2 infections and vaccination uptake. Individuals with six or more contacts per day had higher vaccination uptake than those with fewer than three contacts (aRR 1.08, 95% CI: 1.01 −
− 1.16). We also found that the perception of COVID-19 measures was associated with vaccination uptake. Participants who thought that the control measures were too strict were less likely to be vaccinated compared to those who thought that the control measures were about right (aRR 0.56, 95% CI: 0.53
1.16). We also found that the perception of COVID-19 measures was associated with vaccination uptake. Participants who thought that the control measures were too strict were less likely to be vaccinated compared to those who thought that the control measures were about right (aRR 0.56, 95% CI: 0.53 −
− 0.61).
0.61).
Setting time zero to 1 June 2021, did not substantially change the results of the Poisson regression model (Supplementary Table 3). The results from the Cox regression model were similar compared to those from the Poisson regression model (Supplementary Tables 3 and 4). However, we deemed the Cox regression model less appropriate for the analysis of the data because the strong correlation between age and the time point of vaccination as a result of the age-specific vaccination campaign violates the proportional hazard assumption.
We also studied whether certain characteristics of participants were associated with missed survey waves (n =
= 1,441, 76%). We found that individuals between 40 and 69 years were less likely to have missed survey waves than the youngest age group (18–29 years). Participants living in Geneva and Ticino were more likely to have missed survey waves compared to those living in Espace Mittelland. The same was found for those born in an EU country than those born in Switzerland. Participants with six or more contacts were also more likely to have missed survey waves than those with fewer than three contacts. We did not find strong statistical evidence for associations between missingness and gender, region, education level, employment status, household income, history of testing for SARS-CoV-2, or vaccination (Supplementary Table 5). Participants who missed survey waves had little impact on the results from the Cox regression model, as the unweighted and weighted hazard ratios (HR) were similar (Supplementary Table 3).
1,441, 76%). We found that individuals between 40 and 69 years were less likely to have missed survey waves than the youngest age group (18–29 years). Participants living in Geneva and Ticino were more likely to have missed survey waves compared to those living in Espace Mittelland. The same was found for those born in an EU country than those born in Switzerland. Participants with six or more contacts were also more likely to have missed survey waves than those with fewer than three contacts. We did not find strong statistical evidence for associations between missingness and gender, region, education level, employment status, household income, history of testing for SARS-CoV-2, or vaccination (Supplementary Table 5). Participants who missed survey waves had little impact on the results from the Cox regression model, as the unweighted and weighted hazard ratios (HR) were similar (Supplementary Table 3).
Discussion
This study presents findings from analyses investigating factors associated with COVID-19 vaccination uptake in participants in the CoMix study in Switzerland. We found that vaccination uptake differed between subgroups from June to September 2021, a period during which COVID-19 vaccines were available to the entire adult population in Switzerland. Individuals who were older, male, and students, had a higher educational level, household income, and number of social contacts, and lived in a household with a medically vulnerable person were associated with higher vaccination uptake. In contrast, individuals who lived in rural areas, smaller households, and who perceived COVID-19 measures too strict were associated with lower uptake. There was no significant association between previous SARS-CoV-2 infections and vaccination uptake. Together, these results suggest that socio-demographic factors as well as individual behaviour and attitudes shaped COVID-19 vaccination uptake in Switzerland.
A major strength of our study is the use of the longitudinal CoMix survey to study multiple factors that are associated with COVID-19 vaccination uptake. The survey was based on quotas on age, gender, and region of residence and aimed to be representative of the Swiss population. As a result of the longitudinal data collection over six survey waves and modelling vaccination uptake as a point process using a Poisson regression model, we were able to capture changes in social contacts and attitudes on control measures over time. In France, Germany, and Italy, the introduction of COVID-19 vaccine passports in September 2021 resulted in an increase in vaccination uptake [16]. In our study, the increase in vaccination uptake in 18–49 year olds during the last two survey waves at the end of summer 2021 coincided with the introduction of a COVID-19 vaccination certificate, which was required for participation in certain activities (Supplementary Table 1). Another possible reason for the increase in the vaccination uptake in late summer 2021 could be the easier scheduling of vaccination appointments after the summer holidays. In contrast to the study by Heininger et al. [7], we were also able to study the association of previous SARS-CoV-2 infections and the number of social contacts with COVID-19 vaccination uptake in Switzerland.
Our study also comes with a number of limitations. The potential inclusion of participants from the same household may influence our findings due to shared behaviours among household members. However, we think that such an event would be highly unlikely due to the survey design and the recruitment of participants. Further, the overall vaccination uptake in the study population by September 2021 (75%) was somewhat higher compared to the Swiss adult population (70%). This difference could be a result of the recruitment method within which the CoMix study was biased towards individuals with access to the internet, who may be reached by banner ads, email campaigns, and social media advertisements. In addition, survey participants are likely to be healthier than the general population [17]. In the context of the CoMix study, participants might be more health-conscious and more likely to be vaccinated than the general population. Moreover, we found that individuals from the youngest and oldest age groups, non-German speaking regions, who were born in an EU country, and who had a higher number of contacts were more likely to have missed a survey wave. Therefore, the vaccination uptake and the aRR for these categories could be slightly underestimated. Although accounting for missing data from participants who missed survey waves hardly affected estimated HRs, associations between the place of residence, place of birth, and contact number with vaccination uptake should be interpreted with caution. As indicated by Moser et al. (2018), relative outcome measures like RRs may be less prone to bias than absolute quantities [18]. Further, we did not collect information about the political orientation of participants, which may have an association with COVID-19 vaccination uptake as found for the United States but not for the United Kingdom [19, 20].
Our analysis indicated that older age and higher socio-demographic status were associated with higher COVID-19 vaccination uptake in Switzerland, similar to the findings of some other studies [7, 19, 21–23]. Lazarus et al. have, however, observed considerable heterogeneity in vaccine acceptance between countries [24]. Vaccine hesitancy has also been shown to vary substantially at county level within the US [25]. For example, gender as a predictor of COVID-19 vaccine acceptance and hesitancy varied globally [7, 24, 26, 27]. In our study, women reported lower vaccination uptake than men, possibly due to the mixed guidance for pregnant women or women wanting to become pregnant [28, 29]. Among women, Skjefte et al. also found that younger age, lower income, lower level of education, being unmarried and not having health insurance were associated with vaccine hesitancy [30]. We did not find a significant association between place of birth and vaccination uptake, but systematic reviews indicated low intent to get vaccinated and low uptake in some migrant population groups [31, 32]. We asked participants’ about their perception of current COVID-19 measures, which might reflect trust in the government, which was found to be decisive in vaccine uptake [26]. Moreover, Lazarus et al. stated that vaccine hesitancy is associated with a lack of trust in COVID-19 vaccine safety and science, and scepticism about vaccine efficacy [24]. Finally, we found that individuals with a higher daily number of social contacts had a higher vaccination uptake. This could either be a result of participants increasing their number of contacts after vaccination, or that participants with a higher number of contacts are more willing to get vaccinated to protect themselves and others from infection, severe disease, and death.
Decision-making about vaccination strategies often occurs in the presence of uncertainties [25]. To develop tailored and effective vaccination strategies, it is important to understand the multifactorial causes and context of vaccination hesitancy [22]. Factors associated with vaccine hesitancy or uptake, often encompass political, religious, and socioeconomic aspects, but might vary across time, location, and specific vaccines [33, 34]. Despite the difference in time and context, a study examining the uptake of human papillomavirus (HPV) vaccines in Switzerland also found that individuals living in rural areas tended to be vaccinated less frequently [35]. Vaccination strategies need to be carefully planned to ensure readiness of both the public and the health community, including the need for effective communication about the complexities of vaccination, such as the recognition that side-effects may occur shortly after vaccination while protection from severe disease only follows later. Vaccination strategies also require a broad range of approaches on the individual, provider, health system, and national levels, which is difficult to properly coordinate and promote [36]. Policymakers have historically considered multiple options to increase vaccine uptake, ranging from communication and outreach strategies to monetary (dis)incentives, encouraging parental responsibility, and minimising distrust of expertise [37]. Experts, such as physicians and other health care providers, are still among the most trusted individuals when it comes to health care advice, including for vaccination [20, 25, 38]. Both, science, and health professionals, should be adequately trained in knowledge communication. Low vaccine uptake might be due to access and communication barriers and highlight that it is key to have outreach, and credible, consistent, and unified information about vaccines [3], such as that vaccines are among the most effective measures ever achieved through medical intervention. Engaging with and comprehending individuals sceptical about vaccination is of importance. In our study, we observed minimal changes in the attitudes of individuals who expressed no intention to get vaccinated (16% vs. 14% maintained their attitude throughout the study). We showed, within another panel of participants in the CoMix study in Switzerland, that almost half of individuals who did not intend to be vaccinated lacked trust in vaccines or feared side effects [39]. Horne et al. (2015) underscored the positive influence of factual information on people’s attitudes towards vaccination in relation to communicable disease risks [40]. Future research should focus on exploring effective social intervention strategies to enhance the uptake of vaccination. Finally, transparency about vaccine effectiveness and adverse events to set public expectations should improve trust in vaccines, but messaging should take care to avoid unintentionally overemphasising the risk of rare adverse events [41].
Our analysis suggests that women and individuals from rural areas, people with lower levels of education and lower household income, those who were unemployed, and who perceived the pandemic measures as being too strict were less likely to get vaccinated against COVID-19 in Switzerland. Tailored vaccination strategies towards these communities with lower vaccination uptake can be decisive as COVID-19 vaccination remains an important pillar in preventing severe disease and death.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We like to thank the European Centre for Disease Prevention and Control (ECDC) and the CoMix Europe Working Group for setting up the CoMix study across more than 20 European countries, and the partners at Ipsos MORI for running the survey.
Authors’ contributions
MR, LH, AM, NL, and CA conceived and designed the study. MR performed the analysis and wrote the first draft. MR, LH, AM, JR, AH, NL, and CA contributed to the interpretation of the results. MR, LH and CA wrote the manuscript. MR, LH, AM, JR, AH, NL, and CA commented on the manuscript and approved the final version.
Funding
This study received funding from the European Union’s Horizon 2020 research and innovation program - project EpiPose (No 101003688), the Swiss Federal Office of Public Health (No 142004995) and Swiss National Science Foundation (No 176233). JR was supported by the Swiss National Science Foundation (No 189498).
Data availability
Scripts used for the analysis are available on GitHub: https://github.com/ISPMBern/comix.
Declarations
The CoMix study protocols and questionnaires were approved by the local ethics committee of the Canton of Bern (project number 2020–02926), all methods were carried out in accordance with regulations, and informed consent of participants was obtained.
Not applicable.
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Articles from BMC Public Health are provided here courtesy of BMC
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/152796857
Article citations
Social contact patterns following the COVID-19 pandemic: a snapshot of post-pandemic behaviour from the CoMix study.
Epidemics, 48:100778, 29 Jun 2024
Cited by: 1 article | PMID: 38964131 | PMCID: PMC11413520
Understanding the factors associated with COVID-19 vaccine hesitancy in Venezuela.
BMC Public Health, 24(1):1117, 23 Apr 2024
Cited by: 0 articles | PMID: 38654278 | PMCID: PMC11036563
Government-Nongovernmental Organization (NGO) Collaboration in Macao's COVID-19 Vaccine Promotion: Social Media Case Study.
JMIR Infodemiology, 4:e51113, 19 Mar 2024
Cited by: 0 articles | PMID: 38502184 | PMCID: PMC10988378
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Differences in COVID-19 vaccination uptake in the first 12 months of vaccine availability in Switzerland - a prospective cohort study.
Swiss Med Wkly, 152:w30162, 01 Mar 2022
Cited by: 8 articles | PMID: 35429238
Factors Associated With COVID-19 Non-Vaccination in Switzerland: A Nationwide Study.
Int J Public Health, 68:1605852, 22 May 2023
Cited by: 1 article | PMID: 37284510 | PMCID: PMC10239801
COVID-19 vaccination during pregnancy: coverage and safety.
Am J Obstet Gynecol, 226(2):236.e1-236.e14, 10 Aug 2021
Cited by: 223 articles | PMID: 34389291 | PMCID: PMC8352848
Interventions to increase COVID-19 vaccine uptake: a scoping review.
Cochrane Database Syst Rev, 8:CD015270, 03 Aug 2022
Cited by: 18 articles | PMID: 35920693 | PMCID: PMC9347311
Review Free full text in Europe PMC
Funding
Funders who supported this work.
European Union’s Horizon 2020 (1)
Grant ID: 101003688
Swiss Federal Office of Public Health (1)
Grant ID: 142004995
Swiss National Science Foundation (2)
Grant ID: 189498
Zika virus: causality, open science and risks of emerging infectious diseases
Professor Nicola Low, University of Berne
Grant ID: 176233

 1
1 

