Abstract
Free full text
Severe COPD: Multidisciplinary Consultation to Get the Right Care at the Right Place
In the Netherlands, approximately 600,000 patients are affected by Chronic Obstructive Pulmonary Disease (COPD). COPD is a heterogeneous and common disease, and the third leading cause of mortality worldwide. Despite optimal treatment by pulmonary physicians in secondary or tertiary care, a small proportion of these patients continue to experience uncontrolled disease. These individuals, often referred to as severe COPD, account for a considerable proportion of COPD-related healthcare costs.
The most recent GOLD report define COPD severity based on airflow limitation in combination with symptoms, exacerbations and hospitalizations. However, this view on severe COPD fails to address the heterogeneity of the disease, including characteristics like air trapping, frequent exacerbations, airway inflammation and hypercapnia. Furthermore, the guidelines heavily rely on randomized controlled trials, which have limited external validity, as only a small percentage of COPD patients (5–15%) meets the inclusion criteria for these trials.1 Particularly for severe, difficult-to-control COPD cases, specific disease characteristics serve as essential markers for add-on therapies, such as third-line rehabilitation, (endobronchial) lung volume reduction, non-invasive ventilation, lung transplantation, and biologics targeting airway inflammation.2,3
In the region of South-West Netherlands, these specialized and targeted treatments are provided in different centres. This could lead to incorrect and potentially missed referrals due to various reasons. First, referring physicians may be unaware of the indications and exclusion criteria for these add-on therapies. Second, patients are sequentially referred to different centres for assessment, leading to treatment delays and additional costs. And third, managing the combination of different add-on treatments without central coordination has proven to be challenging. This calls for the need of a centralized regional collaboration.
To address this need, the Centre of Excellence for COPD in South-West Netherlands (Franciscus Gasthuis & Vlietland), specializing in tertiary assessment and treatment with biologics for obstructive diseases, has taken the initiative to organize a weekly digital “multidisciplinary consultation meeting” (MDC). All pulmonologist from our region, treating COPD patients, can regularly join this MDC. An expert panel with regional specialists offering specific add-on COPD interventions, participates in every meeting. These include specialists in lung transplantation and Lung Volume Reduction (LVR) surgery (Erasmus MC), endoscopic LVR (Maasstad Hospital), non-invasive ventilation (Center for Home Mechanical Ventilation, Erasmus MC), and tertiary COPD rehabilitation (Revant). The aims of this regional severe COPD MDC are to (1) improve care accessibility, (2) to prevent incorrect referrals, (3) to reduce patient travel, (4) to manage patient expectations, (5) to enhance regional knowledge in COPD and (6) identify candidates for research studies.
The MDC is conducted as an online meeting where specialized pulmonologists from the aforementioned centres and a specialized advance care planning and COPD physician assistant routinely participate. Weekly, pulmonologists from different regional hospitals join to present difficult-to-control COPD-cases in a standardized format, with a formulated question. Symptoms, medication, disease control and exacerbations, lung function, airway inflammation, thoracic computed tomography, treatable traits, and performance scores are discussed for each patient. Figure (1A) illustrates the various care pathways that can result from the MDC, including (1) recommendations to adjust treatment at the patients’ own centre, (2) suggestions to refer the patient to one or more specialized centres for add-on therapy, and (3) advice to refer the patient for tertiary assessment.
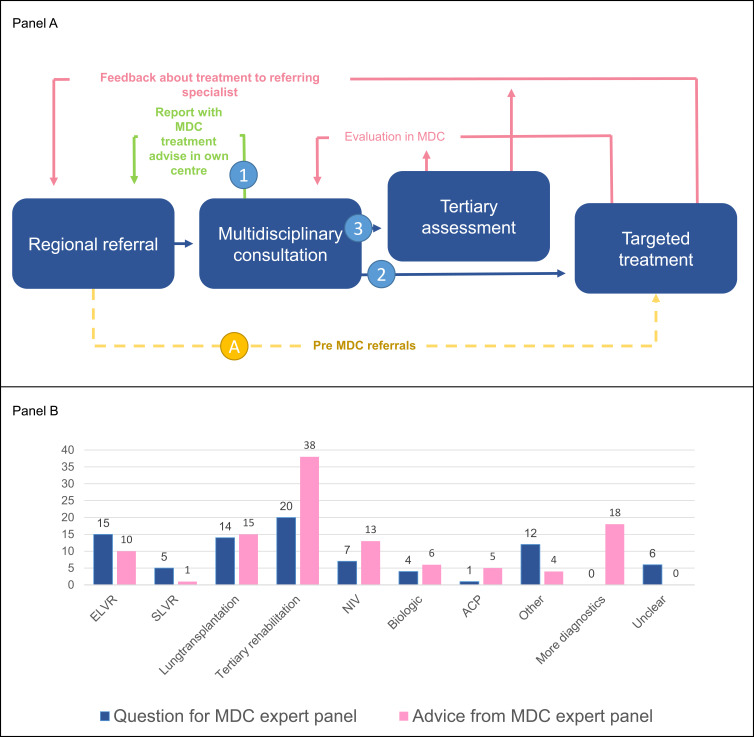
Former (A) and new (1–3) severe COPD care pathways resulting from organizing referrals via a multidisciplinary consultation with experts in different targeted treatments. (B) targeted treatments and advices, divided by the initial question from the referring physician and the advice from the expert panel. (A) shows the pre MDC pathway, in which pulmonologist directly referred to a specialized center, resulting in a single advice for one specific treatment. Pathways 1, 2 and 3 are the novel routes after patients have been presented to the MDC. 1) The referring physician is advised to initiate a certain treatment or additive diagnostics in their own center, 2) referral physicians are advised to refer patients to one of the specialized centers for further treatment, or 3) patients are referred for a tertiary assessment to optimize diagnosis and identify treatable traits (B).
During the initial nine months, the MDC reviewed 61 unique cases from 13 secondary and tertiary hospitals in South-West Netherlands. (Figure 1B) presents the indications for case presentation and the advice provided by the expert panel. In total, 78 specific therapies were proposed to the panel, 110 advices were given by the panel resulting in a discordance of 84%. The most frequently sought indication was for third-line rehabilitation (20 cases), followed by endobronchial lung volume reduction (15 cases) and lung transplantation (14 cases). Multiple recommendations were given in majority of cases, including combinations of third-line rehabilitation with endobronchial lung volume reduction or lung transplantation promoting integrated care. In some cases, the proposed treatment was found to be unnecessary, while alternative advice was provided. The cause of the difference between question for the panel and advice is unknown. Possible reasons may be lack of knowledge of indications of add-on therapies, incomplete filling of the MDC forms by the physicians and multiple stepwise advice (ie, start with non-invasive ventilation awaiting possible lung transplantation).
These findings provide evidence that the implementation of multidisciplinary consultation improves targeted referrals and has the potential to enhance health outcomes for uncontrolled COPD patients. Furthermore, the MDC has improved managing the combination of different add-on treatments with central coordination, specifically when several specialized therapies are indicated. Moreover, this approach helps narrow the knowledge gap among referring physicians regarding targeted treatments for severe COPD. The adoption of the described MDC could offer substantial benefits for both patients and physicians, especially in larger regions.
A multidisciplinary approach has been proven to be effective in improving the quality of life and health outcomes for all COPD patients.4,5 The recent Lancet commission report on COPD by Stolz and colleagues6 mentions multiple suggestions for improving treatment of COPD. Given the complexity and heterogeneity of severe COPD and the development of various add-on therapies, our MDC is a crucial tool not only to guarantee accessibility for all patients with severe COPD but also to streamline the currently available treatments. This will empower local dedicated COPD pulmonologists. In line with our similarly organized and longer standing severe asthma, MDC, which has proven to secure accessibility to specialized care for all patients in our region, reduced referrals and enhanced regional knowledge about severe asthma.7 To our knowledge, this is the first paper describing an MDC for add-on therapies in Severe COPD.
Future steps for enhancing our MDC program involves incorporating advance care planning more comprehensively. Currently, our MDC is used to identify patients who could benefit from advance care planning, but it is not specifically designed as a dedicated care option. This observation is supported by the evaluation over the initial 9-month period, during which advance care planning was only discussed for one patient (Figure 1B). Moreover, the perspective of patients regarding the MDC is currently lacking. We propose that the implementation of a patient advisory board could be advantageous for incorporating the patients’ viewpoint. Additionally, there is currently no direct connection with the general practitioner as part of the care team, despite the significant role they play in the day-to-day management of severe COPD. Finally, quantification of cost saving of healthcare resources due to the centralized MDC advice, instead of sequential duplo or triple analyses in different centers, is needed. Including a comparison between our virtual MDC with participating disciples from multiple centers with referring pulmonologists from external hospitals and an MDC in a hospital in which all disciplines are available.
A known unmet need is the absence of a widely accepted definition of severe COPD, complicating patient selection for our MDC. Currently, there are no clear inclusion or exclusion criteria for our MDC, which likely leads to ambiguity among pulmonologists and unequal patient selection for discussion. Furthermore, there is a need for financial reimbursement to account for the time required for the MDC, ensuring that all critical stakeholders can participate. Finally, establishing a structured registration system for the discussed patients, recommendations, and outcomes would enable proper evaluation and could potentially serve as a model for a national severe COPD registry.
In conclusion, severe COPD represents a complex and heterogeneous disease that poses significant challenges in terms of treatment. The management of severe COPD necessitates input of various specialists, often located in different centres. To ensure optimal and equitable care for all patients, a regional multidisciplinary consultation meeting, involving experts from all relevant centers, is crucial. This collaborative approach allows for comprehensive expertise and enables the development of tailored strategies for all individuals with severe COPD.
Acknowledgments
Participants of Severe Asthma & COPD Network South West Netherlands, besides authors of this research letter:
Esther Vis, MD – Department of Pulmonary medicine, Admiraal de Ruiter ziekenhuis
Chantal Kroese, MD – Department of Pulmonary medicine, Ikazia, Rotterdam, the Netherlands
Stephanie van Loon-Kooij, MD – Department of Pulmonary medicine, Reinier de Graaf ziekenhuis, Delft, the Netherlands
Jeroen van Exsel, MD – Department of Pulmonary medicine, HAGA, Den Haag, the Netherlands
Dennis van Leeuwen, MD – Department of Pulmonary medicine, Spijkenisse Medisch centrum, Spijkenisse, the Netherlands
Jasmijn van Kampen, MD – Department of Pulmonary medicine, MC Haaglanden, Den Haag, the Netherlands
Maurice Jans, MD – Department of Pulmonary medicine, Rivas Beatrixziekenhuis, Gorinchem, the Netherlands
Jelmer Vahl, MD – Department of Pulmonary medicine, Ijsselland ziekenhuis, Capelle aan den IJssel
Remco Djamin, MD – Department of Pulmonary medicine, Amphia ziekenhuis, Breda, the Netherlands
Jacobine Herbrink, MD – Department of Pulmonary medicine, Het van Weel-Bethesda ziekenhuis, Dirksland, the Netherlands
Wouter Blox, MD – Department of Pulmonary medicine, Albert Schweitzer ziekenhuis, Dordrecht, the Netherlands
Jeroen Retera, MD – Department of Pulmonary medicine, Elisabeth-TweeSteden ziekenhuis, Tilburg, the Netherlands
Yordi van Dooren, MD – Department of Pulmonary medicine, Groene Hart ziekenhuis, Gouda, the Netherlands
Disclosure
Dr Gert-Jan Braunstahl reports grants and/or personal fees from GSK, Sanofi, AstraZeneca, ALKAbello, outside the submitted work. Dr Johannes In ‘t Veen reports Unrestricted grant to institution from Teva, Astra Zeneca, Chiesi; Speaker Bureau for Sanofi, Chiesi, GSK, Astra Zeneca, Health Investment, StichtingRoLeX. The authors report no other conflicts of interest in this work.
References
Articles from International Journal of Chronic Obstructive Pulmonary Disease are provided here courtesy of Dove Press
Citations & impact
This article has not been cited yet.
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/160806440
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
The potential for patient-led COPD admission avoidance schemes.
Eur Respir J, 32(4):1128-1129, 01 Oct 2008
Cited by: 0 articles | PMID: 18827166
[Treatment of patients with chronic obstructive pulmonary disease (COPD) by primary care physicians].
Medicina (B Aires), 64(5):445-454, 01 Jan 2004
Cited by: 1 article | PMID: 15560549
Review
Referral and consultation in asthma and COPD: an exploration of pulmonologists' views.
Neth J Med, 61(3):71-81, 01 Mar 2003
Cited by: 4 articles | PMID: 12765227
Guideline-based survey of outpatient COPD management by pulmonary specialists in Germany.
Int J Chron Obstruct Pulmon Dis, 7:101-108, 14 Feb 2012
Cited by: 25 articles | PMID: 22371651 | PMCID: PMC3282602



