Abstract
Free full text

ERS International Congress 2023: highlights from the Respiratory Infections Assembly
Abstract
The 2023 European Respiratory Society Congress took place on a hybrid platform, with participants joining online and in-person in Milan, Italy. The congress welcomed over 20 000 attendees, bringing together exciting updates in respiratory science and medicine from around the world. In this article, early career members of Assembly 10 (Respiratory Infections) summarise a selection of sessions across a broad range of topics, including presentations on bronchiectasis, nontuberculous mycobacteria, tuberculosis, cystic fibrosis and coronavirus disease 2019.
000 attendees, bringing together exciting updates in respiratory science and medicine from around the world. In this article, early career members of Assembly 10 (Respiratory Infections) summarise a selection of sessions across a broad range of topics, including presentations on bronchiectasis, nontuberculous mycobacteria, tuberculosis, cystic fibrosis and coronavirus disease 2019.
Tweetable abstract
This highlights article provides valuable insight into the latest scientific data and updates in clinical practice from Assembly 10 (Respiratory Infections) at #ERSCongress 2023 https://bit.ly/49Mauv1
Introduction
The European Respiratory Society (ERS) International Congress took place in Milan, Italy, in September 2023. The congress welcomed over 20 000 attendees on a hybrid platform, bringing together exciting updates in respiratory science and medicine from all over the globe. Following each congress, early career members of the Respiratory Infections Assembly (Assembly 10) produce a highlights article, summarising interesting sessions from this assembly [1–3]. The current article features sessions across a broad range of topics, including presentations on pneumonia, coronavirus disease 2019 (COVID-19), bronchiectasis, nontuberculous mycobacteria (NTM), tuberculosis (TB) and cystic fibrosis.
000 attendees on a hybrid platform, bringing together exciting updates in respiratory science and medicine from all over the globe. Following each congress, early career members of the Respiratory Infections Assembly (Assembly 10) produce a highlights article, summarising interesting sessions from this assembly [1–3]. The current article features sessions across a broad range of topics, including presentations on pneumonia, coronavirus disease 2019 (COVID-19), bronchiectasis, nontuberculous mycobacteria (NTM), tuberculosis (TB) and cystic fibrosis.
Group 10.01: Respiratory infections and bronchiectasis
State of the art session – management of respiratory infections: the future and the present
Paul G. Thomas (Memphis, TN, USA) opened the session by discussing the fundamental role of lung fibroblasts in maintaining extracellular matrix (ECM) integrity against the recruitment of immune cells [4]. Distinct fibroblast activation states include the ECM-synthesising, damage-responsive and interferon-responsive types. Persistent activity and differentiation to myofibroblasts at late stages of viral infection predispose to chronic inflammation and fibrosis, mediated by ADAMTS4 matrix proteinase [5]. Detected in lower respiratory tract samples, ADAMTS4 indicates unfavourable outcomes in healthy individuals with influenza or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), promoting inflammation and matrix degradation. Its downregulation potentially improves outcomes without impeding viral clearance. ADAMTS4 exerts protective activity against Streptococcus pneumoniae-induced acute airway inflammation, allowing prompt neutrophil migration in bacterial infection. Development of adjunctive fibroblast-targeted agents may enhance respiratory infection management.
Sanjay Haresh Chotirmall (Singapore) explored the lung microbiome as part of a holistic approach to chronic respiratory disease endo-phenotyping [6]. Dysbiosis of the microbiome [7–11] and disrupted lung–gut axis driven by the presence of Pseudomonas [12] in the lungs are associated with disease severity and poor outcomes in stable disease. Neisseria subflava, although previously considered commensal, is a pathobiont in bronchiectasis [13], while air-fungal sensitisation correlates with worse COPD outcomes [14], outlining the impact of environmental exposure [15]. Microbiome identity profiles remain stable during exacerbations, comprising a conserved “core” part and an ancillary part of exacerbation-related pathogens which alter functional composition [16, 17]. Antimicrobial resistance patterns constitute distinct “resistotypes” [18], which are modifiable by antimicrobials. Future antimicrobial clinical trials may warrant stratification by microbiomes to detect key outcomes.
Christophe Carnoy (Lille, France) introduced the European FAIR project inaugurating an adjunctive immunomodulatory approach to antimicrobial-resistant bacterial pneumonia, based on flagellin [19, 20]. Refined by simulation platforms, preclinical experiments were confirmatory against different pathogens and yielded relevant biomarkers (multiomics). Aerosol delivery of the FLAMOD product minimises the systemic impact and required dose. The project is currently conducting toxicology studies in non-human primates, showing homogeneous airway deposition and good tolerance. Scheduled in 2024, a randomised controlled phase 1 dose-escalating trial will assess safety and determine the lowest dose in healthy volunteers. Stratification markers will disclose the target pneumonia population (BIO-PNEU clinical study), while both a patient and clinician cohort exhibit promising prospective acceptability.
Jessica Rademacher (Hannover, Germany) encouraged vaccination in children and adults to prevent S. pneumoniae severe infections and related COPD and asthma exacerbations. Covering more serotypes, a single-dose PCV20 vaccine suffices in adults [21], but sequential PCV15-PPSV23 vaccination is also recommended as per the latest Advisory Committee on Immunization Practices (ACIP). Patients with COPD should receive both pneumococcal and influenza vaccination [22], but commonly refrain due in part to a lack of recommendation by physicians [23]. Apart from the seasonal pandemic and exacerbations of chronic diseases, influenza vaccination also prevents acute cardiovascular events [24]. The adjuvanted MF59 [25] and high dose haemagglutinin (60 μg) [26] vaccines have established effectiveness. To date, two protein-based vaccines against respiratory syncytial virus (RSV) are licensed. A single dose may be administered in adults ≥60 years based on shared clinical decision-making and in individuals at increased risk for severe disease (ACIP). We anticipate the upcoming follow-up results from RSVPreF3 OA phase 3 trial, along with novel vaccines [27, 28].
Acute respiratory infections: what's new? Respiratory medicine meets other disciplines
This oral session was a joint ERS/European Scientific Working Group on Influenza (ESWI) collaboration. The session aimed to provide an update about the latest data on the evolution, epidemiology, pathogenesis, prevention and treatment of influenza, COVID-19 and other respiratory viral infections; to discuss disease pathogenesis with a focus on systemic and mucosal biomarkers; and to discuss strategies to prevent infection by vaccination and management of viral infections.
The session started with Collin Russell (Amsterdam, the Netherlands) showing evidence that seasonal respiratory virus epidemics have returned as a major public health burden, after a significant reduction during the COVID-19 pandemic. Data reveal that influenza and SARS-CoV-2 have both evolved during the last 3 years [29]. Results from RSV in healthy term-born infants demonstrated that RSV leads to the hospitalisation of one in every 56 healthy infants and that immunisation of pregnant woman is a key step to reduce the healthcare burden [30].
Peter Openshaw (London, UK) focused his talk on the mucosal immune response against these respiratory viruses [31]. The comparison between the systemic immunity, induced by intramuscular vaccines, and the mucosal immunity induced by nasal vaccines, demonstrated the compartmentalisation of immunity. The studies presented during this talk, such as ISARIC 4C and PHOSPH-COVID, provided unique insights into the need for monitoring local mucosal immunity by using nasosorption devices [32].
Regarding prevention, Hanna Nohynek (Helsinki, Finland) discussed the latest updates on vaccines against respiratory infections, including COVID-19, invasive pneumococcal disease (IPD), influenza and RSV. Very few respiratory infections were diagnosed during COVID-19 pandemic, but they are now returning and efforts are needed to work on vaccine prevention. For COVID-19, the long-term aim is to develop a broadly protective coronavirus vaccine [33]. For IPD, influenza and RSV, new vaccines are in development using the newest technology and with different target indications, especially for IPD (paediatric, maternal or elderly) [34]. In conclusion, countries need to make a decision on vaccine implementation and to speed up several key steps that participate in vaccine approval. Therefore, although progress is underway, more work is still needed.
Finally, the session finished with the talk of Maxime Patout (Paris, France) focused on new insights for the management of non-COVID-19 respiratory infections. The clinical benefits for three different types of treatments, such as prone positioning, continuous positive airway pressure and steroids were reviewed [35–37]. Data suggested that there is not enough evidence to support their use in non-severe COVID-19 patients. Therefore, more randomised controlled trials are needed to elucidate their use and personalised medicine may help in the management of respiratory infections.
Preconception origins of respiratory disease and allergy: what about immunity and infections?
This session consisted of four talks, showcasing the paradigm that respiratory health and disease are influenced by factors acting before conception [38].
Cecilie Svanes (Bergen, Norway) summarised the main epidemiological findings in different human cohorts and gave an overview of the main factors associated with respiratory disease in the future child. Based on data from the multigenerational RHINESSA study, the prospective children of boys who started to smoke before the age of 15 have a higher risk of asthma and lower lung function [39]. Potential underlying mechanisms were proposed by the RHINESSA cohort on the effect of a father's preconception smoking, in which Kitaba et al. [40] found that overall 19 DNA methylation changes were detected across 14 genes in children of pubertal onset smokers, associated with offspring outcomes in asthma, wheezing and body mass index (BMI). Mothers’ exposure to cleaning agents long before conception is a risk factor for offspring wheezing and asthma [41]. From both the maternal and paternal sides, TB or helminths increase the risk of respiratory disease, relating to both epigenetic and cell immunity changes [42]. The main factors leading to altered phenotypes in the offspring are summarised in figure 1.
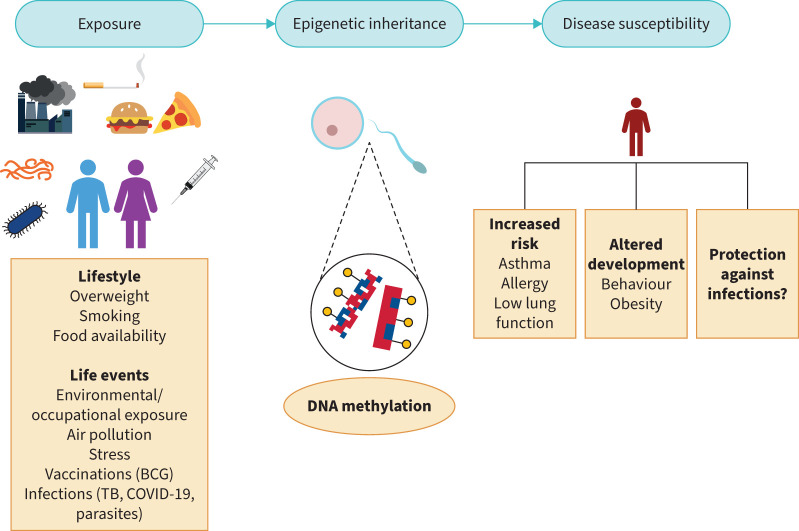
Exposures including lifestyle factors and infections can influence the risk of chronic diseases at the individual level and in the future offspring. Epigenetic changes such as DNA methylation can be perpetuated to the future child, thus inducing potential amendments in phenotypes associated with disease susceptibility and immunity. BCG: bacille Calmette–Guérin; TB: tuberculosis; COVID-19: coronavirus disease 2019.
William Horsnell (Exeter, UK) described murine models used to establish the long-term effects of maternal vaccination, the mechanisms that may support these effects, and the influence of maternal immunity transfer to offspring. Offspring of unvaccinated (MU) or PCV-13 vaccinated (MV) H2Dd/H2Kb female mice were infected with S. pneumoniae strains. Offspring of MV mothers had lower bacterial burden and a high level of maternal protection associated with raised levels of vaccine-specific antibodies. In line with the theory of feto-maternal microchimerism [43], wild-type offspring born to MV IL-4R−/− mothers did not acquire maternal B-cells and had impaired antibody protection. Briefly, the data suggest that maternal vaccination causes long-lasting antibody-mediated immunity and via B-cell maternal microchimerism cell immunity transferred to the offspring can be a determining factor in future immune responses.
Anthony J. Hannan (Parkville, Australia) presented a brief overview of transgenerational epigenetic factors that influence future offspring's disease susceptibility. In a murine model, paternal stress and elevated glucocorticoid exposure induced changes in the microRNA profile of paternal sperm, triggering anxiety in male offspring, and small RNA analysis of sperm showed elevated levels of small non-coding RNAs related to growth factors [44]. The epigenetic state of the sperm can drive transcription in the embryos and transfer intergenerational information [45]. The epigenetic inheritance can be altered by DNA methylation at imprinted genes, sperm small non-coding RNAs, and long-coding RNAs; all can influence offspring phenotypes. A mouse model with Toxoplasma gondii provided evidence that paternal infection can cause changes in the sperm small RNA profile and demonstrated behavioural changes via intergenerational inheritance [46].
Finally, Maria Lerm (Linköping, Sweden) provided insights into the main methods in the investigation of DNA methylation and her research in connection with TB and COVID-19 exposures. Bacille Calmette–Guérin (BCG)-vaccinated subjects showed epigenetic reprogramming and altered DNA methylation of immune cells, resulting in enhanced anti-mycobacterial immunity [47]. Moreover, SARS-CoV-2 can bring about long-standing favourable changes in DNA methylation patterns, associated with better recovery and anti-viral immunity [48]. Protection against infections can be transferred across generations, but data about the future DNA methylation pattern in the offspring are lacking [49]. M. Lerm investigated the peripheral blood mononuclear cells of babies whose mothers had COVID-19 and unveiled that various genes have epigenetic modifications. Preliminary results suggest that epigenetic rewiring can be a decisive factor in the protection against infections in the offspring.
War, climate change, migration and respiratory infections
This oral session discussed some of the urgent interconnected problems influencing respiratory medicine all over the world.
Giovanni Battista Migliori (Varese, Italy) started the discussion with a report about the acute respiratory infections (ARIs) in crisis-affected populations. In a number of recent wars and natural disasters, the death toll can be driven by “indirect” factors. This can include the increased risk of disease and case-fatality brought about by conditions such as displacement into overcrowded camps, food insecurity and breakdown of public health services rather than the direct effects of the crisis. The majority of ARI deaths are driven by acute lower respiratory infections (ALRIs), mainly pneumonia. Nearly all severe ALRI episodes occur in children under 5 years, the elderly and the immunocompromised. In children, viral aetiology accounts for 25–50% of pneumonia cases, predominantly driven by RSV, parainfluenza and influenza viruses. Approximately 50% of cases include either a primary or secondary bacterial infection [50]. At the same time, overcrowded conditions in refugee centres contributed to increased ARI incidence rate, measles transmission and TB detection. This is due in part to the destruction of healthcare services, exposure to high pathogen densities, aggravating weather conditions, regional disease endemicity and low vaccination coverage [51]. G.B. Migliori highlighted the effects of war on the transmission of TB, using a World War I transmission model: war leads to a two-fold risk of developing TB, longer infection cycles and increased multidrug resistance. It is estimated that worldwide, in 2019 there were 272 million migrants out of a global population of 7.7 billion: one in every 30 people [52].
ERS President, Carlos Robalo Cordeiro (Coimbra, Portugal), continued the session with a speech about climate change and respiratory infections, showing that air pollution and climate change are ranked as the World Health Organization's number one threat to global health [53]. C.R. Cordeiro highlighted that air pollution and climate change as well as vaccine hesitancy [54] contribute to the development of respiratory disease. Climate change can lead to health impacts directly, through factors such as heat stress and flood damage, indirectly, through disease vectors, and also through economic and social disruption. These factors are associated with increases in mortality, hospital and intensive care unit admission and visits to general practice. Recently published evidence suggests that climate change can have a direct impact on the sustainability and susceptibility of viral infections, through reductions in anti-viral response, changes to cell surface receptor expression and viral entry, and disruption to epithelial barrier function [55]. On the topic of air pollution, a recent joint workshop report from the ERS, International Society for Environmental Epidemiology, Health Effects Institute and World Health Organization found that long-term exposure to outdoor air pollution can increase the risk of infection and death from COVID-19 [56]. Finally, C.R. Cordeiro concluded with the ERS commitment to sustainability, outlining the work that the ERS has implemented regarding sustainable practices and climate protection projects.
Marijke Proesmans (Leuven, Belgium) considered the effect of climate changes and migration on infection in the paediatric population by epigenetic modifications, placental effects, endocrine and immunological changes, and particulate matter transplacental translocation. Maternal exposure to indoor pollution showed long-term effects, including reductions in forced expiratory volume in 1 s (FEV1) and increased wheeze over 5 years [57]. She also indicated a positive correlation between ambient extreme heat and paediatric morbidity due to paediatric infections and asthma [58].
Finally, Dennis Falzon (Geneva, Switzerland) named COVID-19 a principal point of strong connection between health insults and increased migration. He showed that the major factors that drive the health of refugees and migrants were leadership and governance, financing, service delivery, access to medical products, vaccines and technologies, health information systems, and health workforce [59].
Bronchiectasis
The session on bronchiectasis began with a late-breaking abstract of a multicentre study presented by Lianjun Lin (Beijing, China). L. Lin demonstrated the potential for bronchoalveolar lavage fluid amylase levels as a highly sensitive and specific clinical biomarker for the diagnosis of aspiration, a known bronchiectasis aetiology which is notoriously difficult to diagnose [60].
The session included a wide array of cutting-edge data stemming from the EMBARC registry. Amelia Shoemark (Dundee, UK) presented exciting translational data from the EMBARC-BRIDGE study highlighting distinct metabolomic differences in the neutrophils of bronchiectasis patients versus healthy, age-matched controls, and that metabolomic profiles change according to disease severity. Jennifer Pollock (Dundee, UK) presented EMBARC registry data showing that inhaled corticosteroids (ICS) significantly reduce exacerbations and hospitalisations in bronchiectasis patients with a blood eosinophil count >300 cells·µL−1, with no obvious relationship with mortality, a finding which may advance the development of clinical trials of ICS in this eosinophilic sub-group. Letizia Traversi (Cittiglio, Italy) also presented registry data identifying the significant over/misdiagnosis of COPD in bronchiectasis patients and that the ROSE criteria [61] are a reliable and robust tool for diagnosing COPD–bronchiectasis overlap, a clinically meaningful population shown here to be more clinically severe.
Further advocating for tools for more robust diagnostics, Alejandro A. Diaz (Boston, MA, USA) presented interesting data advocating for the inclusion of artificial intelligence based lung imaging in identifying bronchiectasis in those with COPD, and that COPD individuals with suspected bronchiectasis had increased all-cause mortality, further reinforcing the clinical severity of the COPD–bronchiectasis overlap.
As well as the EMBARC registry, data from the UK Bronchiectasis Registry were also shared. Jennifer Pollock (Dundee, UK) gave a second presentation drawing attention to the prevalence and clinical impact of psychological morbidity in those with bronchiectasis, where anxiety and depression were common and associated with clinical severity and poor outcomes, and the importance of psychological screening in bronchiectasis care.
Impressive results using clinical samples from two key bronchiectasis clinical trials were also shared. Using samples from the phase 2 WILLOW trial of brensocatib [62], Lidia Perea (Barcelona, Spain) showed that brensocatib significantly increases airway levels of secretory leukocyte protease inhibitor, an antiprotease which may dampen the inflammatory response seen in those with bronchiectasis. In addition, using samples from the iBEST trial of inhaled tobramycin [63], Michael Tunney (Belfast, UK) confirmed that quantitative PCR can effectively detect specific pathogens, such as Pseudomonas aeruginosa, within clinical samples and has potential as an effective clinical trial endpoint in investigations concerning antimicrobials.
Rebecca Hull (Dundee, UK) went on to highlight the extreme heterogeneity of P. aeruginosa clones isolated from bronchiectasis patients and that specific variants within these clones are associated with increased biofilm formation or, alternatively, reduced growth in vitro, findings with potential implications for future anti-pseudomonal therapies.
Rounding off the session, Ivan Barone (Milan, Italy) gave an excellent overview of the impact of cardiovascular events in those with bronchiectasis, emphasising a strong association between both conditions and a prominent need for screening and a multidisciplinary care approach in bronchiectasis.
Group 10.02: Tuberculosis and nontuberculous mycobacterial diseases
Advances in the epidemiology, diagnosis and treatment of TB and NTM disease
In this oral session, nine presenters each gave a 5-min presentation about their work on TB and NTM.
Ole Skouvig Pedersen (Aarhus, Denmark), presented a meta-analysis on global treatment outcomes of extensively drug-resistant TB [64]. In an analysis of 94 studies with 10 223 patients recruited from 2005 to 2023, the authors reported a pooled success of 44.2%, with a slight improvement after 2013. Management of multidrug-resistant (MDR)-TB was discussed by Nana Kiria (Tbilisi, Georgia), reporting safety and efficacy of the BPaL (bedaquiline, pretomanid and linezolid) [65] regimen in Georgia in a retrospective study of 16 patients who all achieved sputum conversion after a mean of 33 days, with only four patients experiencing adverse effects.
223 patients recruited from 2005 to 2023, the authors reported a pooled success of 44.2%, with a slight improvement after 2013. Management of multidrug-resistant (MDR)-TB was discussed by Nana Kiria (Tbilisi, Georgia), reporting safety and efficacy of the BPaL (bedaquiline, pretomanid and linezolid) [65] regimen in Georgia in a retrospective study of 16 patients who all achieved sputum conversion after a mean of 33 days, with only four patients experiencing adverse effects.
Karen Wolmarans (Cape Town, South Africa) gave preliminary data on lung function and positron emission tomography (PET)/computed tomography (CT) findings in a cohort of 106 patients with clinical response to TB treatment and a negative sputum culture for TB after 16 weeks of treatment. They found that patients with persistent lung inflammation, defined as standardised uptake value >50 with PET/CT scans, had a statistically relevant lower diffusing capacity, FEV1 and forced vital capacity (FVC). Lung function tests as a means of addressing post-TB lung disease [66] were also the subject of a meta-analysis from Sharenja Ratnakumar (London, UK). Data from 13 studies reporting on 62 932 patients showed that TB survivors have significantly decreased lung function compared to healthy controls, with FEV1 more affected than FVC.
932 patients showed that TB survivors have significantly decreased lung function compared to healthy controls, with FEV1 more affected than FVC.
A case series from Jee Whang Kim (Leicester, UK) showed outcomes following PET/CT and targeted invasive sampling in four asymptomatic immunocompetent household pulmonary TB contacts with normal chest radiographs. The study found metabolically active culturable TB infection, prior to features of subclinical disease becoming evident with clinical screening.
Mirae Park (London, UK) analysed the diagnostic accuracy of TB PCR testing for the detection of Mycobacterium tuberculosis in bronchoalveolar lavage samples in culture-positive pulmonary TB cases and found it more accurate than smear microscopy.
Dong Nguyen Van (Da Nang, Vietnam) presented a meta-analysis of two- versus three-drug regimens in the treatment of Mycobacterium avium [67]. Seven randomised controlled trials were examined comparing efficacy of the two treatments regarding bacteriological responses, mortality, and acquired macrolide resistance, and no statistically relevant differences were found. Jann-Yuan Wang (Taipei, Taiwan) explored in a prospective multicentre study the application of electronic nose (eNose), a breathomics analyser [68], in the clinical assessment of patients with confirmed NTM colonisation. Accuracy of eNose in confirming NTM pulmonary disease, measured as area under curve, was similar to that of an expert panel. Ying Na Ho (Singapore) presented a study of longitudinal 7 years follow-up of lung functions in patients affected by Mycobacterium abscessus pulmonary disease (MAPD) [67]. Patients with MAPD had a significant rate of decline of FEV1 compared to idiopathic bronchiectasis. MAPD patients had lower BMI and were younger than patients with idiopathic bronchiectasis.
Clinical problems in TB and other respiratory infections
During the poster session about clinical problems in TB and other respiratory infections, the presenters discussed the impact that pulmonary contagious diseases still have on society, ranging from TB to SARS-CoV-2 pneumonia.
Igor Ivanes (Chisinau, Republic of Moldova) explored different characteristics of TB in Moldova, including reduction in the diagnosis of TB in children under the conditions of the COVID-19 pandemic, to the impact of the disease on the evolution of pregnancy, delivery and perinatal outcomes. Despite the efforts made to improve the management of TB in Algeria, there are still fatal forms of TB. Fettal Nadia (Sidi Bel Abbes, Algeria) showed the data of a retrospective cohort with a mortality rate of 4%. Sofia El Hanafy (Casablanca, Morocco) presented a case series of 38 patients with pseudotumour TB characterised by clinical, radiological and endoscopic features which can mimic a bronchogenic carcinoma. Selsabil Daboussi (Tunis, Tunisia) showed how TB relapses are a public health problem in Tunisia, with a high risk of developing MDR-TB.
In a multicentre retrospective study at four South Korean hospitals, Hyonsoo Joo (Seoul, Republic of Korea) studied the correlation between COPD development and TB infection. Similar to results found by Stolz et al. [69], suggesting that pulmonary infections are a cause of COPD, in this study the authors found that 13.6% of the patients developed COPD with a strong correlation with the severity of TB sequelae.
“Tripledemic” was a word coined by Usman Kahara (Birmingham, UK) to describe the inpatient burden of winter respiratory viral illness in a district general respiratory unit in 2022: influenza, RSV and COVID-19. The study showed that, surprisingly, having two concurrent viruses during the COVID-19 pandemic did not worsen patient outcomes.
Houda Rouis (Ariana, Tunisia) explored the correlation between imaging in non-cystic fibrosis bronchiectasis and prognosis scores, finding that extensive lesions on high-resolution chest radiography are associated with a higher FACED score [70] without significant correlation with BSI (Bronchiectasis Severity Index) score [71].
Finally, the poster session included a number of posters relating to the COVID-19 pandemic. Post-COVID-19 pulmonary complications in the chest clinic of Oran, Algeria, were described by Abdelmajid Snouber (Oran, Algeria). Prognostic information 90 days after diagnosis of COVID-19 was reviewed for 158 patients that underwent invasive mechanical ventilation by Masamichi Mineshita (Kawasaki, Japan), who found that factors such as age, comorbidities, low lymphocyte count and renal impairment were all associated with poor prognosis. From Ukraine, Nataliia Habshydze (Dnipro, Ukraine) studied COVID-19 and endothelial dysfunction, finding that patients with low saturation and high C-reactive protein during the acute phase of the disease had higher endothelin-1 (used as an endothelial dysfunction marker) levels following infection. The effectiveness of efferent therapy based on nanoparticle silica in the treatment of SARS-CoV-2 pneumonia was evaluated by Oksana Viltsaniuk (Vinnytsya, Ukraine) with evidence of a reduced time of hospitalisation, number of complications and mortality. Nathalie De Vos (Brussels, Belgium) proposed a theragnostic approach to guide therapeutic decisions in COVID-19 aiming to diminish sequelae. Data that highlighted the need for pro-active healthcare after a hospital admission to diagnose and manage newly acquired long-term conditions 1 year after SARS-CoV-2 pneumonia were presented by Rachael Evans (Leicester, UK).
Group 10.03: Adult cystic fibrosis
Multiple studies examined the changes in the elexacaftor-tezacaftor-ivacaftor (ETI) era. Shahid Sheikh (Columbus, OH, USA) evaluated CT scan modifications after 1 year of therapy, revealing a decrease in mucous plugging and, to a lesser extent, in hyperinflation [72]. Federica Bellino (Milan, Italy) conducted an analysis to assess the variability in the response to ETI, finding significant heterogeneity in terms of percent predicted FEV1, BMI, sweat chloride concentration and CFQ-R (Cystic Fibrosis Questionnaire – Revised) score changes after 6 months, with a moderate correlation between BMI and percent predicted FEV1. Inbal Golan-Tripto (Beer Sheva, Israel) analysed the sputum of 15 cystic fibrosis patients with previous isolation of NTM, discovering a 60% decrease of NTM isolation after 1 year of ETI [73].
Even in the era of cystic fibrosis transmembrane conductance regulator (CFTR) modulators, P. aeruginosa infection remains one of the main challenges in people with cystic fibrosis [3, 74]. In light of this issue, Urania Rappo (Cambridge, MA, USA) presented a phase 1b/2a trial to evaluate phage therapy with BX004-A for chronic P. aeruginosa pulmonary infection in stable cystic fibrosis patients. The study drug was well-tolerated, with a reduction of P. aeruginosa colony forming units at 15 days and no emerging resistance to BX004-A.
Claire Houston (Belfast, UK) investigated the factors underlying increased pulmonary exacerbations in patients with cystic fibrosis, finding lower levels of innate host defence proteins (antiprotease, antimicrobials and immunomodulatory proteins) in the sputum of frequent exacerbators.
In non-cystic fibrosis bronchiectasis, treatment with brensocatib was found effective in prolonging time to first exacerbation [62]. Ariel Teper (Hastings-on-Hudson, NY, USA) conducted a study on pharmacokinetics and safety of brensocatib in patients with cystic fibrosis, showing results comparable to those described for healthy subjects and bronchiectasis patients, regardless of concomitant therapy with CFTR modulators.
The use of inhaled antibiotics remains pivotal in the therapy of cystic fibrosis. Nicholas Simmonds (London, UK) reported interim findings from a post-marketing safety study in cystic fibrosis treated with levofloxacin inhalation solution (LIS) in Germany and in the UK, whose primary aim was to evaluate the occurrence of haemoptysis, hepatotoxicity and tendon rupture. The analysis revealed no differences in liver disease between the LIS and the non-LIS cohort. The incidence of tendon rupture was very low. In the UK registry, haemoptysis was minimal in the LIS cohort, with higher but non-significant rates in Germany, consistent with phase 3 trial reports [75].
Astrid Vermaut (Oud-Heverlee, Belgium) presented a study on the cellular immune landscape in end-stage cystic fibrosis lungs, showing that the end-stage cystic fibrosis inflammatory profile involves the adaptive immune system (mostly B-cells and CD8+ T-cells), with a heterogeneity among different end-stage cystic fibrosis lungs.
Moving on to the new challenges and opportunities for cystic fibrosis patients, Paola Iacotucci (Naples, Italy) showed how the use of e-health technologies could reduce costs. Finally, Almudena Felipe Montiel (Rubí, Spain) reported that, as age increases, patients with cystic fibrosis develop comorbidities that need to be assessed, such as psychiatric, haematological, renal, rheumatic, cardiac and immunological disorders, but also malignancies, neurological and thyroid issues.
Conclusion
As one of the largest ERS assemblies, Assembly 10 encompasses a broad range of clinical and scientific topics in areas including bronchiectasis, NTM, cystic fibrosis, COVID-19 and TB. Here, we have presented a selection of presentations from numerous high-quality respiratory infection sessions at the 2023 ERS Congress. We hope this offers the reader the chance to be informed of some of the latest developments from Assembly 10 and encourage future participation in the ERS Congress.
Footnotes
Provenance: Commissioned article, peer reviewed.
Conflict of interest: F. Bindo reports no conflicts of interest.
Conflict of interest: G. Fumagalli reports no conflicts of interest.
Conflict of interest: K. Myroniuk-Konstantynovych reports no conflicts of interest.
Conflict of interest: E. Papadopoulou reports no conflicts of interest.
Conflict of interest: D. Paróczai reports no conflicts of interest.
Conflict of interest: L. Perea reports no conflicts of interest.
Conflict of interest: J. Pollock reports travel grants for conference attendance from Asthma+Lung UK, the American Thoracic Society, the European Respiratory Society and the British Association for Lung Research.
Conflict of interest: O. Popovych reports no conflicts of interest.
Conflict of interest: C. Premuda reports a European Respiratory Society Abstract Grant in Cystic Fibrosis.
Conflict of interest: M.B. Long reports travel grants for conference attendance from Asthma+Lung UK, the British Thoracic Society and the American Thoracic Society.
Conflict of interest: H.R. Keir reports honoraria received for lectures from Insmed Inc. and travel grants from Asthma+Lung UK for conference attendance.
References
Articles from ERJ Open Research are provided here courtesy of European Respiratory Society
Citations & impact
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/163381882
Article citations
ERS International Congress 2023: highlights from the Respiratory Clinical Care and Physiology Assembly.
ERJ Open Res, 10(3):178-2024, 20 May 2024
Cited by: 0 articles | PMID: 38770003 | PMCID: PMC11103686
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
ERS International Congress 2022: highlights from the Respiratory Infections Assembly.
ERJ Open Res, 9(3):628-2022, 22 May 2023
Cited by: 2 articles | PMID: 37228292 | PMCID: PMC10204818
ERS International Congress 2021: highlights from the Respiratory Infections Assembly.
ERJ Open Res, 8(2):642-2021, 01 Apr 2022
Cited by: 1 article | PMID: 35615420 | PMCID: PMC9124871
Review Free full text in Europe PMC
ERS International Congress 2020: highlights from the Respiratory Infections assembly.
ERJ Open Res, 7(2):91-2021, 19 Apr 2021
Cited by: 1 article | PMID: 33898612 | PMCID: PMC8053904
ERS International Congress 2023: highlights from the Paediatrics Assembly.
ERJ Open Res, 10(1):853-2023, 01 Jan 2024
Cited by: 1 article | PMID: 38410713 | PMCID: PMC10895434

 10 and
10 and 

