Abstract
Background
The inability to predict treatment response of colorectal cancer patients results in unnecessary toxicity, decreased efficacy and survival. Response testing on patient-derived organoids (PDOs) is a promising biomarker for treatment efficacy. The aim of this study is to optimize PDO drug screening methods for correlation with patient response and explore the potential to predict responses to standard chemotherapies.Methods
We optimized drug screen methods on 5-11 PDOs per condition of the complete set of 23 PDOs from patients treated for metastatic colorectal cancer (mCRC). PDOs were exposed to 5-fluorouracil (5-FU), irinotecan- and oxaliplatin-based chemotherapy. We compared medium with and without N-acetylcysteine (NAC), different readouts and different combination treatment set-ups to capture the strongest association with patient response. We expanded the screens using the optimized methods for all PDOs. Organoid sensitivity was correlated to the patient's response, determined by % change in the size of target lesions. We assessed organoid sensitivity in relation to prior exposure to chemotherapy, mutational status and sidedness.Results
Drug screen optimization involved excluding N-acetylcysteine from the medium and biphasic curve fitting for 5-FU & oxaliplatin combination screens. CellTiter-Glo measurements were comparable with CyQUANT and did not affect the correlation with patient response. Furthermore, the correlation improved with application of growth rate metrics, when 5-FU & oxaliplatin was screened in a ratio, and 5-FU & SN-38 using a fixed dose of SN-38. Area under the curve was the most robust drug response curve metric. After optimization, organoid and patient response showed a correlation coefficient of 0.58 for 5-FU (n = 6, 95% CI -0.44,0.95), 0.61 for irinotecan- (n = 10, 95% CI -0.03,0.90) and 0.60 for oxaliplatin-based chemotherapy (n = 11, 95% CI -0.01,0.88). Median progression-free survival of patients with resistant PDOs to oxaliplatin-based chemotherapy was significantly shorter than sensitive PDOs (3.3 vs 10.9 months, p = 0.007). Increased resistance to 5-FU in patients with prior exposure to 5-FU/capecitabine was adequately reflected in PDOs (p = 0.003).Conclusions
Our study emphasizes the critical impact of the screening methods for determining correlation between PDO drug screens and mCRC patient outcomes. Our 5-step optimization strategy provides a basis for future research on the clinical utility of PDO screens.Free full text

Organoids as a biomarker for personalized treatment in metastatic colorectal cancer: drug screen optimization and correlation with patient response
Abstract
Background
The inability to predict treatment response of colorectal cancer patients results in unnecessary toxicity, decreased efficacy and survival. Response testing on patient-derived organoids (PDOs) is a promising biomarker for treatment efficacy. The aim of this study is to optimize PDO drug screening methods for correlation with patient response and explore the potential to predict responses to standard chemotherapies.
Methods
We optimized drug screen methods on 5–11 PDOs per condition of the complete set of 23 PDOs from patients treated for metastatic colorectal cancer (mCRC). PDOs were exposed to 5-fluorouracil (5-FU), irinotecan- and oxaliplatin-based chemotherapy. We compared medium with and without N-acetylcysteine (NAC), different readouts and different combination treatment set-ups to capture the strongest association with patient response. We expanded the screens using the optimized methods for all PDOs. Organoid sensitivity was correlated to the patient’s response, determined by % change in the size of target lesions. We assessed organoid sensitivity in relation to prior exposure to chemotherapy, mutational status and sidedness.
Results
Drug screen optimization involved excluding N-acetylcysteine from the medium and biphasic curve fitting for 5-FU & oxaliplatin combination screens. CellTiter-Glo measurements were comparable with CyQUANT and did not affect the correlation with patient response. Furthermore, the correlation improved with application of growth rate metrics, when 5-FU & oxaliplatin was screened in a ratio, and 5-FU & SN-38 using a fixed dose of SN-38. Area under the curve was the most robust drug response curve metric. After optimization, organoid and patient response showed a correlation coefficient of 0.58 for 5-FU (n =
= 6, 95% CI -0.44,0.95), 0.61 for irinotecan- (n
6, 95% CI -0.44,0.95), 0.61 for irinotecan- (n =
= 10, 95% CI -0.03,0.90) and 0.60 for oxaliplatin-based chemotherapy (n
10, 95% CI -0.03,0.90) and 0.60 for oxaliplatin-based chemotherapy (n =
= 11, 95% CI -0.01,0.88). Median progression-free survival of patients with resistant PDOs to oxaliplatin-based chemotherapy was significantly shorter than sensitive PDOs (3.3 vs 10.9
11, 95% CI -0.01,0.88). Median progression-free survival of patients with resistant PDOs to oxaliplatin-based chemotherapy was significantly shorter than sensitive PDOs (3.3 vs 10.9 months, p
months, p =
= 0.007). Increased resistance to 5-FU in patients with prior exposure to 5-FU/capecitabine was adequately reflected in PDOs (p
0.007). Increased resistance to 5-FU in patients with prior exposure to 5-FU/capecitabine was adequately reflected in PDOs (p =
= 0.003).
0.003).
Conclusions
Our study emphasizes the critical impact of the screening methods for determining correlation between PDO drug screens and mCRC patient outcomes. Our 5-step optimization strategy provides a basis for future research on the clinical utility of PDO screens.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13046-024-02980-6.
Introduction
Therapeutic options for the treatment of patients with metastatic colorectal cancer (mCRC) are expanding rapidly, but heterogeneity in treatment responses, ranging from 10 to 90%, remains a fundamental challenge [1–4]. Predicting to which treatment a patient will respond is one of the holy grails in cancer research for enabling personalized care and improving patient survival. Despite considerable research in the field of predictive biomarkers, with the main focus on genetic biomarkers, there are clinically limited means to predict treatment efficacy. Genetic biomarkers do not predict response to chemotherapy, the cornerstone of treatment of mCRC. Additionally, genetic biomarkers like RAS and BRAF mutational status do not robustly predict treatment response for targeted treatments [5]. As a result, many patients receive ineffective, costly drugs and suffer unnecessary toxicities.
A promising predictive biomarker is in vitro response testing using patient-derived organoids (PDOs) [6, 7]. PDOs are (cancer) stem-cell derived, 3D self-organizing and proliferating structures comprised of epithelial cells representing their corresponding tumour genomically and phenotypically and are well suited for (high throughput) drug screening [7–11]. This makes PDOs a novel promising biomarker to predict treatment response for various cancer and treatment types, and a valuable screening platform to identify new treatment types [7, 12, 13]. Previous studies involving colorectal cancer (CRC) patients have demonstrated a correlation between organoid response and patient response to different forms of chemotherapy and targeted treatment [7, 14–22]. However, these results are not consistent, especially not for oxaliplatin which is one of the main treatments for mCRC [20, 23]. Variation between studies arise by using different combination screen set-ups, different response evaluation readouts and differences in components used in the screening medium [6, 7, 20, 24–26]. Especially the use of N-acetyl cysteine (NAC) in organoid culture media is point of debate [11]. NAC is known to interfere with platinum-based chemotherapy [27, 28] and notably studies that used NAC in oxaliplatin screening found no correlation between organoid sensitivity and patient response [20, 23]. This signals the need for first improving and standardizing drug screening methodologies before PDO screens can reliably be prospectively tested as biomarker in the clinic.
In this study, we aim to optimize the PDO drug screening methods with regards to screening medium, combination screen set-up, drug screen readout, curve fitting and drug response curve metrics. Subsequently, we explore if these optimized PDO screens can adequately predict treatment response in patients for standard-of-care systemic chemotherapies 5-FU/capecitabine, irinotecan- and oxaliplatin-based combination treatment. In addition, we investigate whether clinical factors, like mutational status, primary tumour location (sidedness) and prior chemotherapy treatment affect organoid sensitivity.
Methods
Study design
We included organoids of 23 patients based on the following criteria: diagnosed with mCRC, tissue for organoid culture was obtained prior to receiving a new line of standard-of-care systemic therapy for metastatic disease (either from primary tumour or metastatic disease) and available clinical data (including treatments given, response scans and vital status). Tissue samples were collected during surgery or fine-needle biopsies within the Biobanking protocol HUB-Cancer (TCBIO #12–093, n =
= 15) or within the prospective clinical trial Organoids to Predict Therapy Response In Colorectal Cancer (OPTIC [29] #17–356, n
15) or within the prospective clinical trial Organoids to Predict Therapy Response In Colorectal Cancer (OPTIC [29] #17–356, n =
= 8). Written informed consent was obtained prior to study inclusion. We first optimized drug screen methods, by examining the optimal screening medium, readout type, curve fitting, drug response curve (DRC) metrics and combination screen set-up, and we evaluated whether the optimization steps affect the correlation of the PDO screens with patient response (Fig. 1). After drug screen optimization on 5–11 PDOs per condition, we expanded the screens for the complete set of 23 PDOs and assessed the correlation with clinical response per treatment category. Additionally, we evaluated organoid sensitivity in relation to prior exposure to chemotherapy, mutational status and sidedness.
8). Written informed consent was obtained prior to study inclusion. We first optimized drug screen methods, by examining the optimal screening medium, readout type, curve fitting, drug response curve (DRC) metrics and combination screen set-up, and we evaluated whether the optimization steps affect the correlation of the PDO screens with patient response (Fig. 1). After drug screen optimization on 5–11 PDOs per condition, we expanded the screens for the complete set of 23 PDOs and assessed the correlation with clinical response per treatment category. Additionally, we evaluated organoid sensitivity in relation to prior exposure to chemotherapy, mutational status and sidedness.
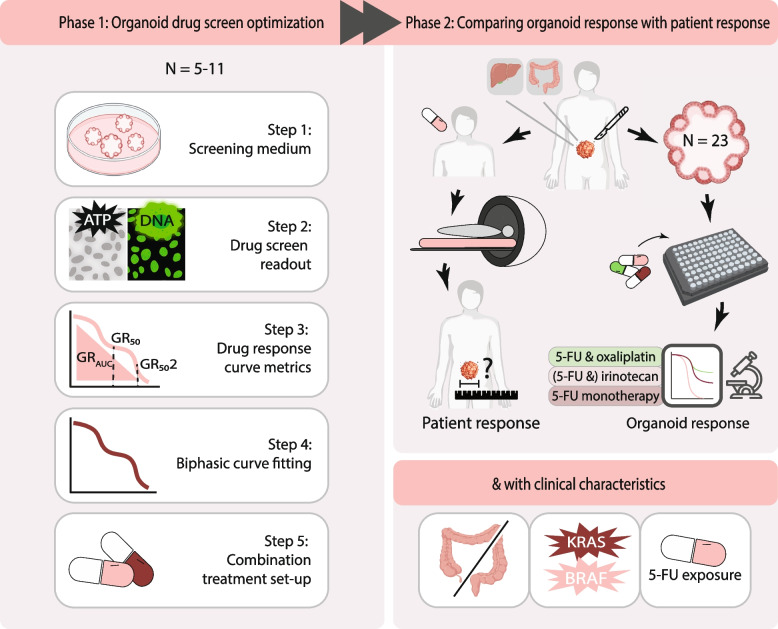
Schematic overview of the study. Tissue from metastatic and primary CRC tumours was obtained via resection or biopsy prior to starting a new line of systemic treatment. PDOs were cultured and screened for standard-of-care treatments while the patient received standard systemic treatment. PDO drug screens were optimized by comparing various methods using a limited set of 5–11 PDOs, either among one another or by correlation with patient response. For all patients, organoid and patient response were compared for treatment given after the organoid was established
Clinical data collection
Clinical data was collected from the electronic patient database by data managers who were blinded for the drug screen response data. The following variables were collected: sex, date of primary and metastatic disease diagnosis, number and location of metastases upon diagnosis of metastatic disease, TNM status, mismatch repair status, mutational status of the tumour (including RAS and BRAF status), and sidedness of the primary tumour (defined as right-sided (coecum-transverse colon), left-sided (splenic flexure-sigmoid) and rectosigmoid/rectal. The mutation status has been determined by NGS panels Ion Torrent PGM Cancer Hotspot panel v2Plus/Plus2/Plus3, mMIPs PATH gene panel combined with SeqNext or AvL Panel V1.2. Class I and II BRAF mutations were considered pathogenic, but not Class III [30]. RAS mutations included KRAS amplifications. Treatment information was collected, including primary tumour resection, local treatment of metastases (including metastasectomy or ablation), adjuvant chemotherapy (type treatment received), and the type and duration of treatment for each systemic palliative therapy line given. Chemotherapy exposure prior to organoid establishment was defined as any given systemic treatment including adjuvant treatment. A radiologist, who was blinded for the organoid screen data, reassessed all CT scans, for each treatment line according to RECIST 1.1. Clinical response on treatment was defined as the percentage size change of all target lesions during treatment, compared to the baseline scan. Progression-free survival for each treatment line was determined as the days between the start of a given treatment and the date of progressive disease on the response scan. If a patient received local treatment for metastatic target lesions, the progression-free survival date was censored for the date of the local treatment.
Organoid culture isolation and establishment
PDO isolation was performed as van de Wetering et al. (2015) described [10]. PDOs were passaged using mechanical dissociation by pipetting and enzymatic dissociation with TrypLE Express (Gibco, Breda, the Netherlands, #12604021) for 5–10 minutes at 37
minutes at 37 °C, washed using organoid culturing medium and re-plated by embedding in a solution of ice-cold Matrigel (Corning, Amsterdam, the Netherlands, #356231) (70%) and organoid culturing medium (Supplementary Table 1, Additional file 1) and plated as droplets on a pre-warmed 6-well plate. After solidification of the Matrigel, organoid culturing medium, containing Rho-kinase inhibitor (10
°C, washed using organoid culturing medium and re-plated by embedding in a solution of ice-cold Matrigel (Corning, Amsterdam, the Netherlands, #356231) (70%) and organoid culturing medium (Supplementary Table 1, Additional file 1) and plated as droplets on a pre-warmed 6-well plate. After solidification of the Matrigel, organoid culturing medium, containing Rho-kinase inhibitor (10 μM, Abmole Bioscience, Brussels, Belgium, #M1817), was added to the plates. The organoid culture medium was refreshed three times per week. Organoid identity was confirmed using a single-nucleotide polymorphism (SNP) array targeting 64 SNPs using TagMan OpenArray technology in combination with the QuantStudio 12
μM, Abmole Bioscience, Brussels, Belgium, #M1817), was added to the plates. The organoid culture medium was refreshed three times per week. Organoid identity was confirmed using a single-nucleotide polymorphism (SNP) array targeting 64 SNPs using TagMan OpenArray technology in combination with the QuantStudio 12 K Flex Real-Time PCR System at the Utrecht Sequencing Facility (USEQ). We calculated genetic distances of PDO DNA versus blood DNA, assigning values based on SNP comparisons (1 for XX vs XY and YY vs XY, 2 for XX vs YY, −
K Flex Real-Time PCR System at the Utrecht Sequencing Facility (USEQ). We calculated genetic distances of PDO DNA versus blood DNA, assigning values based on SNP comparisons (1 for XX vs XY and YY vs XY, 2 for XX vs YY, − 2 for no call, and
2 for no call, and ±
± 0.333 for invalid calls). PDOs with a genetic distance <
0.333 for invalid calls). PDOs with a genetic distance < 5 were included in the drug screens.
5 were included in the drug screens.
Organoid in vitro drug screens
The timeline of the drug screen was as follows: On day − 1, PDOs were sheared and re-plated. Day 0, PDOs were harvested by incubating with 1
1, PDOs were sheared and re-plated. Day 0, PDOs were harvested by incubating with 1 mg/mL Dispase II (Life Technologies Europe B.V., Zuid-Holland, the Netherlands, #17105041) for 30
mg/mL Dispase II (Life Technologies Europe B.V., Zuid-Holland, the Netherlands, #17105041) for 30 minutes at 37
minutes at 37 °C, washed twice using organoid culturing medium with Rho-kinase inhibitor, filtered using a 100 and 20
°C, washed twice using organoid culturing medium with Rho-kinase inhibitor, filtered using a 100 and 20 μm mesh filter to collect the PDOs which have passed through the 100
μm mesh filter to collect the PDOs which have passed through the 100 μm filter but not through the 20
μm filter but not through the 20 μm filter, to remove debris and single cells. PDOs were resuspended in organoid screening medium with Rho-kinase inhibitor (5
μm filter, to remove debris and single cells. PDOs were resuspended in organoid screening medium with Rho-kinase inhibitor (5 μM, Abmole Bioscience, Brussels, Belgium, #M1817) with 5% Matrigel® for a final 125,000 PDOs/20
μM, Abmole Bioscience, Brussels, Belgium, #M1817) with 5% Matrigel® for a final 125,000 PDOs/20 mL concentration. The organoid screening medium was composed of the organoid culture medium (Supplementary Table 1, Additional file 1) with the following adjustments: 1
mL concentration. The organoid screening medium was composed of the organoid culture medium (Supplementary Table 1, Additional file 1) with the following adjustments: 1 ng/mL human recombinant EGF (Sigma-Aldrich, #A9165) and 10
ng/mL human recombinant EGF (Sigma-Aldrich, #A9165) and 10 ng/mL heregulin (Peprotech, London, UK, #100–03) to avoid interference by epidermal growth factor (EGF) with panitumumab sensitivity. Using an automated Multidrop™ Combi Reagent Dispenser, 40
ng/mL heregulin (Peprotech, London, UK, #100–03) to avoid interference by epidermal growth factor (EGF) with panitumumab sensitivity. Using an automated Multidrop™ Combi Reagent Dispenser, 40 μL of PDO suspension was dispensed in clear-bottomed, black-walled 384-well plates with ultra low-attachment coating (Corning, Zuid-Holland, the Netherlands, #4588). Drug concentrations were selected to obtain a complete drug response curve for the majority of PDOs, ranging from no growth inhibition at the lowest concentrations and near complete cell death at the highest concentrations. Drug concentration ranges included concentrations within the clinically relevant range [31]. Drug concentrations in combination screens were selected based on equal contribution in growth inhibition of both compounds. A 10-point concentration range of the treatments (Supplementary Table 2, Additional file 1), the positive control (Staurosporine) and negative control 1% (Dimethyl sulfoxide, Phosphate Buffered Saline or combination depending on the solvent used), were dispensed in technical quadruplicates using a Tecan Fluent liquid handler or Tecan D300E dispenser. The following commonly used CRC treatments were screened: 5-fluorouracil (5-FU), SN-38 (active metabolite of irinotecan), oxaliplatin, panitumumab, combination treatment 5-FU & oxaliplatin, and combination treatment 5-FU & SN-38. On day 5, readouts were obtained by quantifying cell viability using CellTiter-Glo 3D (Promega, #G9681, 40
μL of PDO suspension was dispensed in clear-bottomed, black-walled 384-well plates with ultra low-attachment coating (Corning, Zuid-Holland, the Netherlands, #4588). Drug concentrations were selected to obtain a complete drug response curve for the majority of PDOs, ranging from no growth inhibition at the lowest concentrations and near complete cell death at the highest concentrations. Drug concentration ranges included concentrations within the clinically relevant range [31]. Drug concentrations in combination screens were selected based on equal contribution in growth inhibition of both compounds. A 10-point concentration range of the treatments (Supplementary Table 2, Additional file 1), the positive control (Staurosporine) and negative control 1% (Dimethyl sulfoxide, Phosphate Buffered Saline or combination depending on the solvent used), were dispensed in technical quadruplicates using a Tecan Fluent liquid handler or Tecan D300E dispenser. The following commonly used CRC treatments were screened: 5-fluorouracil (5-FU), SN-38 (active metabolite of irinotecan), oxaliplatin, panitumumab, combination treatment 5-FU & oxaliplatin, and combination treatment 5-FU & SN-38. On day 5, readouts were obtained by quantifying cell viability using CellTiter-Glo 3D (Promega, #G9681, 40 μL/well) with a Tecan Spark plate reader and CyQUANT Direct proliferation assay (Invitrogen, C7026, 20
μL/well) with a Tecan Spark plate reader and CyQUANT Direct proliferation assay (Invitrogen, C7026, 20 μL/well) with Perkin Elmer Operetta® CLS™. A baseline readout was measured on day 0 in a separate plate with PDOs without treatment. Drug screens were performed in at least two duplicate experiments on different days. Percentage viability and growth rate inhibition (GR) metrics values were calculated [32]. GR values range from 1 to −
μL/well) with Perkin Elmer Operetta® CLS™. A baseline readout was measured on day 0 in a separate plate with PDOs without treatment. Drug screens were performed in at least two duplicate experiments on different days. Percentage viability and growth rate inhibition (GR) metrics values were calculated [32]. GR values range from 1 to − 1, with 0 to 1 for partial growth inhibition, 0 for complete cytostasis, and 0 to −
1, with 0 to 1 for partial growth inhibition, 0 for complete cytostasis, and 0 to − 1 for cell death. Four parameter log-logistic curves and biphasic sigmoid curves were fit using the DRC package in R [33] and the biphasic dose-response model in GraphPad, respectively. We calculated the Akaike information criterion (AIC) values of both models for 5-FU & oxaliplatin, to objectify goodness-of-fit. As AIC values of the biphasic model were lower (median decrease 9.5, range 2.5–26.7), response curves for 5-FU & oxaliplatin were fit using a biphasic model instead of a log-logistic model, resulting in GR501 and GR502 parameters. The GRAUC (area under the non-fitted ‘curve’ of the raw GR values), GR50 (concentration that gives half-maximal growth rate inhibition), GR501 and GR502 (concentration of 50% growth rate inhibition of the upper and lower part of the biphasic curve, respectively) were calculated. Normalized values for GRAUC and GR50(2) were calculated using the maximum and minimum measured parameter per treatment to compare different treatment types with different concentration ranges.
1 for cell death. Four parameter log-logistic curves and biphasic sigmoid curves were fit using the DRC package in R [33] and the biphasic dose-response model in GraphPad, respectively. We calculated the Akaike information criterion (AIC) values of both models for 5-FU & oxaliplatin, to objectify goodness-of-fit. As AIC values of the biphasic model were lower (median decrease 9.5, range 2.5–26.7), response curves for 5-FU & oxaliplatin were fit using a biphasic model instead of a log-logistic model, resulting in GR501 and GR502 parameters. The GRAUC (area under the non-fitted ‘curve’ of the raw GR values), GR50 (concentration that gives half-maximal growth rate inhibition), GR501 and GR502 (concentration of 50% growth rate inhibition of the upper and lower part of the biphasic curve, respectively) were calculated. Normalized values for GRAUC and GR50(2) were calculated using the maximum and minimum measured parameter per treatment to compare different treatment types with different concentration ranges.
Statistical methods
Drug screens were optimized by comparing correlation coefficients of different PDO screening methods with clinical response. Where applicable, two-sided Pearson correlation tests were utilized to examine linear associations between continuous variables. Spearman correlation tests were employed when the data did not meet the assumptions of normality. Associations between clinical response and organoid response were examined by scatterplots. Univariate cox proportional hazard regression analysis was performed to estimate the hazard ratio (HR) with a 95% CI. AUC values were transformed to a standard normal distribution to estimate the HR. Kaplan-Meier survival curves were used to plot progression-free survival, and a two-sided Wald test was used to compare survival between patients with different organoid sensitivity. PDOs were classified as sensitive if the normalized GRAUC of the 5-FU & oxaliplatin drug screen was below the upper tertile. This cut-off was based on the response rate of approximately 60% for patients treated with FOLFOX in the first line in order to evaluate whether the upper third most resistant PDOs indeed predict failure of FOLFOX [1, 2]. We evaluated organoid sensitivity in relation to prior exposure to chemotherapy, mutational status and sidedness using boxplots. A two-sided Mann-Whitney U-test were applied for comparing 2 groups. Analysis was performed in R (version 4.0.3). DRCs and derived metrics were fit and calculated with the GRmetrics (version 1.16.0) and DRC (version 3.0–1) packages. Heatmaps were plotted using the Pheatmap (version 1.0.12) package.
Results
Patient cohort
The study cohort consists of 23 mCRC patients who were treated with standard-of-care systemic therapy for metastatic disease. Four PDOs were derived from primary tumours and 19 from liver metastases (Table (Table1).1). Most patients were chemotherapy-naïve when the PDO was established (14/23). The clinical characteristics of the included patients reflect the heterogeneous mCRC population (Supplementary Table 3, Additional file 1). The cohort includes 10 RAS-mutants, three BRAF-mutants and 10 RAS/BRAF-wildtype tumours. The cohort comprises five patients with rectal tumours, 11 patients with left-sided tumours, and seven patients with right-sided tumours (Supplementary Table 3, Additional file 1). Evaluable treatments in the first line of treatment after PDO establishment include capecitabine monotherapy (prodrug of 5-FU, n = 6), 5-FU & oxaliplatin combination treatment (n
= 6), 5-FU & oxaliplatin combination treatment (n = 13) and irinotecan-based treatment (5-FU & irinotecan combination treatment or irinotecan monotherapy, n
= 13) and irinotecan-based treatment (5-FU & irinotecan combination treatment or irinotecan monotherapy, n = 4). Late-line treatments include 5-FU & oxaliplatin combination treatment (n
= 4). Late-line treatments include 5-FU & oxaliplatin combination treatment (n =
= 1), irinotecan-based treatment (n
1), irinotecan-based treatment (n =
= 6) and panitumumab (n
6) and panitumumab (n =
= 6). Bevacizumab treatment was given to the vast majority of the patients (n
6). Bevacizumab treatment was given to the vast majority of the patients (n =
= 19). However, this treatment is not evaluable in vitro, since its main effect is on the tumour vasculature [34].
19). However, this treatment is not evaluable in vitro, since its main effect is on the tumour vasculature [34].
Table 1
Overview of evaluable treatments per patient
| Patient ID | Evaluable treatment 1 | Response 1 | Evaluable treatment 2 | Response 2 | Evaluable treatment 3 | Response 3 | Mutational status | PDO origin | Stage at presentation | Sidedness |
|---|---|---|---|---|---|---|---|---|---|---|
| 04 | 5-FU | SD | 5-FU & irinotecan | SD | 5-FU & oxaliplatin | PR | RAS mutant | Metastatic | IV | Left |
| 06 | 5-FU | SD | RAS mutant | Metastatic | IV | Left | ||||
| 07 | 5-FU | SD | RAS mutant | Metastatic | IV | Left | ||||
| 11 | 5-FU | PD | Wildtype | Metastatic | IV | Right | ||||
| 16 | 5-FU | SD | Panitumumab | PD | BRAF mutant | Primary | IV | Right | ||
| 18 | 5-FU | PD | Wildtype | Metastatic | III | Rectum | ||||
| 01 | Irinotecan | SD | RAS mutant | Metastatic | II | Rectum | ||||
| 02 | 5-FU & irinotecan | SD | RAS mutant | Metastatic | III | Right | ||||
| 23 | 5-FU & irinotecan | SD | Panitumumab | SD | BRAF mutant | Metastatic | III | Left | ||
| 20 | 5-FU & irinotecan | PD | ||||||||
| 20 | 5-FU & oxaliplatin | PD | RAS mutant | Primary | IV | Left | ||||
| 03 | 5-FU & oxaliplatin | PD | RAS mutant | Primary | IV | Right | ||||
| 05 | 5-FU & oxaliplatin | PR | RAS mutant | Primary | IV | Right | ||||
| 08 | 5-FU & oxaliplatin | PR | Panitumumab | SD | Wildtype | Metastatic | IV | Rectum | ||
| 09 | 5-FU & oxaliplatin | SD | BRAF mutant | Metastatic | IV | Left | ||||
| 10 | 5-FU & oxaliplatin | PR | Panitumumab | SD | Wildtype | Metastatic | IV | Left | ||
| 12 | 5-FU & oxaliplatin | PR | 5-FU & irinotecan | SD | Panitumumab | SD | Wildtype | Metastatic | IV | Left |
| 13 | 5-FU & oxaliplatin | SD | Irinotecan | SD | RAS mutant | Metastatic | IV | Left | ||
| 14 | 5-FU & oxaliplatin | PR | 5-FU & irinotecan | PR | Wildtype | Metastatic | III | Rectum | ||
| 15 | 5-FU & oxaliplatin | PR | 5-FU & irinotecan | SD | Panitumumab | SD | Wildtype | Metastatic | III | Rectum |
| 17 | 5-FU & oxaliplatin | PR | 5-FU & irinotecan | SD | RAS mutant | Metastatic | IV | Right | ||
| 19 | 5-FU & oxaliplatin | PD | Wildtype | Metastatic | III | Left | ||||
| 21 | 5-FU & oxaliplatin | PD | Wildtype | Metastatic | II | Right | ||||
| 22 | Panitumumab | PR | Wildtype | Metastatic | IV | Left |
Table describing the evaluable treatments, ranked per primary evaluable treatment. The first, second and third lines after organoid establishment are shown for each patient, along with the patient’s best RECIST response during treatment. The RAS/BRAF mutational status of the original tumour, PDO origin, tumour stage at presentation and primary tumour location (sidedness) are presented. All patients had a proficient mismatch repair (pMMR) tumour. Patient 20 was resistant to FOLFOXIRI triplet chemotherapy and is, therefore, evaluable for 5-FU & oxaliplatin and 5-FU & irinotecan. Clinically capecitabine (prodrug 5-FU) is used often, while in in vitro screens 5-FU is evaluated
5-FU 5 Fluorouracil, CAP Capecitabine, ID Identification, PD Progressive disease, PDO Patient-derived organoid, PR Partial response, SD Stable disease
Organoid drug screen quality
The drug screen quality was analyzed by examining the Z’-factor [35], correlation in DRC metrics among the biological replicates and Bland-Altman plot for the difference in GRAUC between replicates. The mean Z’-factor for all PDOs and treatments was 0.64 with only 4% below 0.5, indicating a good quality drug screen (Supplementary Table 4, Additional file 1). Biological replicates were not included in the analysis if the runs had a Z’-factor <
< 0.3 or if technical errors had occurred (e.g. dispensing error). When drug suspension errors occurred or replicate curves deviated, the respective biological replicates were excluded (9% of the drug screens) and a third and/or fourth run was performed. The calculated DRC metrics GRAUC GR50 and GRmax of different included biological replicates were significantly correlated (Spearman correlation >
0.3 or if technical errors had occurred (e.g. dispensing error). When drug suspension errors occurred or replicate curves deviated, the respective biological replicates were excluded (9% of the drug screens) and a third and/or fourth run was performed. The calculated DRC metrics GRAUC GR50 and GRmax of different included biological replicates were significantly correlated (Spearman correlation > 0.84, p
0.84, p <
< 0.05, (Supplementary Fig. 1A, Additional file 1). The mean difference in GRAUC between included replicates was −
0.05, (Supplementary Fig. 1A, Additional file 1). The mean difference in GRAUC between included replicates was − 0.09, with limits of agreement ranging from −
0.09, with limits of agreement ranging from − 1.17 to 0.98 (Supplementary Fig. 1B, Additional file 1). The DRC per PDO for each treatment screened are displayed in Supplementary Fig. 2A, B, Additional file 1.
1.17 to 0.98 (Supplementary Fig. 1B, Additional file 1). The DRC per PDO for each treatment screened are displayed in Supplementary Fig. 2A, B, Additional file 1.
Phase 1: drug screen optimization
Step 1: removal of N-acetyl cysteine from screening medium
We compared screening medium with and without NAC for oxaliplatin-based growth inhibition assays. We confirmed that NAC increased resistance to oxaliplatin-based treatment, with a 24% increase in the median GRAUC (Supplementary Fig. 3A, Additional file 1). Withdrawal of NAC from the PDO drug screening medium had no disadvantageous effect on organoid growth of the untreated control, with a growth rate from day 0 to day 5 of 5.5 with NAC (95% CI 4.2, 6.7) and 6.8 without NAC (95% CI 5.5, 8.1). Moreover, the correlation with clinical response improved after removal of NAC (Pearson correlation 0.77 without NAC vs 0.3 with NAC, Table Table2).2). We, therefore, continued all drug screens in the following steps for oxaliplatin-based treatment without NAC.
Table 2
Comparison of organoid drug screening conditions
| Comparison | Condition 1 | Condition 2 |
|---|---|---|
| Screening medium 5-FU & oxaliplatin | With NAC (CQ ratio, GR) r | Without NAC (CQ ratio, GR) r |
| Readout 5-FU & oxaliplatin | CQ (ratio without NAC, GR) r | CTG (ratio without NAC, GR) r |
| Drug response curve metrics: Viability vs GR 5-FU & oxaliplatin | Viability (ratio without NAC) r | GR (ratio without NAC) r |
| Drug response curve metrics: Viability vs GR 5-FU & SN-38 | Viability (CTG fixed) r | GR (CTG fixed) r |
| Drug response curve metrics: Viability vs GR 5-FU | Viability (CTG) r | GR (CTG) r |
| Combination treatment set-up 5-FU & oxaliplatin | Fixed (CTG with NAC, GR) r | Ratio (CQ without NAC, GR) r |
| Combination treatment set-up 5-FU & SN-38 | Fixed (CTG, GR) r | Ratio (CTG, GR) r |
Pearson correlation coefficients of PDO response with patient response for different PDO drug screening conditions, with 95% confidence interval
5-FU 5 Fluorouracil, CTG CellTiter-Glo, CQ CyQUANT, GR Growth rate, NAC N-acetyl cysteine, SN-38 active metabolite of irinotecan
Step 2: drug screen readout (CellTiter-Glo versus CyQUANT)
Various approaches exist for quantifying organoid viability as a proxy for drug response. We used ATP-based CellTiter-Glo, as this luminescence-based readout is most commonly used in literature as it is a rapid, high-throughput readout [36]. In addition, we explored the nuclear fluorescent-based CyQUANT readout. CyQUANT offers the benefit of directly measuring number of viable cells instead of relying on surrogate measures [37]. We found that the Pearson correlation between drug sensitivity measurements (GRAUC) utilizing CellTiter-Glo and measurements utilizing CyQUANT was 0.78 for 5-FU monotherapy (95% CI 0.50, 0.92), 0.69 for 5-FU & SN-38 combination treatment (95% CI -0.04, 0.94) and 0.57 for 5-FU & oxaliplatin combination treatment (95% CI -0.23, 0.91 Supplementary Fig. 3B-D, Additional file 1). As drug sensitivity measurement for 5-FU & oxaliplatin combination obtained from the CyQUANT readout showed limited concordance with the CellTiter-Glo readout, we further explored the CyQUANT readout for reflecting patient response to this drug combination in 6 PDOs. We found that CyQUANT and CellTiter-Glo measurements showed similar Pearson correlations with patient response of 0.77 and 0.81, respectively (Table (Table22).
Step 3 and 4: viability, growth rate metrics and curve fitting
For all evaluated treatments, we compared GR metrics to percentage viability measurements (Supplementary Fig. 3E, Additional file 1). Using GR metrics instead of percentage viability corrects for confounders in organoid drug sensitivity, related to differences in cell division rate in untreated controls. Applying GR metrics improved correlations with patient response compared to percentage viability for 5-FU & oxaliplatin (Pearson correlation 0.6 vs 0.46), 5-FU & SN-38 combination treatment (Pearson correlation 0.66 vs 0.2) and 5-FU monotherapy (Pearson correlation 0.58 vs 0.30, Table Table2).2). Response curves of most drugs exhibit a sigmoidal shape. Interestingly, we observed a biphasic drug response with a static plateau for 5-FU & oxaliplatin combination screens (Fig. (Fig.22A).
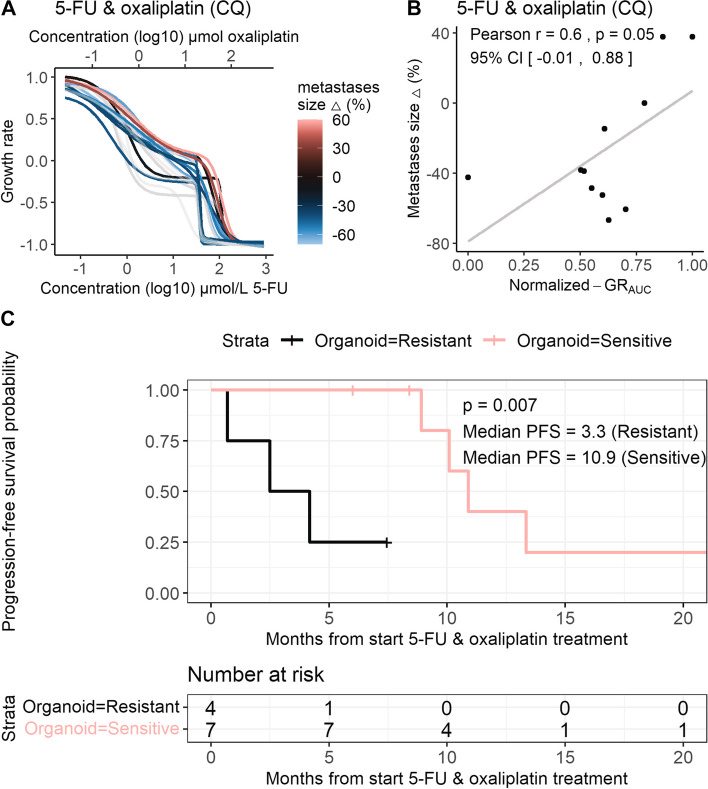
Association of tumour size change and PFS with organoid response to 5-FU & oxaliplatin. A DRCs of organoid sensitivity to 5-FU & oxaliplatin combination treatment screened in a 1.8:1 ratio. B Scatterplots show the correlation between patient response (% size change during treatment) and organoid response measured (GRAUC) for 5-FU & oxaliplatin combination treatment screened in a 1.8:1 ratio. C Kaplan-Meier progression-free survival curves of patients stratified by organoid sensitivity to 5-FU & oxaliplatin, based on normalized GRAUC (cut-off upper tertile =
= 0.63). Censoring events are indicated by vertical bars on the corresponding curve. The table underneath each plot denotes the numbers at risk. Log-rank test-based p value is shown. Abbreviations: 5-FU (5-fluorouracil), DRC (drug response curve), GRAUC (area under the growth rate inhibition curve), PFS (progression-free survival)
0.63). Censoring events are indicated by vertical bars on the corresponding curve. The table underneath each plot denotes the numbers at risk. Log-rank test-based p value is shown. Abbreviations: 5-FU (5-fluorouracil), DRC (drug response curve), GRAUC (area under the growth rate inhibition curve), PFS (progression-free survival)
Step 5: combination treatment set-up, ‘fixed’ versus ‘ratio’
Finally, we evaluate the most optimal strategy for combination screens for respectively 5-FU & oxaliplatin and 5-FU & SN-38 as these drugs are standardly used in combination in clinical practice. We compared combination drug screens using a (fixed) ratio with increasing dosage of both 5-FU & oxaliplatin (‘ratio’) versus using a fixed concentration of oxaliplatin and increasing only 5-FU (‘fixed’). Applying drugs in a ‘ratio’ versus ‘fixed’ combination influenced the correlation with clinical response and results were contradictory for oxaliplatin and irinotecan combination treatment. For oxaliplatin, using a fixed concentration of 0.05 μM oxaliplatin and increasing 5-FU (‘fixed’) did not show a positive correlation with patient response to 5-FU & oxaliplatin, as indicated by a Pearson correlation of −
μM oxaliplatin and increasing 5-FU (‘fixed’) did not show a positive correlation with patient response to 5-FU & oxaliplatin, as indicated by a Pearson correlation of − 0.25, versus 0.6 when screened in a 1.8:1 ratio, Table Table2.2. For irinotecan, using a fixed concentration of 0.01
0.25, versus 0.6 when screened in a 1.8:1 ratio, Table Table2.2. For irinotecan, using a fixed concentration of 0.01 μM SN-38 and increasing 5-FU (‘fixed’) resulted in a Pearson correlation of 0.66, versus a 0.3 when screened in a 1500:1 ratio (Table (Table22).
μM SN-38 and increasing 5-FU (‘fixed’) resulted in a Pearson correlation of 0.66, versus a 0.3 when screened in a 1500:1 ratio (Table (Table22).
Phase 2: correlation of organoid response using the optimized drug screen methods with patient response
Next, the optimized screening methods were used to examine the association between organoid and patient response on the complete set of PDOs per treatment type, for 5-FU & oxaliplatin, irinotecan-based treatment and 5-FU monotherapy.
5-FU & oxaliplatin
We expanded the CyQUANT screens for evaluating organoid sensitivity and correlation with patient response to 5-FU & oxaliplatin on 14 PDOs, of which 11 PDOs were derived from metastatic lesions. 5-FU & oxaliplatin comprises the largest treatment cohort and the majority of patients was treated in the first line (n =
= 13), directly after the organoid biopsy was obtained. Sensitivity of PDOs derived from metastatic lesions to 5-FU & oxaliplatin without NAC, screened in a 1.8:1 ratio and measured by GRAUC, showed a Pearson correlation of 0.6 (p
13), directly after the organoid biopsy was obtained. Sensitivity of PDOs derived from metastatic lesions to 5-FU & oxaliplatin without NAC, screened in a 1.8:1 ratio and measured by GRAUC, showed a Pearson correlation of 0.6 (p =
= 0.053, Fig. Fig.2A,2A, B) with change in tumour size during 5-FU & oxaliplatin treatment. The median GRAUC was 0.57 for PDOs derived from patients with a decrease in size of metastatic lesions and 0.87 for PDOs derived from patients with stable or an increase in size of metastatic lesions (p
0.053, Fig. Fig.2A,2A, B) with change in tumour size during 5-FU & oxaliplatin treatment. The median GRAUC was 0.57 for PDOs derived from patients with a decrease in size of metastatic lesions and 0.87 for PDOs derived from patients with stable or an increase in size of metastatic lesions (p = 0.012). There was discordance between patient response to 5-FU & oxaliplatin and PDO response in two of the three PDOs derived from primary tumours. The Pearson correlation with patient response for PDOs derived from metastases and primary tumours was limited to 0.29 (Supplementary Fig. 4A, Additional file 1). Next to GRAUC, other DRC metrics were evaluated, including the GR502 parameter for biphasic curves. GR502 showed a Pearson correlation of 0.7 (p
= 0.012). There was discordance between patient response to 5-FU & oxaliplatin and PDO response in two of the three PDOs derived from primary tumours. The Pearson correlation with patient response for PDOs derived from metastases and primary tumours was limited to 0.29 (Supplementary Fig. 4A, Additional file 1). Next to GRAUC, other DRC metrics were evaluated, including the GR502 parameter for biphasic curves. GR502 showed a Pearson correlation of 0.7 (p =
= 0.02) with patient response to 5-FU & oxaliplatin (Supplementary Fig. 4B, Additional file 1). We explored PFS as a secondary outcome measure for patient response. First, in a Cox proportional hazards model, the hazard ratio was estimated to be 2.30 (95% CI 0.68, 7.71, p
0.02) with patient response to 5-FU & oxaliplatin (Supplementary Fig. 4B, Additional file 1). We explored PFS as a secondary outcome measure for patient response. First, in a Cox proportional hazards model, the hazard ratio was estimated to be 2.30 (95% CI 0.68, 7.71, p =
= 0.2). Secondly, PDOs were classified as sensitive or resistant based on the GRAUC. PFS of patients with PDOs classified as sensitive was substantially longer compared to patients with resistant PDOs (median PFS 3.3 vs 10.9
0.2). Secondly, PDOs were classified as sensitive or resistant based on the GRAUC. PFS of patients with PDOs classified as sensitive was substantially longer compared to patients with resistant PDOs (median PFS 3.3 vs 10.9 months, log rank p
months, log rank p =
= 0.007, Fig. Fig.22C).
0.007, Fig. Fig.22C).
Irinotecan-based treatment
Ten patients received irinotecan-based treatment in 1st or 2nd treatment line, either monotherapy (n =
= 2) or in combination with 5-FU (n
2) or in combination with 5-FU (n =
= 8). For irinotecan-based treatment, organoid sensitivity to a fixed dose SN-38 and increasing concentrations 5-FU (with NAC, using CellTiter-Glo) measured by GRAUC showed a Pearson correlation of 0.61 (p
8). For irinotecan-based treatment, organoid sensitivity to a fixed dose SN-38 and increasing concentrations 5-FU (with NAC, using CellTiter-Glo) measured by GRAUC showed a Pearson correlation of 0.61 (p =
= 0.059) with patient response (Fig. (Fig.3A,3A, B). For 5-FU & SN-38 no other DRC parameters then GRAUC were suitable for measuring drug sensitivity. GR50 could not reliably be measured due the absence of an evident lower plateau in the DRC of these screens (Fig. (Fig.3A).3A). As patients in this cohort were treated in different lines, PFS could not reliably be compared.
0.059) with patient response (Fig. (Fig.3A,3A, B). For 5-FU & SN-38 no other DRC parameters then GRAUC were suitable for measuring drug sensitivity. GR50 could not reliably be measured due the absence of an evident lower plateau in the DRC of these screens (Fig. (Fig.3A).3A). As patients in this cohort were treated in different lines, PFS could not reliably be compared.
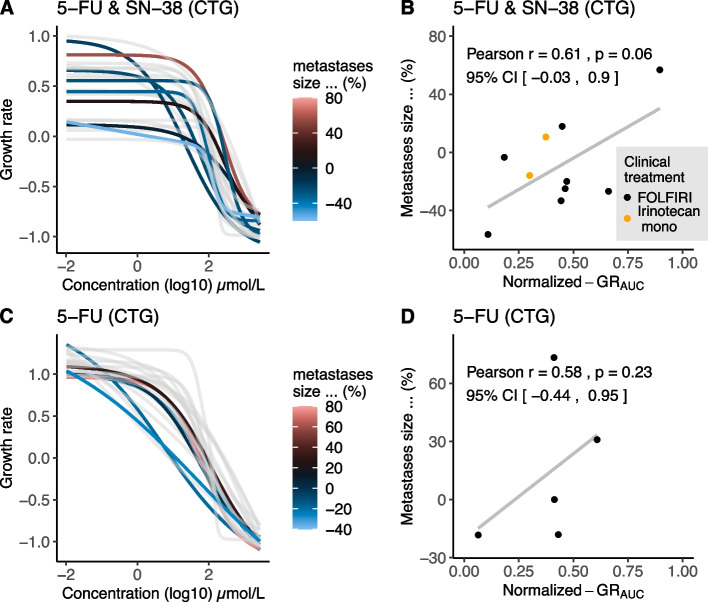
Association of tumour size change and organoid response to irinotecan-based treatment and 5-FU monotherapy. A DRCs of organoid sensitivity to 5-FU & SN-38 combination treatment. B Scatterplots show the correlation between patient response (% size change during treatment) and organoid response measured (GRAUC) for (5-FU &) SN-38. C DRCs of organoid sensitivity to 5-FU monotherapy. D Scatterplots show the correlation between patient response (% size change during treatment) and organoid response measured (GRAUC) for 5-FU monotherapy. Abbreviations: 5-FU (5-fluorouracil), DRC (drug response curve), CTG (CellTiter-Glo), GRAUC (area under the growth rate inhibition curve), SN-38 (active metabolite of irinotecan)
5-FU
Six patients were treated with capecitabine monotherapy (prodrug of 5-FU) which allows a direct single agent comparison of patient response with organoid response to 5-FU. All six patients received capecitabine as 1st treatment line and directly after the organoid biopsy was obtained. Organoid sensitivity to 5-FU (with NAC, using CellTiter-Glo) measured by GRAUC showed a Pearson correlation of 0.58 (p =
= 0.23) with % change in tumour size during capecitabine treatment (Fig. (Fig.3C,3C, D).
0.23) with % change in tumour size during capecitabine treatment (Fig. (Fig.3C,3C, D).
PDOs reflect clinical heterogeneity in drug sensitivity, effect of prior treatment, primary tumour sidedness and mutational status
Finally, as all PDOs in the cohort were screened for commonly used treatments in CRC, allowing comparison of drug sensitivity for patients with different tumour characteristics. We investigated the impact of mutational status, primary tumour location, and prior chemotherapy exposure on organoid drug sensitivity. When we examined organoid sensitivity for different standard-of-care drugs, a wide range of responses was seen (Fig. (Fig.4A).4A). Some PDOs display a generally resistant phenotype (e.g. PDO 21) to most treatments, while other PDOs display a differential treatment response (e.g. PDO 19). We found that PDOs obtained from patients with a left-sided RAS/BRAF-wildtype tumour (n =
= 4) were more sensitive to EGFR-inhibitor panitumumab, compared to PDOs obtained from patients with right-sided or rectal RAS/BRAF-wildtype tumours, RAS-mutant tumours and BRAF-mutant tumours (n
4) were more sensitive to EGFR-inhibitor panitumumab, compared to PDOs obtained from patients with right-sided or rectal RAS/BRAF-wildtype tumours, RAS-mutant tumours and BRAF-mutant tumours (n =
= 19, median normalized GRAUC 0.17 vs 0.74, p
19, median normalized GRAUC 0.17 vs 0.74, p =
= 0.138). Interestingly, we observed varying organoid sensitivity to panitumumab within the group of left-sided RAS/BRAF-wildtype tumours (Fig. (Fig.4B).4B). Organoid sensitivity to chemotherapeutic treatment with 5-FU was increased in organoids derived from RAS mutant tumours (n
0.138). Interestingly, we observed varying organoid sensitivity to panitumumab within the group of left-sided RAS/BRAF-wildtype tumours (Fig. (Fig.4B).4B). Organoid sensitivity to chemotherapeutic treatment with 5-FU was increased in organoids derived from RAS mutant tumours (n =
= 10, median normalized GRAUC 0.42 vs 0.64, p
10, median normalized GRAUC 0.42 vs 0.64, p =
= 0.057, Fig. Fig.44C).
0.057, Fig. Fig.44C).
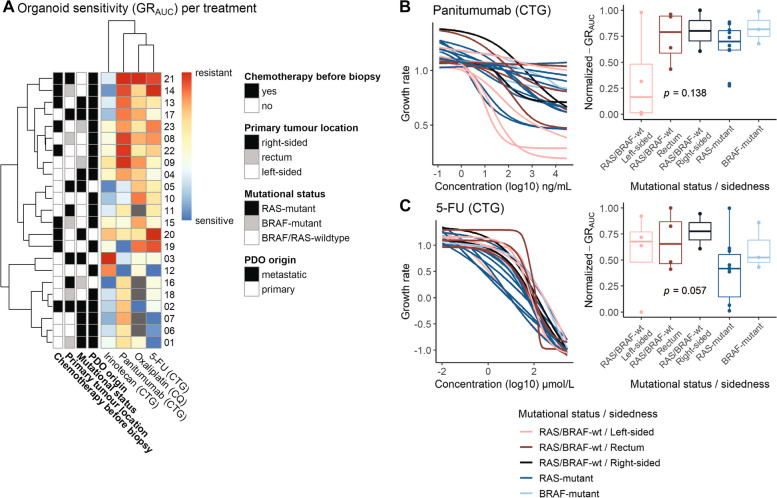
Organoid sensitivity based on primary tumour location and mutational status. A Clustered heatmap of the normalized GRAUC, with characteristics of the patient indicated in the first four columns for chemotherapy exposure prior to PDO establishment (adjuvant or first line), the primary tumour location (left- versus right-sided), mutational status (BRAF-mutant, RAS-mutant and RAS/BRAF-wildtype) and PDO origin (metastatic and primary tumour). The normalized GRAUC are illustrated as a heatmap with a column for each treatment type examined, with PDOs that were not screened for oxaliplatin in grey. B and C) The DRCs for panitumumab (B) and 5-FU (C) treatment and boxplots of the GRAUC for PDOs categorized according to the tumour’s mutational status and sidedness (RAS/BRAF-wildtype and left-sided; RAS/BRAF-wildtype and rectal; RAS/BRAF-wildtype and right-sided; RAS-mutant and BRAF-mutant. Boxplots show the minimum, median, maximum, upper and lower quartiles and individual data points. Abbreviations: 5-FU (5-flouruoracil), DRC (drug response curve), CTG (CellTiter-Glo), CQ (CyQUANT), GRAUC (area under the growth rate inhibition curve), PDO (patient-derived organoid), SN-38 (active metabolite of irinotecan), wt (wildtype)
PDOs from tumours exposed to 5-FU or capecitabine (in combination with oxaliplatin) before establishment (n =
= 9), mainly in the form of adjuvant treatment (n
9), mainly in the form of adjuvant treatment (n =
= 6), are more resistant to 5-FU than untreated PDOs (median normalized GRAUC of 0.86 versus 0.43, p
6), are more resistant to 5-FU than untreated PDOs (median normalized GRAUC of 0.86 versus 0.43, p =
= 0.003). However, this resistance does not extend to other chemotherapy types (Fig. 5).
0.003). However, this resistance does not extend to other chemotherapy types (Fig. 5).
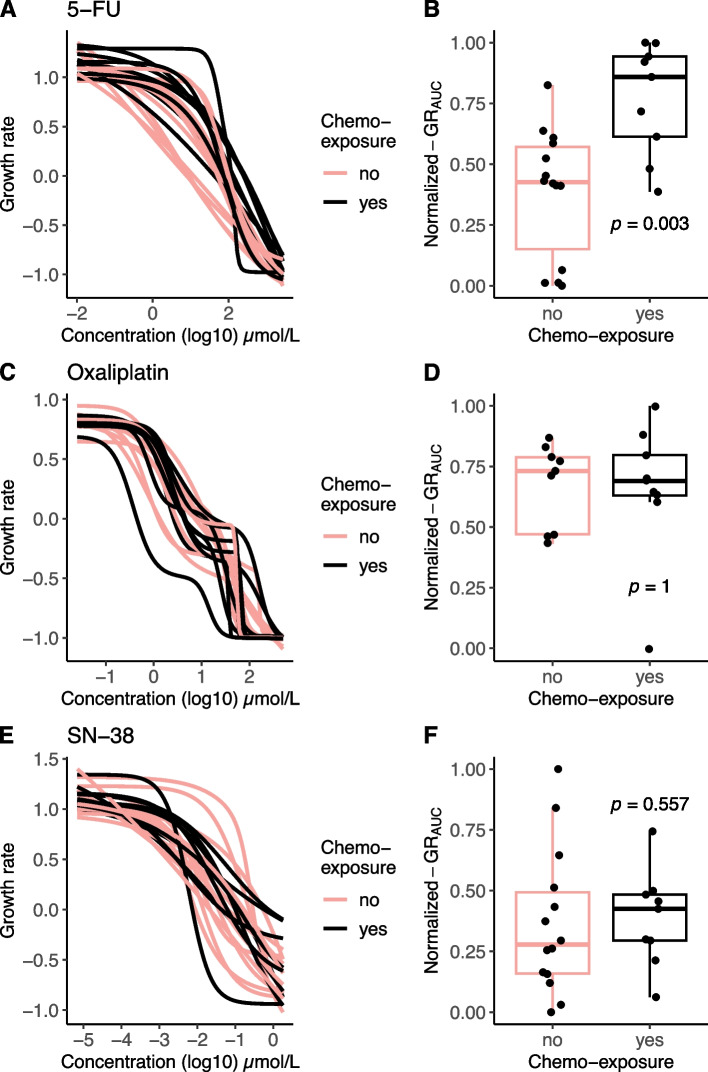
Increased resistance to 5-FU after prior exposure to chemotherapy. The association between prior chemotherapy exposure to patients before the biopsy for PDOs was established and organoid response (GRAUC) is shown for 5-FU, oxaliplatin and SN-38. A, C and D. The DRC of organoid sensitivity with red curves indicating 5-FU or capecitabine containing chemotherapy exposure. B, D and F Boxplots of normalized GRAUC for patients that were exposed to chemotherapy versus chemotherapy-naïve patients. Boxplots show the minimum, median, maximum, upper and lower quartiles and individual data points. Abbreviations: 5-FU (5-flouruoracil), GRAUC (area under the growth rate inhibition curve), SN-38 (active metabolite of irinotecan)
Discussion
Our study shows that CRC PDO drug screens need optimization and standardization before being reliably utilized as biomarker for patient response in clinical practice. A standardized screening protocol could enhance cross-study comparisons and improve reproducibility as significant variation exists regarding screening methods used in different studies [7, 24]. To establish a drug screening method that adequately reflects the clinical situation, we used an inverse approach. Starting from the patient’s response, we fine-tuned different parameters of the drug sensitivity assays in a small population. This enhanced the accuracy PDOs in reflecting the patient’s sensitivity. For subsequent evaluation of the predictive value of the optimized screening method in the complete set, we used a cohort of heterogeneous PDOs, well reflecting the clinical population. We optimized the drug screening method through five steps, for which the results are summarised in Table Table3.3. The first step regards the medium composition, as it is already known that changing medium components can have dramatic effects on chemosensitivity [38]. It was previously reported that specifically NAC affects sensitivity to oxaliplatin in CRC organoids [28]. This can be explained by the fact that NAC causes detoxification of oxaliplatin through glutathione synthesis and can, therefore, interfere with organoid sensitivity to platinum-based chemotherapy, yet does not affect sensitivity to 5-FU or irinotecan [27]. In line with these results, our screens confirmed increased resistance to oxaliplatin-based treatment with NAC-containing screening medium. This led to the necessity of using high, clinically irrelevant oxaliplatin doses and we found a reduced correlation with clinical response when NAC was added to the screening medium [31]. Notably, studies that use NAC in oxaliplatin screening found no correlation between organoid sensitivity and patient response [20, 23]. Therefore, we recommend removing NAC from the medium in oxaliplatin-based drug screens. Secondly, we compared two types of drug screen readouts to define the most optimal readout. The ATP-based readout is most commonly used for PDO drug screening. Nevertheless, based on the compound mechanism of action, ATP measurements can lead to misleading results as metabolic activity does not always correlate with cell viability [36]. Therefore, we explored the use of a well-established readout based on DNA-content for 2D cell lines (CyQUANT) to measure cell viability in PDO-based screens. Nuclear fluorescent-based assays such as CyQUANT or propidium iodide dye combined with Hoechst are less affected by cell changes unrelated to viability, such as senescence. Propidium iodide and Hoechst have previously demonstrated their suitability for high-throughput screening of colorectal adenoma PDOs [39]. CyQUANT was used previously in a prospective organoid-guided interventional trial with positive results, albeit with modest clinical benefit [40]. We confirmed that drug sensitivity measurements with the CyQUANT readout instead of the ATP-based CellTiter-Glo readout was possible in 3D-based screens and did not affect the correlation with patient response. CyQUANT may, therefore, serve as promising alternative drug screening method, enabling screening with fewer than 10 organoids per well. Thirdly, in line with previous research showing that bias caused by the proliferation rate of PDOs can be avoided by using GR metrics for organoid response analysis [32], we confirm that using GR metrics improved the correlation with patient response. Despite good correlations of PDO and clinical response in studies employing both percentage viability and GR metrics [6, 7], we found that GR metrics showed better correlation with patient response than percentage viability metrics. Previous studies used DRC parameters AUC, IC50, GR50 or GRmax to evaluate organoid response [14–16, 23]. In our research, GRAUC proved robust and patient-response reflective. For full sigmoidal/biphasic curves, GR50(2) could also serve as reliable drug sensitivity measures. Fourthly, the conventional approach in all previous studies involved log-logistic curve fitting. Nonetheless, goodness-of-fit improved by applying biphasic curve fitting for 5-FU & oxaliplatin in our study. Finally, we optimized the drug screen set-up for combination screens and found that a fixed concentration of SN-38 is recommended for SN-38 based combination screening. This might be explained by the fact that 5-FU can inhibit the in vitro efficacy of SN-38 at high concentrations [41], although one study showed positive results where 5-FU & SN-38 was used in a ratio [21]. For oxaliplatin-based treatments, a ratio screen is preferred to capture the additive effect of both compounds. This is in line with studies that used a comparable ratio [14, 16, 22] or a drug matrix and found a good association with patient response, while no association was found in studies that used different methods for combination screens [20, 23].
Table 3
Recommendations for CRC organoid drug screening
| Topic | Evidence | Recommendations |
|---|---|---|
| 1. Medium composition | Resistance to oxaliplatin-based treatment increases with NAC in screening medium. | Remove NAC from screening medium in oxaliplatin-based drug screens. |
| 2. Readouts | CellTiter-Glo measurements are in agreement with CyQUANT measurements. | Both readouts can be used. CyQUANT provides the advantage of performing drug screens with 5–10 PDOs per well. |
| 3. DRC metrics | GR metrics showed better correlation with patient response than percentage viability metrics. GRAUC is the most robust DRC metric and best reflects PDO and patient response. | Apply GR metrics to correct for confounders in organoid drug sensitivity, related to differences in natural cell division rate. Employ GRAUC for comparison with patient response, or GR50(2) if a clear lower curve plateau is present. |
| 4. DRC fitting | PDOs exhibit a biphasic drug response to 5-FU & oxaliplatin. | Apply a biphasic model for DRC fitting instead of a log-logistic model. |
| 5. Combination treatment set-up | SN-38 & 5-FU in a ratio combination screen did not reflect patient response to 5-FU & irinotecan. Oxaliplatin & 5-FU with a fixed oxaliplatin concentration did not reflect patient response to 5-FU & oxaliplatin. | Use a fixed concentration of SN-38 and increase the 5-FU concentration for 5-FU & SN-38 combination screens. Use a concentration ratio 5-FU:oxaliplatin for oxaliplatin-based combination screens. |
5-FU 5 Fluorouracil, CTG CellTiter-Glo, CQ CyQUANT, DRC Drug response curve, GRAUC area under the growth rate inhibition curve, NAC N-acetylcysteine, PDO Patient-derived organoid, SN-38 active metabolite of irinotecan
Regarding the correlation of PDO response with clinical response, our findings are in line with previous results. In a recent systematic review the overall positive predictive value for organoid informed treatment for CRC is 68% and the negative predictive value is 78% for standard of care chemotherapy, targeted therapy and radiotherapy [6]. In literature, consistent results are seen for 5-FU and irinotecan-based treatment, showing good correlations of the AUC with both RECIST response and PFS in several, relatively small, studies which align with our results [6, 7, 14–16, 23]. In our study, organoid response (GRAUC) positively correlated with patient response (% size change in metastatic lesions) for 5-FU & oxaliplatin, despite the small sample size. Furthermore, classifying PDOs as sensitive and resistant based on GRAUC, resulted in a clinically relevant difference in median PFS in the sensitive and resistant group, which is in line with previous reports including PDOs treated with 5-FU & oxaliplatin [14, 22]. In addition to the correlation with patient response, we show that CRC PDOs adequately reflect key clinical aspects regarding drug sensitivity and capture heterogeneity in treatment response. Patient response to EGFR inhibitors is influenced by factors such as tumour sidedness and RAS/BRAF mutational status. In line with the findings of large clinical trials [42, 43] and PDO screens [44], PDOs from patients with a left-sided colon RAS/BRAF-wildtype tumour were most sensitive to panitumumab in our cohort. In addition to mutational status, we showed that the resistance after prior 5-FU or capecitabine containing treatment is well captured in PDOs. This implies that PDOs provide a representative model for the 5-FU resistant state after prior chemotherapy exposure, supported by increased PDO resistance after 5-FU treatment in a recent study [45]. As recognized in daily clinical practice, adjuvant chemotherapy might also affect response to palliative treatment. In this context, PDOs could be applied to study resistance mechanisms and evasion strategies. It also underlines the importance of deriving organoids directly before a new treatment starts, as prior treatments affect sensitivity to subsequent therapies.
It is essential to acknowledge the limitations that stress the need for subsequent larger prospective studies to validate our results. In this small retrospective study utilizing biobank samples, most samples were not initially collected for direct comparison with patient response. Consequently, these samples were not acquired immediately before initiating the evaluated treatment, which compromises the accuracy of comparison with patient response. The cohort’s diversity further stems from the fact that the collected tissue does not exclusively mirror the metastatic lesions under evaluation in patient responses; it might encompass primary tissue or other resected metastases. Both may lead to an underestimation of the correlation with response. The limited number of PDOs in the treatment subgroups constrains the demonstration of significant correlations with patient response for all treatments and prohibits drawing strong conclusions. Moreover, the small sample size can lead to sampling bias with individual variations having a disproportionate impact on outcomes, and difficulty in accounting for confounding variables. The optimization of drug screen methods requires evaluation of generalizability and validation of our PFS cut-off in an independent, larger cohort before applying in other laboratories. Of note, relative PDO sensitivity is influenced by the sensitivity of other PDOs in the cohort it is compared to. To prevent misinterpretation, it is essential to compare individual drug screens to large cohorts, ensuring consistency and avoiding errors due to differences in sensitivity across groups.
Prospective validation is currently ongoing in the OPTIC trial [29]. Here, we establish PDOs for mCRC patients from newly obtained biopsies immediately prior to the start of treatment, and directly compare patient response with organoid response. Further drug screen optimization regarding duration of drug exposure and assay miniaturization [45], is key to advance towards the clinical application of PDOs for personalized treatment. PDO drug screen optimization should be extended beyond mCRC to other stages of disease and other types of cancer [46–48]. PDOs have been used for screening targeted treatments, treatment in the non-metastatic stage, such as radiotherapy for rectal cancer, and experimental treatments [49, 50]. A prior prospective study to guide experimental targeted treatments did not show clinical benefit [51], underscoring the additional need for refinement of screens for other treatment types.
Conclusions
Our study emphasizes the critical impact of the screening methods for determining correlation between PDO drug screens and mCRC patient outcomes. We used a 5-step optimization strategy including NAC removal from the screening medium, using biphasic or logistic curve fitting based on the type of treatment, applying growth rate metrics and selecting ratio or fixed concentrations depending on the combination treatments used. By using the optimized methods, PDO response correlated with patient response for oxaliplatin-based treatment. This optimization provides a basis for future research on the clinical utility of PDO screens. Furthermore, PDOs adequately reflect the effect of prior treatment, primary tumour sidedness and mutational status, supporting their use for modeling colorectal cancer in vitro.
Acknowledgements
We extend our gratitude to Utrecht Platform for Organoid Technology (UPORT) for their pivotal role in patient enrollment and tissue acquisition. We acknowledge the commitment of all participating hospitals in the recruitment and enrollment of eligible patients. We thank the patients for providing consent to the HUB-Cancer Biobank and OPTIC study.
Abbreviations
| 5-FU | 5-Fluorouracil |
| ATP | Adenosine triphosphate |
| AIC | Akaike information criterion |
| AUC | Area under the curve |
| CRC | Colorectal cancer |
| CI | Confidence interval |
| CT | Computed tomography |
| DMSO | Dimethylsulfoxide |
| DNA | Desoxyribonucleïnezuur |
| DRC | Drug response curve |
| EGF(R) | Epidermal growth factor (receptor) |
| FOLFOX | 5-FU & oxaliplatin |
| FOLFIRI | 5-FU & irinotecan |
| GR | Growth rate |
| GR50 | Concentration that gives 50% growth rate inhibition |
| GR501/2 | Concentration that gives 50% growth rate inhibition of the upper and lower part of the biphasic curve |
| GRAUC | Area under the non-fitted ‘curve’ of the raw GR values |
| GRmax | Concentration that gives maximal growth rate inhibition |
| HR | Hazard ratio |
| mCRC | Metastatic colorectal cancer |
| NAC | N-acetyl cysteine |
| NGS | Next generation sequencing |
| pMMR | Proficient mismatch repair |
| PDO | Patient-derived organoid |
| PFS | Progression-free survival |
| RECIST | Response evaluation criteria in solid tumours |
| SNP | Single-nucleotide polymorphism |
Authors’ contributions
OK, JR, SB, SE, RV and MK initiated the project. AB, LV and GC contributed to the successful enrollment of a diverse and representative study population. LS collected the clinical data. MB revised all CT scan reports according to RECIST 1.1. EW, LS, EK and CV designed the experiments. KCP and CHB performed the experiments and contributed to the analyses. EK and MD analyzed the PDO drug screen data. RO and MH were major contributors to interpreting the drug screen data. LS and EW analyzed the PDO drug screen and clinical data and wrote the manuscript. JR was a major contributor in writing the manuscript. SE and BV advised in the statistical analysis and BPV provided the script for the biphasic curve fitting. SB, CV, SE, OK and MK reviewed the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by HUB Organoids B.V. and Cancer Genomics Center (NWO Gravitation Program).
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request after ethical approval. The underlying code for this study is not publicly available but may be made available to qualified researchers on reasonable request from the corresponding author. The organoid models are available and can be requested via Foundation Hubrecht Organoid Biobank (https://www.hubrechtorganoidbiobank.org/).
Declarations
The collection of patient data and tissue for the generation of organoids has been performed according to the guidelines of the European Network of Research Ethics Committees (EUREC) following European, national, and local law. This research was performed under the HUB-Cancer biobanking protocol and OPTIC protocol. The Biobank Research Ethics Committee of the UMC Utrecht (TCBio) approved the biobanking protocol: 12–093 HUB-Cancer. The medical ethical committee of the University Medical Center Utrecht (UMCU) approved the prospective clinical trial Organoids to Predict Therapy Response In Colorectal Cancer (OPTIC #17–356 [24]). All donors participating in this study signed informed consent. The study was performed in accordance with the Declaration of Helsinki.
Not applicable.
Miriam Koopman reports institutional financial interests with Amgen, Bayer, Bristol-Myers Squibb, Merck-Serono, Nordic Pharma, Pierre Fabre, Servier, Sirtex, Roche, Sanofi, and Personal Genome Diagnostics. Miriam Koopman reports the following non-financial interests: an advisory role for ZON-MW, membership of the scientific board of the Dutch Cancer Society (KWF), chairmanship of the Dutch Colorectal Cancer Group (DCCG), and principal investigator (PI) of the Prospective Dutch Colorectal Cancer (PLCRC) cohort. Jeanine Roodhart reports institutional financial interests with BMS, Pierre Fabre, Servier, Cleara, Xilis, DoMore diagnostics and HUB organoids B.V. Jeanine Roodhart reports an advisory role for Bayer, BMS, Merck-Serono, Pierre Fabre, Servier, AMGEN and board member of Foundation Hubrecht Organoid Biobank. Liselot Valkenburg-van Iersel reports financial interests with and an advisory role for Servier and Pierre Fabre. All other authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lidwien P. Smabers and Emerens Wensink both authors share equal contribution.
Sylvia F. Boj and Jeanine M. Roodhart both authors share last authorship.
Contributor Information
Sylvia F. Boj, Email: [email protected].
Jeanine M. Roodhart, Email: [email protected].
References
Articles from Journal of Experimental & Clinical Cancer Research : CR are provided here courtesy of BMC
Full text links
Read article at publisher's site: https://doi.org/10.1186/s13046-024-02980-6
Read article for free, from open access legal sources, via Unpaywall:
https://jeccr.biomedcentral.com/counter/pdf/10.1186/s13046-024-02980-6
Citations & impact
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/160834886
Article citations
Advancements in Research and Treatment Applications of Patient-Derived Tumor Organoids in Colorectal Cancer.
Cancers (Basel), 16(15):2671, 26 Jul 2024
Cited by: 0 articles | PMID: 39123399 | PMCID: PMC11311786
Review Free full text in Europe PMC
The Transformative Role of 3D Culture Models in Triple-Negative Breast Cancer Research.
Cancers (Basel), 16(10):1859, 13 May 2024
Cited by: 1 article | PMID: 38791938 | PMCID: PMC11119918
Review Free full text in Europe PMC
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Patient-Derived Organoid Model in the Prediction of Chemotherapeutic Drug Response in Colorectal Cancer.
ACS Biomater Sci Eng, 8(8):3515-3525, 13 Jun 2022
Cited by: 6 articles | PMID: 35696669
Patient-derived organoids can predict response to chemotherapy in metastatic colorectal cancer patients.
Sci Transl Med, 11(513):eaay2574, 01 Oct 2019
Cited by: 341 articles | PMID: 31597751
Patient-derived Organoid Model for Predicting the Chemoresponse in Patients With Colorectal Cancer.
In Vivo, 37(4):1751-1759, 01 Jul 2023
Cited by: 1 article | PMID: 37369516 | PMCID: PMC10347944
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
Health Technol Assess, 12(15):iii-ix, xi-162, 01 Jan 2008
Cited by: 34 articles | PMID: 18462574
ReviewBooks & documents Free full text in Europe PMC
Funding
Funders who supported this work.

 #2 and
#2 and 


