Abstract
Background
Diabetic ketoacidosis (DKA) is a life-threatening emergency that can result from delayed diagnosis of type 1 diabetes mellitus (T1DM). Three-quarters of Australian children with a new diagnosis of T1DM visit their general practitioner (GP) the week prior to developing DKA, with similar trends observed internationally.Objective
To summarise interventions in general practice to reduce diagnostic delay in paediatric T1DM and to evaluate their effectiveness.Methods
Six databases (Ovid, Web of Science, CINAHL, Evidence-Based Medicine Reviews, Google Scholar and EMBASE) were searched. Any English language, less than 20 years study involving interventions targeting GPs specifically in the prevention of paediatric DKA, was included. Primary outcomes were (a) the number of children presenting to the hospital in DKA following diagnostic delay after a GP visit and (b) DKA rate. The secondary outcome was changes in GPs' behaviour regarding timeliness of referrals. Two reviewers completed title, abstract and full-text review, with conflicts resolved by a third reviewer. ROBINS-I risk of bias was used for appraisal. High heterogeneity among studies rendered meta-analysis unsuitable. Structured tabulation of results was completed for analysis. The date of last search was 2 July 2023.Results
Eight studies were included (three conference abstracts and five peer-reviewed publications.) We identified six intervention types attempting to facilitate timely diagnosis of type 1 diabetes in the general practice setting: direct communication, indirect communication, education sessions, electronic clinical decision support tools, updated referral pathways and provision of glucose and/or ketone monitors. Due to the limited number of peer-reviewed studies identified by this review, we were not able to identify the extent to which these interventions were successful.Conclusion
Paucity of information regarding study methodology and high heterogeneity among study design and outcome measures limited our conclusions regarding acceptability, effectiveness and reach. Future studies should include GPs in their design and consider the sustainability of interventions in the long term.Prospero registration number
CRD42023412504.Free full text

Have interventions aimed at assisting general practitioners in facilitating earlier diagnosis of type 1 diabetes in children been successful in preventing acute complications? A systematic review
Abstract
Abstract
Background
Diabetic ketoacidosis (DKA) is a life-threatening emergency that can result from delayed diagnosis of type 1 diabetes mellitus (T1DM). Three-quarters of Australian children with a new diagnosis of T1DM visit their general practitioner (GP) the week prior to developing DKA, with similar trends observed internationally.
Objective
To summarise interventions in general practice to reduce diagnostic delay in paediatric T1DM and to evaluate their effectiveness.
Methods
Six databases (Ovid, Web of Science, CINAHL, Evidence-Based Medicine Reviews, Google Scholar and EMBASE) were searched. Any English language, less than 20 years study involving interventions targeting GPs specifically in the prevention of paediatric DKA, was included. Primary outcomes were (a) the number of children presenting to the hospital in DKA following diagnostic delay after a GP visit and (b) DKA rate. The secondary outcome was changes in GPs’ behaviour regarding timeliness of referrals. Two reviewers completed title, abstract and full-text review, with conflicts resolved by a third reviewer. ROBINS-I risk of bias was used for appraisal. High heterogeneity among studies rendered meta-analysis unsuitable. Structured tabulation of results was completed for analysis. The date of last search was 2 July 2023.
Results
Eight studies were included (three conference abstracts and five peer-reviewed publications.) We identified six intervention types attempting to facilitate timely diagnosis of type 1 diabetes in the general practice setting: direct communication, indirect communication, education sessions, electronic clinical decision support tools, updated referral pathways and provision of glucose and/or ketone monitors. Due to the limited number of peer-reviewed studies identified by this review, we were not able to identify the extent to which these interventions were successful.
Conclusion
Paucity of information regarding study methodology and high heterogeneity among study design and outcome measures limited our conclusions regarding acceptability, effectiveness and reach. Future studies should include GPs in their design and consider the sustainability of interventions in the long term.
PROSPERO registration number
CRD42023412504.
Introduction
The importance of timely diagnosis of paediatric type 1 diabetes
Timely recognition and treatment of paediatric type 1 diabetes mellitus (T1DM) is crucial in the prevention of diabetic ketoacidosis (DKA). DKA is a life-threatening complication of T1DM that occurs when insulin levels are insufficient, resulting in metabolic deterioration and progressive acidosis without treatment.1 2 Almost half of children with previously undiagnosed T1DM present to hospital with DKA.3 For most children with T1DM, the first and only experience of DKA is at first presentation for specialist care.4 A diagnosis of T1DM can have an overwhelming impact on both the child and their parents.5 6 This can be exacerbated when a child’s diagnosis is coupled with a hospital stay and DKA.7 A single episode of moderate to severe DKA in early childhood has been associated with irreversible cognitive impairment during development and lowered IQ.8 DKA in new-onset T1DM is preventable if recognised early, allowing for commencement of insulin treatment. It is recommended that when a child with suspected new-onset T1DM presents for medical review, immediate point-of-care testing should be completed to confirm suspicion of hyperglycaemia, with same-day referral for consideration of insulin therapy if hyperglycaemia is documented.9,11 Given that paediatric DKA rates are increasing worldwide,12 interventions to streamline and optimise the management of new-onset paediatric T1DM are of vital importance.
Delays impeding timely diagnosis
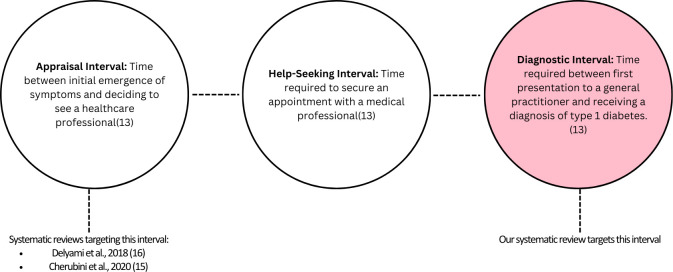
A child’s pathway to a T1DM diagnosis can be described with three distinct intervals (see figure 1), each of which is characterised by unique challenges that can hinder a timely diabetes diagnosis. The first interval, the ‘appraisal interval’, is the time between the onset of initial T1DM-related symptoms and parental recognition that help is required from a medical practitioner.13 Common T1DM-related symptoms include fatigue, polyuria, polydipsia and weight loss.14 The appraisal interval can last anywhere from a few days to up to 6 months, with the median being 17–21 days.13 Interventions to prevent DKA within this phase of the diagnostic pathway typically target the appraisal interval through public health campaigns, with varying levels of success.15 16 These campaigns intend to raise awareness of the symptoms of T1DM and the importance of early diagnosis.
months, with the median being 17–21 days.13 Interventions to prevent DKA within this phase of the diagnostic pathway typically target the appraisal interval through public health campaigns, with varying levels of success.15 16 These campaigns intend to raise awareness of the symptoms of T1DM and the importance of early diagnosis.
The second interval in the pathway to a T1DM diagnosis is the ‘help-seeking’ interval, which is defined as the time needed from realising that there is something wrong with securing a medical appointment.13 There is a paucity of data exploring the extent of this delay, with variation among different healthcare systems.17 In Australia, 54.2% of patients needing urgent care can secure an appointment with a general practitioner (GP) within 24 hours.18
The third interval is referred to as the diagnostic interval, defined as the time between first presentation to the healthcare practitioner to receive a formal diagnosis of T1DM and insulin treatment.13 Best practice guidelines from both primary and secondary care recommend immediate diagnosis and same-day referral.9,11 In Australia, where diagnostic delay exists, the median is 2 days, and in 25% of cases, delay can be more than 5
days, and in 25% of cases, delay can be more than 5 days.14 The two most cited reasons for diagnostic delay include awaiting additional pathology testing for confirmation of T1DM and consideration of alternate diagnoses.14 19 These represent two key opportunities where the diagnostic delay interval can be reduced.
days.14 The two most cited reasons for diagnostic delay include awaiting additional pathology testing for confirmation of T1DM and consideration of alternate diagnoses.14 19 These represent two key opportunities where the diagnostic delay interval can be reduced.
Targeting the diagnostic interval is crucial, as 75%–80% of children presenting with DKA at first diagnosis of diabetes in Australia have visited their GP the week prior.14 20 A systemic approach to the reduction of the diagnostic interval is required to prevent deterioration to DKA and its pervasive, irreversible sequelae. T1DM in children is difficult to diagnose in general practice, as symptoms are non-specific and often attributable to various more common childhood illnesses, or to general childhood growth and development.21 As such, innovations are required that address the non-specific nature of initial T1DM presentations to busy general practice. We were unable to find past systematic reviews that have assessed this area specifically.
The aim of this review is to summarise the current interventions that have targeted diagnostic delay of T1DM in general practice and to evaluate their effectiveness.
Methods
We conducted a systematic review to summarise the interventions applied within general practice to reduce diagnostic delay for T1DM and to evaluate their effectiveness. A protocol for this systematic review was registered with PROSPERO, ID: CRD42023412504, and published.22
Search strategy
Six databases (Ovid (MEDLINE), Web of Science, EMBASE, CINAHL, Evidence-Based Medicine Reviews (EBM Reviews) and Google Scholar) were searched in June and July of 2023 for both publications and grey literature. The final date of the search was 2 July 2023. The search strategies for each database can be found in online supplemental file 1. There was slight variation between each database in order to suit the specific database that was searched.
Grey literature
A grey literature search was conducted to identify any studies that were not in the electronic databases. In particular, conference abstracts from the following proceedings were searched:
Australia New Zealand Society for Paediatric Endocrinology & diabetes.
American Diabetes Association.
European Association for the Study of Diabetes.
International Society for Paediatric and Adolescent Diabetes.
Screening processes
Title, abstract and full-text screening for exclusion and inclusion of publications were completed by two independent reviewers. Where there were inconsistencies in the opinions of the two independent reviewers, a third reviewer was engaged to resolve the difference. This was managed using Covidence.23
Eligibility criteria
The inclusion and exclusion criteria for this study are summarised in table 1.
Table 1
| Inclusion | Exclusion |
| Study characteristics | |
| Non-randomised studies of interventionsFeasibility studiesRandomised controlled trialsControlled population observational trials | |
| Participants | |
| Interventions targeting DKA prevention in children and young people (under 18).(At first diagnosis of type 1 diabetes only) | Adult DKAT2DMRepeat presentations of DKA after a diagnosis was already made |
| Intervention type/setting | |
| Interventions that reduce the diagnostic delay interval in the general practice settings. | Publicity campaigns/awareness campaigns targeted at schools and communities. |
| Report characteristics | |
| Completed within the last 20 years.English languageAny healthcare systemGrey literature | |
DKAdiabetic ketoacidosisT2DMtype 2 diabetes mellitus
Study characteristics
We anticipated that there would be limited data available in this research area and that it is difficult to randomise intervention groups to answer this research question, particularly in the form of randomised controlled trials. As a result, we decided to focus on non-randomised studies of interventions and feasibility studies in this review, as we anticipated that there would not be any randomised controlled trials in this area. We did not place many restrictions based on study type, due to the limited data in this research area.
Participants
We included studies that targeted interventions that improved recognition of T1DM in children and young people. As a result, our patient group was defined as children under 18. In terms of intervention recipients, we only included studies with GPs as recipients of the intervention.
Outcome measures
Our primary outcome of interest was the number of children presenting to hospital with DKA, who experienced diagnostic delay following a visit with their GP. Our secondary outcome of interest was GPs’ behaviours with regard to timely referral for patients with suspected or confirmed type 1 diabetes. Examples of this include the use of point-of-care testing rather than referring for laboratory testing or making same-day referrals rather than delayed referrals. Following a review of the included studies, we identified that reporting on these outcome measures was highly limited and deviated from our research protocol22 to include a third outcome, DKA rate.
Report characteristics
We restricted this investigation to solely include studies completed within the last 20 years and studies that were reported in English.
Data extraction
Two independent reviewers were involved in data extraction. We recorded the following information, in line with our published protocol.22 Data were initially extracted via Covidence and then imported into a Microsoft Word document for verification purposes. The extraction to Microsoft Word was not noted in the protocol paper.
Initials of individual extracting the data and date of data extraction.
An assigned ID number to the publication agreed on by the individuals partaking in the extraction.
Study setting, region and year completed.
The type of study completed in the publication: observational cohort study, case–control study, feasibility study, etc.
Recruitment strategy and whether intervention was only applied to a cluster of general practice clinics.
Intervention type and length.
Definition of control groups/methods of comparison.
Outcome type: DKA presentations, children with reduced diagnostic delay time and GPs’ behaviour.
Statistical analysis methods used.
Key results.
Key conclusions.
Whether any correspondence is required.
Potential conflicts of interest and sources of funding.
Miscellaneous.
Author correspondence
Authors of conference abstracts deemed suitable for inclusion in the review were contacted via email address. One author returned contact via email, providing further information about the number of children in diagnostic delay preintervention and postintervention, contextual information regarding COVID-19’s impact on the interventions, as well as copies of the intervention delivery materials and further information regarding how clinical referral pathways were updated and implemented. The corresponding data that met our data extraction criteria was then extracted along with the data in the abstract.
Data analysis
ROBINS-I assessment
ROBINS-I assessment24 was undertaken by two independent reviewers on five of the eight studies included in the review. We assessed risk of bias (RoB) by assessing seven key bias domains: bias due to confounding, bias in the selection of participants into the study, bias in the classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in measurement of outcomes, bias in the selection of reported results. Two independent reviewers used the ROBINS-I overall RoB judgement table.24 Any disagreement between the two independent reviewers was discussed between the two reviewers and a third reviewer was brought in where necessary. RoB was classified as either low, moderate, serious or critical RoB in each of the seven domains. ‘NI’ was documented where there was insufficient information provided in the studies to make a decision regarding RoB.
Following appraisal via ROBINS-I analysis24 and assessment of heterogeneity among the investigations, it was determined that the studies were not sufficiently similar enough to warrant meta-analysis. Instead, non-statistical synthesis was undertaken to summarise all studies included in the analysis and then to assess each of the outcomes in this systematic review.
First, to describe the interventions applied in each of the studies, a table describing all the interventions by intervention type was constructed (table 2). Interventions delivered in each of the studies were split into six categories: GP education, updating clinical referral pathways, direct communication, indirect communication, electronic clinical decision support tools and provision of glucose/ketone monitors. Studies included in this review were categorised into intervention types and summarised this way to facilitate systematic analysis and comparison, particularly due to the diversity of interventions delivered and the variation in methodologies employed by each of the studies. To classify each of the interventions, the research team identified common themes among the studies and classified the interventions accordingly. The criteria for allocating a particular intervention to the intervention type are summarised in table 2.
Table 2
| Intervention-type category | Criteria for inclusion |
| GP education | This included sessions facilitated by GPs to improve awareness of symptoms, referral pathways and recommended clinical actions on suspicion of type 1 diabetes. |
| Updated referral pathways | This included updating clinical management guidelines. |
| Direct communication with GPs | This included explanatory letters regarding the intervention, specific feedback to GPs following a timely or delayed referral. (The differentiating factor between direct and indirect communication was that the communicated information was targeted and specific to individual GPs). |
| Indirect communication with GPs | This included postcards mailed to GPs raising awareness of symptoms of diabetes. |
| Electronic clinical decision support tools | This included electronic alerts to GPs that are triggered at the point of care. |
| Provision of glucose and/or ketone monitors | This included provision of physical glucose and/or ketone monitors from the researchers to GP clinics. |
GPgeneral practitioner
We summarised intervention types used in each study in table 3. Following this, a structured summary table was constructed, with investigations ordered from lowest RoB to highest risk within the table. Within the structured summary table, we reported the intervention type, number of GPs reached with the intervention, intervention length and reported outcome measures (1A: the number of children presenting in DKA following the diagnostic delay, 1B: the number of children presenting in DKA and 2: GP timely referral behaviour). The structured summary table is presented in table 4 of the ‘Results section’. In terms of synthesis and analysis of the outcomes measured in this review (1A: the number of children presenting in DKA following diagnostic delay, 1B: the number of children presenting in DKA and 2: GP timely referral behaviour), a structured summary table was only completed for outcome 1B and narrative synthesis was completed for outcomes 1A and 2. This is due to the limited number of studies that reported on outcomes 1A and 2. For outcome 1B, the results were synthesised by listing the number and calculating the percentage of children presenting in DKA at baseline and during the intervention, and the percentage change. This is presented in table 5 of the ‘Results’ section.
Table 3
| Author, year | GP education | Updating clinical referral pathways | Direct | Indirect | Electronic clinical decision support tools | Provision of glucose and/or ketone monitors |
| Darmonkow et al, 202131 | Nationally accredited GP education course | – | – | Posters raising awareness of the signs and symptoms of DKA were sent to primary care physician offices. | – | – |
| King et al, 201229 | 12 clinics visited over 2 years | – | Letters explaining intervention, newsletter blast about T1DM symptoms | – | – | Once-off provision of glucose/ketone metres to practices. |
| Patwardhan et al, 201830 | 12 sessions over 2 years | – | – | – | – | – |
| Ahmed et al, 201628 | GPs reminded about existing referral pathways | – | – | – | – | – |
| Townson et al, 201627 | Education/training on how to use metres, presentations to GPs and practice nurses on two continuing professional development days | – | – | – | – | One-off provision of glucose/ketone metres to practices, training on how to utilise them provided. |
| Shetty and Dyban, 2022*26 | Embedded diabetes education in the Cardiff Protected Education Teaching sessions. | Referral guidelines for suspected T1DM were updated to encourage point-of-care testing and immediate referral. Explanatory letters were provided to GPs in the intervention locale. | Explanatory letters, direct feedback following a prompt or delayed T1DM diagnosis | – | – | – |
| Agwu and Lane, 2016*32 | – | – | – | – | When a venous blood glucose pathology referral is requested by a GP, a real-time alert appears prompting the GP to instead complete a point-of-care test, with the result guiding future management. | – |
| Jelley et al, 2010*33 | – | – | – | Postcard sent to GP with symptoms of T1DM | – | – |
DKAdiabetic ketoacidosisGPgeneral practitionerT1DMtype 1 diabetes mellitus
Table 4
| Author, year, location, study type | Intervention type(s) | Number of GPs that received the intervention, intervention length | Outcome 1A: Number of patients experiencing diagnostic delay/number of new-onset T1DM diagnoses | Outcome 1B: Number of patients in DKA/number of total new-onset T1DM diagnoses | Outcome 2: GPs’ behaviour/appraisal of the intervention | Consideration of statistical confounders |
| Darmonkow et al, 2021, Canada, non-randomised intervention study*31 | GP education sessions,Indirect communication with GPs | Number of GPs: 159Intervention length: 2 years | Not measured. | Pre: 157During: 107Post: 148 | Not measured | Effect of confounders was considered through the comparison of different time periods in the region: preintervention, during-intervention and postintervention. In the analysis, there was demographic stratification and consideration of many variables within the analysis phase. |
| King et al, 2012, Australia, controlled population intervention study29 | GP education sessions, supplied glucose/ketone metres, direct communication with GPs. | Number of GPs: unclearIntervention length: 2 years | Not measured. | Pre: 15/40During: 4/29 | Not measured | Effect of confounding variables was considered with a comparison to hospital data from a nearby locale with a very similar population demographic, a ‘control’ population. Data were also collected for a baseline and intervention in both control and intervention populations. Choice of statistical analysis measure accounts for random variation. |
| Patwardhan et al, 2018, Australia, non-randomised intervention study30 | GP education sessions | Number of GPs: unclearIntervention length: 2 years | Not measured. | Pre: (45/82)During: 6/24 | Not measured | Effect of confounding variables is considered with the use of a comparator measure, measuring DKA hospitalisation prior to the intervention and comparing this to during the intervention. The study has also assessed presentations based on demographic characteristic and selected analysis measures (multivariate binary logistic regression) accounts for potential confounders. |
| Ahmed et al, 2016, Saudi Arabia, non-randomised intervention study28 | GPs ‘reminded’ about referral pathways | Number of GPs: unclear.Intervention length: 4 years | Not measured. | Pre: 243/541During: 82/200 | Not measured | Effects of confounding were minimised with the use of a 10-year frequency rate of DKA before the intervention window. Analysis was stratified by age. |
| Townson et al, 2016, Wales, feasibility study27 | GP education sessions, supplied glucose/ketone metres. | Number of GPs: 560 clinicians, 73 practices.Intervention length: 12 months. months. | Not measured. | Not measured. | Qualitative interviews conducted with 9 GPs: GPs felt they had increased their use of point-of-care tests, excluding diabetes as a possibility more frequently. Glucose/ketone metres served as a physical reminder to test. GPs felt repeat education sessions are required to retain the information provided. | Qualitative methods were utilised in this study to measure the effectiveness of the interventions. No statistical confounders. |
| Shetty and Dyban, 2022, Wales, non-randomised intervention study*†26 | GP education sessions, direct communication with GPs, updated clinical referral pathways | Number of GPs: unclearIntervention length: 2 years | Pre: 7/40During: 4/60 | Pre: 12/40During: 17/60 | 91% of children had point-of-care testing completed on diagnosis postintervention as opposed to 75% preintervention. 53 GPs surveyed after education sessions, 51 reported that they will change their clinical practice, 2 reported that they would not. | There was a comparison of DKA admissions, and diagnostic delay preintervention and during intervention. Reported methods of analysis are limited as this is a conference abstract, |
| Agwu and Lane, 2016, England, non-randomised intervention study with 10 year audit* ‡32 | Clinical decision support tool (electronic pop-up alert) | Number of GPs: unclearIntervention length: 3 months. months. | Pre: 2/11During: 0/15 | Pre: 5/11During: 5/15 | 19% reduction in pathology tests ordered (p=0.02)772 tests ordered in the 3 months preintervention, 626 tests ordered in the 3 months preintervention, 626 tests ordered in the 3 months postintervention. months postintervention. | There was a comparison of DKA admissions, and diagnostic delay preintervention and during intervention. There was also measurement of pathology tests requested preintervention and during intervention. Reported methods of analysis are limited as this is a conference abstract. |
| Jelley et al, 2010, USA, non-randomised intervention study*33 | Indirect communication with GPs | Number of GPs: unclearIntervention length: 6 months months | Not measured | Pre: 60/193During: 17/55 | Not measured. | There was a comparison of DKA admissions pre and during intervention. Reported methods of analysis are limited as this is a conference abstract, |
DKAdiabetic ketoacidosisGPgeneral practitionerT1DMtype 1 diabetes mellitus
Table 5
| Author, year | DKA rate pre intervention (number of children in DKA/number of new T1DM diagnoses) | DKA rate postintervention (number of children in DKA/number of new T1DM diagnoses) | Change |
| Townson et al, 201627 | 45% (243/541) | 41% (82/200) | −4% |
| Shetty and Dyban, 2022*26 | 30% (12/40) | 28% (17/60) | −2% |
| King et al, 201829 | 54.90% (45/82) | 25% (6/24) | −29.9% |
| Ahmed et al, 201228 | 37.50% (15/40) | 14% (4/29) | −23.5% |
| Agwu and Lane, 2016*32 | 45% (5/11) | 33% (5/15) | −12% |
| Jelley et al, 2010*33 | 31% (60/193) | 31% (17/55) | 0 |
Note: DKA rate is measured as the number of patients presenting in DKA divided by the total number of new T1DM diagnoses in the measured timeframe. DarmonkowPatwardhan et al’s study30 was removed from the summary table as it measured DKA rate as an incidence per 100 000 and not per new T1DM diagnosed. *Studies that are conference abstracts with no corresponding publication. Shetty provided further information as the corresponding publication is not ready yet.
000 and not per new T1DM diagnosed. *Studies that are conference abstracts with no corresponding publication. Shetty provided further information as the corresponding publication is not ready yet.
DKAdiabetic ketoacidosisT1DMtype 1 diabetes mellitus
A summary of the interventions used and the effect on outcomes measured in each investigation is provided in table 4.
Patient and public involvement
None.
Search results
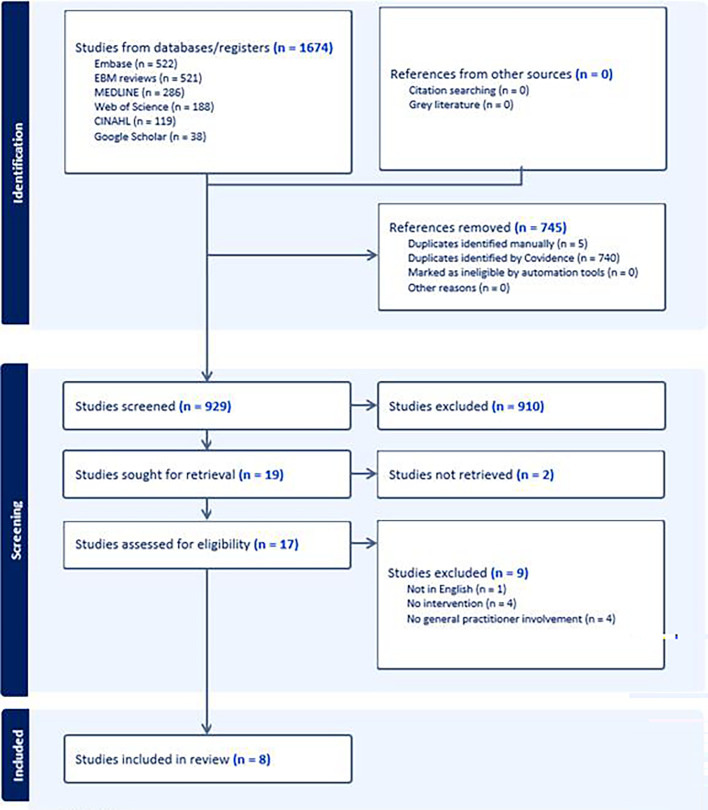
Following the systematic search of the six databases, 1674 publications were identified and imported into Covidence.23 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses25 flow chart in figure 2 summarises the search, screening and selection process. No additional studies were identified in the search for grey literature.
Author correspondence
Authors of the three conference abstracts deemed suitable for inclusion in the review were contacted by email. The author of Shetty and Dyban26 returned additional material regarding the methods and results of the study completed.
RoB: results
Three of the studies were excluded from Risk Of Bias In Non-randomised Studies of Interventions (ROBINS-I) assessment as they were conference abstracts and there was insufficient information to conduct ROBINS-I analysis. These studies are indicated by an asterisk in the summary tables. The five studies that were assessed all largely constituted low RoB among all domains. Moderate RoB was identified in two studies’ selection of participants, and one study’s deviation from the intended intervention. Two studies were classified as NI for the domain regarding bias due to deviation from the intended intervention. For the Townson et al27 investigation, the intervention was not evaluated over time and with qualitative interviews, therefore, there is no information on whether there was bias from the intended interventions over time. For the Ahmed et al28 study, the intervention methods specifically used to remind primary healthcare practitioners of the updated same-day referral pathways are not clearly reported, it is, therefore, difficult to know whether there was deviation. No domains were classified as high RoB, and no publications were excluded from the review following the ROBINS-I assessment. The full ROBINS-I assessment is in online supplemental appendix 1.
Key findings
Of the eight studies included, five were peer-reviewed publications27,31 and three were conference abstracts.26 32 33 Interventions sites spanned six countries (Australia (n=2), the USA, Saudi Arabia, Canada, England and Wales (n=2)) and ranged in length from 3 months to 4 years. Study designs included non-randomised intervention studies (n=6),2628 30,33 controlled population intervention studies (n=1)29 and feasibility studies (n=1).27 Seven of the eight studies addressed the primary outcomes,2628,33 while three addressed the secondary outcomes.26 27 32 Variation in reporting of research methods as well as measurement and reporting of outcomes was observed and informed our conclusion that meta-analysis could not be warranted. Six studies reported achieving a statistically significant reduction in DKA rate during the intervention period.28,33 Two of these reported that DKA rate returned back to baseline postintervention,31 33 whereas the others did not measure this. Due to the limited number of investigations included in the review, the large variation in interventions, methodologies, measured outcomes and approaches, and the results of the ROBINS-I analysis, synthesis of cumulative evidence was not conducted, and as a result, we did not evaluate the certainty of cumulative evidence generated in this review. A summary of the key findings is provided in tables2 tables2 3. 3. Summary tables2 tables2 3 3 have reordered the studies depending on the RoB assessment.
months to 4 years. Study designs included non-randomised intervention studies (n=6),2628 30,33 controlled population intervention studies (n=1)29 and feasibility studies (n=1).27 Seven of the eight studies addressed the primary outcomes,2628,33 while three addressed the secondary outcomes.26 27 32 Variation in reporting of research methods as well as measurement and reporting of outcomes was observed and informed our conclusion that meta-analysis could not be warranted. Six studies reported achieving a statistically significant reduction in DKA rate during the intervention period.28,33 Two of these reported that DKA rate returned back to baseline postintervention,31 33 whereas the others did not measure this. Due to the limited number of investigations included in the review, the large variation in interventions, methodologies, measured outcomes and approaches, and the results of the ROBINS-I analysis, synthesis of cumulative evidence was not conducted, and as a result, we did not evaluate the certainty of cumulative evidence generated in this review. A summary of the key findings is provided in tables2 tables2 3. 3. Summary tables2 tables2 3 3 have reordered the studies depending on the RoB assessment.
Intervention types
Six studies included GP education as an intervention,26,31 two studies provided glucose and/or ketone metres to clinics,27 29 two studies included direct communication with GPs,26 29 one study included updated referral pathways,26 two studies included indirect communication with GPs31 33 and one study included a clinical decision support tool.32 Four studies paired the GP interventions with a publicity campaign, simultaneously targeting the appraisal and help-seeking intervals.27 30 31 33
Four of the eight studies employed a singular intervention,28 30 32 33 two employed two interventions27 31 and two employed three interventions.26 29 A summary of each study and intervention type used, with examples, is provided below (table 3).
Outcome 1A: rate of diagnostic delay emerging from general practice preintervention and postintervention
Two of the eight studies (both conference abstracts) included in this systematic review reported on the number of children that experienced diagnostic delay following referral from general practice preintervention and postintervention.26 32 The first study (Shetty and Dyban26) included GP education sessions, direct communication with GPs and updated clinical referral pathways as part of their intervention.26 A decrease in children presenting in DKA following a diagnostic delay from general practice was reported over the 2-year period of the intervention, from 18% (7/38) of new T1DM diagnoses preintervention to 7% (4/60) postintervention.26 The second study (Agwu and Lane32) employed a clinical decision support tool as their sole intervention, for the length of 3 months.32 A decrease was also reported from 18% (2/11) of new T1DM diagnoses preintervention to 0% (0/15) postintervention.32 Both studies also reported on DKA rate, where the first reported having maintained a similar DKA rate (30%–28.3%),26 and the other reported a decrease (45%–33%).32
months.32 A decrease was also reported from 18% (2/11) of new T1DM diagnoses preintervention to 0% (0/15) postintervention.32 Both studies also reported on DKA rate, where the first reported having maintained a similar DKA rate (30%–28.3%),26 and the other reported a decrease (45%–33%).32
Outcome 1B: DKA rate preintervention and postintervention
Seven of the eight studies measured DKA rate preintervention and postintervention.2628,33 Six of these studies reported DKA rate as the percentage of patients with new T1DM diagnoses presenting to hospital in DKA during the measured time frame.2628,30 32 33 Using this metric, five out of the seven studies reported a decrease in DKA rate.2628,30 32 One study did not report a change from baseline after the intervention.33 These results are summarised in table 5.
One study measured DKA rate as an incidence per 100 000 in an age-stratified population for a 2-year period.30 This study reported a decrease from baseline during the study period; 38.48 per 100
000 in an age-stratified population for a 2-year period.30 This study reported a decrease from baseline during the study period; 38.48 per 100 000 during intervention period compared with 55.61 per 100
000 during intervention period compared with 55.61 per 100 000 before the intervention period.30 However, this study also measured DKA incidence 2 years following the intervention and found that it returned to baseline again at 54.53 per 100
000 before the intervention period.30 However, this study also measured DKA incidence 2 years following the intervention and found that it returned to baseline again at 54.53 per 100 000.30
000.30
Outcome 2: GPs’ behaviour following the intervention
Three of the eight studies reported GPs’ behaviours as an outcome.26 27 32 GPs’ use of point-of-care tests and willingness to change practice following the intervention were the two main measures of this outcome reported by these studies.
Usage of point-of-care tests
GPs’ use of point-of-care tests when diagnosing T1DM was assessed in all three studies.26 27 32 Agwu and Lane reported a 19% reduction in pathology test referrals requested by a GP.32 Shetty and Dyban reported an increase in point-of-care testing for children diagnosed with new T1DM, where 75% had had point-of-care testing completed preintervention and 91% postintervention.26 Townson et al reported that GPs felt as though they were conducting point-of-care testing more often, that the provision of glucose/ketone monitors served as physical reminders to test and that they excluded T1DM as a possibility more frequently this way.27
GPs’ desire to change practice after the intervention
Two of the three studies assessed GPs’ desire to change practice postintervention.26 27 Shetty and Dyban, reported that 51 out of 53 GPs would change their practice following education sessions, information about the other two GPs is not provided.26 Townson et al reported a similar sentiment among GPs, that recognised the importance of keeping T1DM front of mind. However, GPs also felt that repeat education sessions would be required over time to retain the information provided at information sessions.27
Appraisal
Strengths and limitations of the studies included in this review
Three out of the eight studies included in this review were conference abstracts,26 32 33 where correspondence could only be established with an author from one of the three studies.26 Therefore, the ability to draw strong conclusions from these studies is limited. Further, six of the eight studies did not report how many GPs they had reached with their intervention.26,3032 33 While this can be difficult to measure, it is important contextual information providing insight into the scope of the intervention. None of the investigations which employed more than one intervention were able to identify which intervention contributed to the effect observed in their results.
While diagnostic delay following presentation to a GP was prioritised as the first outcome, this was only measured in two of the eight studies,26 32 while the rest measured DKA rate. Using DKA rate as the sole measure of intervention effectiveness is also problematic, as it does not provide insight into the exact nature of the delay that led to the hospital presentation, and whether this was potentially preventable with interventions applied in the general practice context. For example, if a child presents to their GP already in DKA, the child would more likely have benefited from interventions directed toward the appraisal or help-seeking intervals. It should be noted, however, that clinical deterioration in terms of severity of presentation (eg, venous pH, serum bicarbonate) may be avoided with timely identification of hyperglycaemic and ketosis. The quality improvement innovation measured each stage of delay that leads to a DKA presentation and found that while DKA rates did not decrease significantly from baseline (30%–28.3%), diagnostic delay following a visit with the GP did decrease significantly by 11%.26 It was found that delayed presentation to hospital without encountering a GP accounted for 70% of DKA presentations postintervention.26 This delay in presentation to a GP or directly to hospital could be attributable to the COVID-19 pandemic coinciding with the intervention period, where potential symptoms of T1DM were interpreted as symptoms of COVID-19 infection by parents and patients, or where there was anxiety around seeking medical assistance.26 The SARS-Cov-2 infection also has been documented to increase risk of T1DM onset in children, which could also contribute to the increase observed.34 Three studies also included publicity intervention components29 31 33 and solely reported DKA rate as an outcome, therefore, it is difficult to establish whether the reduction in DKA rates observed was attributed to the GP education interventions that were delivered or to the raising public awareness of the symptoms of T1DM. It is, therefore, challenging to quantify the effectiveness of the intervention based on DKA rates alone, as it does not provide a clear picture of the specific delay experienced by the patient. DKA rate is important to measure as it is the clinical endpoint we are seeking to prevent, however, there are several confounding variables that may obscure the true impact of the intervention; therefore, it should not be used alone as a measure of intervention effectiveness.
Three out of the eight studies measured GPs’ behaviour as an outcome.26 27 32 It should be noted that the study implementing the clinical decision support tool had an intervention window of 3 months, with a small amount of people presenting with new-onset T1DM during that time.32 This makes it difficult to draw appropriate statistical conclusions on the impact of the intervention on diagnostic delay or rates of DKA. It did, however, measure hundreds of diabetes pathology test referrals where a more reliable conclusion can be drawn. The other two studies measuring GP behaviour used appropriate sample sizes, and therefore, more confident statistical conclusions can be drawn.26 27
months, with a small amount of people presenting with new-onset T1DM during that time.32 This makes it difficult to draw appropriate statistical conclusions on the impact of the intervention on diagnostic delay or rates of DKA. It did, however, measure hundreds of diabetes pathology test referrals where a more reliable conclusion can be drawn. The other two studies measuring GP behaviour used appropriate sample sizes, and therefore, more confident statistical conclusions can be drawn.26 27
The review-specific issues within each study included are summarised below in table 6.
Table 6
| Author, date (citation) | Review-specific issues: |
| Darmonkow et al, 202131 |
|
| King et al, 201229 |
|
| Patwardhan et al, 201830 |
|
| Ahmed et al, 201628 |
|
| Townson et al, 201627 |
|
| Shetty and Dyban, 2022)26 |
|
| Agwu and Lane, 201632 |
|
| Jelley et al, 201033 |
|
DKAdiabetic ketoacidosis
Discussion
The six categories of intervention identified during this systematic review were: GP education, referral pathway changes, direct communication with GPs, indirect communication with GPs, clinical decision support tools and provision of glucose and/or ketone monitors. Due to the limited number of studies identified in this review, the heterogeneity in methodology, approach and measured outcomes of each of the studies included, and the limited reporting of methodology in some cases, we cannot draw confident conclusions regarding the effectiveness of any one of these interventions on the timeliness of T1DM diagnosis in general practice settings.
Comparison with existing tertiary review data
A tertiary review of existing systematic reviews focusing on quality improvement interventions applied in the broader general practice context identified that GP education, direct communication with GPs, clinical decision support tools, point-of-care reminders demonstrated a quality improvement effect.35 Systemic changes (which would correspond to referral pathway changes in our review) were not measured in this tertiary review.35 Neither was indirect communication measured in the tertiary review35 but was found to be ineffective in a randomised controlled trial implementing a quality improvement initiative for ischaemic heart disease and/or diabetes that passively disseminated worksheets to GPs.36
GPs in the feasibility study reported that education sessions would need to be repeated to retain the information.27 Longevity of the impact of these interventions was measured in two investigations, and despite their successes during the intervention window, a sustained effect following the intervention window was not demonstrated.29 31 Follow-up is required to understand whether the interventions have a lasting legacy impact postcessation. The tertiary review also considered sustainability of quality improvement interventions applied in the broader general practice context, to which there were also significant research gaps.35 They underscored the importance of the role of clinical leadership by singular individuals or small groups in maintaining the quality improvement effect of the interventions that have been applied.35 Qualitative interviews with diabetes quality improvement trialists in general practice have recommended that consideration of sustainability, reach and scale is required from the beginning of the intervention design to ensure that an intervention is delivered with feasibility, acceptability and sustainability in mind.37
Two systematic reviews already exist assessing the impact of public health campaigns for the purposes of raising awareness around the symptoms of T1DM.15 16 In Deylami et al’s 2018 review, a lack of information about the methods utilised in the studies meant that an accurate conclusion regarding the impact of the interventions could not be drawn.16 Cherubini et al’s 2021 review conducted a meta-analysis of the pooled effect of publicity campaigns on DKA rate. This effect was reported as a reduction in DKA rate of 7.20% (95% CI 0.99% to 13.41%).15 Similarly, our systematic review observed decreases in diagnostic delay, DKA rate and positive changes in GP behaviour, however, the insufficient documentation of methodologies in the three abstracts makes it difficult to confidently draw this conclusion.
Given the recommendations for same-day referral,9,11 the interventions described within this review have been designed to promote urgent (same-day) diagnosis and referral of patients with suspected new-onset T1DM from the general practice setting. The changes observed in diagnostic delay, DKA rates and GPs’ behaviours demonstrate that interventions with active involvement of GPs can lead to promising outcomes. However, further information on the methodology in several studies is needed to draw more confident conclusions about the effectiveness of these outcomes. Further, follow-up is required for information about the legacy effect of these interventions. Clinical decision support tools have demonstrated promising results,32 by reducing diagnostic delay and improving GP behaviour, although the clinical decision support tool was only used over 3 months. No subsequent studies using the same intervention have yet been completed that demonstrate sustained benefits over a longer time period.
months. No subsequent studies using the same intervention have yet been completed that demonstrate sustained benefits over a longer time period.
The intention of all interventions included in this review is around quality improvement and GP behaviour change, improving the ability to recognise T1DM and to promptly refer to the hospital. However, existing literature exploring the diagnostic delay interval further would suggest that the interventions included in this review address only one aspect of diagnostic delay.14 While these interventions target the controllable aspect of diagnostic delay; GP behaviour, there are also external, less controllable challenges that exist within the diagnostic interval that could also be addressed. For example, presentations of T1DM to general practice are often non-specific initially, as the child may not present with any of the ‘classical’ symptoms of T1DM.38 Given the unique context of general practice, only three consulted GPs before implementing the intervention,26 27 31 with the Townson et al27 investigation describing a GP advisory group that designed and determined the appropriate intervention. Bottom up research approaches, such as codesign methodologies, may provide additional insight regarding the specific challenges that GPs face when diagnosing paediatric T1DM, so that interventions can be designed accordingly. GP involvement is required to address the commonly non-specific nature of T1DM presentations, a noted research gap that is not addressed by any of the interventions assessed in this review. Interventions that support GPs to address these challenges can be explored in addition to the quality improvement measures that have been outlined here.
Strengths and limitations of this review
The strength of this review is that interventions specifically targeting the diagnostic interval, and outcomes relating to GP behaviours were assessed. It also outlines that DKA rates alone are not a sufficient outcome measure when assessing the effectiveness of interventions as children with prolonged appraisal/help-seeking intervals may already have established DKA at the time of first review.14 We have outlined key research gaps in the lack of involvement of GPs when designing interventions targeted at the diagnostic interval, as well as the lack of follow-up to measure long-term impact.
A significant limitation of this review was that only five publications and three abstracts were included. There were limitations to the amount of information available in the abstracts, limiting the capability for strong conclusions to be drawn. Documentation of our primary outcome, namely the proportion of patients with diagnostic delay following a visit with a GP was only measured in two studies. Due to the heterogeneity in methodology and reporting of outcomes, a meta-analysis could not be conducted for pooled estimates of the impact of interventions on outcome measures. These restricted our ability to draw stronger conclusions during this review. Due to the use of multiple intervention components, it is difficult to determine which intervention component was effective or if the components worked in synergy to impact DKA rates. There was also high heterogeneity in the interventions themselves, for example, with ‘GP education’ comprising several different approaches and methods. The lack of framework-driven interventions also renders it difficult to assess scalability, acceptability and reach. The observational nature of the included studies, as well as the small sample sizes, are also significant limitations. As a result of these limitations, we are not able to draw conclusions surrounding the effectiveness of the intervention types included in this review.
Conclusion
This systematic review identified that GP education, clinical decision support tools, updating clinical referral pathways, direct and indirect communication with GPs, and provision of glucose and/or ketone monitors have been employed as interventions to attempt to facilitate earlier diagnosis of type 1 diabetes in the general practice setting. Due to the limited information identified by this review, it is not possible to draw confident conclusions regarding the effectiveness of these interventions specifically for the general practice setting. We have also identified important gaps in research knowledge surrounding the long-term impact of these interventions and a lack of inclusion of GPs in the design of the interventions. Given the worldwide issue of increasing DKA rates, targeting these issues is crucial moving forward.
supplementary material
online supplemental file 1
online supplemental file 2
Footnotes
Funding: CB has received the Australian Government Research Training Program Stipend Scholarship to support her PhD. Publication support has been provided by the NHMRC Centre for Research Excellence in Digital Technology to Transform Chronic Disease Outcomes. Award numbers: N/A.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-085635).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Data availability statement
No data are available. All data relevant to the study are included in the article or uploaded as online supplemental information.
References
Review Process File
Articles from BMJ Open are provided here courtesy of BMJ Publishing Group
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Have interventions aimed at assisting general practitioners in facilitating earlier diagnosis of type 1 diabetes in children been successful? A systematic review protocol.
BMJ Open, 13(12):e076459, 30 Dec 2023
Cited by: 1 article | PMID: 38159949 | PMCID: PMC10759093
Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.
Cochrane Database Syst Rev, 2(2022), 01 Feb 2022
Cited by: 12 articles | PMID: 36321557 | PMCID: PMC8805585
Review Free full text in Europe PMC
Exploring the User Acceptability and Feasibility of a Clinical Decision Support Tool Designed to Facilitate Timely Diagnosis of New-Onset Type 1 Diabetes in Children: Qualitative Interview Study Among General Practitioners.
JMIR Form Res, 8:e60411, 23 Sep 2024
Cited by: 0 articles | PMID: 39312767 | PMCID: PMC11459099
School-based education programmes for the prevention of unintentional injuries in children and young people.
Cochrane Database Syst Rev, 12:CD010246, 27 Dec 2016
Cited by: 26 articles | PMID: 28026877 | PMCID: PMC6473192
Review Free full text in Europe PMC
Funding
Funders who supported this work.
Australian Government Research Training Program Scholarship (1)
Grant ID: N/A
NHMRC Centre for Research Excellence in Digital Technology to Transform Chronic Disease Outcomes (1)
Grant ID: N/A

 1,2
1,2