Abstract
Introduction
Patients with COPD who exhibit elevated levels of anxiety and/or depression are typically less able to improve symptoms and physical activity levels following a programme of pulmonary rehabilitation (PR). The objective of the present study was to provide proof of concept that offering an intervention comprising cognitive behavioural therapy (CBT) alongside physical activity behavioural modification strategies (BPA) during PR is more effective in improving physical activity outcomes compared to PR and CBT alone.Methods
32 patients with COPD (mean±sd forced expiratory volume in 1 s 42±14% predicted) were assigned 1:1 to receive PR+CBT+BPA or PR+CBT. BPA comprised motivational interviews, step-count monitoring, feedback using a pedometer and goal setting. Assessments included accelerometer-derived steps per day, movement intensity, 6-min walk distance (6MWD) and Hospital Anxiety and Depression Scale (HADS) scores.Results
The magnitude of improvement across physical activity outcomes was greater for the PR+CBT+BPA compared to the PR+CBT intervention (by 829 steps per day (p=0.029) and by 80±39 vector magnitude units (p=0.042), respectively). Compared to PR and CBT alone, the PR+CBT+BPA intervention induced greater clinically meaningful improvements in HADS anxiety scores (by -2 units, 95% CI -4-1 units) and 6MWD (by 33±20 m).Conclusions
Providing anxious and/or depressed patients with COPD with a combined intervention of CBT and BPA during PR presents more favourable improvements in physical activity outcome measures compared to CBT alone during PR.Free full text

Cognitive behavioural therapy combined with physical activity behavioural modification strategies during pulmonary rehabilitation in patients with COPD
Abstract
Introduction
Patients with COPD who exhibit elevated levels of anxiety and/or depression are typically less able to improve symptoms and physical activity levels following a programme of pulmonary rehabilitation (PR). The objective of the present study was to provide proof of concept that offering an intervention comprising cognitive behavioural therapy (CBT) alongside physical activity behavioural modification strategies (BPA) during PR is more effective in improving physical activity outcomes compared to PR and CBT alone.
Methods
32 patients with COPD (mean±sd forced expiratory volume in 1 s 42±14% predicted) were assigned 1:1 to receive PR+CBT+BPA or PR+CBT. BPA comprised motivational interviews, step-count monitoring, feedback using a pedometer and goal setting. Assessments included accelerometer-derived steps per day, movement intensity, 6-min walk distance (6MWD) and Hospital Anxiety and Depression Scale (HADS) scores.
Results
The magnitude of improvement across physical activity outcomes was greater for the PR+CBT+BPA compared to the PR+CBT intervention (by 829 steps per day (p=0.029) and by 80±39 vector magnitude units (p=0.042), respectively). Compared to PR and CBT alone, the PR+CBT+BPA intervention induced greater clinically meaningful improvements in HADS anxiety scores (by −2 units, 95% CI −4–1 units) and 6MWD (by 33±20 m).
Conclusions
Providing anxious and/or depressed patients with COPD with a combined intervention of CBT and BPA during PR presents more favourable improvements in physical activity outcome measures compared to CBT alone during PR.
Tweetable abstract
Improvements in daily physical activity (PA) outcomes are optimised when anxious and/or depressed patients with COPD undertake rehabilitation that incorporates a PA behavioural modification intervention alongside cognitive behavioural therapy https://bit.ly/3qICJst
Introduction
It is well documented that patients with COPD experience significantly lower levels of physical activity compared to healthy age-matched individuals [1–4]. Alongside this, it is acknowledged that low levels of physical activity are associated with poor prognosis for exacerbation of COPD, leading to increased rates of hospitalisation and mortality [4]. Therefore, interventions to achieve a sustained improvement in physical activity are urgently needed in this population [2].
However, recent systematic reviews and meta-analyses on interventions to promote levels of physical activity in patients with COPD have reported inconsistent findings [5–7]. These interventions included pulmonary rehabilitation (PR), physical activity counselling as a standalone intervention or alongside PR, health monitoring and nocturnal noninvasive ventilation (NNIV) [5–7]. Of these interventions, physical activity counselling both as a standalone intervention and alongside PR provided the most effective intervention, especially when implemented alongside PR [5, 6]. In addition, recent research has shown that although PR is effective for improving functional capacity, it does not necessarily translate into improved physical activity outcomes unless physical activity behavioural modification strategies are incorporated [8]. Therefore, it is evident that a combination of both PR and behavioural interventions is necessary to see meaningful improvements in physical activity outcomes.
Interestingly, our earlier systematic review and meta-analysis found that patients with greater baseline physical activity levels (>4000 steps per day) showed greater improvements in steps per day compared to those with lower baseline physical activity levels (≤4000 steps per day), following a programme of physical activity counselling [5]. In patients with low baseline physical activity (≤4000 steps per day), studies that have implemented physical activity counselling alongside PR have reported an insignificant effect on steps per day [9–11]. Furthermore, patients with COPD who exhibit lower baseline exercise capacity prior to PR are less likely to achieve significant improvements in physical activity [12]. Indeed, patients demonstrating a 6-min walk distance (6MWD) >350 m exhibit clinically meaningful improvements in steps per day compared to patients with a 6WMD ≤350 m [12]. The higher likelihood of physical activity improvement in this subgroup of patients is probably because they are more conditioned to cope with the physiological demands of the intervention and have greater self-efficacy, motivation and willingness to engage and improve their physical activity levels with the support of these interventions [12].
In addition, those reporting elevated levels of anxiety and/or depression are typically less able to manage symptoms and less likely to improve physical activity or 6MWD following PR [13, 14]. This may in part be due to anxiety and fear of exacerbating symptoms, leading many to avoid their day-to-day activities as a mechanism to manage their symptoms [15]. Meanwhile, with depression, people are typically led into a sedentary lifestyle through low mood and poor motivation, which in turn causes further physical inactivity and deconditioning [16].
Cognitive behavioural therapy (CBT) is an evidence-based intervention that can be implemented to help manage symptoms of anxiety and depression in patients with COPD [17]. Specifically, Heslop-Marshall et al. [17] developed a brief COPD-specific CBT intervention that can be delivered by respiratory nurses and demonstrated that two to six fortnightly sessions either in clinic or at home were clinically effective in reducing symptoms of anxiety in patients with moderate to severe COPD. However, in a study implementing CBT alongside PR, similar improvements were shown in depression, anxiety and quality-of-life symptoms, when compared to PR alone [18]. It is therefore envisaged that adding physical activity behavioural modification strategies to CBT during PR may optimise improvements in physical activity outcomes through improved mood and better physical conditioning in this population [13, 14].
In our original study [8], we found that a combination of physical activity behavioural modification strategies and exercise training during PR was more effective than PR alone in improving physical activity levels in patients with COPD, characterised by variable levels of anxiety and/or depression. However, the original study did not specifically look at the effects of CBT added to physical activity behavioural modification strategies (BPA) during PR on anxious and/or depressed patients with COPD.
Accordingly, in this retrospective analysis of our original study [8], we evaluated the effect of combining CBT with BPA during PR on physical activity outcomes (steps per day, movement intensity) specifically in patients with COPD who exhibit elevated anxiety and/or depression levels at the outset of a PR programme. Considering the efficacy of PR+BPA in patients with COPD [8], and the known benefits of CBT to alleviate psychological difficulties in patients with COPD [17], we envisage that a combination of CBT+PR+BPA would be superior to the provision of CBT+PR alone in improving physical activity outcomes in patients with COPD.
Methods
Study design
This is a retrospective analysis of data from a randomised controlled trial [8] which was prospectively registered at www.clinicaltrials.gov (NCT03749655) and complied with National Institute for Health and Care Research Health Research Authority requirements (reference 18/YH/0376). In this retrospective analysis we focused solely on data from patients with COPD who exhibited high baseline levels of anxiety and/or depression (Hospital Anxiety and Depression Scale (HADS) ≥8). The cut off (≥8) for the diagnosis of anxiety and/or depression using the HADS questionnaire was defined by Nowak et al. [19] and was reported to have high sensitivity (80%) and specificity (90%) in patients with COPD [20]. This was achieved through the randomisation process in the original randomised controlled trial [8], with 1:1 allocation to either PR+BPA or PR, stratified for HADS (<8 or ≥8) and 6MWD (<300 m or ≥300 m; figure 1). Once randomised, those stratified for HADS ≥8 received CBT as part of standard care provided by the Newcastle upon Tyne Hospitals NHS Foundation Trust (NuTH) on top of their randomised allocation to PR+BPA or PR (i.e. PR+BPA+CBT or PR+CBT).
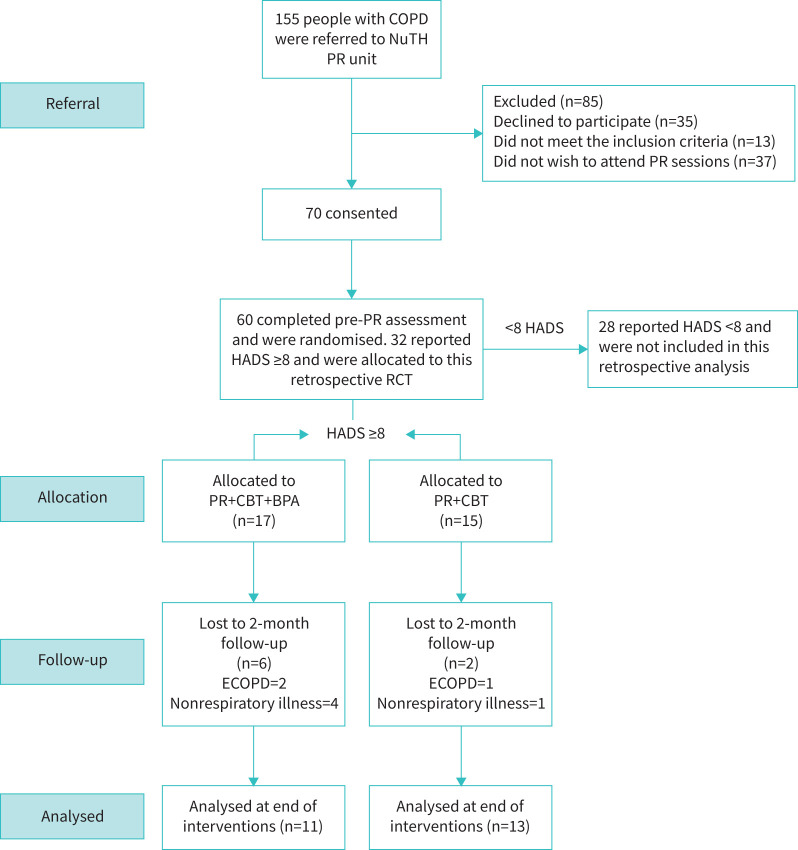
Consolidation Standards of Reporting Trials diagram of the study. NuTH: Newcastle upon Tyne Hospitals NHS Foundation Trust; PR: pulmonary rehabilitation; HADS: Hospital Anxiety and Depression Scale; RCT: randomised controlled trial; CBT: cognitive behavioural therapy; BPA: physical activity behavioural modification strategies; ECOPD: exacerbation of COPD.
Participants
Patients with COPD were recruited from NuTH chest clinic and PR services. Respiratory nurses and physiotherapists informed those eligible about the study and asked their willingness to participate in the study. Inclusion criteria included 1) COPD confirmed by obstructive spirometry (post-bronchodilator forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) ratio <0.70); 2) clinically stable male or female aged ≥40 years; 3) optimised medical therapy; 4) able to provide informed consent. Exclusion criteria included 1) orthopaedic, neurological or other concomitant disease that significantly impaired normal biomechanical movement patterns, as judged by the investigator; 2) moderate or severe COPD exacerbation within 4 weeks prior to study enrolment; 3) unstable ischaemic heart disease, including myocardial infarction within 6 weeks prior to study enrolment; 4) moderate or severe aortic stenosis or hypertrophic obstructive cardiomyopathy; 5) uncontrolled hypertension; or 6) another condition likely to limit life expectancy to <1 year (principally metastatic malignancy). Upon meeting the study entry criteria, those who agreed to participate were contacted by the research team. Detailed information regarding the study was provided and written informed consent was obtained prior to the study.
Pulmonary rehabilitation
The 8-week PR programme was delivered according to the British Thoracic Society guidelines on PR [21], with specific details regarding the PR programme available elsewhere [8]. Briefly, the 8-week PR programme comprised two 60-min sessions of exercise training per week, consisting of progressive, individualised aerobic exercise on a cycle ergometer/treadmill and resistance exercises using specific gym equipment/free weights. In addition, a 30-min session of education was delivered once per week by a multidisciplinary team comprising physiotherapists, dieticians, respiratory nurses and occupational therapists.
BPA
Specific details regarding the BPA are available elsewhere [8]. Patients received a one-to-one semi-structured motivational interview with the researcher at baseline lasting 15 min. During this time, motivational issues, favourite activities, facilitators and barriers to physical activity and strategies to become more physically active were discussed [22]. Following this, patients created three action plans, which were used throughout the programme to stimulate self-motivation to improve levels of physical activity.
BPA involved the provision of a pedometer (Fitbug, London, UK), an individualised daily step-count target (reviewed twice weekly for 8 weeks), and a step-count diary that was shared with a member of the research team at the end of every PR session. Each week, the researcher used the step count diary to calculate a new daily step-count target, by increasing the preceding week's average daily step-count by 10%. In addition, the researcher dedicated 10 min following the PR session to provide education on the importance of physical activity and advice on how to increase physical activity levels, referring to people's three action plans formed at baseline.
CBT
CBT lasting ~30 min was administered to patients with COPD with a HADS ≥8, as part of standard PR service by respiratory nurses at either the chest clinic or at home. Specific details regarding delivery of CBT in this study can be found in a previously published randomised controlled trial [17]. Briefly, CBT focused on four key elements: behaviour, cognition/thoughts, feelings/emotions and physical sensations, with the aim of understanding how these experiences were interpreted [17]. Furthermore, to aid symptoms of anxiety and depression, several techniques including education on anxiety, depression and COPD, distraction techniques, breathing control, relaxation and rating achievement/pleasure of physical activity were used [17].
Outcome measures
All outcome measures were assessed 1 week prior to the onset of the PR programme and 1 week following completion of the PR programme. Objective measures of physical activity, including steps per day, intensity of physical activity (expressed as vector magnitude units (VMU)) and time spent in various domains of physical activity (sedentary, light and moderate vigorous physical activity) were assessed using the Actigraph wGT3X (Actigraph, Pensacola, FL, USA), validated for use in COPD [23, 24]. VMU, the sum of movements in three planes over each minute, were used to quantify the intensity of daily physical activity using the Actigraph triaxial accelerometer (Actigraph wGT3X) [25, 26]. VMU as an outcome measure is reported as the mean intensity of physical activity per minute over a specific period of accelerometer wear time, which is outlined later. Patients were instructed to wear an Actigraph accelerometer during waking hours for seven consecutive days, prior to the onset of PR and following completion of PR. Valid physical activity data from the Actigraph accelerometer were based on a minimum wear time of 8 h on ≥4 weekdays within the 7-day period [27, 28]. Patients’ experiences of physical activity were assessed using the Clinical Visit PROactive Physical Activity in COPD (C-PPAC) instrument, validated for use in COPD [29]. The instrument combines 12 questions regarding patients’ subjective thoughts on amount and difficulty of physical activity alongside objective physical activity outcome data from the Actigraph accelerometer [27]. Based on these data, three categories were generated (amount of physical activity, difficulty of physical activity and total physical activity experience) ranging from 0 to 100, where higher numbers indicated a better score of physical activity experience. Other outcome measures included 1) the 6MWD [30]; 2) quadriceps muscle strength (one leg extension repetition maximum using a calibrated Myometer (MIE Medical Research, Leeds, UK), and endurance (30-s sit-to-stand repetitions) and 3) upper body strength (handgrip dynamometer) [31–33]; 4) health-related quality of life (QoL) (COPD assessment test (CAT)) [34]; 5) the Clinical COPD Questionnaire (CCQ) [35]; 6) anxiety and depression (HADS) [36]; and 7) Medical Research Council (MRC) dyspnoea scale [37].
Data analysis
Characteristics of patients with COPD and outcome data at baseline and following PR are reported as means±sd or 95% confidence intervals unless otherwise stated. All analyses were completed using SPSS version 28 (IBM, London, UK), with an intention-to-treat statistical analysis used for all outcome measures and missing data handled using a multiple imputation approach. Within- and between-group differences pre- to post-intervention are reported as mean (95% CI). Independent-samples t-tests were implemented to compare baseline group characteristics. A two-way repeated-measures ANOVA was implemented for all outcome variables, to identify differences between the two interventions. Statistical significance was set at p<0.05 for all analyses.
Results
Participants
In total, 32 patients with HADS ≥8 (for anxiety and/or depression) provided consent for the study and were randomised to PR+CBT+BPA (n=17) and PR+CBT (n=15) (figure 1). Throughout the study, eight patients were lost due to nonrespiratory illness (n=5) and COPD exacerbations (n=3). Therefore, 24 patients completed the post-PR assessment visit, with 11 completing the PR+CBT+BPA and 13 completing the PR+CBT interventions (table 1). No significant differences in baseline lung function and physical activity characteristics were reported prior to both interventions (table 1).
TABLE 1
Baseline characteristics
| PR+CBT+BPA | PR+CBT | p-value | |
| Participants | 17 | 15 | |
| Age | 66±4 | 71±5 | 0.306 |
| Male/female | 4/13 | 7/8 | NA |
| BMI kg·m−2 | 27±7 | 25±5 | 0.493 |
| FEV1 L | 1.07±0.40 | 0.94±0.50 | 0.155 |
| FVC L | 2.19±0.60 | 2.01±0.60 | 0.676 |
| FEV1 % pred | 44±16 | 41±12 | 0.098 |
| FVC % pred | 71±20 | 73±40 | 0.445 |
| FEV1/FVC % | 49±13 | 46±14 | 0.228 |
| 6MWD m | 276±22 | 259±23 | 0.161 |
| Physical activity steps per day | 2972±437 | 2962±466 | 0.217 |
| MVPA min | 6±2 | 6±2 | 0.537 |
| CAT score | 29±1 | 25±1 | 0.666 |
| HADS anxiety score | 13±1 | 11±1 | 0.075 |
| HADS depression score | 11±2 | 10±2 | 0.579 |
Data are presented as n or mean±sem, unless otherwise stated. PR: pulmonary rehabilitation; CBT: cognitive behavioural therapy; BPA: physical activity behavioural modification strategies; BMI: body mass index; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; 6MWD: 6-min walk distance; MVPA: moderate vigorous physical activity; CAT: COPD Assessment Test; HADS: Hospital Anxiety and Depression Scale; NA: not applicable.
Physical activity outcomes
Individual responses to Actigraph accelerometer-derived physical activity outcomes are shown in figures 2 and and3.3. Post-PR, the magnitude of improvement in steps per day was significantly greater (p=0.029) for the PR+CBT+BPA compared to PR+CBT interventions (by 829 steps per day, 95% CI 91–1564 steps per day) (table 2, figure 2). This difference was within the clinically important improvement margins (600–1100 steps per day) [38]. Following the completion of PR, the PR+CBT+BPA exhibited a significantly greater (p=0.042) improvement in the intensity of physical activity (by 80 VMU, 95% CI 3–162 VMU) (table 2, figure 3) compared to the PR+CBT intervention.
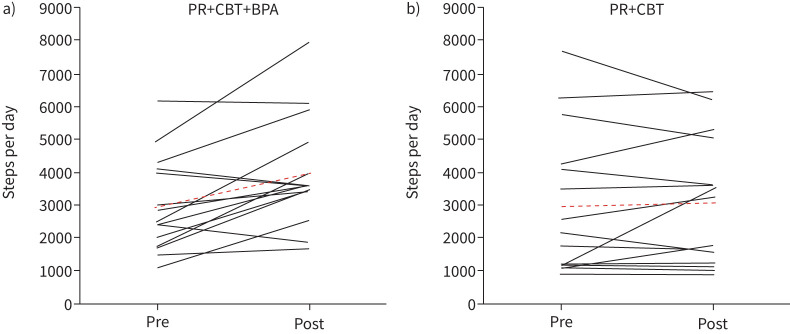
Individual responses to a) pulmonary rehabilitation (PR)+cognitive behavioural therapy (CBT)+physical activity behavioural modification strategies (BPA) and b) CBT+PR for changes in steps per day.
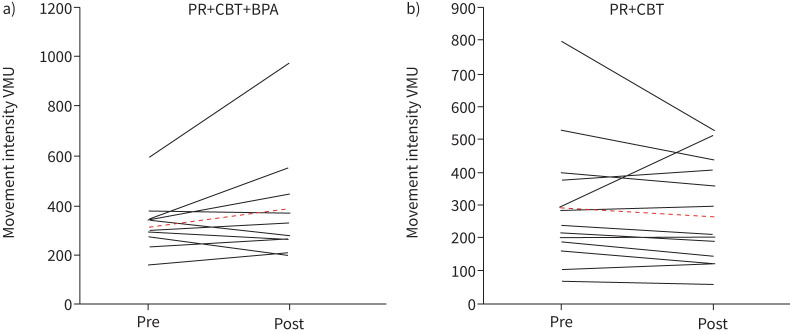
Individual responses to the a) pulmonary rehabilitation (PR)+cognitive behavioural therapy (CBT)+physical activity behavioural modification strategies (BPA) and b) CBT+PR for changes in movement intensity. VMU: vector magnitude units.
TABLE 2
Change in physical activity outcome measures in the pulmonary rehabilitation (PR)+cognitive behavioural therapy (CBT)+physical activity behavioural modification strategies (BPA) (n=17) and PR+CBT (n=15) interventions
| Baseline | Post-PR | Within-group mean difference (95% CI) | p-value | Between-group difference (95% CI) | p-value | |
| Steps per day | ||||||
 PR+CBT+BPA PR+CBT+BPA | 2972±437 | 3920±422 | 948±247 | 0.001 | 829±360 | 0.029 |
 PR+CBT PR+CBT | 2962±466 | 3018±450 | 119±262 | 0.654 | ||
| Intensity of physical activity VMU | ||||||
 PR+CBT+BPA PR+CBT+BPA | 311±37 | 362±38 | 51±27 | 0.063 | 80±39 | 0.042 |
 PR+CBT PR+CBT | 298±39 | 266±41 | −31±28 | 0.278 | ||
| Sedentary time min per day | ||||||
 PR+CBT+BPA PR+CBT+BPA | 513±18 | 461±21 | −52±16 | 0.004 | −18±24 | 0.458 |
 PR+CBT PR+CBT | 545±19 | 511±22 | −34±18 | 0.065 | ||
| Light physical activity time min per day | ||||||
 PR+CBT+BPA PR+CBT+BPA | 158±12 | 148±10 | −10±10 | 0.306 | −3±14 | 0.805 |
 PR+CBT PR+CBT | 142±13 | 135±11 | −7±10 | 0.529 | ||
| MVPA min per day | ||||||
 PR+CBT+BPA PR+CBT+BPA | 6±2 | 9±2 | 3±1 | 0.013 | 2±2 | 0.307 |
 PR+CBT PR+CBT | 6±2 | 7±2 | 1±2 | 0.305 | ||
| C-PPAC total score | ||||||
 PR+CBT+BPA PR+CBT+BPA | 47±3 | 61±9 | 14±2 | 0.001 | 10±3 | 0.002 |
 PR+CBT PR+CBT | 58±7 | 62±3 | 4±3 | 0.192 | ||
| C-PPAC difficulty score | ||||||
 PR+CBT+BPA PR+CBT+BPA | 43±4 | 63±4 | 20±3 | 0.001 | 13±4 | 0.003 |
 PR+CBT PR+CBT | 52±4 | 59±4 | 7±3 | 0.033 | ||
| C-PPAC amount score | ||||||
 PR+CBT+BPA PR+CBT+BPA | 44±4 | 63±4 | 19±3 | 0.001 | 13±4 | 0.005 |
 PR+CBT PR+CBT | 53±4 | 59±4 | 6±3 | 0.033 |
Data are presented as mean±sd, unless otherwise stated. VMU: vector magnitude units; MVPA: moderate vigorous physical activity; C-PPAC: Clinical visit PROactive Physical Activity in COPD.
Experiences of physical activity
Individual responses to the C-PPAC instrument are shown in figure 2. Post-PR, the total score of the C-PPAC instrument was improved by a clinically important margin (>4 points) [27] in the PR+CBT+BPA intervention compared with the PR+CBT intervention, with a between-group difference of 10 points (95% CI 5–19 points, p=0.002 (table 2). For the difficulty score of the C-PPAC instrument, a clinically important margin (>6 points) [27] of 13 points (95% CI 5–22 points, p=0.003 (table 2) was found. Finally, the amount score of the C-PPAC instrument improved by clinically important margin (>6 points) [27] of 13 points (95% CI 4–21 points, p=0.005 (table 2).
Anxiety and depression
Post-PR, a clinically important difference (<1.5 units) [39], in the magnitude of reduction in HADS anxiety score (by −2 unit, 95% CI −4–1 units; p=0.137) (table 3) was demonstrated in favour of the PR+CBT+BPA compared to the PR+CBT intervention. Following completion of PR, a clinically important difference in the magnitude of reduction (<1.5 units) in HADS depression score was demonstrated across both interventions, with a between-group difference of −1 unit (95% CI −3–1 units; p=0.125) (table 3).
TABLE 3
Change in exercise capacity, muscular strength/endurance, quality of life and anxiety and depression outcome measures in the pulmonary rehabilitation (PR)+cognitive behavioural therapy (CBT)+physical activity behavioural modification strategies (BPA) (n=17) and PR+CBT (n=15) interventions
| Baseline | Post-PR | Within-group mean difference (95% CI) | p-value | Between-group mean difference (95% CI) | p-value | |
| 6MWD m | ||||||
 PR+CBT+BPA PR+CBT+BPA | 276±22 | 339±18 | 63±15 | <0.001 | 33±20 | 0.118 |
 PR+CBT PR+CBT | 259±23 | 289±19 | 30±15 | 0.044 | ||
| Handgrip kg | ||||||
 PR+CBT+BPA PR+CBT+BPA | 18.6±1.5 | 19.8±1.6 | 1.2±2.3 | 0.595 | 3.5±1.1 | 0.003 |
 PR+CBT PR+CBT | 23.4±1.7 | 21.1±1.8 | −2.3±2.5 | 0.383 | ||
| QMVC kg | ||||||
 PR+CBT+BPA PR+CBT+BPA | 22.5±1.6 | 27.4±1.7 | 4.9±1.0 | <0.001 | 1.5±1.2 | 0.342 |
 PR+CBT PR+CBT | 21.2±1.7 | 24.6±1.8 | 3.4±1.1 | 0.004 | ||
| Sit-to-stand reps | ||||||
 PR+CBT+BPA PR+CBT+BPA | 9±1 | 12±1 | 3±1 | <0.001 | 1±1 | 0.023 |
 PR+CBT PR+CBT | 9±1 | 11±1 | 2±1 | 0.003 | ||
| CCQ (total) | ||||||
 PR+CBT+BPA PR+CBT+BPA | 3.1±0.3 | 2.6±0.3 | −0.5±0.2 | 0.034 | −0.8±0.3 | 0.020 |
 PR+CBT PR+CBT | 3.2±0.3 | 3.5±0.3 | 0.3±0.2 | 0.206 | ||
| CCQ (symptoms) | ||||||
 PR+CBT+BPA PR+CBT+BPA | 2.9±0.2 | 2.4±0.3 | −0.5±0.2 | 0.023 | −0.5±0.4 | 0.655 |
 PR+CBT PR+CBT | 3.4±0.2 | 3.4±0.3 | 0.0±0.3 | 0.973 | ||
| CCQ (functional) | ||||||
 PR+CBT+BPA PR+CBT+BPA | 2.9±0.3 | 2.6±0.3 | −0.3±0.3 | 0.257 | −0.2±0.4 | 0.564 |
 PR+CBT PR+CBT | 3.2±0.3 | 3.1±0.3 | −0.1±0.3 | 0.778 | ||
| CCQ (mental) | ||||||
 PR+CBT+BPA PR+CBT+BPA | 2.7±0.4 | 1.6±0.4 | −1.1±0.3 | 0.002 | −1.1±0.5 | 0.034 |
 PR+CBT PR+CBT | 2.4±0.4 | 2.4±0.4 | 0.0±0.4 | 0.938 | ||
| CAT | ||||||
 PR+CBT+BPA PR+CBT+BPA | 29±1 | 31±1 | 2±1 | 0.519 | −2±2 | 0.092 |
 PR+CBT PR+CBT | 25±1 | 29±1 | 4±2 | 0.020 | ||
| HADS anxiety | ||||||
 PR+CBT+BPA PR+CBT+BPA | 13±1 | 10±1 | −3±1 | 0.002 | −2±1 | 0.137 |
 PR+CBT PR+CBT | 11±1 | 10±1 | −1±1 | 0.277 | ||
| HADS depression | ||||||
 PR+CBT+BPA PR+CBT+BPA | 11±1 | 8±1 | −3±1 | <0.001 | −1±1 | 0.125 |
 PR+CBT PR+CBT | 10±2 | 8±1 | −2±1 | 0.003 | ||
| MRC | ||||||
 PR+CBT+BPA PR+CBT+BPA | 3±1 | 3±1 | 0±1 | 0.302 | 0±1 | 0.205 |
 PR+CBT PR+CBT | 3±1 | 3±1 | 0±1 | 0.208 |
Data are presented as mean±sd, unless otherwise stated. 6MWD: 6-min walk distance; QMVC: quadriceps muscle voluntary capacity; CCQ: Clinical COPD Questionnaire; CAT: COPD Assessment Test; HADS: Hospital Anxiety and Depression Scale; MRC: Medical Research Council dyspnoea scale.
Other outcomes
The 6MWD significantly improved following both PR+CBT+BPA and CBT+PR interventions, with no significant between group differences (table 3). However, the between-group difference (33±20 m) in 6MWD exceeded the clinically meaningful margins (30 m) (table 3) [40]. Both PR+CBT+BPA and CBT+PR demonstrated a clinically meaningful (>2 point) [39] worsening in CAT scores; however, the worsening was smaller in the PR+CBT+BPA group (table 3). Significant differences in upper body strength were demonstrated in favour of the PR+CBT+BPA group (table 3). Significant improvements in lower body strength were demonstrated in both the PR+CBT+BPA and PR+CBT interventions; however, no between-group differences in lower body strength were demonstrated (table 3).
Discussion
The novel findings of this study suggest that providing anxious and/or depressed patients with COPD with a combined intervention of CBT, physical activity behavioural modification strategies and PR, presents more favourable improvements in several physical activity outcome measures including steps per day, movement intensity and experiences of physical activity, compared to providing CBT alone during PR.
The magnitude of improvement in daily physical activity (by 828 steps per day) in the present study compares favourably with the majority of studies showing clinically important improvements across interventions of PR+physical activity [9, 10, 41, 42], telecoaching [43] and physical activity urban training [44] in patients with COPD. Such similarities in physical activity improvements are fundamental to patients with COPD with elevated anxiety/depression for several reasons. Firstly, previous literature has highlighted the negative impact that anxiety and/or depression may have on baseline levels of physical activity and the associated link between low levels of physical activity and increased risk of hospitalisation and mortality [4, 16]. This is particularly relevant in the current study, as the average baseline physical activity levels of our study population (2960 steps per day) were substantially lower than the average levels reported in previous studies implementing PR+physical activity in patients with COPD (~4200 steps per day) [9, 10, 41, 42, 45]. Linking closely to this, it has recently been evidenced that reduced baseline physical activity levels will probably constrain the effectiveness of physical activity interventions of this nature, highlighting the importance of our findings [5].
Accordingly, it's important to recognise the justification for these findings and gauge a better understanding of why the combined PR+CBT+BPA intervention may more effectively support physically inactive patients with COPD, compared to the CBT+PR intervention. Considering CBT, which is based upon a model of “talking therapy”, patients can focus their negative thoughts and emotions on specific events that cause behavioural avoidance and explore the reasoning behind them [46]. Through the phrase “it's not the event, but what individuals make of the event that is important”, patients are able to identify unhelpful thoughts and behaviours, relieving anxious and depressive thoughts during stressful events such as exercise [46]. Subsequently, patients with COPD are less fearful during daily physical activities, preventing the vicious cycle of panic and avoidance during unexpected stages of breathlessness [15].
However, as reported in the CBT+PR group, simply alleviating anxious and/or depressive thoughts and emotions through CBT and improving exercise capacity through PR, does not automatically translate into improved physical activity levels. One reason for this links to the vicious cycle of inactivity model [47]. Within this, two vicious cycles, characterised by dyspnoea and/or deconditioning, lead to worsening of anxiety and/or breathing sensations during physical activity. As a result, patients begin to change their physical activity behaviour, choosing a sedentary lifestyle over greater levels of physical activity in response to the symptoms associated with their condition [48]. Therefore, the addition of BPA, including education on the benefits of physical activity and incorporation of behaviour change techniques such as goal setting, action planning and self-monitoring, alongside CBT and PR, may empower and motivate anxious/depressed patients with COPD to engage in more daily physical activities [8, 49].
Based on the novel findings of this study, it is plausible to suggest that through the mechanisms of behavioural modification strategies, PR, and CBT, as detailed earlier, deconditioned patients with COPD may improve physical activity by clinically meaningful margins. Furthermore, if these improvements can be replicated across future studies and clinical practice, patients may see additional improvements in key clinical outcomes including exacerbation risk, and hospital admissions, due to their close association with sustained improvements in physical activity [4, 50–53].
Another relevant finding from this study was the clinically important difference in anxiety following completion of the CBT+PR+BPA intervention, emphasising the potential beneficial effects of combining CBT with physical activity behavioural strategies on anxiety. One proposed reason for this may link to the previously detailed association between anxiousness and physical activity in patients with COPD, particularly with reference to fear avoidance [54]. Specifically, a recent study provided preliminary evidence that disease-specific anxiety and fear avoidance have a specific influence on predicted physical activity levels in patients with COPD who displayed lower relative physical capacity [54]. As a result, the smaller improvement in anxiety in those undertaking CBT+PR may have been associated with the poor baseline physical capacity and physical activity levels, leaving patients in continuous fear and avoidance of physical activity.
A clinically important difference in 6MWD following completion of both interventions was reported, confirming the effectiveness of PR for improving exercise capacity [55]. Interestingly, those who completed the CBT+PR+BPA intervention experienced superior improvements in 6MWD, which exceeded the clinically meaningful margin (30 m). Importantly, a significant improvement for the intensity of physical activity was found for the CBT+BPA+PR intervention, with a significant between-intervention magnitude of change in intensity of physical activity. It's plausible to suggest that the reduction in anxiety and fear as well as greater confidence in managing symptoms during daily activities would encourage patients to complete daily activities at a greater pace/intensity [15]. In turn, these greater intensities may have translated into improved experiences of physical activity, as reported through the significant improvement in C-PPAC instrument outcomes. The clinical relevance of this finding is important due to the severe reduction in walking pace typically reported in patients with severe COPD, that is known to be associated with poor prognosis [56]. Often, the intensity of physical activity presents an indication of a patient's ability to conduct physical activity, providing a breakdown of the time taken to complete a task. Unlike steps per day, which gives an overall accumulation of activity over a set period, the intensity of physical activity provides better understanding of how patients’ symptoms impact physical activity and how they cope/engage with daily tasks [56]. Through observing improvements in both the duration (steps per day) and intensity (VMU) of physical activity, its plausible to suggest that patients in the current study were able to increase both the amount of walking activity and the pace at which walking activity was undertaken.
Based on the novel findings of this study, it's important to highlight that despite the equally poor physical activity levels (≤4000 steps per day) and 6MWD (≤350 m) across all patients with COPD in both the PR+CBT+BPA and PR+CBT groups, the combination of PR+CBT+BPA resulted in greater improvements for several outcomes including physical activity and 6MWD compared to PR+CBT. These findings provide vital evidence that combining the three elements of this intervention can challenge earlier claims that physical activity counselling interventions alongside PR are effective in improving physical activity levels only in patients with COPD exhibiting greater levels of physical activity (>4000 steps per day) and exercise capacity (>350 m) at baseline [9–12].
Study limitations
Several limitations should be considered from this study. Firstly, this retrospective analysis was unable to assess the true effect of CBT. This was due to CBT being part of standard care across NuTH, meaning we couldn't modify standard care for the purpose of this research. Secondly, eight out of 32 patients were lost during the study, meaning that only 24 patients with COPD completed both pre and post assessments. As a result, generalisability of the findings to clinical practice may be limited at this stage. Nevertheless, the 25% dropout rate across the study duration is in line with the average dropout rate reported by the UK National COPD Audit Programme for pulmonary rehabilitation [57]. Thirdly, CBT engages several techniques including education on anxiety and depression, thereby aiding the mitigation of the intensity of these symptoms. Nevertheless, despite our finding of a clinically important difference in anxiety following completion of the CBT+PR+BPA intervention, we cannot reliably confirm that the additional contact with the CBT specialist did not assist patients to improve their mental health, contributing to the observed benefit. Furthermore, all components of the intervention (CBT, PR and BPA) included factors that are difficult to keep separate while being delivered collectively (e.g. the PR+CBT group may receive elements of behaviour change which may contribute to BPA). Indeed, exercise training as part of PR may aid improvements in daily physical activity, albeit to a smaller extent [5]. Finally, due to the intervention and all outcome measures being administered by a single researcher in a face-to-face manner, blinding of assessors was not possible. Our inability to blind assessors and those receiving the intervention may have reduced the overall quality of evidence and increased the risk of bias towards the intervention, however due to the study protocol this was unavoidable.
Conclusion
Incorporating CBT and physical activity behavioural modification interventions into a standard PR programme may provide patients with COPD who exhibit low baseline levels of physical activity and elevated anxiety and/or depression with clinically important improvements in physical activity levels and experiences of physical activity, alongside improvements in exercise capacity, health-related quality of life and anxiety. Further development and delivery of this combined intervention may support the management/treatment of patients with COPD who exhibit high levels of anxiety and/or depression, consequently lowering the risk of hospital admissions, morbidity and mortality, associated with physical inactivity in COPD.
Footnotes
Provenance: Submitted article, peer reviewed.
This study is registered at www.clinicaltrials.gov with identifier number NCT03749655. Individual participant data that underlie the results, reported in this article, will be shared after de-identification. Documents available will include the study protocol, statistical analysis plan and analytic code and will be available following publication to anyone who wishes to access the data.
Conflict of interest: M. Armstrong has no conflicts of interest to disclose for this study.
Conflict of interest: E. Hume has no conflicts of interest to disclose for this study.
Conflict of interest: L. McNeillie has no conflicts of interest to disclose for this study.
Conflict of interest: F. Chambers has no conflicts of interest to disclose for this study.
Conflict of interest: L. Wakenshaw has no conflicts of interest to disclose for this study.
Conflict of interest: G. Burns has received a grant from NIHR for a CBT study.
Conflict of interest: K. Heslop Marshall received a grant from NIHR for a CBT study and director of pivotal healthcare training for CBT skills.
Conflict of interest: I. Vogiatzis is an associate editor of this journal.
References
Articles from ERJ Open Research are provided here courtesy of European Respiratory Society
Full text links
Read article at publisher's site: https://doi.org/10.1183/23120541.00074-2023
Read article for free, from open access legal sources, via Unpaywall:
https://openres.ersjournals.com/content/erjor/early/2023/06/15/23120541.00074-2023.full.pdf
Citations & impact
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/154167266
Article citations
Effect of 12-week head-down strong abdominal breathing on cognitive function in patients with stable chronic obstructive pulmonary disease: a single-centre randomised controlled trial protocol.
Trials, 25(1):351, 30 May 2024
Cited by: 0 articles | PMID: 38816733 | PMCID: PMC11140949
Pulmonary Rehabilitation with and without a Cognitive Behavioral Intervention for Breathlessness in People Living with Chronic Obstructive Pulmonary Disease: Randomized Controlled Trial.
J Clin Med, 12(23):7286, 24 Nov 2023
Cited by: 1 article | PMID: 38068337 | PMCID: PMC10707579
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Clinical Trials
- (2 citations) ClinicalTrials.gov - NCT03749655
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Behavioural modification interventions alongside pulmonary rehabilitation improve COPD patients' experiences of physical activity.
Respir Med, 180:106353, 09 Mar 2021
Cited by: 17 articles | PMID: 33735798
Factors associated with the effect of pulmonary rehabilitation on physical activity in patients with chronic obstructive pulmonary disease.
Geriatr Gerontol Int, 17(1):17-23, 04 Dec 2015
Cited by: 6 articles | PMID: 26634413
Effects of low-intensity exercise and home-based pulmonary rehabilitation with pedometer feedback on physical activity in elderly patients with chronic obstructive pulmonary disease.
Respir Med, 109(3):364-371, 29 Jan 2015
Cited by: 53 articles | PMID: 25682543
Inspiratory muscle training, with or without concomitant pulmonary rehabilitation, for chronic obstructive pulmonary disease (COPD).
Cochrane Database Syst Rev, 1:CD013778, 06 Jan 2023
Cited by: 23 articles | PMID: 36606682 | PMCID: PMC9817429
Review Free full text in Europe PMC

 1,2
1,2 


