Abstract
Free full text

Beyond misinformation: developing a public health prevention framework for managing information ecosystems
Abstract
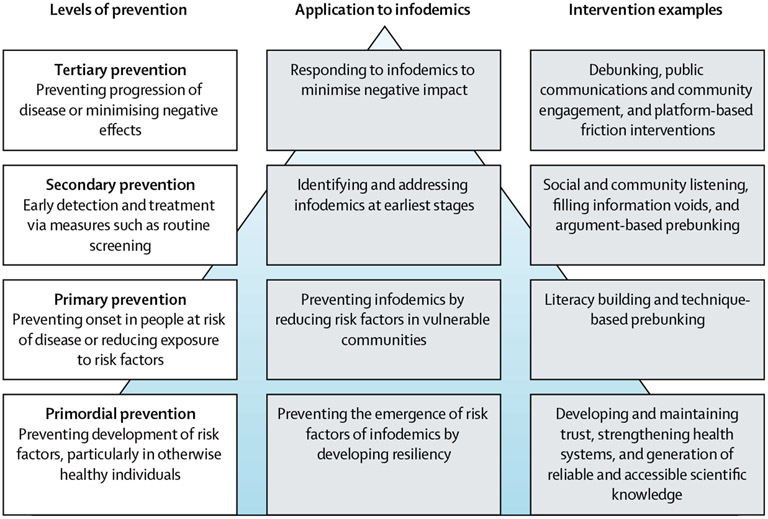
The COVID-19 pandemic has highlighted how infodemics (defined as an overabundance of information, including misinformation and disinformation) pose a threat to public health and could hinder individuals from making informed health decisions. Although public health authorities and other stakeholders have implemented measures for managing infodemics, existing frameworks for infodemic management have been primarily focused on responding to acute health emergencies rather than integrated in routine service delivery. We review the evidence and propose a framework for infodemic management that encompasses upstream strategies and provides guidance on identifying different interventions, informed by the four levels of prevention in public health: primary, secondary, tertiary, and primordial prevention. On the basis of a narrative review of 54 documents (peer-reviewed and grey literature published from 1961 to 2023), we present examples of interventions that belong to each level of prevention. Adopting this framework requires proactive prevention and response through managing information ecosystems, beyond reacting to misinformation or disinformation.
Introduction
The COVID-19 pandemic has highlighted how misinformation, disinformation, information overload, and information voids can pose a challenge and threat to public health. The term infodemic has been used to describe the situation in which there is an overwhelming abundance of information, including false, misleading, or unnecessary information, in digital and physical environments during an epidemic.1 Various factors drive the creation and spread of health misinformation. Issues can arise from predatory journals or preprint papers publishing inaccurate or unverified scientific information, medical professionals spreading disinformation for financial or political gain, or the media misreporting scientific research.2-6 The algorithmic design of social media platforms could also contribute to the dissemination of problematic content.7 Additionally, the absence of credible and accessible health information, often referred to as information voids, can promote misinformation.8 Factors such as consumers’ political views, emotions, age, and ability to process abstract information can also affect their susceptibility to misinformation.9
However, infodemics are not only driven by misinformation and disinformation; rather, they can influence and be influenced by the broader information ecosystem, which refers to the dynamics of how people consume, produce, interact with, and behave around information.8,10 There are two main dimensions to the information ecosystem: the supply side, which is shaped by the quantity and quality of media (including factors such as content and reach of media outlets, internet and mobile penetration and usage, presence of social media platforms, and the legal frameworks that govern the media sector), and the demand side, which encompasses people’s behaviours around media and non-media information sources (including people’s information needs, access to information, trust in sources, information-sharing behaviours, and information literacy).10 During emergencies such as a pandemic, both the supply and demand sides of the information ecosystem can undergo rapid changes. For example, new information sources could emerge and people’s demand for information could increase due to fear or uncertainty.8
Infodemics pre-date the COVID-19 pandemic, but the pandemic raised awareness of their potential to negatively affect public health outcomes. Infodemics are hypothesised to hinder individuals from making informed decisions about their health and consequently lead to morbidity or mortality.11 Examples of harm that have been reported in connection with the COVID-19 infodemic include methanol poisoning, improper use of medications such as hydroxychloroquine and ivermectin for COVID-19 treatment, negative attitudes toward masking, reduced vaccination intent or uptake, and stigma or discrimination against specific population groups at high risk of COVID-19.8,12-17 Moreover, physicians have reported that medical misinformation has made it more difficult for them to provide care for their patients with COVID-19·18 It has been suggested that infodemics could also have broader effects than negative outcomes for that specific health epidemic, such as reduction of public trust in health institutions and economic burden due to increased morbidity and mortality,11,19 including costs that take away resources from other public health activities.
In response, public health authorities, civil society organisations, and other actors have implemented various measures, ranging from fact-checking on social media to training health-care workers in interpersonal communication for addressing patient questions.20 Such efforts have been collectively referred to as infodemic management, defined by WHO as the systematic use of evidence-based approaches to manage infodemics and reduce their effect on health behaviours during health emergencies.21 Infodemic management is a practice that is informed by diverse disciplines, including (but not limited to) epidemiology, risk communication, data science, social and behavioural sciences, media studies, and marketing.22,23
Public health practitioners and academics have proposed various frameworks to describe the crucial components of addressing infodemics. For example, Eysenbach suggested a framework that promotes high-level strategies, such as increasing eHealth literacy and information monitoring.24 Kirk Sell and colleagues similarly presented priorities for a national strategy to address health misinformation in the USA, which includes detailed descriptions of potential interventions (eg, establishing guidelines for reporting on misinformation).25 WHO has proposed a comprehensive set of actions with policy-level recommendations, such as forming strategic partnerships across sectors.1 Scales and colleagues applied epidemiological models to outline a process for managing the COVID-19 infodemic through real-time surveillance and rapid response to misinformation.26
Although these frameworks are useful for public health practitioners, they collectively leave gaps that limit their applicability to the complex and evolving challenges posed by infodemics. Several frameworks provide a wide range of potential interventions but do not give clear guidance on the process for deploying different types of interventions. Other frameworks focus on emergency response and consequently do not account for upstream strategies that address underlying determinants of infodemics. Furthermore, a framework that is based on a single discipline, such as epidemiology, can be too narrow to fully capture the breadth of approaches needed.27
The overall aim of this Health Policy is to propose a unifying, expansive framework that addresses these gaps in existing frameworks—namely their little focus on upstream strategies beyond emergency response, insufficient guidance on identifying and categorising different types of interventions, or narrow scope due to framing infodemic management within one discipline. We sought to present an overview of interventions that can aid public health practitioners and policy makers in conceptualising and strategising their responses to the ongoing and future infodemics, including broader applications to non-acute settings.
Extending the public health prevention model to infodemic management
We chose the public health prevention model to inform the development of our framework because it provides an ideal theoretical basis for addressing the gaps in existing infodemic management frameworks. The public health prevention model is a conceptual framework that outlines distinct stages of prevention efforts aimed at addressing health issues and categorises health interventions into four levels of prevention.28-30
These four levels of prevention are: primordial prevention, which seeks to prevent the emergence of risk factors by addressing environmental, policy, or social conditions;28,31 primary prevention, which aims to prevent the onset of a specific condition in people who are already at risk;28,32,33 secondary prevention, which aims to detect and treat a condition in its early or preclinical stage by implementing measures such as routine medical screening;34,35 and tertiary prevention, which includes interventions that are designed to prevent progression of disease, minimise suffering, or alleviate symptoms to avoid subsequent disability or complications.36,37
The public health prevention model has been used to inform a wide range of public health topics, such as cancer control, cardiovascular disease prevention, mental health promotion, and injury prevention.38-41 Examples of the use of this model include a review of approaches to cancer prevention in low-income and middle-income settings38 and a guide for nurse practitioners to plan a regimen for the prevention of cardiovascular disease in patients who are HIV positive.39 In addition to the widespread use of this model in public health and preventive medicine, its different levels of prevention comprehensively capture both acute and upstream interventions. Furthermore, the model has distinct stages that can help practitioners identify appropriate interventions depending on the intended level of prevention.
For each level of prevention, we sought to apply the same underlying principles to the context of infodemics and provide specific examples of interventions that fall under each level (figure). We then present the implications of our framework, including recommendations for the public health community, and the limitations of our approach.
Primordial prevention: preventing the emergence of risk factors for infodemics
Primordial prevention is the initial stage of preventive measures, which aim to intervene before risk factors for disease emerge in societies or communities. This level involves interventions that address environmental, policy, or social determinants of health, such as designing built environments that promote physically active lifestyles. In the context of infodemics, primordial prevention can include interventions that help develop communities and health systems that are resilient to infodemics.
Developing and maintaining trust
Developing and maintaining trust is a key component of primordial prevention. Research suggests that trust in government, science, or health-care workers can influence levels of belief in misinformation or acceptance of protective health behaviours.42-46 Examples of interventions to develop trust include communication practices by public health authorities and officials that follow established principles of risk communication. These principles include, but are not limited to, acknowledging uncertainty, being transparent, and encouraging dialogue between health authorities and communities.47 Beyond communication practices, routine health programmes and activities that are accessible and functioning for all population groups can also foster trust.48,49 More focused interventions can also be used to increase trust. For example, the Bridging Research, Accurate Information and Dialogue model uses recurring conversation circles (ie, group discussions between community members and experts) as an intervention to develop trust between minority ethnic communities and public health experts.50 Another example includes the use of infographics to explain the process of scientific research to increase trust in science.51
Strengthening health systems
Primordial prevention strategies can address the underlying vulnerabilities within health systems. For example, having sustained financing or human resource management plans for infodemic management can contribute to reducing vulnerabilities within the health system.52 On a more operational level, the Robert Koch Institute in Germany has identified and assessed available data sources for social listening and established a framework and workflow for reporting infodemic insights.53 Another potential intervention is capacity building for health-care workers and public health professionals in areas such as social listening, generation of infodemic insights, and intervention development. WHO has developed a training programme that uses simulation exercises to develop the skills and knowledge of health professionals in these areas.54 Likewise, the European Centre for Disease Prevention and Control has launched an electronic-learning course designed to assist public health practitioners and risk communicators in addressing the spread of vaccination misinformation online.55 More specifically, health-care workers can be trained in skills such as motivational interviewing to effectively interact with patients who might have been exposed to health misinformation.56
Generation of reliable and accessible scientific knowledge
Another form of primordial prevention is the generation of high-quality scientific evidence that is easily accessible. For example, to counter the negative effect of predatory journals disseminating harmful health misinformation, public health professionals can proactively seek to publish their work in peer-reviewed journals that are open-access.2 At an organisational level, academic and public health institutions can establish policies ensuring that their published outputs are freely accessible to the public, similar to WHO’s open access policy.57 Interventions in this area could also involve the retraction of published articles containing false or misleading health information. Alongside systemic safeguards such as journal oversight to enforce retraction or downranking of retracted articles in databases, public health professionals can refrain from citing or endorsing retracted studies.2,58 Moreover, transparency from social media platforms can facilitate the creation of scientific evidence, especially in the realm of infodemic management. For example, the Digital Services Act in the EU includes a provision granting researchers access to data from online platforms or search engines.59 By leveraging such regulations, researchers can strengthen the body of evidence that is needed to inform other types of infodemic management interventions.
Primary prevention: preventing the onset of infodemics among individuals at risk
Primary prevention refers to strategies for preventing the onset of a specific condition among individuals at risk, such as vaccinating individuals to protect them from pathogens that they could be exposed to. Likewise, primary prevention in our proposed framework includes interventions that aim to prevent infodemics from occurring particularly in individuals vulnerable to misinformation or other negative outcomes of infodemics.
Improving literacy
Interventions can be developed to empower individuals who are economically or socially marginalised by improving their health, science, news, or digital literacy. Specific examples of interventions include theory-based education and training programmes to improve digital health literacy in older adults, students, or individuals from low and middle socioeconomic groups.60-62 For example, self-directed online modules and in-person lectures have been used in places such as the USA and South Korea to teach older adults concepts and skills related to online misinformation, web search engines, or reliable information sources.63,64 Similarly, an intervention with an asynchronous online course has been used to improve the ability of American college students to evaluate the credibility of online sources.61 Free digital literacy training curriculum and materials are also available.65
Technique-based prebunking
Broad-spectrum inoculation, or technique-based prebunking, is a type of primary intervention that could empower individuals susceptible to misinformation or at an increased risk of being affected by infodemics.66 Based on psychological inoculation theory, broad-spectrum inoculation exposes individuals to common manipulation techniques to pre-emptively inform them of how they could be misinformed in the future.66-68 For example, short videos can be used to inoculate individuals against commonly used persuasion techniques, such as presentation of false dichotomies or use of emotionally evocative content.67 Similarly, technique-based prebunking can also be used in the form of an online browser game, in which players create and spread hypothetical social media posts while learning how to use common misinformation techniques.69
Secondary prevention: identifying and addressing infodemics at the earliest stages
In public health and preventive medicine, secondary prevention involves measures such as routine medical screening, which enables early detection and treatment of a condition. Similarly, the goal of secondary prevention of infodemics is to proactively identify early warning signs of infodemics and to take swift action to contain them before they affect the wider population.
Social and community listening
One example of secondary prevention is the detection and analysis of infodemic signals, which involves collecting data from both offline and online sources to answer specific research questions or meet predetermined programme objectives. For example, WHO has been monitoring online conversations related to COVID-19 to understand community questions, confusion, and misinformation narratives to identify and prioritise COVID-19 response activities.70 This process is commonly referred to as social listening and involves monitoring of digital, social, and traditional media. To ensure diversity and reduce bias in the data, offline sources (eg, hotline call logs or community polls) can also be used, as shown in the mpox rumour tracking report by Internews71 or the State of Vaccine Confidence Insights Reports by the US Centers for Disease Control and Prevention.72 Data collection and categorisation can be enhanced with artificial intelligence.73 Once quantitative and qualitative data are analysed and synthesised, infodemic insights (ie, learnings about circulating narratives and their level of risk to public health) can be generated to inform activities and intervention development.74
Filling information voids
Another area of secondary prevention is proactive measures to fill information voids. Information voids refer to situations where there is little credible and accessible health information to address community concerns or questions. To address this issue, one strategy that can be used in the early stages of an infodemic is to proactively identify potential information voids and saturate information ecosystems with high-quality health information that directly answers community concerns or questions, if such information is available.75 For instance, the New York City Department of Health and Mental Hygiene identified early on in their COVID-19 misinformation surveillance efforts that community members had concerns about vaccine ingredients. In response, the Department quickly expanded their talking points and developed multimodal materials that addressed vaccine ingredient worries.76 Similarly, during the first wave of the COVID-19 pandemic in 2020 in Madagascar, the non-governmental organisation Doctors for Madagascar had informal interviews with community leaders, health-care workers, and local health authorities to understand the effect of misinformation. On the basis of the information gathered from the interviews, the organisation used live music performances to address information voids about topics such as COVID-19 transmission routes.77 In situations of evolving evidence and scientific uncertainty in which there is scarce high-quality health information, interventions to fill information voids might need to be supplemented by other strategies, such as public communications and community engagement (eg, working with trusted community members or leaders, health organisations, or media outlets) to help guide communities through uncertainty in real-time and with continuous communication activities.8,78
Argument-based prebunking
Narrow-spectrum inoculation, also known as argument-based prebunking,66 could be used at the secondary level to address specific pieces of misinformation detected in the early stages of an infodemic. Although this approach is based on the same theory as technique-based prebunking, it is different because it targets specific false or misleading claims rather than manipulation techniques in general.66,69 An example of argument-based prebunking is delivering messages that caution people about anticipated false claims regarding the safety of mRNA vaccines or the rapid approval of COVID-19 vaccines, which are based on actual instances of misinformation found on social media.79
Tertiary prevention: acute responses to minimise negative effects of infodemics
Tertiary prevention in public health and preventive medicine involves preventing disease progression or alleviating symptoms. Similarly, in our proposed framework, tertiary prevention aims to reduce the negative effect of infodemics on public health. This approach involves implementing reactive activities to slow the spread of an infodemic or mitigate the negative effect of an infodemic on people’s health or public health programmes after the infodemic has become established.
Debunking
One type of tertiary prevention that has been widely used includes debunking or fact-checking, which consists of refuting inaccurate claims or misperceptions with factual information.80 Debunking can include the use of credible information with links to expert sources, offering an alternative explanation for the misinformation, and delivering repeated corrections.80 Health-care professionals, government ministries of health, news media, and hospitals have implemented strategies and activities to debunk health misinformation.81-83
Public communications and community engagement
Public and mass communication strategies can also be considered a form of tertiary prevention. This approach involves the dissemination of accurate and evidence-based health information across various channels and in multiple formats. For example, communication strategies to inform the public during the COVID-19 pandemic included, but were not limited to, the use of toll-free hotlines, billboards, leaflets, press briefings, social media, and websites.84 In addition to the traditional channels used to disseminate evidence-based health information, the optimisation of web traffic and search engine visibility can be used.85 To further enhance engagement with hard-to-reach communities, public health practitioners have also adopted strategies such as working with messengers trusted by the community (eg, faith leaders, small business owners, and community-based organisations).48,86 Partnerships with the media sector can also be considered to prevent inaccuracies or exaggeration in reporting.2 For example, the Pan American Health Organization released a guide for journalists to help them with responsible coverage of COVID-19.87 Furthermore, insights gathered through community listening can enhance public communication through activities such as adaptation and updating of campaign content.88
Platform-based friction interventions
Platform-based friction interventions could help prevent the spread of harmful misinformation in digital and social media as a form of tertiary prevention. These interventions introduce obstacles (ie, friction) that make it more difficult for harmful misinformation to spread, including content moderation and platform regulation.89,90 For example, by removing or flagging conspiratorial content on platforms such as X (formerly known as Twitter), Reddit, and Facebook, they become less likely to reappear in the information ecosystem.90 WHO has collaborated with digital and social media companies to review and enhance their misinformation moderation policies.91 Furthermore, behavioural interventions such as simple reminders or nudges that encourage people to consider the accuracy of the information they encounter could help stop the spread of false information on social media.92-94 Visual cues to signal verified accounts has also been proposed as a strategy to highlight domain-specific expertise and, consequently, prevent pseudoscientific claims on social media.2 Although the implementation of these interventions typically does not fall within the mandate of public health authorities, public health researchers or practitioners could support formative research and implementation research to develop, implement, or evaluate such interventions. Such efforts could be particularly meaningful in the context of some social media platforms changing or weakening their content moderation policies.95
Discussion
Addressing infodemics through the preventive lens of public health offers several advantages. This framework expands the scope of infodemic management beyond emergency response, while still recognising its importance, and emphasises the need to develop upstream interventions before public health emergencies occur. Furthermore, this breadth encourages public health professionals to consider developing interventions beyond only responding to misinformation, such as debunking or other communication interventions.
Taking a broad preventive approach involves the consideration of the information ecosystem. An information ecosystem approach ensures that public health interventions are effective by considering all levels of prevention, including routine activities that address infodemics. Focusing resources and interventions on only secondary and tertiary levels will probably leave gaps in addressing the full range of challenges that infodemics present and could result in inadequately addressing underlying social, cultural, and historical factors. Developing interventions to increase trust at the primordial and primary levels would help increase population resilience before public health emergencies occur and shows the importance of upstream strategies for addressing infodemics alongside acute responses. For example, higher levels of trust in health-care workers or governments appear to be associated with decreasing levels of belief in misinformation or conspiracies.44-46
The information ecosystem approach also highlights that misinformation is just one aspect of a complex ecosystem and is not created or consumed in isolation. Factors from the demand side of an information ecosystem, such as people’s information needs,96 literacy levels,97 or trust in specific political leaders,98 have been proposed to shape the emergence or circulation of misinformation. Additionally, factors from the supply side, such as the design of social media platforms99-101 or the quality of information from public figures,102 have been suggested to play a role in influencing the spread of misinformation. Thus, although reactive interventions to counter misinformation (eg, debunking or mass communication) are crucial in some contexts, they should not be the sole focus.
Enacting this framework would require a paradigm shift within public health and would probably require policy-level or systems-level attention for allocating technical, financial, and human resources to the management of information ecosystems. Coordinated effort and collaboration between various actors would be necessary for interventions to be consistently and comprehensively designed and implemented, especially at the primordial and primary prevention levels. Civil society organisations, educational systems, media organisations, and other community-based organisations all play an important role in addressing underlying vulnerabilities of communities in the context of information ecosystems. Moreover, robust partner networks can be used across multiple levels of prevention; for example, a strong network of fact-checking organisations can be instrumental in developing trust, identifying information voids, or disseminating health information to diverse communities. Additionally, it is essential to identify, work directly with, and address the needs of community members who are particularly susceptible to infodemics, such as communities with language barriers or historically marginalised communities with low trust in health authorities. A practical approach for public health authorities and practitioners to help in achieving this is by prioritising community-centred interventions, exemplified by the Bridging Research, Accurate Information and Dialogue model50 mentioned earlier.
It could also be necessary to conduct assessments within health systems to identify organisational barriers that impede the implementation of management strategies of information ecosystems. Health authorities should continue to review and evaluate their management strategies for the COVID-19 infodemic, including risk communication approaches. This evaluation could yield insights that improve the implementation of interventions to manage information ecosystems, especially in the context of rebuilding trust. Specifically, it is important to reflect on whether risk communication by health authorities could affect public confusion or misinterpretation during health emergencies. Examples of such challenges might include difficult-to-understand policy guidance documents, changing stances on virus transmission, and inconsistent advice regarding masking.103-105
However, an information ecosystem approach could also result in ethical pitfalls. Within preventive public health, quaternary prevention has been defined as protecting individuals from medical interventions that are likely to cause more harm than good. Some publications have defined quaternary prevention even more broadly, extending beyond the prevention of overdiagnosis or overtreatment, and positioning it as an ethical approach that applies to other levels of disease prevention.106,107 This approach is especially crucial when considering the potentially unethical or harmful consequences of infodemic management interventions,108 such as concerns about privacy, the effect of content moderation on free speech, and the monitoring of closed social media. The concept of quaternary prevention appears to be new and less established in the context of infodemic management interventions. Therefore, we did not include it in the proposed framework, but examples such as ongoing efforts to create ethical guidelines for social listening109 can be classified as quaternary prevention and could be added as another layer.
Our framework can also be potentially expanded by considering regulatory and legal interventions specifically tailored to address disinformation. For example, legislators, medical boards, or professional associations could implement disciplinary measures for health professionals who spread disinformation, such as revoking their certification or licenses.110,111 In Europe, the law enforcement agency Europol has removed online links to advertisements or marketplaces promoting fake COVID-19 pharmaceutical products.112 These strategies are typically not within the purview of public health and were therefore not included in our framework. However, public health professionals could explore areas such as counter-disinformation governance and cyber security, while also considering the ethical implications of applying these interventions to public health.113
We acknowledge several limitations to our approach. First, there are intrinsic limitations of a narrative review, such as selection bias. For example, our review of interventions was limited to literature published in English, which could have resulted in the omission of relevant interventions and studies discussed in other languages. Second, although we have provided examples of interventions within each level of prevention, we were not able to comment on the effectiveness of the interventions in a systematic way. Further research is needed to evaluate the effectiveness of the interventions and determine which ones are most effective in different contexts.11,23 Third, our proposed framework does not outline specific timings for starting various interventions. We acknowledge the importance of considering timing when preventing and responding to infodemics in practice, especially in settings where it is not feasible to continuously do all four levels of prevention. Decisions about when to start interventions are contextual and require consideration of factors such as the available resources and the nature of the current infodemic-related issues. Fourth, some interventions have elements that can encompass multiple levels of prevention, making it less clear-cut to categorise them into a single level. For instance, community engagement can be applied to activities to develop trust or public communication. Therefore, the prevention framework should serve as a guide rather than a rigid categorisation system.
Ultimately, the framework we propose highlights a gap in the existing literature on infodemiology and a need for research to better establish the chains of causality between the levels of prevention. Associations between risk factors, information exposure, health behaviours, and health outcomes must be better understood. Researchers must investigate the relative effects of different components of the information ecosystem, including not only misinformation and disinformation but also information overloads and information voids. Developing indicators for measuring the effect of exposure to misinformation, disinformation, information voids, and information overloads is also crucial, particularly regarding their effects on the intent and uptake of health behaviours. Such indicators can also promote formative research to identify communities or individuals susceptible to infodemics, which is particularly important for effective development of interventions at the primary prevention level. In the same way we approach any challenge in public health, combining a preventive and holistic approach requires a better understanding of the overall ecosystem, and only then can we be prepared for future infodemics.
Acknowledgments
The findings, conclusions, and views expressed in this article are those of the authors and do not necessarily represent the official position of the Task Force for Global Health, US Centers for Disease Control and Prevention (CDC), the US Department of Health and Human Services, the School of Public Health at Brown University, or the Commissioned Corps for the US Public Health Service. We thank Abigail Shefer (US CDC, Atlanta, GA, USA), Shibani Kulkarni (US CDC, Atlanta, GA, USA), and Sabrina L Jin (US CDC, Atlanta, GA, USA) for their contributions to this manuscript. During the preparation of this work the authors used ChatGPT in order to improve readability. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Contributor Information
Atsuyoshi Ishizumi, Task Force for Global Health, Decatur, GA, USA; US Centers for Disease Control and Prevention, Atlanta, GA, USA.
Jessica Kolis, US Centers for Disease Control and Prevention, Atlanta, GA, USA.
Neetu Abad, US Centers for Disease Control and Prevention, Atlanta, GA, USA.
Dimitri Prybylski, US Centers for Disease Control and Prevention, Atlanta, GA, USA.
Kathryn A Brookmeyer, US Centers for Disease Control and Prevention, Atlanta, GA, USA.
Christopher Voegeli, US Centers for Disease Control and Prevention, Atlanta, GA, USA.
Claire Wardle, School of Public Health, Brown University, Providence, RI, USA.
Howard Chiou, US Centers for Disease Control and Prevention, Atlanta, GA, USA; Commissioned Corps, US Public Health Service, Rockville, MD, USA.
References
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/162699465
Article citations
Harm reduction techniques among cisgender gay, bisexual, and queer men using anabolic androgenic steroids: a qualitative study.
Harm Reduct J, 21(1):196, 11 Nov 2024
Cited by: 0 articles | PMID: 39523302 | PMCID: PMC11552109
Exploring organizational aspects that promote health-related preventive behavior: using the example of work-related SARS-CoV-2 infection control measures in Germany, August 2020 to November 2021.
Front Public Health, 12:1388996, 02 Oct 2024
Cited by: 0 articles | PMID: 39416946 | PMCID: PMC11480029
Detecting and monitoring concerns against HPV vaccination on social media using large language models.
Sci Rep, 14(1):14362, 21 Jun 2024
Cited by: 0 articles | PMID: 38906941 | PMCID: PMC11192875
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
A Public Health Research Agenda for Managing Infodemics: Methods and Results of the First WHO Infodemiology Conference.
JMIR Infodemiology, 1(1):e30979, 01 Jan 2021
Cited by: 45 articles | PMID: 34604708 | PMCID: PMC8448461
Framework for Managing the COVID-19 Infodemic: Methods and Results of an Online, Crowdsourced WHO Technical Consultation.
J Med Internet Res, 22(6):e19659, 26 Jun 2020
Cited by: 222 articles | PMID: 32558655 | PMCID: PMC7332158
A Comprehensive Analysis of COVID-19 Misinformation, Public Health Impacts, and Communication Strategies: Scoping Review.
J Med Internet Res, 26:e56931, 21 Aug 2024
Cited by: 0 articles | PMID: 39167790 | PMCID: PMC11375383
Review Free full text in Europe PMC
Infodemics and Vaccine Confidence: Protocol for Social Listening and Insight Generation to Inform Action.
JMIR Public Health Surveill, 10:e51909, 24 Oct 2024
Cited by: 0 articles | PMID: 39447166 | PMCID: PMC11544329
Funding
Funders who supported this work.
Intramural CDC HHS (1)
Grant ID: CC999999