Abstract
Free full text

The Impact of Rationing Nursing Care on Patient Safety: A Systematic Review
Associated Data
Abstract
Background
Rationing of nursing care (RONC) has been associated with poor patient outcomes and is a growing concern in healthcare. The aim of this systematic study was to investigate the connection between patient safety and the RONC.
Material/Methods
A thorough search of electronic databases was done to find research that examined the relationship between restricting nurse services and patient safety. The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Two reviewers (M.L. and A.P.) independently screened the titles and abstracts, and full-text articles were assessed for eligibility. Data were extracted, and a quality assessment was performed using appropriate techniques.
Results
A total of 15 studies met the inclusion criteria. The studies included in the review demonstrated a correlation between rationing of nursing care and patient safety. The results of these studies revealed that there is an inverse relationship between rationing of nursing care and patient safety. The review found that when nursing care is rationed, there is a higher incidence of falls, medication errors, pressure ulcers, infections, and readmissions. In addition, the review identified that the work characteristics of nurses, such as workload, staffing levels, and experience, were associated with RONC.
Conclusions
RONC has a negative impact on patient safety outcomes. It is essential for healthcare organizations to implement effective strategies to prevent the RONC. Improving staffing levels, workload management, and communication amo0ng healthcare providers are some of the strategies that can support this.
Background
In recent years, the healthcare industry has experienced a significant shift toward an awareness of the need for improving patient safety and quality of care. Patient safety is a critical aspect of healthcare and is essential in maintaining the well-being of patients [1,2]. However, RONC has become a common problem in healthcare institutions, affecting the quality of patient care and the safety of patients [3,4]. RONC refers to the intentional withholding or delay in provision of nursing care essential to maintaining the health and well-being of patients. This can lead to various adverse events, including medication errors, falls, pressure ulcers, and other complications.
The conceptual model of missed nursing care developed by Kalisch et al clearly states that structural factors that contribute to missed care include resources in the work environment, including material resources, teamwork, and team communication [5]. In a situation where any element is missing or not fully met, this will result in a delay or omission of care. It has been postulated that the most important factors influencing the omission of nursing care are staffing of the ward and lack of teamwork. The Kalisch concept, which considers the omission or lack of nursing care, emphasizes that this is a common threat that generates medical errors that directly affect patient safety. In addition, Schubert et al used a model to show that rationing of care is directly related to patient outcomes. In addition, research on rationing is intended to be a starting point for developing specific organizational strategies and standards of nursing practice necessary to achieve desired outcomes and patient safety [6]. Several studies have investigated the relationship between RONC and patient safety[7,8]. Missed nursing care is a result of many other factors of the nursing staff’s professional functioning, including low job satisfaction, high stress levels, an increase in staff turnover, a rise in job absenteeism, and the risk of burnout [9–11]. Nursing care is rationed based on psychological variables, including life satisfaction and life orientation. Low life satisfaction and a more negative outlook on life have been proven to be associated with a higher incidence of missing nursing care [12,13] Several strategies have suggested the need to address the problem of nursing care rationing and its impact on patient safety. One such strategy is implementation of workload management tools that enable nurses to prioritize care activities and identify patients who require immediate attention. Another strategy is improvement of staffing levels, which can reduce workload and prevent rationing of care [14]. The literature suggests that the discussion of appropriate nurse staffing levels and the measurement of workload is an area of considerable research that has been ongoing for several decades and continues to be assessed and evaluated. Despite the literature available on nurse workload and staffing requirements, there is still no specific method or tool to assess their impact on quality-of-care outcomes, patients, and staff. The issue is still relevant and continues to be included in new studies. It is now suggested that it would be optimal to review the available tools and to consider and develop a way to use them optimally, taking into account costs and consequences [15]. In addition, providing nurses with adequate resources, such as medical equipment and training, can improve their ability to provide safe and high-quality care. In addition to this fostering a positive work environment with opportunities for professional development and support for staff well-being, it can contribute to a reduction rationing and an improvement in patient safety [1,13]. Finally, developing a culture of transparency and open communication can facilitate the reporting and resolution of incidents related to rationing and improve the overall quality and safety of care.
Despite all this information and suggestions, it is still essential to address the growing ethical concerns of nursing care rationing and patient safety. Therefore, it is necessary to explore the factors that contribute to RONC and how it impacts patient safety. A systematic review of the literature on the topic will provide an in-depth analysis of the research conducted in this field, identifying the key factors that contribute to nursing care rationing and how it affects patient safety. This evaluation will offer helpful insights into the subject’s present level of research and make suggestions for further study and application.
Objectives
The objective of this study was to provide a comprehensive and evidence-based understanding of the relationship between RONC and patient safety. This review aimed to identify and synthesize the available literature on the extent and causes of nursing care rationing, its impact on patient safety, and the potential strategies to mitigate its negative effects. By systematically analyzing and synthesizing relevant studies, this review will provide a more detailed and robust understanding of the complex relationship between RONC and patient safety, and thus offer insights and recommendations to support healthcare professionals, policymakers, and researchers to better address this important issue. The results of this review may also contribute to development of evidence-based guidelines and policies to improve patient safety and promote delivery of high-quality nursing care.
Material and Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16,17]. The review protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (registration number: CRD42020201395).
Search Strategy
Two independent reviewers (M.L. and A.P.) conducted a comprehensive search in 6 electronic databases. The search strategy planning is shown in Table 1. The search was restricted to articles published in English from 2010 to the present. The search strategy was adapted to each database.
Table 1
Issue of research interest.
| Relevant databases | Academic Search Ultimate | |||
| CINAHL Complete | ||||
| ERIC | ||||
| MEDLINE | ||||
| International Pharmaceutical Abstracts | ||||
| Health Source: Nursing/Academic Edition | ||||
| Search profile keywords | ‘care left undone’ OR ‘implicit ration*’ OR ‘miss* care’ OR ‘nurs* ration* care’ OR miss* care’ OR ‘omi* care’ OR ‘task* undone’ OR ‘underuse care” unfinis* care’ OR ‘unmet* care’ AND ‘accessibility’ OR ‘adverse outcom*’ OR ‘allocation*’ OR ‘accident*’ OR ‘bedsores’ OR | OR ‘burnout’ OR ‘dissatisfaction’ OR ‘dose’ OR ‘death’ OR ‘environment’ OR ‘error’ OR ‘factor*’ OR‘fall’ OR ‘health consequence*’ OR ‘health outcome’ OR ‘hospital*’ OR ‘infection*’OR ‘in-hospital mortality’ OR ‘information*’ OR ‘injury’ OR ‘instrumental*’ OR ‘management’ OR ‘medical equipment’ OR | OR medication dispensing’ OR ‘medication fall*’ OR ‘mortal*’ OR ‘negative effec* for patient*’ OR ‘neglect*’ OR ‘outcome’ OR ‘patient* advers* event*’ OR ‘patient* incident*’ OR ‘patient-import* outcome*’ OR ‘patient* outcom*’ OR ‘patient* outcom* indicator*’ OR patient* perception* OR ‘patient-related outcom*’ OR | ‘patient* safety’ OR ‘pressure ulcers’ OR prevalence’ OR ‘quality assessment*’ ‘readmissions’ OR ‘report’ OR ‘restraint*’ OR ‘safe rating*’ OR ‘satisfaction’ OR “Setting*’ OR ‘staff*’ OR ‘staffing’ OR ‘support’ OR ‘the shor* and longterm* effect*’ OR ‘workload’ |
Selection Criteria
The inclusion criteria for the studies were: (1) original research studies that evaluated the association between RONC and patient safety and patient outcomes, (2) studies that focused on acute care settings, (3) studies that included registered nurses as participants, and (4) studies published in English language. The exclusion criteria were: (1) studies that did not evaluate the association between RONC and patient safety, (2) studies that focused on non-acute care settings, (3) studies that did not include registered nurses as participants, and (4) studies published in languages other than English.
Data Extraction
Two independent reviewers (M.L. and A.P.) screened the titles and abstracts of the identified articles and selected the articles that met the inclusion criteria. The full-texts of the selected articles were then reviewed, and data were extracted using a pre-defined data extraction form. The data extraction form included the following items: study design, study population, sample size, intervention/exposure, and key findings (Table 1). Discrepancies in the selection of articles and data extraction were resolved through discussion and consensus.
Quality Assessment
The quality of the selected studies was assessed using the Cochrane Risk of Bias tool for randomized controlled trials and the Newcastle-Ottawa Scale for observational studies [18]. The quality assessment was conducted by 2 independent reviewers, and discrepancies were resolved through discussion and consensus.
Data Synthesis
A narrative synthesis was conducted to summarize the findings of the selected studies. The studies were grouped according to the outcome measures, and findings were summarized and presented in tables and figures. Due to the heterogeneity of the studies in terms of research design, demographic, and outcome measures, a meta-analysis was not carried out.
Publication Bias
The funnel plots of the included studies were visually inspected to determine the likelihood of publication bias. Egger’s test was also employed to assess the funnel plots’ asymmetries. Egger’s test evaluates the significance of the constant α of the linear regression equation, where the dependent variable y is the standardized value of the effects of individual studies, and the independent variable x is the precision (ie, the inverse of the estimated standard error). The further away from 0 the value of the coefficient, the greater the asymmetry [19].
Results
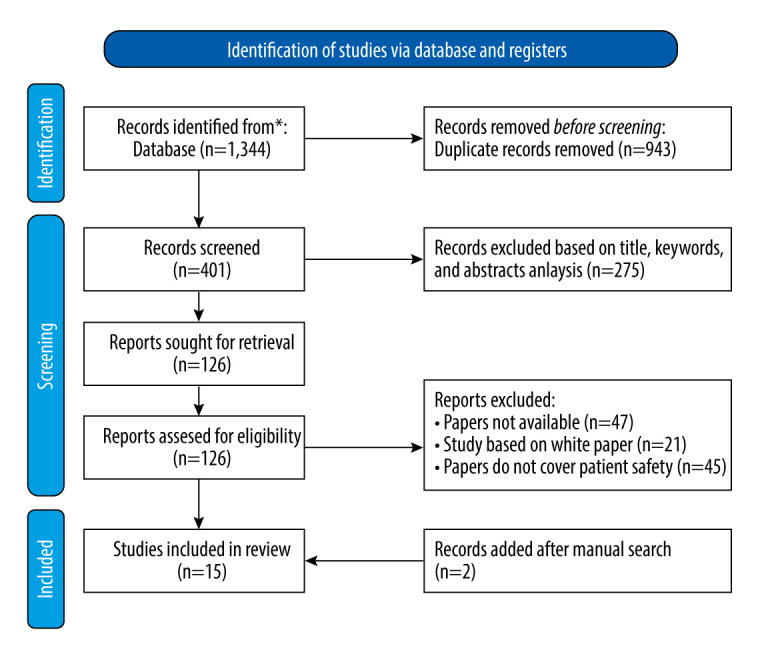
The search strategy for this systematic review involved multiple databases, including Academic Search Ultimate, CINAHL Complete, ERIC, MEDLINE, International Pharmaceutical Abstracts, and Health Source: Nursing/Academic Edition. A total of 1344 records were identified in the first phase, and after the removal of duplicates records, 401 unique papers were analyzed. The second phase involved rejecting 275 records based on title, keywords, and abstract analysis, resulting in 126 papers eligible for comprehensive analysis. From these, 113 records were excluded after a full-text analysis, resulting in 13 full-text papers eligible for detailed examination. Additionally, a manual search was conducted on various search engines and using citations identified manually in the selected articles that were not in the original query results. This step aimed to ensure that relevant papers that met the scope of the review were included. We finally included and analyzed 15 full-text papers. Figure 1 provides a flow diagram that reports the outcomes obtained in each phase, and Table 2 presents all the articles selected and analyzed.
Table 2
Extracted data from the articles.
| Article | Citation and year | Study design | Study population | Sample size | Aim of the study | Research instrument | Statistical tests | Intervention/exposure | Results |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Gurková et al. 2020 | A cross-sectional study | European nurses from four countries (Croatia, the Czech Republic, Poland and Slovakia) | N=1353 | Nurses’ perceptions of the safety climate in four selected central European countries; relationship between safety climate and unfinished nursing care | The Hospital Survey on Patient Safety Culture; the Perceived Implicit Rationing of Nursing Care | Descriptive statistic Pearson’s correlations and multipleregression. Cronbach’salpha coefficient. AP-value<0.05 | ‘Perceived Patient Safety’ and ‘Reporting of Incident Data’ | Significant differences were found between countries in all unit/hospital/outcome dimensions.‘Perceived Patient Safety’ and ‘Reporting of Incident Data’ were associated with aspects of ‘OrganizationalLearning’ and ‘Feedback and Communication about Error’. Higher prevalence of unfinished nursing care is associated with more negative perceptions of patient safety climate |
| 2 | Ausserhofer et al. 2013 | Multicenter-cross sectional | Registered nurses (RNs) working in 132 surgical, medical and mixed surgical-medical units within 35 Swiss acute care hospitals | N=1630 | Explore the relationship between PSC and patient outcomes in Swiss acute care hospitals | The 9 item Safety Organizing Scale | Multilevel multivariate logistic regression | Patient safety climate and patient outcomes | In none of our regression models was PS C a significant predictor for any of the seven patient outcomes |
| 3 | Dhainiet et al. 2020 | Longitudinal study | RNs | N=90 | Explore the trends and variability of rationing of care per shift between individual nurses, services over time, and its relationship with work environment factors | The Basel extent of rationing of nursing care (BERNCA) | Intraclass correlation coefficients (ICC); inear mixed models | Rationing of care per shift | Rationing of care was positively associated with nurses’ self-perceived workload in both shifts, but not with patient-to-nurse ratios |
| 4 | Papastavrou et al. 2014 | Descriptive, correlational design | Patients and nurses from ten medical and surgical units of five general hospitals | N=352 patients and 318 nurses | Explore whether patient satisfaction is linked to nurse-reported rationing of nursing care and to nurses’perceptions of their practice environment; identify the threshold score of rationing by comparing the level of patient satisfaction factors acrossrationing levels | The BERNCA scale, the RPPE scale, the Patient Satisfaction scale to | Kendall’s correlation coefficient, multiple regression analysis | Patient satisfaction link to nurse-reported rationing of nursing care | care rationing and work environment were related to patient satisfaction, even after controlling for nurse and patient characteristic; even at the lowest level of rationing (i.e. 0.5) patients indicated low satisfaction |
| 5 | Jarosz et al. 2022 | Cross-sectional study | Nurses working in urology departments | N=130 | Assess the level of rationing care, fatigue, job satisfaction and occupational burnout | Link Burnout Questionnaire, Job Satisfaction Scale, Nursing Care Rationing Scale and Modified Fatigue Impact Scale | The basic descriptive statistics, the Kolmogorov-Smirnov distribution normality test, a series of correlation analyzes with the Pearson r coefficient, the Student’s t-test for independent samples and linear regression analysis | Level of rationing care, fatigue, job satisfaction and occupational burnout | The level of rationing nursing care in urology departments is similar to that in other departments |
| 6 | Renner et al. 2022 | Time-series cross-sectional analysis | RNs from nursing homes | N=3269 | Describe changes in levels and patterns of implicit rationing of nursing care in Swiss nursing homes over time | The Basel Extent of Rationing of Nursing Care instrument | Multiple linear mixed models | Changes in levels and patterns of implicit rationing of nursing care | Overall increases of rationing of care activities over the five-year period studied, with documentation and social activities most rationed at both measurement points |
| 7 | Schubert et al. 2013 | Cross sectional multi-center study | RNs from 35 acute care hospitals | N=1633 | Describe the levels and association of implicit rationing of nursing care in Swiss acute care hospitals | Basel Extent of Rationing of Nursing Care (BERNCA) instrument. | three level regression models | Associations between nine selected potential rationing predictors and implicit rationing of nursing care | better unit level staff resource adequacy and a more favorable hospital level safety climate were both consistently significantly associated with lower rationing levels |
| 8 | Gil et al. 2022 | Observational, analytical, descriptive, concurrent and quantitative study | Nursing professionals from eight Inpatient Units | N=104 | Relate nursing workloads to professional job satisfaction | The Overall Job Satisfaction scale | the Mann-Whitney U test, the Kruskal-Wallis K test, Cohen’s d | Nursing workloads to professional job satisfaction | Higher levels of satisfaction in the variables “relationship with immediate boss” and “relationship with fellow workers”, and lower levels in “relationship with senior management” and “organizational system of the unit” |
| 9 | Młynarska et al. 2020 | Ccross-sectional survey | Anaesthesiological nurses | N=150 | Assess the rationing level of nursing care among staff in the intensive care units | The PIRNCA, The Modified Fatigue Impact Scale (MFIS) | The Mann-Whitney test; Kruskal-Wallis test; the Spearman correlation coefficient, the regression model | The rationing level of nursing care | The higher the level of fatigue, the greater the rationing of care and the less satisfaction from work |
| 10 | Gehriet et al. 2021 | Multicenter observational study | Psychiatric hospital RNs | N=1300 | Describe health care quality by exploring hospital structures such as nurse staffing and the work environment | The nurse survey consisted of 164 items covering three dimensions-work environment, patient safety climate, and the rationing of care. The unit-level questionnaire included 57 items, including the number of beds, number of nurses, and nurses’ education levels | Multilevel regression linear mixed models and generalized linear mixed models | Nurse staffing and the work environment | Study will contribute to improvement strategies for nurses’ work environments and patient experiences in Swiss psychiatric hospitals |
| 11 | Witczak et al. 2021 | Cross-sectional study | RNs | N=245 | Determine the extent of nursing care rationing and its relationship with patient safety | Hospital Survey on Patient Safety Culture (HSOPSC) and the Perceived Implicit Rationing of Nursing Care (PIRNCA) | Hierarchical multiple regression analysis | Nursing care rationing and its relationship with patient safety | The PIRNCA scores were negatively correlated with the HSOPSC subscales;the PIRNCA scores among the internal unit were significantly higher than in the intensive care and surgical units |
| 12 | Zhu et al. 2019 | Cross-sectional research | RNs and Patients | N=nurse (n=7802) and Patient (n=5430) | Test the mediation effect of rationing of nursing care (RONC) and the relationship this has between nurse staffing and patient outcomes | The China Nurse Survey | Logistic regression analyses; Structural equation modeling (SEM) | Mediation effect of rationing of nursing care | A lack of nurse staffing leads to RONC, which leads to poorer patient outcomes |
| 13 | Rochefort et al. 2016 | Cross-sectional survey | RNs working in one of 7 NICUs in the province of Quebec | N=285 | Assess these relationships | The Neonatal Extent of Work Rationing Instrument (NEWRI) | Multivariable linear regression | Rationing of nursing interventions | The rationing of nursing interventions appears to influence parent and infant readiness for discharge, as well as pain control in NICUs |
| 14 | Uchmanowicz et al. 2021 | Cross-sectional survey | RNs | N=547 | Assess the effects of nurses’ life satisfaction and life orientation on the level of nursing care rationing | The Basel Extent of Rationing of Nursing Care-R (BERCA-R), the Satisfaction with Life Scale (SWLS) and the Life Orientation Test (LOT-R) | Bivariate analyses | Life satisfaction and life orientation on the level of nursing care rationing | More pessimistic nurses with low and moderate levels of life satisfaction, and those with a neutral life orientation, presented with significantly higher BERCA-R scores |
| 15 | Duffy et al. 2018 | Cross-sectional correlational study | RNs | N=138 | Describe and evaluate the factors associated with missed nursing care in an acute care community hospital | The MISSCARE survey; the Practice Environment Scale Nursing Work Index (PES-NWI) | Regression mode | Factors associated with missed nursing care | The extent of missed nursing care is consistent with other studies, was greater on medical-surgical and telemetry units compared with specialty units, and was negatively associated with staffing/resources, satisfaction with current position |
Characteristics of the Included Studies
The 15 articles included in the analysis were published between 2010 and 2022, with 12 of the articles published between 2015 and 2022 [1,2,7,8,12,20–23,23–28]. The study designs varied from cross-sectional to longitudinal, observational, and quantitative. The study populations included registered nurses (RNs) from various healthcare settings such as medical, surgical, mixed surgical-medical, and psychiatric hospitals, nursing homes, and inpatient units. The sample sizes ranged from 90 to 7802 participants. The main intervention/exposure variables included perceived patient safety, incident report data, patient safety climate, rationing of care per shift, patient satisfaction, level of rationing of care, nursing workloads, nurse staffing, missed nursing care, and nursing interventions. Overall, the studies aimed to investigate the relationship between RONC and various outcomes such as patient safety, patient satisfaction, nursing workloads, professional job satisfaction, and missed nursing care.
Several studies examined the association between nursing care rationing and patient outcomes. Ausserhofer et al found that implicit RONC was a more robust predictor of patient outcomes than patient safety climate (PSC). Patient satisfaction probability significantly decreased as implied rationing of nursing services increased, and there was a significant increase in the odds of nurse-reported medication errors, bloodstream infections, and pneumonia [21]. In the article by Papastavrou et al, care rationing and work environment were linked to patient satisfaction even after controlling for nurse and patient variables. Even at the lowest degree of rationing, the modified regression model findings demonstrated that patients indicated low satisfaction [22]. Zhu et al found that nurses working in units with lower nurse-to-patient ratios reported higher scores on RONC, illustrating an increased level of withheld nursing care [26]. Rochefort, Bailey, and Sean revealed that 54.4% of respondents said pain was not well managed on their unit, and 15.2% of respondents believed parents and infants were not prepared for their discharge from NICU. According to multivariate analyses, reports of rationing parental support and teaching, as well as infant comfort care, were linked to less favorable perceptions of neonatal pain control, although RNs’ assessments of parent and infant preparedness for discharge was inversely correlated with limiting discharge planning [28]. The results of Duffy et al on deficient nursing care were consistent with other studies, showing it was more common on telemetry and medical-surgical units than on specialist units [27]. Some previous studies have investigated the rate of nursing care rationing and its association with workload and job satisfaction. Dhaini et al found that the rate of rationing of nursing activities exceeded 10% during day and night shifts. Rationing of care was positively associated with nurses’ self-perceived overwork in both shifts, but not with patient-to-nurse ratios [2]. Jarosz et al found that while nursing care is rarely rationed, the experience of fatigue ranged between sometimes and often. Job satisfaction is at an average level, and the level of rationing nursing care in urology departments is similar to that in other departments [7]. Schubert et al found that 98% of the participating nurses reported that they had to ration at least one of the nursing tasks listed in the Basel Extent of Rationing of Nursing Care for Nursing Homes (BERNCA). The mean rationing level of 1.69 indicates that on average the nurses reported ‘rarely’ being unable to perform the nursing tasks listed in the BERNCA [29]. Uchmanowicz et al found that nurses with low and moderate levels of life satisfaction, as well as those with a pessimistic or neutral life orientation, had higher scores on the BERCA-R than more optimistic nurses with high levels of life satisfaction [8]. Finally, Renner et al found that there were overall increases of rationing of care activities over the 5-year period studied, with documentation and social activities most rationed at both measurement points, and a considerable increase in rationing of activities of daily living was observed [23]. Młynarska et al found that sociodemographic factors did not affect the rationing level of nursing care in the intensive care unit; the average quality of patient care was 6.05/10 points, while the average job satisfaction rating was 7.13/10 points [25].
Discussion
The literature shows that restricting nursing care has a detrimental effect on patient safety. The level of missing nurse care was found to be greater on medical-surgical and telemetry units than on specialized units, which is consistent with earlier studies. The level of RONC was positively associated with nurses’ self-perceived overwork, but patient-to-nurse ratios were not.
The literature suggests there is an urgent need for nurse leaders to take action to address the issue of RONC. The results of previous studies also indicate that cross-cultural comparisons allow for the examination of differences and similarities in safety dimensions across countries [22]. A study found that areas with potential for implementing strategies for improvement in 4 countries studied were staffing, non-punitive response to errors, and teamwork across hospital units [20].
Studies indicate that higher prevalence of understaffed nursing care is associated with more negative perceptions of patient safety [25]. Implicit RONC was also the most reliable predictor of patient satisfaction, nurse-reported prescription mistakes, bloodstream infections, and pneumonia. Higher levels of implicit RONC led to a significant decrease in the odds of patient satisfaction and a significant increase in the odds of nurse-reported medication errors, bloodstream infections, and pneumonia after controlling for major organizational variables and hierarchical data structure [2].
The findings imply that general medical/surgical units should monitor nursing care levels, as this could support the identification of any imbalances in the “work system,” such as insufficient nurse staffing or a lack of a skill mix to meet patients’ needs [26]. It may be possible for nurse managers to use measures to keep rationing at a level where patient safety is not compromised by identifying the thresholds at which it begins to negatively affect patient outcomes.
Throughout the course of the 10 years covered by the studies we included in this review, there was an overall increase in the rationing of care activities, with social and documentation activities showing the greatest rationing at both assessment periods. Moreover, a large rise in rationing of daily living activities was seen. The increased rates of RONC and long-term deterioration of staff resources are a troubling development, especially considering their potential detrimental effects on residents and caregivers [21]. Policy makers and nursing home management should consider routinely monitoring RONC to evaluate the quality of nursing home care and determine the proper staffing levels and skill combinations.
The studies we reviewed offer compelling evidence of the detrimental effects of nursing care rationing on patient safety. The results suggest that the issue of RONC needs to be urgently addressed by nurse leaders [22]. Regular monitoring of the RONC may help detect imbalances in the “work system,” such as inadequate nurse staffing or skill mix levels to meet patients’ needs, allowing nurse managers to implement interventions to maintain rationing at a level that mitigates any risk to patient safety.
Finally, we would like to emphasize the importance of the socio-ecological domain in the rationing of care. Jones et al [30] emphasized that the rationing of care as a global phenomenon is a complex socio-ecological problem that requires constant interdisciplinary exchange and consolidation of knowledge. Rationing of care is constantly juxtaposed with the problem of allocating social resources and ensuring quality health care for all. The authors point out that the sustainable development of care rationing requires cooperation on many levels, from computer science and engineering to psychology and ethics, for optimal understanding of unfinished care. Collaboration across many disciplines is necessary, and it seems crucial to recognize the activities that are being undertaken. These activities can be carried out in an additive (multidisciplinary), synthetic, and harmonized (interdisciplinarity) or integrated and transcendent (transdisciplinarity) interdisciplinary way [31]. Gidden’s proposed structure, covering both the social system and social psychology, despite its limitations and criticism, can constructively lead to a more comprehensive and unified theory [30].
Study Limitations
Although we tried to include all relevant articles in this review, many articles could not be included due to the researchers’ lack of access to some databases; therefore, only open access English language articles were included. Based on researchers’ knowledge, even after searching various databases and sources, there is no adequate definition of nursing care rationing. In addition, it is recommended that researchers conduct more qualitative studies to develop an appropriate definition of nursing care rationing. An important aspect of care rationing research is structuration theory, which should be recommended in further research.
Conclusions
The results and conclusions from the studies we reviewed indicate that rationing of nursing care is a widespread issue in healthcare settings across different countries and specialties. The amount of nursing care that was missing is consistent with other research, with greater levels observed in medical-surgical and telemetry units, and higher levels of rationing were negatively associated with staffing/resources, job satisfaction, and collegial nurse-physician interactions.
The present review also indicates that higher levels of implicit rationing of nursing care are associated with significant decreases in patient satisfaction and significant increases in the odds of nurse-reported medication errors, bloodstream infections, and pneumonia. Determining the levels at which rationing begins to have a negative impact on patient outcomes may allow nurse managers to introduce interventions to keep rationing at a level where patient safety is not jeopardized. The variability in rationing activities was found to be associated with nurses’ self-perceived workload.
Implications
The present study highlights the need for urgent nurse leader action and future research to address the issue of nursing care rationing and to improve patient outcomes. Nursing homes, hospitals, and other healthcare settings need to consider regular monitoring of rationing of nursing care to assess nursing home care quality and determine adequate staffing levels and skill mixes. Additionally, employers should develop implementation programs for young workers to avoid burnout and invest in factors increasing nurses’ satisfaction, such as improving workplace culture. The links among organizational and environmental factors, care rationing, and patient satisfaction must also be confirmed by additional research.
Availability of Data and Materials
All relevant data are included in this article. If necessary, it is possible to contact the corresponding author to obtain additional materials.
Abbreviations
| PSC | patient safety climate |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| RONC | rationing of nursing care |
| RNs | registered nurses |
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: This research was funded by the Ministry of Science and Higher Education of Poland under the statutory grant of the Wrocław Medical University (SUBZ.E250.23.020)
References
Articles from Medical Science Monitor: International Medical Journal of Experimental and Clinical Research are provided here courtesy of International Scientific Information, Inc.
Citations & impact
This article has not been cited yet.
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/158644120
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.
Cochrane Database Syst Rev, 2(2022), 01 Feb 2022
Cited by: 12 articles | PMID: 36321557 | PMCID: PMC8805585
Review Free full text in Europe PMC
Rationing of Nursing Care and Its Relationship with Nurse Staffing and Patient Outcomes: The Mediation Effect Tested by Structural Equation Modeling.
Int J Environ Res Public Health, 16(10):E1672, 14 May 2019
Cited by: 16 articles | PMID: 31091660 | PMCID: PMC6572194
Beyond the black stump: rapid reviews of health research issues affecting regional, rural and remote Australia.
Med J Aust, 213 Suppl 11:S3-S32.e1, 01 Dec 2020
Cited by: 10 articles | PMID: 33314144
Rationing of nursing care and nurse-patient outcomes: a systematic review of quantitative studies.
Int J Health Plann Manage, 29(1):3-25, 07 Jan 2013
Cited by: 64 articles | PMID: 23296644
Review

 2,5,6,E,G and
2,5,6,E,G and