Abstract
Free full text
Coronary Artery Bypass Grafting for a Young Female Patient With Chronic Active Epstein-Barr Virus Infection
Abstract
A 24-year-old woman with chronic active Epstein-Barr virus (CAEBV) infection successfully underwent coronary artery bypass grafting for triple coronary arteries with chronic total occlusion and aneurysms. This case underscores the importance of accurate assessment and treatment of coronary artery lesions in patients with CAEBV infection.
History of Presentation
A 24-year-old female patient with chronic active Epstein-Barr virus (CAEBV) infection came to our hospital (Keio University School of Medicine, Tokyo, Japan) with a report of chest pain and dyspnea on exertion. Her vital signs were stable, and the electrocardiogram showed no obvious ST-T-wave changes (Figure 1). The patient was admitted for re-examination of coronary artery lesions because of the onset of recurrent angina with a low threshold.
Past Medical History
At the age of 17 years, 7 years before this admission, she received a diagnosis of CAEBV infection. At that time, she underwent coronary angiography (CAG), which showed chronic total occlusion (CTO) of both the right coronary artery (RCA) and the left anterior descending (LAD) artery with aneurysms. While considering coronary artery bypass grafting (CABG), we prioritized umbilical cord blood transplantation for the worsening CAEBV infection. Following transplantation, the CAEBV infection was controlled. She had no symptoms of angina, and she received optimal medical therapy.
Differential Diagnosis
The differential diagnosis for young patients with coronary artery disease includes autoimmune disease, such as Kawasaki disease or Takayasu disease, spontaneous coronary artery dissection, or atherosclerosis secondary to familial hypercholesterolemia.
Investigations
Cardiac magnetic resonance (CMR) imaging showed nontransmural late gadolinium enhancement in the inferolateral, apical-inferior, and midapical anterior left ventricular wall (Figure 2A). In addition, stress CMR demonstrated perfusion defects in all 3 coronary artery areas (Figures 2B and and2C).2C). Computed tomography (CT) demonstrated a 14-mm aneurysm in the left main trunk and suggested CTOs in all 3 coronary arteries. Transthoracic echocardiography showed a left ventricular ejection fraction of 50% with asynergy of the apical anterior and inferior septum. CAG showed 3 coronary arteries with CTO, with 90% stenosis in the proximal LAD artery (Figures 3D to 3F), worsened compared with the evaluations of her previous CAG findings (Figures 3A to 3C). In addition, the bilateral internal thoracic arteries were observed to be occluded on angiography.
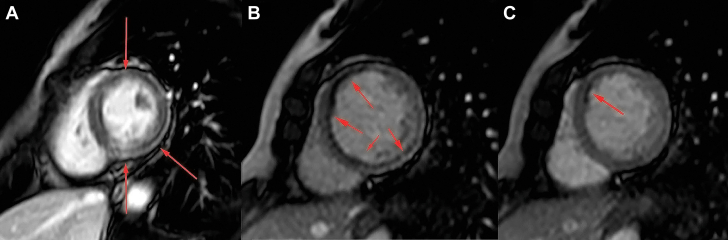
Cardiac Magnetic Resonance
(A) Nontransmural late gadolinium enhancement is observed in the inferolateral, apical inferior, and mid-apical anterior left ventricular wall (arrows). Perfusion defect was detected in the (B) anteroseptal, inferior, and inferolateral walls during stress (arrows) and in the (C) anteroseptal wall at rest (arrow).
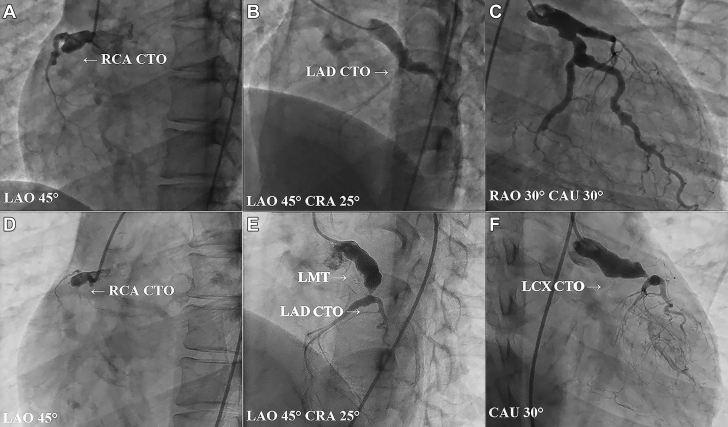
Comparing the Evaluations With Coronary Angiography Between the Ages of 17 and 24 Years
Angiographic findings (A to C) at the age of 17 years and (D to F) at the age of 24 years. (A) Right coronary artery (RCA) with chronic total occlusion (CTO). (B) Left anterior descending (LAD) artery with chronic total occlusion. (C) Left circumflex (LCX) artery without significant stenosis. (D) Right coronary artery with chronic total occlusion (E) Left anterior descending artery with chronic total occlusion penetrating only through its septal branch and the first diagonal branch with 90% stenosis in the proximal left anterior descending artery. (F) Left circumflex artery with chronic total occlusion. CAU = caudal; CRA = cranial; LAO = left anterior oblique; LMT = left main trunk; RAO = right anterior oblique.
Management
We had a discussion with our heart team to decide on CABG using radial artery and saphenous vein graft (SVG) as the treatment method for this 24-year-old female patient with triple-vessel CTO. Although there was no obvious elevation of myocardial enzymes and changes in the electrocardiogram over time, we decided to perform CABG after 10 days in the hospital for examination, considering her frequent symptoms. CABG was performed using an on-pump beating heart, with the left radial artery connected to the second diagonal branch and the SVG connected to the first diagonal branch, the obtuse marginal (OM) branch, and the posterior descending (PD) artery sequentially. The main trunks of the LAD artery and the RCA consisted of occluded lumen; the radial artery was connected to the second diagonal branch to ensure blood flow of the distal LAD artery, and first diagonal branch–OM branch–PD artery sequential bypass was performed to prevent occlusion of the SVG connecting to the PD. All procedures were completed without any complications.
Discussion
To the best of our knowledge, this is the first report of a patient with CAEBV infection who underwent CABG for 3-vessel CTO coronary artery disease. Epstein-Barr virus (EBV) infects most people at some point in their lives, and it usually causes mild or no symptoms. However, CAEBV infection is one of the EBV-positive T-cell or natural killer (NK) cell lymphoproliferative disorders with high morbidity and mortality.1 PD-1 inhibitors and other drugs are currently being studied for their effectiveness; however, the number of patients is small, and the treatment strategy has not been established.2 Common complications are hemophagocytic syndrome, liver failure, gastrointestinal ulceration, and lymphoid tumors such as malignant lymphoma and leukemia.3 Cases in patients with CAEBV infection are also complicated with cardiac lesions such as coronary artery disease, coronary artery aneurysms, myocarditis, valvular disease, heart failure, and pulmonary hypertension.4 Furthermore, a study from Japan reported an incidence of myocarditis of 6% and of coronary aneurysm of 9% in patients with CAEBV infection. The diagnosis of Kawasaki disease could be clear when the patient presents to the hospital in childhood with associated symptoms. However, it is difficult to rule out the possibility of Kawasaki disease in adults, such as in this case. Histopathologic examination could distinguish between the Kawasaki disease and CAEBV infection because neutrophil activation is predominant in Kawasaki disease, whereas lymphocyte predominance is observed in CAEBV infection. Therefore, it is often difficult to differentiate the coronary aneurysms of Kawasaki disease from those of CAEBV infection. Although we do not believe that there is a history of Kawasaki disease in this case, we cannot rule out the possibility that the disease may have developed asymptomatically and that the patient may have been completely affected. Coronary artery disease in CAEBV infection is caused by lymphoid vasculitis, which involves local inflammatory cell chemotaxis, recruitment, adhesion, and infiltration, as well as cytotoxic injury and secretion.4,5 Latent membrane protein (LMP)-1 infected by EBV enhances the production of vascular endothelial growth factor (VEGF), which leads to degradation of vessel walls.4 Cytotoxic secretion is promoted by EBV-positive NK/T cells, and this results in aggravating vascular lesions.4 Patients with CAEBV infection who have cardiac lesions have been reported to have a much poorer prognosis than patients without cardiac lesions.3,6
Previous studies of vascular lesions mainly focused on autopsy cases, and knowledge of the optimal treatment plan or treatment response for cardiovascular lesions is still lacking. CAEBV-related cardiovascular diseases are classified into direct injury and immune injury. Possible treatments include antiviral therapy, anti-inflammatory therapy, and management of cardiovascular complications. Antithrombotic drugs are mainly administered in patients with coronary artery stenosis or aneurysms. There have been reports of regression of coronary artery lesions after umbilical cord blood transplantation.7 However, in our case, the coronary artery lesions had progressed over the 7 years since her umbilical cord blood transplantation. Finally, the patient required revascularization.4 Given that there were no reports of CABG for severe coronary artery occlusion and aneurysm, our patient requires close follow-up. Her coronary artery aneurysm requires follow-up for its size because there has been a case of rupture leading to sudden death.8
Follow-Up
After the procedure, the patient recovered smoothly, with CT showing that all grafts were patent (Supplemental Figures 1A and 1B). She was discharged in good condition without any symptoms on the 13th postoperative day. At 3-month follow-up, she remains angina free and back to her regular work as a dental hygienist.
Conclusions
A 24-year-old woman underwent CABG for her triple coronary arteries with CTO secondary to CAEBV. Our case provides important insights into the efficacy of CABG for a young patient with coexisting severe coronary artery lesions resulting from CAEBV.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental figure, please see the online version of this paper.
References
Articles from JACC Case Reports are provided here courtesy of Elsevier
Citations & impact
This article has not been cited yet.
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/160643386
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Early diagnosis and follow-up of chronic active Epstein-Barr-virus-associated cardiovascular complications with cardiovascular magnetic resonance imaging: A case report.
Medicine (Baltimore), 95(31):e4384, 01 Aug 2016
Cited by: 6 articles | PMID: 27495050 | PMCID: PMC4979804
Review Free full text in Europe PMC
Chronic active Epstein-Barr virus infection manifesting as coronary artery aneurysm and uveitis.
Virol J, 17(1):166, 29 Oct 2020
Cited by: 10 articles | PMID: 33121509 | PMCID: PMC7597064
Chronic active Epstein-Barr virus infection with giant coronary aneurysms.
Am J Clin Pathol, 105(6):733-736, 01 Jun 1996
Cited by: 27 articles | PMID: 8659448
[Chronic active Epstein-Barr virus infection with multiple vascular lesions successfully treated by cord blood transplantation].
Rinsho Ketsueki, 61(10):1502-1507, 01 Jan 2020
Cited by: 0 articles | PMID: 33162448






