Abstract
Objectives
While older adults showed higher mortality during COVID-19 pandemic, protective behaviours (knowledge regarding coping with COVID-19 symptoms and preventive behaviours) were highlighted to be important to prevent the spread of infection. This study aimed to identify individual and community-level variables influencing deficient knowledge regarding coping with COVID-19 and not-practicing COVID-19 of older adults during the pandemic.Design
This is a secondary analysis of a cross-sectional study using the 2020 Korea Community Health Survey (KCHS).Setting
255 community public health centres nationwide, South Korea.Methods and analysis
Using 2020 KCHS data, multilevel logistic regression analysis was conducted on 55 005 adults aged 65 years or older.Results
Older adults who reside alone, as opposed to with their spouse and who lack the support of another individual exhibited insufficient COVID-19 coping-related knowledge (OR: 1.142, p<0.001) and poor preventive behaviours (OR: 1.177, p<0.001). Furthermore, lower municipal social welfare budget levels were associated with worse health behaviours (OR: 0.062, p<0.001). Specifically, older adults living in rural areas were less likely to engage in COVID-19 preventive behaviours compared with those in urban areas (OR: 1.247, p<0.001). Additionally, the effectiveness of mass media as a motivating factor for adopting preventive measures was only significant in rural populations (OR: 0.944, p<0.05).Conclusions
Both individual-level and community-level approaches are necessary as an initial response during the pandemic. Since elderly people living alone with low socioeconomic status are vulnerable groups with poor health behaviours, it is helpful to provide social support on how to respond to infectious diseases and manage symptoms. In addition, it is important to expand the municipal social welfare budget to promote health equity between regions through appropriate health behaviour education and the strengthening of public medical services.Free full text

Predictors of older adults’ health behaviours to prevent COVID-19 transmission: a multilevel analysis
Associated Data
Abstract
Abstract
Objectives
While older adults showed higher mortality during COVID-19 pandemic, protective behaviours (knowledge regarding coping with COVID-19 symptoms and preventive behaviours) were highlighted to be important to prevent the spread of infection. This study aimed to identify individual and community-level variables influencing deficient knowledge regarding coping with COVID-19 and not-practicing COVID-19 of older adults during the pandemic.
Design
This is a secondary analysis of a cross-sectional study using the 2020 Korea Community Health Survey (KCHS).
Setting
255 community public health centres nationwide, South Korea.
Methods and analysis
Using 2020 KCHS data, multilevel logistic regression analysis was conducted on 55 005 adults aged 65 years or older.
005 adults aged 65 years or older.
Results
Older adults who reside alone, as opposed to with their spouse and who lack the support of another individual exhibited insufficient COVID-19 coping-related knowledge (OR: 1.142, p<0.001) and poor preventive behaviours (OR: 1.177, p<0.001). Furthermore, lower municipal social welfare budget levels were associated with worse health behaviours (OR: 0.062, p<0.001). Specifically, older adults living in rural areas were less likely to engage in COVID-19 preventive behaviours compared with those in urban areas (OR: 1.247, p<0.001). Additionally, the effectiveness of mass media as a motivating factor for adopting preventive measures was only significant in rural populations (OR: 0.944, p<0.05).
Conclusions
Both individual-level and community-level approaches are necessary as an initial response during the pandemic. Since elderly people living alone with low socioeconomic status are vulnerable groups with poor health behaviours, it is helpful to provide social support on how to respond to infectious diseases and manage symptoms. In addition, it is important to expand the municipal social welfare budget to promote health equity between regions through appropriate health behaviour education and the strengthening of public medical services.
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic has been ongoing since March 2020 and shows varied symptoms (eg, mild upper respiratory tract illness, severe viral pneumonia with respiratory failure and even death).1 In South Korea, cumulatively, 26 044 deaths were reported spanning across all ages, while nearly 83.83% of deaths occurred in the population aged over 70 years due to infection of COVID-19. Furthermore, older age has been reported to be strongly associated with higher mortality owing to insufficient immune functions and comorbidities; thus, older adults show higher susceptibility to COVID-19.2 3
044 deaths were reported spanning across all ages, while nearly 83.83% of deaths occurred in the population aged over 70 years due to infection of COVID-19. Furthermore, older age has been reported to be strongly associated with higher mortality owing to insufficient immune functions and comorbidities; thus, older adults show higher susceptibility to COVID-19.2 3
Owing to the limited pharmacological intervention regarding the disease, health-related behaviours, including contact-limiting strategies (eg, social distancing),4 wearing masks5 and hand hygiene,6 were strongly recommended by the WHO and the Korean government to minimise SARS-CoV-2 virus transmission from persons to communities.7 However, the internet and fake news spread by the media increased fear and worry during the rapid virus transmission and disrupted information spread regarding COVID-19 transmission, treatment and control.8 This phenomenon (‘infodemic’) was considered a major pandemic period challenge to overcome. The infodemic was profoundly associated with reduced health literacy (ie, the ability to access healthcare systems, gain knowledge and make decisions) in the USA and Europe.9 10 Knowledgeability and preventive behaviour practice regarding COVID-19 are correlated with comprehensive health literacy; therefore, it is essential for protecting the health of individual persons and communities from infectious disease.11
Older adults have been shown to have poor health literacy due to low levels of education and lack of learning ability, suggesting their vulnerability to potentially high harm during a pandemic crisis. In particular, older adults experienced difficulties in gaining health-related information during this period and were misled to judge and use the available information.12 Health literacy is associated with various predictors, including demographic and social factors (eg, using media and degrees of social support).13 Furthermore, older adults tend to be affected by various social discriminants (eg, race and ethnicity, households and occupation), which can significantly affect health outcomes for those with COVID-19.14 During the pandemic, most older adults experienced social isolation, which, in turn, imposed economic and psychosocial burdens on them.15 A previous review reported that neighbours’ social support and access to regional health services (ie, community factors) are associated with health literacy proficiency among older adults.10 Above studies have suggested that older adults’ health-related behaviours and influencing factors should be interpreted at the community level; however, the factors affecting those behaviours have been examined limitedly, and only individual-level factors have been discussed by a few reviews.14 15 For example, some reviews have discussed the higher levels of individual risk perception during pandemics as an imperative mediating factor for enhancing preventive behaviours.16 Furthermore, multiple demographic factors (eg, female, higher education, being married, larger family size) were regarded as confounding factors for the higher frequency of preventive behaviours in Taiwan.17 Psychological factors (eg, anxiety, mental distress, post-traumatic stress disorder and anger) can also significantly influence acceptance of preventive pandemic-related behaviours.18
A previous review highlighted government pressure regarding compliance with COVID-19 prevention practices, media exposure, information access, personal protective equipment (PPE), healthcare services and social support as influencing health behaviour factors.19 Furthermore, regional factors (eg, living in areas with high poverty and density and low-quality healthcare) were associated with higher community vulnerability to COVID-19-associated deaths in a study in Indonesia.20 This suggests that the factors influencing COVID-19-related health behaviours should be interpreted at the community level and compared across different regions, especially concerning selecting vulnerable groups with poor health behaviours and reducing health inequity among different areas. However, little is known about community-level factors and regional difference factors regarding older adults’ health behaviours in the initial stage of the pandemic.
This study aims to identify vulnerable groups by considering community-level and regional factors, as well as individual-level factors influencing older adults’ poor health behaviours during the initial pandemic period. The study objectives are (1) to verify individual and community factors related to knowledge regarding coping with disease symptoms and preventive behaviours, and (2) to compare different confounding factors by region. This study defines health behaviours as a concept that includes both knowledge and practice of health-protective behaviours. Knowledge is defined as the strategies employed when a person is aware of COVID-19 symptoms. Health-protective behaviour practices are defined as the degree of behaviour performance necessary for preventing COVID-19 spread according to government guidelines.
Methods
Data and subjects
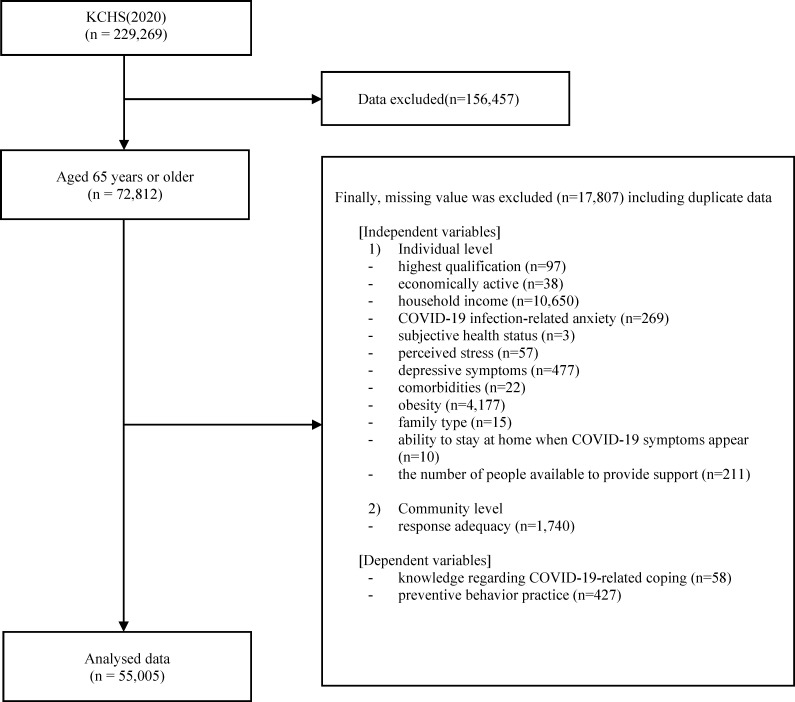
This study used raw data from the 2020 Korea Community Health Survey (KCHS) conducted by the Korea Centers for Disease Control and Prevention Agency (KDCA). The KCHS is an annual survey that collects information on the health status of adults aged 19 years or older living in South Korea. Interviewers surveyed individuals in all 255 community public health centres in the country. The data were collected from August to October 2020 using random sampling and stratified to ensure a representative sample. Each community health centre provided approximately 900 respondents, with a total sample size of 229 269. This study focused on adults aged 65 or older without missing data in the outcome and explanatory variables, resulting in a final sample size of 55
269. This study focused on adults aged 65 or older without missing data in the outcome and explanatory variables, resulting in a final sample size of 55 005 participants (figure 1).
005 participants (figure 1).
Theoretical framework
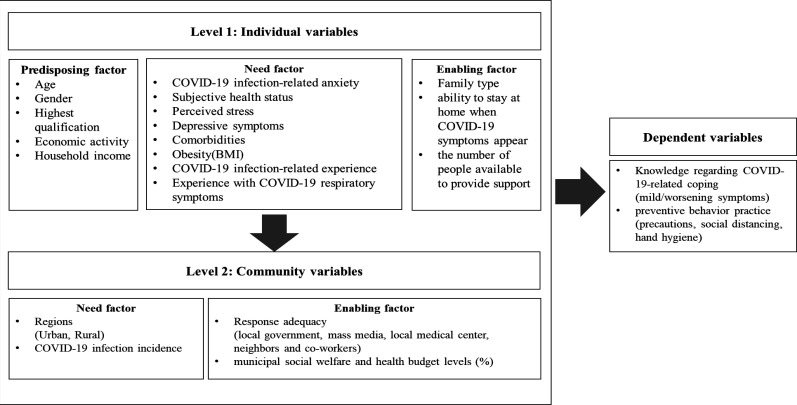
Based on the Andersen21 Health Behaviour Model (HBM), this study aimed to identify the factors affecting health behaviours, including knowledge regarding COVID-19-related preventive behaviour practice in older adults. Andersen’s HBM is useful for explaining health behaviour and finding influencing factors. The model includes predisposing factors that represent a particular characteristic of an individual; need factors that indicate the disability or disease status, which is the most direct factor for health behaviour; and enabling factors that facilitate health behaviour.
This study’s theoretical framework comprised two dependent variables to identify initial responses to infectious diseases in older adults, including (1) knowledge regarding COVID-19-related coping (coping with the onset of infection) and (2) preventive behaviour practice (precautions, social distancing, hand hygiene). Each variable was identified as individual-level or community-level (figure 2).
Variables
Independent variables
Individual-level variables
Age, gender, highest qualification, economic activity and household income were selected as predisposing factors. Sex was divided into male and female, and age was categorised into youngest-old (65–74 years), middle-old (75–84 years) and oldest-old (≥85 years) based on a previous study.22 The highest qualification was classified into four categories (elementary or below, middle, high school and college degree or above), and economic activity was classified as ‘yes (engaged in paid employment)’ or ‘no (not employed)’. Finally, household income was categorised into quartiles using the household equalisation index (monthly income divided by the square root of the number of household members).
The need factors comprised COVID-19 infection-related anxiety (5-point scale, not at all ‘1’ to very much so ‘5’), subjective health status (5-point scale: very bad ‘1’ to very good ‘5’), perceived stress (4-point scale: hardly feel stress ‘1’ to very much ‘4’), depressive symptoms (Patient Health Questionnaire, the sum of 9 items (0–27 points), 4-point scale: not at all ‘0’ to almost every day ‘3’ for each item), comorbidities (hypertension, diabetes), obesity determined by body mass index (obese: 25 kg/m2 or more), COVID-19 infection-related experience and experience with COVID-19 respiratory symptoms.
kg/m2 or more), COVID-19 infection-related experience and experience with COVID-19 respiratory symptoms.
Enabling factors included family type (living with a spouse, living with others except for spouse and living alone), ability to stay at home when COVID-19 symptoms appear and the number of people available to provide support (none, 1–2 and >3).
Community-level variables
As need factors, the regions were classified into urban and rural areas, and COVID-19 infection incidence (per 100 000 persons) from 17 cities and provinces was used.23 In South Korea, all metropolitans have populations over 1 million and contain minor entities known as ‘Dong’, whereas the other cities have populations over 50 000 and contain smaller entities known as ‘Dong’, ‘Eup’ and ‘Myeon’. A ‘Dong’ refers to a unit in an urban area; an ‘Eup’ is a unit for a population of over 20 000; and a ‘Myeon’ is the smallest among these three units. Therefore, we defined urban areas as ‘Dongs’ (including metropolitan areas) and ‘Eup’ and ‘Myeon’ as rural areas. COVID-19 infection incidence was dichotomously defined as above average (high) and below average (low) for 17 cities and provinces.
000 persons) from 17 cities and provinces was used.23 In South Korea, all metropolitans have populations over 1 million and contain minor entities known as ‘Dong’, whereas the other cities have populations over 50 000 and contain smaller entities known as ‘Dong’, ‘Eup’ and ‘Myeon’. A ‘Dong’ refers to a unit in an urban area; an ‘Eup’ is a unit for a population of over 20 000; and a ‘Myeon’ is the smallest among these three units. Therefore, we defined urban areas as ‘Dongs’ (including metropolitan areas) and ‘Eup’ and ‘Myeon’ as rural areas. COVID-19 infection incidence was dichotomously defined as above average (high) and below average (low) for 17 cities and provinces.
The enabling factors include response adequacy (local government-Si (City)/Gun(county)/Gu(borough), mass media, local medical centre and neighbours/coworkers. Furthermore, the municipal social welfare and health budget levels (%) of the Korean Statistical Information Service were used.24 Response adequacy (5-point scale: not at all appropriate ‘1’ to very appropriate ‘5’) was a continuous variable, and municipal social welfare and health budget levels (%) were dichotomously defined as above average (high) and below average (low) for 17 cities and provinces.
Dependent variables
Dependent variables were selected: (1) knowledge regarding COVID-19-related coping and (2) preventive behaviour practice (precautions, social distancing, hand hygiene). Factors influencing health behaviours for preventing infectious diseases were verified by exploring the predictors of these two dependent variables.
First, regarding knowledge about COVID-19-related coping, questionnaires assessed coping involving mild (fever, cough and fatigue without signs of severe pneumonia) or aggravated symptoms (severe respiratory distress, chest pain and confusion, indicating potential severe illness requiring immediate medical attention). According to the KDCA (2020) guidelines,25 in response to mild symptoms, ‘contacting the call center of the KDCA and public health center that provides disease information’, ‘immediately visiting a hospital or public health center’, ‘immediately visiting a screening clinic’ and ‘isolation at home for three to four days and observing symptoms’ have been defined as the correct responses, but ‘maintaining daily life by taking cold medicine’ and ‘lacking knowledge’ have been defined as poor coping. In response to aggravated symptoms, ‘isolation at home for three to four
days and observing symptoms’ have been defined as the correct responses, but ‘maintaining daily life by taking cold medicine’ and ‘lacking knowledge’ have been defined as poor coping. In response to aggravated symptoms, ‘isolation at home for three to four days and observing symptoms’, ‘maintaining daily life by taking cold medicine’ and ‘lack of knowledge’ were defined as deficient coping. Those who knew the correct coping methods for both mild and aggravated symptoms were classified into the ‘practice-health behavior group (0)’, and those who were unsatisfied with even one item were classified into the ‘deficient knowledge regarding coping with symptoms (1)’.
days and observing symptoms’, ‘maintaining daily life by taking cold medicine’ and ‘lack of knowledge’ were defined as deficient coping. Those who knew the correct coping methods for both mild and aggravated symptoms were classified into the ‘practice-health behavior group (0)’, and those who were unsatisfied with even one item were classified into the ‘deficient knowledge regarding coping with symptoms (1)’.
Second, preventive behaviour practice was evaluated by combining three components: precautions, social distancing and hand hygiene. The three components included: precautions (six items: rest when sick, cover respiratory tract when coughing, periodic ventilation/disinfection, wearing a mask in indoor facilities, wearing a mask when it is difficult to keep a distance of 2 m outdoors), social distance (four items: keeping a 2
m outdoors), social distance (four items: keeping a 2 m distance, refraining from visiting hospital/going out and meeting others, contacting close people without face-to-face contact) and hand hygiene (five items: before eating, after going to the bathroom, after returning from an outing, washing hands under running water for 30
m distance, refraining from visiting hospital/going out and meeting others, contacting close people without face-to-face contact) and hand hygiene (five items: before eating, after going to the bathroom, after returning from an outing, washing hands under running water for 30 s using soap and hand sanitiser). Those who satisfied all three components were classified into the ‘practice-health behavior group (0)’, and those who were unsatisfied with even one item were classified into the ‘not-practicing preventive behaviors on COVID-19 infection (1)’.
s using soap and hand sanitiser). Those who satisfied all three components were classified into the ‘practice-health behavior group (0)’, and those who were unsatisfied with even one item were classified into the ‘not-practicing preventive behaviors on COVID-19 infection (1)’.
Patient and public involvement
Because this is a secondary data analysis study, previously collected data was used. Thus, there are no related patients.
Statistical analysis
A three-step modelling approach, using a multilevel logistic regression, was conducted to analyse individual-level and community-level factors affecting dependent variables. The Model 0 (ie, the null model) had no variables; Model 1 included only individual variables; Model 2 included community variables and all individual variables. Subsequently, we analysed the outcomes separately by region (urban and rural) to identify the difference. Intraclass correlation (ICC) was used to measure the effect of variables at individual and community levels. Parameter estimation results were reported using ORs and CIs. The study compared the fitting performances of each model using Akaike’s information criterion (AIC) and −2log-likelihood (−2LL). The lower the AIC or the lower the −2LL, the higher the model performance.
All statistical analyses were performed using the R software (V.4.2.1).
Results
Demographic and general characteristics
The demographic, individual and community characteristics of the 55 005 participants are summarised in table 1. Of the participants, 53.7% were youngest-old, 38.6% were middle-old and 7.7% were oldest-old; 57.6% were women; and the highest proportion of educational level was elementary school or below (58.7%). Most participants were economically inactive (64.1 %) and suffered from diabetes or hypertension (61.3%) but were not obese (72.2%). However, experience with COVID-19 and its symptoms was low (99.8% and 99%), suggesting that the collected data reflected the response pattern of older adults to COVID-19 during the first nationwide transmission.26 A total of 244 administrative areas were included in this study; the percentage of urban and rural areas was 45% and 55%, respectively.
005 participants are summarised in table 1. Of the participants, 53.7% were youngest-old, 38.6% were middle-old and 7.7% were oldest-old; 57.6% were women; and the highest proportion of educational level was elementary school or below (58.7%). Most participants were economically inactive (64.1 %) and suffered from diabetes or hypertension (61.3%) but were not obese (72.2%). However, experience with COVID-19 and its symptoms was low (99.8% and 99%), suggesting that the collected data reflected the response pattern of older adults to COVID-19 during the first nationwide transmission.26 A total of 244 administrative areas were included in this study; the percentage of urban and rural areas was 45% and 55%, respectively.
Table 1
 005)
005)| Variables | Subgroups | N (%) or mean±SD |
| Individual level | ||
| Age group | Youngest-old (65~74 years) | 29 535 (53.7) 535 (53.7) |
| Middle-old (75~84 years) | 21 249 (38.6) 249 (38.6) | |
| Oldest-old (≥85 years) | 4221 (7.7) | |
| Gender | Male | 23 308 (42.4) 308 (42.4) |
| Female | 31 697 (57.6) 697 (57.6) | |
| Highest qualification | Elementary school or below | 32 313 (58.7) 313 (58.7) |
| Middle school | 9211 (16.7) | |
| High school | 9028 (16.4) | |
| Degree or above | 4453 (8.1) | |
| Economic activity | Yes | 19 772 (35.9) 772 (35.9) |
| No | 35 233 (64.1) 233 (64.1) | |
| Household income (quartile (Q)) | Q1 (lowest) | 13 839 (25.2) 839 (25.2) |
| Q2 | 14 410 (26.2) 410 (26.2) | |
| Q3 | 13 271 (24.1) 271 (24.1) | |
| Q4 (highest) | 13 485 (24.5) 485 (24.5) | |
| COVID-19 infection-related anxiety | 4.1±0.8 | |
| Subjective health status | 3.0±0.9 | |
| Perceived stress | 1.7±0.7 | |
| Depressive symptoms (PHQ-9) | 2.2±3.2 | |
| Comorbidities (diabetes or hypertension) | Yes | 33 723 (61.3) 723 (61.3) |
| No | 21 282 (38.7) 282 (38.7) | |
| Obesity | Yes | 15 302 (27.8) 302 (27.8) |
| No | 39 703 (72.2) 703 (72.2) | |
| COVID-19 infection-related experience | Yes | 117 (0.2) |
| No | 54 888 (99.8) 888 (99.8) | |
| Experience with COVID-19 respiratory symptoms | Yes | 536 (1.0) |
| No | 54 469 (99.0) 469 (99.0) | |
| Family type | Living with a spouse | 33 880 (61.6) 880 (61.6) |
| Living with others except for spouse | 6245 (11.4) | |
| Living alone | 14 880 (27.1) 880 (27.1) | |
| Ability to stay at home when COVID-19 symptoms appear | Able | 799 (1.5) |
| Unable | 54 206 (98.5) 206 (98.5) | |
| The number of people available to provide support | None | 13 384 (24.3) 384 (24.3) |
| One to two | 25 005 (45.5) 005 (45.5) | |
| Three and above | 16 616 (30.2) 616 (30.2) | |
| Community level | ||
| Regions | Urban | 24 735 (45.0) 735 (45.0) |
| Rural | 30 270 (55.0) 270 (55.0) | |
| Response adequacy (local government) | 4.03±0.91 | |
| Response adequacy (mass media) | 4.09±0.79 | |
| Response adequacy (local medical centre) | 3.96±0.83 | |
| Response adequacy (neighbours and coworkers) | 4.01±0.74 | |
COVID-19 infection incidence (per 100 000 persons) 000 persons) | Low (below average) | 42 949 (78.1) 949 (78.1) |
| High (above average) | 12 056 (21.9) 056 (21.9) | |
| Municipal social welfare and health budget levels | Low (below average) | 33 614 (61.1) 614 (61.1) |
| High (above average) | 21 391 (38.9) 391 (38.9) | |
PHQPatient Health Questionnaire
Individual and community factors influencing deficient knowledge regarding coping with COVID-19 symptoms
To analyse differences in factors among communities, we performed multilevel analysis at three different levels (Models 0, 1 and 2). As a result, Model 2 was also the most explanatory (ICC: 0.064) and fitted model (AIC: 31 795.6) for deficient knowledge regarding coping with COVID-19 symptoms, compared with Model 0 (ICC: 0.067, AIC: 32 222.5).
Among the predisposing factors, the oldest adults (OR 1.321, p<0.001) had poor knowledge, whereas those with a higher educational level (OR 0.770, p<0.001) and higher household income (OR 0.805, p<0.001) had relatively sufficient knowledge. Regarding need factors, older adults with lower anxiety related to COVID-19 (OR=0.855, p<0.001), higher depressive symptoms (OR=1.04, p<0.001) and no experience with respiratory symptoms during COVID-19 (OR=0.574, p<0.001), rather than having experience with them, predicted lower levels of knowledge regarding coping with COVID-19 symptoms. Regarding enabling factors, living with a spouse (OR 1.140, p=0.001), compared with living alone, was correlated with a higher level of knowledge and having at least one supportive person positively affected knowledge level (OR 0.902, p=0.016).
At the community level, the responsiveness of local medical centres (OR 0.884, p<0.001) predicted a lower knowledge level (table 2).
Table 2
| Variables | Deficient knowledge regarding coping with symptoms | Not-practicing preventive behaviours on COVID-19 infection | ||||
| Model 0 | Model 1 OR (95% CI) CI) | Model 2 OR (95% CI) CI) | Model 0 | Model 1 OR (95% CI) CI) | Model 2 OR (95% CI) CI) | |
| Intercept | 0.088*** | 0.432*** | 0.637 | 2.324*** | 11.735*** | 21.309*** |
| Individual level | ||||||
| Age group | ||||||
 Youngest-old (65~74 years) Youngest-old (65~74 years) | ||||||
 Middle-old (75~84 years) Middle-old (75~84 years) | 1.123*** (1.049 to 1.203) | 1.134*** (1.059 to 1.214) | 1.246*** (1.191 to 1.303) | 1.253*** (1.198 to 1.311) | ||
 Oldest-old (≥85 years) Oldest-old (≥85 years) | 1.309*** (1.169 to 1.465) | 1.321*** (1.059 to 1.214) | 1.449*** (1.327 to 1.581) | 1.458*** (1.336 to 1.592) | ||
| Gender | ||||||
 Male Male | ||||||
 Female Female | 1.064 (0.992 to 1.142) | 1.070 (0.998 to 1.148) | 0.767*** (0.733 to 0.803) | 0.774*** (0.739 to 0.81) | ||
| Highest qualification | ||||||
| Elementary school or below | ||||||
 Middle school Middle school | 0.875* (0.799 to 0.957) | 0.874* (0.799 to 0.957) | 0.788*** (0.745 to 0.834) | 0.793*** (0.743 to 0.839) | ||
 High school High school | 0.844*** (0.766 to 0.93) | 0.840*** (0.762 to 0.925) | 0.693*** (0.653 to 0.735) | 0.697*** (0.657 to 0.74) | ||
 Degree or above Degree or above | 0.774*** (0.675 to 0.887) | 0.770*** (0.672 to 0.883) | 0.604*** (0.558 to 0.653) | 0.609*** (0.563 to 0.659) | ||
| Economic activity | ||||||
 Yes Yes | ||||||
 No No | 1.033 (0.964 to 1.108) | 1.031 (0.961 to 1.106) | 1.108*** (1.059 to 1.16) | 1.116*** (1.066 to 1.168) | ||
| Household income (quartile (Q)) | ||||||
 Q1 (lowest) Q1 (lowest) | ||||||
 Q2 Q2 | 0.926 (0.853 to 1.006) | 0.928 (0.854 to 1.007) | 1.050 (0.99 to 1.114) | 1.057 (0.996 to 1.122) | ||
 Q3 Q3 | 0.892* (0.814 to 0.976) | 0.891* (0.814 to 0.977) | 0.876*** (0.823 to 0.931) | 0.885*** (0.832 to 0.941) | ||
 Q4 (highest) Q4 (highest) | 0.805*** (0.73 to 0.889) | 0.805*** (0.729 to 0.889) | 0.819*** (0.767 to 0.874) | 0.832*** (0.779 to 0.888) | ||
| COVID-19 infection-related anxiety | 0.841*** (0.809 to 0.874) | 0.855*** (0.822 to 0.889) | 0.770*** (0.749 to 0.792) | 0.785*** (0.763 to 0.807) | ||
| Subjective health status | 0.999 (0.964 to 1.035) | 1.003 (0.968 to 1.039) | 0.876*** (0.855 to 0.898) | 0.882*** (0.861 to 0.903) | ||
| Perceived stress | 0.962 (0.92 to 1.006) | 0.958 (0.916 to 1.002) | 0.910*** (0.883 to 0.938) | 0.908*** (0.881 to 0.936) | ||
| Depressive symptoms (PHQ-9) | 1.040*** (1.03 to 1.051) | 1.040*** (1.03 to 1.05) | 1.046*** (1.038 to 1.055) | 1.046*** (1.038 to 1.054) | ||
| Comorbidities (diabetes or hypertension) | ||||||
 No No | ||||||
 Yes Yes | 1.051 (0.987 to 1.119) | 1.048 (0.984 to 1.116) | 1.007 (0.966 to 1.049) | 1.004 (0.963 to 1.046) | ||
| Obesity | ||||||
 Yes Yes | ||||||
 No No | 0.948 (0.886 to 1.015) | 0.947 (0.885 to 1.013) | 0.996 (0.953 to 1.041) | 0.994 (0.951 to 1.039) | ||
| COVID-19 infection-related experience | ||||||
 Yes Yes | ||||||
 No No | 0.866 (0.462 to 1.625) | 0.861 (0.458 to 1.615) | 1.642* (1.104 to 2.441) | 1.613* (1.083 to 2.404) | ||
| Experience with COVID-19 respiratory symptoms | ||||||
 Yes Yes | ||||||
 No No | 0.572*** (0.452 to 0.724) | 0.574*** (0.453 to 0.727) | 0.870 (0.698 to 1.084) | 0.866 (0.695 to 1.081) | ||
| Family type | ||||||
 Living with a spouse Living with a spouse | ||||||
 Living with others except for spouse Living with others except for spouse | 1.249*** (1.13 to 1.38) | 1.237*** (1.119 to 1.367) | 1.014 (0.947 to 1.085) | 1.008 (0.942 to 1.079) | ||
 Living alone Living alone | 1.142*** (1.061 to 1.23) | 1.140*** (1.058 to 1.227) | 1.179*** (1.12 to 1.24) | 1.177*** (1.118 to 1.238) | ||
| Ability to stay at home when COVID-19 symptoms appear | ||||||
 Able Able | ||||||
 Unable Unable | 0.864 (0.68 to 1.099) | 0.879 (0.691 to 1.118) | 0.946 (0.806 to 1.11) | 0.959 (0.817 to 1.125) | ||
| The number of people available to provide support | ||||||
| None | ||||||
 One to two One to two | 0.885** (0.821 to 0.954) | 0.887** (0.823 to 0.956) | 0.791*** (0.751 to 0.833) | 0.791*** (0.751 to 0.833) | ||
 Three and above Three and above | 0.897* (0.825 to 0.975) | 0.902* (0.83 to 0.981) | 0.740*** (0.699 to 0.783) | 0.743*** (0.702 to 0.787) | ||
| Community level | ||||||
 Regions Regions | ||||||
 Urban Urban | ||||||
 Rural Rural | 1.073 (0.956 to 1.205) | 1.247*** (1.141 to 1.363) | ||||
| Response adequacy (local government) | 0.967 (0.916 to 1.021) | 1.019 (0.983 to 1.057) | ||||
| Response adequacy (mass media) | 1.033 (0.981 to 1.088) | 0.989 (0.956 to 1.023) | ||||
| Response adequacy (local medical centre) | 0.884*** (0.832 to 0.939) | 0.966 (0.928 to 1.006) | ||||
| Response adequacy (neighbours and coworkers) | 0.994 (0.994 to 1.046) | 0.896***(0.866 to 0.928) | ||||
COVID-19 infection incidence (per 100 000 persons) 000 persons) | ||||||
 Low (below average) Low (below average) | ||||||
 High (above average) High (above average) | 0.956 (0.814 to 1.124) | 0.909 (0.732 to 1.129) | ||||
| Municipal social welfare and health budget levels | ||||||
 Low (below average) Low (below average) | ||||||
 High (above average) High (above average) | 1.070 (0.917 to 1.248) | 0.602***(0.498 to 0.728) | ||||
| Variance | ||||||
 Level-2 intercept (SE) Level-2 intercept (SE) | 0.2349 | 0.2313 | 0.2246 | 0.6540 | 0.6222 | 0.5099 |
 ICC ICC | 0.067 | 0.066 | 0.064 | 0.166 | 0.159 | 0.134 |
| Model fit | ||||||
 −2LL −2LL | 32 218.6 218.6 | 31 770 770 | 31 731.6 731.6 | 62 574 574 | 60 458 458 | 60 311.8 311.8 |
 AIC AIC | 32 222.5 222.5 | 31 819.9 819.9 | 31 795.6 795.6 | 62 578 578 | 60 508 508 | 60 375.8 375.8 |
Note.: *pp<0.05, **p<0.01, *** p<0.001, the p value is calculated from a t-value, which is the estimated coefficient divided by its standard errorSE;.
AICAkaike information criteriaICCintraclass correlation−2LLlog-likelihood valuesPHQPatient Health Questionnaire
Individual and community factors influencing not-practicing preventive behaviours regarding COVID-19 infection
The predictive factors of non-practicing preventive behaviours against COVID-19 infection were also analysed by multilevel analysis. Model 2 was also the most explanatory (ICC: 0.134) and fitted model (AIC: 60 375.8) for predicting poor behaviours compared with Model 1 (ICC: 0.166, AIC: 62 578).
Regarding predisposing factors, older age (OR: 1.458, p<0.001) and economic inactivity (OR: 1.116, p<0.001), rather than economic activity, predicted higher levels of not-practicing preventive behaviours against COVID-19 infection. Moreover, those who were women (OR: 0.774, p<0.001), had a higher educational level (OR:0.609, p<0.001) and higher household income (OR: 0.832, p<0.001) had a lower level of poor behaviours. Among the need factors, higher levels of anxiety related to COVID-19 (OR: 0.785, p<0.001), subjective health status (OR: 0.882, p<0.001) and perceived stress (OR: 0.908, p<0.001) were associated with an increased level of not-practicing preventive behaviours during the COVID-19 pandemic. However, more depressive symptoms (OR: 1.046, p<0.001) and not experiencing COVID-19 (OR: 1.613, p=0.019) predicted higher levels of poor behaviours. Regarding enabling factors, living alone (OR: 1.177, p<0.001), rather than living with a spouse or others and having at least one person available to provide support (OR: 0.791, p<0.001, and OR: 0.743, p<0.001), were significant factors for predicting higher levels of not-practicing preventive behaviours.
At the community level, living in rural areas (OR: 1.247, p<0.001), rather than urban areas, predicted poor behaviours during COVID-19, whereas the responsiveness of neighbours and coworkers (OR: 0.896, p<0.001) and higher municipal social welfare and health budget levels (OR: 0.602, p<0.001) reflected increased poor behaviours (table 2).
Differences in influencing factors between living in urban and rural areas regarding not-practicing preventive behaviours regarding COVID-19 infection
To further explore differences in factors that influenced the non-practicing preventive behaviours of older adults living in rural and urban areas, respectively, we divided older adults into two groups (living in rural areas vs living in urban areas) and performed subgroup analysis. Older age (urban, OR=1.360 vs rural, OR=1.544), higher level of depressive symptoms (urban, OR=1.041
vs rural, OR=1.544), higher level of depressive symptoms (urban, OR=1.041 vs rural, OR=1.053) and living alone (urban, OR=1.154
vs rural, OR=1.053) and living alone (urban, OR=1.154 vs rural, OR=1.201) were related to a higher tendency of not practicing preventive behaviours commonly in older adults living in urban and rural areas, respectively. Female sex (urban, OR=0.748
vs rural, OR=1.201) were related to a higher tendency of not practicing preventive behaviours commonly in older adults living in urban and rural areas, respectively. Female sex (urban, OR=0.748 vs rural, OR=0.781), higher level of educational status (urban, OR=0.659
vs rural, OR=0.781), higher level of educational status (urban, OR=0.659 vs rural, OR=0.547), higher household income (urban, OR=0.858
vs rural, OR=0.547), higher household income (urban, OR=0.858 vs rural, OR=0.821) and higher level of anxiety related to infection (urban, OR=0.755
vs rural, OR=0.821) and higher level of anxiety related to infection (urban, OR=0.755 vs rural, OR=0.813), higher subjective health status (urban, OR=0.866
vs rural, OR=0.813), higher subjective health status (urban, OR=0.866 vs rural, OR=0.898), higher perceived stress (urban, OR=0.912
vs rural, OR=0.898), higher perceived stress (urban, OR=0.912 vs rural, OR=0.902), higher number of supportive people (urban, OR=0.853
vs rural, OR=0.902), higher number of supportive people (urban, OR=0.853 vs rural, OR=0.639), proper responsiveness of neighbours and coworkers (urban, OR=0.905
vs rural, OR=0.639), proper responsiveness of neighbours and coworkers (urban, OR=0.905 vs rural, OR=0.888) and higher social welfare and health budget levels (urban, OR=0.607
vs rural, OR=0.888) and higher social welfare and health budget levels (urban, OR=0.607 vs rural, OR=0.657) were associated with practicing preventive behaviours in rural and urban areas. However, non-economic activity, compared with economic activity, was positively associated with not-practicing protective behaviours only in rural areas (OR=1.258, p<0.001), whereas no experience with COVID-19 infection rather than having experience with it had a positive correlation with not-practicing preventive behaviours only in urban areas (OR=1.939, p<0.001).
vs rural, OR=0.657) were associated with practicing preventive behaviours in rural and urban areas. However, non-economic activity, compared with economic activity, was positively associated with not-practicing protective behaviours only in rural areas (OR=1.258, p<0.001), whereas no experience with COVID-19 infection rather than having experience with it had a positive correlation with not-practicing preventive behaviours only in urban areas (OR=1.939, p<0.001).
At the community level, an increased tendency toward ‘not-practicing health-protective behaviors’ was examined based on local government responsiveness (OR=1.093, p<0.001), whereas a decreased tendency in this regard was observed based on mass media responsiveness (OR=0.944, p=0.028) only in older rural adults. However, neighbour and coworker responsiveness (urban, OR=0.905 vs rural, OR=0.888) and higher municipal social welfare and health budget (urban, OR=0.607
vs rural, OR=0.888) and higher municipal social welfare and health budget (urban, OR=0.607 vs rural, OR=0.657) diminished poor behaviours in both rural and urban residents (table 3).
vs rural, OR=0.657) diminished poor behaviours in both rural and urban residents (table 3).
Table 3
| Not-practicing preventive behaviours on COVID-19 infection | ||
| Variables | Urban (N=24 735) 735) | Rural (N=30 270) 270) |
| Intercept | 31.334*** | 16.351*** |
| Individual level | ||
| Age group | ||
 Youngest-old (65~74 years) Youngest-old (65~74 years) | ||
 Middle-old (75~84 years) Middle-old (75~84 years) | 1.146*** (1.075–1.221) | 1.350*** (1.266–1.44) |
 Oldest-old (≥85 years) Oldest-old (≥85 years) | 1.360*** (1.193–1.55) | 1.544*** (1.371–1.74) |
| Gender | ||
 Male Male | ||
 Female Female | 0.748*** (0.701–0.797) | 0.781*** (0.732–0.834) |
| Highest qualification | ||
 Elementary school or below Elementary school or below | ||
 Middle school Middle school | 0.847*** (0.783–0.915) | 0.756*** (0.696–0.821) |
 High school High school | 0.788*** (0.729–0.851) | 0.600*** (0.548–0.657) |
 Degree or above Degree or above | 0.659*** (0.596–0.728) | 0.547*** (0.481–0.623) |
| Economic activity | ||
 Yes Yes | ||
 No No | 1.258*** (1.175–1.347) | 1.023 (0.961–1.088) |
| Household income (quartile(Q)) | ||
 Q1 (lowest) Q1 (lowest) | ||
 Q2 Q2 | 1.076 (0.979–1.182) | 1.056 (0.978–1.141) |
 Q3 Q3 | 0.900* (0.821–0.988) | 0.898* (0.825–0.978) |
 Q4 (highest) Q4 (highest) | 0.858** (0.781–0.943) | 0.821*** (0.748–0.901) |
| COVID-19 infection-related anxiety | 0.755*** (0.726–0.785) | 0.813*** (0.781–0.846) |
| Subjective health status | 0.866*** (0.836–0.897) | 0.898*** (0.868–0.929) |
| Perceived stress | 0.912*** (0.874–0.952) | 0.902*** (0.864–0.942) |
| Depressive symptoms (PHQ-9) | 1.041*** (1.03–1.053) | 1.053*** (1.04–1.066) |
| Comorbidities (diabetes or hypertension) | ||
 No No | ||
 Yes Yes | 1.012 (0.955–1.073) | 0.994 (0.937–1.054) |
| Obesity | ||
 Yes Yes | ||
 No No | 0.952 (0.895–1.013) | 1.029 (0.965–1.097) |
| COVID-19 infection-related experience | ||
 Yes Yes | ||
 No No | 1.358 (0.8–2.305) | 1.939*(1.054–3.565) |
| Experience with COVID-19 respiratory symptoms | ||
 Yes Yes | ||
 No No | 0.938 (0.682–1.29) | 0.815 (0.598–1.111) |
| Family type | ||
 Living with a spouse Living with a spouse | ||
 Living with others except for spouse Living with others except for spouse | 1.074 (0.982–1.175) | 0.963 (0.867–1.068) |
 Living alone Living alone | 1.154***(1.072–1.243) | 1.201***(1.12–1.289) |
| Ability to stay at home when COVID-19 symptoms appear | ||
 Able Able | ||
 Unable Unable | 0.817 (0.661–1.01) | 1.154 (0.903–1.474) |
| The number of people available to provide support | ||
 None None | ||
 One to two One to two | 0.869*** (0.81–0.932) | 0.704*** (0.651–0.76) |
 Three and above Three and above | 0.853*** (0.788–0.924) | 0.639*** (0.588–0.694) |
| Community level | ||
| Response adequacy (local government) | 0.963 (0.918–1.011) | 1.093** (1.035–1.155) |
| Response adequacy (mass media) | 1.028 (0.983–1.076) | 0.944* (0.898–0.994) |
| Response adequacy (local medical centre) | 0.954 (0.904–1.008) | 0.973 (0.916–1.034) |
| Response adequacy (neighbours and coworkers) | 0.905*** (0.862–0.95) | 0.888*** (0.837–0.925) |
COVID-19 infection incidence (per 100 000 persons) 000 persons) | ||
 Low (below average) Low (below average) | ||
 High (above average) High (above average) | 0.870 (0.683–0.109) | 1.374 (0.964–1.958) |
| Municipal social welfare and health budget levels | ||
 Low (below average) Low (below average) | ||
 High (above average) High (above average) | 0.607*** (0.484–0.762) | 0.657* (0.452–0.953) |
Note.: *pp<0.05, **p<0.01, *** p<0.001, the p value is calculated from a t-value, which is the estimated coefficient divided by its standard errorSE.
PHQPatient Health Questionnaire
Discussion
This study identified the individual and community factors significantly associated with knowledge regarding COVID-19-related coping and preventive behaviour practice among those aged 65 years or older. In the pandemic’s early stages (eg, SARS-CoV-2 pandemic in March 2020 when there was no vaccine), non-pharmaceutical interventions, including knowledge about coping and preventive behaviour practices, were very effective for preventing disease spread.27 Interestingly, the incidence rates of poor health behaviours regarding knowledge and practice were 8.8% and 68.9%, respectively. This suggests that older adults had relatively high rates of poor preventive behaviour practices during the initial COVID-19 period, thus requiring more interventions for improving their preventive behaviours.
Poor health behaviour-related individual variables regarding knowledge and practice were as follows. Regarding predisposing factors, age and education/income level were positively and negatively associated with poor health behaviours, respectively. People with higher incomes and education were more likely to comply with infectious disease prevention behaviours (eg, social distancing and wearing masks).28 29 Low-income people working to earn a living may find it difficult to work from home; this may interfere with self-protection behaviours.29 Therefore, it is desirable to conduct education to improve this vulnerable population’s preventive behaviours during the initial pandemic response phase. Furthermore, older adults and socioeconomically vulnerable groups are less likely to practice preventive behaviours (eg, self-isolation).30 Regarding the necessary factors for health behaviours in this study, low COVID-19-related anxiety was associated with poor health behaviours. Similarly, a previous study has shown that higher COVID-19-related fear induced stricter hygiene practices.27 Thus, infectious disease-related concern and awareness can positively affect individuals’ knowledge and practice of preventive behaviour. However, older adults often feared going out, lacked preventive behaviour-related knowledge and had concerns about infecting family members.31 Therefore, it is crucial to alleviate older adults’ concerns by helping them understand and practice daily health behaviours by providing education at local medical centres on symptom-related coping and preventive behaviours.
Regarding the enabling factors of health behaviours, poor health behaviours were related to living alone and a lack of helpful social support systems. A previous study has shown that older married or cohabitating people pay more attention to their health, acquire health knowledge and show more positive preventive beliefs and practice behaviours because they receive support from spouses or partners.32 Therefore, local governments must provide practical help to older adults living alone, who face difficulties in receiving help from others, by guiding them in coping with infectious disease symptoms, linking them to medical centres for symptom management and supporting accessible health resources. Furthermore, without a social support system, isolation can deepen. Psychological support can reduce isolation and maintain regular sleep and meal times, cognitive stimulation and physical activity to promote community health.33 However, many helpers can increase social contact opportunities, leading to increased exposure to infectious agents.34 35 An alternative to this is the development of telemedicine and remote nursing interventions through information and communication technology for those living alone during pandemics.
This study found that the factors associated only with COVID-19 coping-related knowledge were experience with respiratory symptoms during COVID-19 (individual variables) and adequacy of local medical centre response (community variables). During the COVID-19 pandemic, groups with respiratory symptoms were often strongly associated with poor behaviour. If people with symptoms do not respond appropriately, they can become sources of infection for spreading the virus. Therefore, the government should promote the call centre contact information of the Centers for Disease Control and Prevention, thus allowing people to request early symptom help and conduct regular education for transmission prevention and symptom management. Community variables indicated that the understanding of infection-related coping was low when local medical centres did not respond appropriately. If there is a new infectious disease outbreak, regional public health centres and local medical centres must operate screening clinics, provide prompt responses to emergencies and conduct infectious disease prevention and management training. Regional medical centres must fulfil their role as infection control training institutions by providing guidelines on pre-pandemic countermeasures and regular training opportunities.36
In this study, the individual factors associated only with preventive behaviour practice were sex, economic activity, subjective health status, COVID-19 infection-related experience and perceived stress. This study found that male participants practiced preventive behaviours inappropriately. Female participants showed greater sensitivity to risk situations and more recommended infectious disease prevention behaviours; therefore, the seriousness of infectious diseases and quarantine rules must be emphasised to men.37 Furthermore, a worse subjective health status indicates poorer preventive behaviour practice. However, good individual subjective health status indicated higher preventive behaviour compliance.37 Older adults with low mental and physical functions had fewer infectious disease information resources and fewer coping behaviours for health maintenance under social restrictions.38 Therefore, operating a health programme that balances physical activity and encourages preventive behaviours among older adults with perceived poor health may be effective. COVID-19 infection-related experience was highly related to preventive behaviour practice. This may increase perceived severity, resulting in greater attention.37 However, it is necessary to emphasise the perceived severity of infectious diseases from the point before the infection and induce preventive actions to prepare for dealing with these diseases. Furthermore, a previous study has shown that, under psychological distress conditions, infectious disease exposure risk was high because of preventive behaviour non-compliance.33 This study found that higher depressive symptoms were associated with poorer preventive behaviour practice, but stress promoted preventive behaviour. Thus, those with a high perceived severity regarding infection and who follow precautionary measures can be relatively stressed. During the pandemic, people were isolated and experienced moderate stress levels because of lockdowns; about 10% of these individuals may have languished because of poor mental health; therefore, timely psychological public health interventions are necessary for preventing stress escalation into depressive symptoms.39
To enhance preventive behaviour practice, we must consider community factors along with person-centred approaches. The community-level variables related to preventive behaviour practice were region, neighbour/coworker response adequacy and municipal social welfare and health budget. In this study, rural residents had poorer preventive behaviour practices than urban residents. The infection may spread in the early pandemic stages from densely populated metropolitan areas to neighbouring areas.40 Although infection control measures should be followed strictly in cities with high infection risk, recommendations for preventive behaviour practice should also be strengthened in rural areas. Infection-related awareness within one’s social surroundings, such as local communities, can affect one’s risk perception and engagement in preventive behaviours.41 Social media activation can replace neighbour and colleague roles for those lacking human resources to achieve positive preventive behaviour changes while also remotely sharing accurate infectious disease-related information.42 Furthermore, ‘municipal social welfare and health budget’ was most associated with preventative behaviour practice in this study. The pandemic is a public health issue; therefore, several supplementary budgets for providing social assistance (eg, stabilising people’s livelihoods and providing emergency disaster subsidies) have been approved in Korea.43 Regional social welfare budgets must be expanded, and public healthcare investment for infectious disease prevention and control, health promotion and education must be strengthened.
Regarding preventive behaviour practice, the ratio of poor behaviours was higher in rural areas and the influencing factors differed by region. Older rural adults were associated with poor behaviours when they had no COVID-19 infection-related experience, higher local government response adequacy and lower mass media response adequacy. This study found that mass media greatly influenced rural residents, who may find it more difficult to access health information because of structural barriers (eg, lack of professional medical personnel and limited media exposure).44 Furthermore, older rural people did not properly practice preventive behaviours and lacked information on transmission, prevention measures, infection symptoms, treatments and prognosis.45 Urban residents were relatively active in accessing and sharing infectious disease-related knowledge through mobile phones, shared media networks and communities, but rural residents seemed to have a low ability to obtain the latest information; therefore, they require an information channel to update their infection-related knowledge and understanding.45 Paradoxically, while rural residents perceived the local government as responding adequately to the crisis, they had poor behaviours. Although such residents recognised that local governments were coping properly during the pandemic, real-world positive behaviours could not be elicited. Therefore, local governments must provide reliable information and actively publicise preventive measures. Local community-level control measures (eg, minimum contact strategy) indicate increased preventive behaviour practice among older adults.32 Environmental manipulation and policies (eg, social distancing, lockdown and public facility disinfections) are crucial structural factors encouraging individuals to practice preventive behaviours. However, older urban adults showed poorer preventive behaviour practices without economic activity. Because economic activity dynamics can increase infection spread risk, those engaged in economic activities pay greater attention to infection and perform better preventive behaviours.34 Therefore, cities must strengthen their preventive measures and compliance recommendations among economically inactive populations.
Ultimately, older adults in rural areas or those living alone often exhibit poorer knowledge and behaviours regarding COVID-19 prevention. To address this, policymakers should enhance communication strategies through local networks, like community centres and expand the social welfare budget to support education and provide timely responses in medically underserved areas. This can include deploying mobile health units and establishing telehealth services.46 47 Health practitioners should also create customised, audio-visual health education programmes to improve understanding among older adults. Additionally, strengthening preventive measures with regular follow-ups and checks is crucial to ensure the effectiveness of these interventions.
While this study has provided some implications for the association between individual-level and community-level variables and poor health behaviours, this study has some limitations. First, it was difficult to determine the causal relationship between the variables because cross-sectional data were used. Second, regarding secondary data analysis, variable usage was limited and data on poor behaviours were self-reported, which can bias study results if subjects respond based on social desirability. In addition, the results may be biased due to non-randomly occurring missing values, particularly in the proportion of income data missing, necessitating cautious interpretation of findings. Third, the findings have limited generalisability for global application because of the presence of an infectious disease response system and the sociocultural and geographical particularities of South Korea. In the future, longitudinal studies should include various community variables (eg, the status of public medical institutions and screening clinics by region) and observe behavioural changes from the beginning of an infectious disease outbreak to its end. Furthermore, studies must be conducted comparing symptom-related coping and preventive behaviour practices across various countries.
Conclusion
This study identified the individual-level and community-level variables affecting COVID-19 coping-related knowledge and preventive behaviour practice among older adults in South Korea and revealed the disparities of those factors between different regions. This study provides clues for healthcare providers and health policy managers to select vulnerable groups (eg, older adults living alone in rural areas) and promote community-level information transfer effectively. The study findings can be used to formulate pandemic response policies for preventing infection spread and reducing regional disparities. It is necessary to respond to infectious diseases, operate residual treatment centres, supply PPE, develop and distribute vaccines and promote preventive measures by expanding local government’s municipal healthcare and welfare budgets and support for institutions and healthcare personnel. In addition, regular information publicity and education through audiovisual media are needed to increase the compliance rate of preventive behaviour among older adults living in rural areas.
Acknowledgements
This study supported by Korea Disease Control and Prevention Agency and the Korean Academy of Community Health Nursing.
Footnotes
Funding: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (RS-2024-00338005).
Prepub: Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-083890).
Patient consent for publication: Not applicable.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics approval: This study used an open access data set from the Korea Centers for Disease Control and Prevention Agency and did not contain any personal information about the selected patients; the study was approved by the Institutional Review Board (IRB) of D University in Korea and received a review exemption (IRB No. 1044371-202302-HR-001-01).
Data availability statement
Data are available upon reasonable request.
References
Review Process File
Articles from BMJ Open are provided here courtesy of BMJ Publishing Group
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Preventive behaviours and family inequalities during the COVID-19 pandemic: a cross-sectional study in China.
Infect Dis Poverty, 10(1):100, 20 Jul 2021
Cited by: 9 articles | PMID: 34284821 | PMCID: PMC8290209
The Determinants of Adherence to Public Health and Social Measures Against COVID-19 Among the General Population in South Korea: National Survey Study.
JMIR Public Health Surveill, 9:e35784, 17 Jan 2023
Cited by: 3 articles | PMID: 36446132 | PMCID: PMC9848439
Infection preventive behaviors and its association with perceived threat and perceived social factors during the COVID-19 pandemic in South Korea: 2020 community health survey.
BMC Public Health, 22(1):1381, 19 Jul 2022
Cited by: 3 articles | PMID: 35854280 | PMCID: PMC9294775
Substance use during the COVID-19 pandemic: What is really happening?
Psychiatriki, 33(1):17-20, 21 Feb 2022
Cited by: 13 articles | PMID: 35255473
Review
Funding
Funders who supported this work.
Ministry of Science and ICT, South Korea (1)
Grant ID: RS-2024-00338005

 2
2