Abstract
Objective
Cervical cancer screening rates are low in Japan. Therefore, when a woman is pregnant, this is a good opportunity to visit an obstetrics and gynecology clinic to have cervical cytology. This study aimed to clarify the association between cervical cancer screening and the management of pregnant women's health.Methods
We prospectively examined the relationships between cervical cytological results during prenatal checkups and the following factors: participant's background, cytological sampling instruments, and awareness of cytological results.Results
Of the 2725 participants, 71 showed abnormal results defined as atypical squamous cells of undetermined significance or higher grade (ASC-US+). ASC-US+ detection rates were higher in smokers, younger participants, those with a low education, those without cancer screening in the past 2 years, and those who received cytology using a spatula or brush. A multivariable logistic regression analysis identified smoking (adjusted odds ratio: 2.99 [95% confidence interval: 1.41-6.33]) and a spatula/brush (adjusted odds ratio: 2.46 [95% confidence interval: 1.09-5.53]) as independent variables associated with detecting ASC-US+. Among the participants, 39.4% (28/71) self-reported "no abnormalities," despite obtaining an ASC-US+ result.Conclusions
Pre-pregnancy smoking and cytological sampling tools may contribute to detecting ASC-US+. Patients with detected abnormalities need accurate information and reliable follow-up.Free full text

Risk factors for positive cervical cytology during early pregnancy screening and awareness of positive cytological results in Japan: a report from the Pregnant Women Health Initiative
Associated Data
Abstract
Objective
Cervical cancer screening rates are low in Japan. Therefore, when a woman is pregnant, this is a good opportunity to visit an obstetrics and gynecology clinic to have cervical cytology. This study aimed to clarify the association between cervical cancer screening and the management of pregnant women’s health.
Methods
We prospectively examined the relationships between cervical cytological results during prenatal checkups and the following factors: participant’s background, cytological sampling instruments, and awareness of cytological results.
Results
Of the 2725 participants, 71 showed abnormal results defined as atypical squamous cells of undetermined significance or higher grade (ASC-US+). ASC-US+ detection rates were higher in smokers, younger participants, those with a low education, those without cancer screening in the past 2 years, and those who received cytology using a spatula or brush. A multivariable logistic regression analysis identified smoking (adjusted odds ratio: 2.99 [95% confidence interval: 1.41–6.33]) and a spatula/brush (adjusted odds ratio: 2.46 [95% confidence interval: 1.09–5.53]) as independent variables associated with detecting ASC-US+. Among the participants, 39.4% (28/71) self-reported “no abnormalities,” despite obtaining an ASC-US+ result.
Conclusions
Pre-pregnancy smoking and cytological sampling tools may contribute to detecting ASC-US+. Patients with detected abnormalities need accurate information and reliable follow-up.
Introduction
Cervical cancer is primarily caused by persistent human papillomavirus (HPV) infection. According to a 2018 report, 1 the morbidity and mortality rates of cervical cancer in many countries in the last 10 years have remained the same or declined. However, in Japan, approximately 11,000 individuals are diagnosed with cervical cancer every year, and approximately 2900 die from this condition, with an upward trend observed in morbidity and mortality rates. The incidence of cervical cancer peaks at the age of 40 years, and its prevalence increases in women aged 20 to 30 years. 2 In Japan, HPV vaccination was initiated in 2010 as an Emergency Vaccination Promotion Program for Cervical Cancer. In April 2013, HPV vaccines were approved as national immunization program vaccines. Two months later, the active recommendations for HPV vaccination were suspended. As a result of this suspension, the HPV vaccination rate in Japan continued to decline below 1%. 3 Although these recommendations resumed in April 2022, the 2030 World Health Organization goal of “90% of girls fully vaccinated against HPV by age 15 years” 4 might be impossible to achieve.
The cervical cancer screening rate by cervical cytology in the last 2 years in Japan was 43.7%, 5 which was below the average screening rate (61.6%) of the Organization for Economic Cooperation and Development member countries. 6 The screening rates in Japan by age group were 13.1% for women aged 20 to 24 years and 32.1% for those aged 25 to 29 years. 5 Although the cervical cancer screening rate is low in Japan, almost all pregnant women in Japan undergo prenatal checkups including cervical cytology according to the guidelines established by the Ministry of Health, Labour and Welfare. 7 Therefore, 86.8% of pregnant women undergo this procedure. 8 In a report of malignant tumors detected during pregnancy in Japan, cervical cancer was the most common (71.4%), and 92.0% of cervical cancer or cervical intraepithelial neoplasia (CIN) grade 3 cases were diagnosed by cancer screening in the early stage of pregnancy. 9 In Japan, pregnancy is an important opportunity for cancer screening, detection of disease, and subsequent continuous screening.
Cervical cancer screening by HPV detection has been introduced in limited municipalities as a free cancer screening program by 2024. The Guideline for Gynecological Practice 2020: Japan Society of Obstetrics and Gynecology allows the use of cotton swabs for cervical cytology in pregnant women to avoid bleeding. In fact, cotton swabs are used for cervical cytological sampling in two-thirds of facilities. 8 This practice raises the issue of whether cotton swabs as a sampling tool for cervical cytology, which are avoided in non-pregnant women, are appropriate during pregnancy.
Maruyama et al. 10 conducted a retrospective study of the medical records of women who gave birth at a single institution from 2014 to 2017. Cervical cytology abnormalities were detected during prenatal checkups and subsequent follow-up, and they clarified the necessity of cervical cytology tests during prenatal checkups. Of the 3393 women, only 18.8% underwent cervical cytology testing within 1 year before pregnancy. In 2641 women who underwent cervical cytology during pregnancy, abnormalities were found in 79 (3%), in whom 70 were first detected during pregnancy. The importance of cervical cytology testing during prenatal checkups was confirmed in this previous study. We launched a new multicenter, prospective, observational study to confirm the current situation of cervical cancer screening across Japan. The Pregnant Women Health Initiative project was initiated to determine the effect of infectious disease screening tests performed during antenatal checkups on the long-term maintenance and promotion of maternal and child health. We aimed to identify issues related to cervical cancer screening during pregnancy, including the frequency of abnormal cytology, differences in positive rates by a cervical cytology sampling tool, social background, knowledge of HPV, and a cervical cancer screening history.
Patients and methods
Patients and questionnaire
To conduct our prospective cohort study, we recruited pregnant women who had visited the Obstetrics and Gynecology Departments of 8 university hospitals and 17 regional core hospitals in Japan between June 2018 and September 2019. Pregnant women aged 20 years or older who were due to give birth in any of the participating institutions were consecutively provided verbal and written explanations of the research purpose. Additionally, they were assigned a participant number and a quick response code by the doctor in charge. The participants were provided with the URL of the online questionnaire through e-mail, entered their participant number, and completed the questionnaire. The survey was conducted using the security-enhanced questionnaire creation tool “Survey Monkey.” The questionnaire contained questions related to the participants’ career, social background, awareness of cervical cytology results, and knowledge of HPV infection. Additionally, data on the patients’ background, test results, and detailed examination results were obtained from the attending physicians in the participating institutions after each delivery. All patients’ details were de-identified.
Associations between cervical cytology and questionnaire responses
In this study, we analyzed the associations between the results of cervical cytology and the participants’ responses to questions regarding their age, delivery history, smoking status, household income, educational background, history of cervical cancer screening before pregnancy, HPV vaccination history, and cytological sampling tools.
Cervical cytology classification
The results of cervical cytology were classified in accordance with the Bethesda system. A normal result was negative for intraepithelial lesion or malignancy (NILM). Abnormal results included atypical squamous cells of undetermined significance (ASC-US), a low-grade squamous intraepithelial lesion (LSIL), a high-grade squamous intraepithelial lesion (HSIL), atypical squamous cells cannot exclude HSIL (ASC-H), squamous cell carcinoma (SCC), atypical glandular cells (AGC), adenocarcinoma in situ (AIS), and adenocarcinoma. ASC-US+ included all cytological abnormalities except for NILM, LSIL+ included LSIL, ASC-H, HSIL, SCC, AGC, AIS, and adenocarcinoma, and HSIL+ included ASC-H, HSIL, SCC, AGC, AIS, and adenocarcinoma. The reporting of this study conforms to the STROBE guidelines. 11
Statistical analysis
According to the results of cervical cytology, the participants were classified into the NILM group or the ASC-US+ group. A statistical analysis of the background of each group was performed. Nonresponses by participants and details unknown by physicians were excluded from the analysis.
The questionnaire items used to evaluate the relationship between the screening participants’ awareness of test results and cytological abnormalities were analyzed using the χ2 test. In a multivariable logistic regression analysis, explanatory variables were selected among the number of births, age, pre-pregnancy smoking status, household income, educational background, cancer screening rate, vaccination history, and sampling tools using the backward-stepwise method based on the Akaike information criteria. The odds ratio (OR) and 95% confidence interval (CI) were calculated. The two-sided significance level was set at 0.05. Statistical analyses were performed using R software, version 4.1.0 (www.r-project.org).
Ethical considerations
Pregnant women who consented to participate in the study submitted a signed consent form to the cooperating institution and registered as a participant by scanning their assigned quick response code or sending e-mails to the research office. This study has been approved by the research ethics committee of Yokohama City University and the cooperating institutions in accordance with the “Ethical Guidelines for Medical Research in Humans” and the Helsinki Declaration of 1975 as revised in 2013 (Approval No. B180500011; date of approval: 25/5/2018).
Results
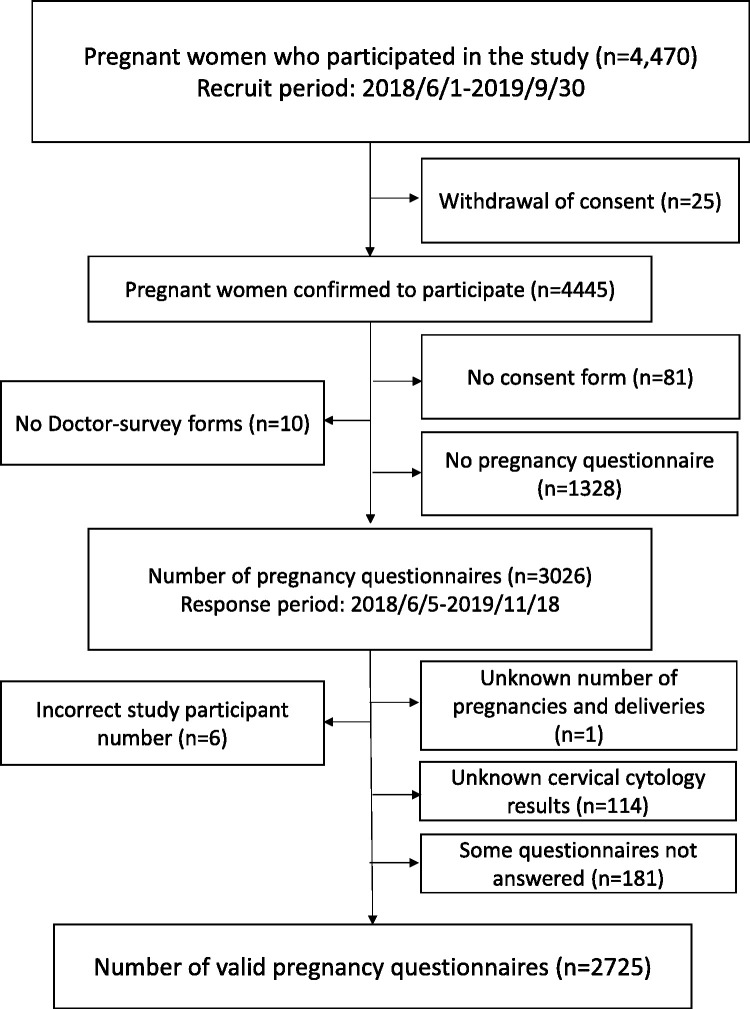
Among the 4470 pregnant women who provided consent to participate in this study between 1 June 2018 and 30 September 2019, 2725 were included in the final analysis. We excluded patients who did not submit a consent form or questionnaire form or those with inadequate responses to the questionnaire items on cervical cancer (Figure 1).
Table 1 shows the background information of the participants. There were 2654 participants in the NILM group and 71 participants in the ASC-US+ group in which the cytological abnormality detection rate was 2.7%. The mean age of all participants was 33.4 (standard deviation: 4.9) years. The study population included 604 participants in their 20 s, 1817 in their 30
s, 1817 in their 30 s, and 304 in their 40
s, and 304 in their 40 s or older. By age stratum, the ASC-US+ group comprised 25 (4.1%) participants in their 20
s or older. By age stratum, the ASC-US+ group comprised 25 (4.1%) participants in their 20 s, 41 (2.3%) in their 30
s, 41 (2.3%) in their 30 s, and 5 (1.6%) in their 40
s, and 5 (1.6%) in their 40 s or older. The rate of detecting cytological abnormalities was significantly higher in participants with a younger age according to a univariate analysis (p
s or older. The rate of detecting cytological abnormalities was significantly higher in participants with a younger age according to a univariate analysis (p =
= 0.023). Cytological abnormalities were more frequently detected in pre-pregnancy smokers than in pre-pregnancy non-smokers (p
0.023). Cytological abnormalities were more frequently detected in pre-pregnancy smokers than in pre-pregnancy non-smokers (p =
= 0.001). The cytological abnormality detection rate was significantly lower in participants with a university degree or higher than in those who graduated from junior high school/high school/college/specialist schools (p
0.001). The cytological abnormality detection rate was significantly lower in participants with a university degree or higher than in those who graduated from junior high school/high school/college/specialist schools (p =
= 0.041). Among the participants, 1974 had undergone cervical cancer screening 2 years before pregnancy, while 751 had not (including those who were screened
0.041). Among the participants, 1974 had undergone cervical cancer screening 2 years before pregnancy, while 751 had not (including those who were screened >
> 3 years before pregnancy, were never screened, or had an unknown status). The rate of detecting cytological abnormalities was significantly higher in women who had not undergone screening within 2 years before pregnancy than in women who had undergone cancer screening within 2 years (p
3 years before pregnancy, were never screened, or had an unknown status). The rate of detecting cytological abnormalities was significantly higher in women who had not undergone screening within 2 years before pregnancy than in women who had undergone cancer screening within 2 years (p =
= 0.005). In the ASC-US+ group, the rate of detecting cytological abnormalities was higher in participants whose samples were taken using a spatula or brush than in those whose samples were taken using a cotton swab (p
0.005). In the ASC-US+ group, the rate of detecting cytological abnormalities was higher in participants whose samples were taken using a spatula or brush than in those whose samples were taken using a cotton swab (p =
= 0.044). Although the detection rate did not vary based on the HPV vaccination status, this factor was difficult to evaluate because the number of participants who had received the HPV vaccine was relatively small. No significant difference was observed in the rate of detecting abnormalities between the primipara and multipara groups or between each household income group.
0.044). Although the detection rate did not vary based on the HPV vaccination status, this factor was difficult to evaluate because the number of participants who had received the HPV vaccine was relatively small. No significant difference was observed in the rate of detecting abnormalities between the primipara and multipara groups or between each household income group.
Table 1.
Background of the participants.
| Cervical cytology results | |||||||
|---|---|---|---|---|---|---|---|
| Overall | NILM | ASC-US + | |||||
n = = 2725 2725 | n = = 2654 2654 | n = = 71 71 | |||||
| n | % | n | % | n | % | p value | |
| Age at enrollment (years) | |||||||
 20–29 20–29 | 604 | 22.2 | 579 | 95.9 | 25 | 4.1 |  0.023 0.023 |
 30–39 30–39 | 1817 | 66.7 | 1776 | 97.7 | 41 | 2.3 | |
 40+ 40+ | 304 | 11.2 | 299 | 98.4 | 5 | 1.6 | |
| History of deliveries | |||||||
 Primipara Primipara | 1371 | 50.3 | 1329 | 96.9 | 42 | 3.1 | 0.131 |
 Multipara Multipara | 1354 | 49.7 | 1325 | 97.9 | 29 | 2.1 | |
| Smoking before pregnancy | |||||||
 Yes Yes | 370 | 13.6 | 351 | 94.9 | 19 | 5.1 | 0.001 |
 No No | 2355 | 86.4 | 2303 | 97.8 | 52 | 2.2 | |
| Household income (10,000 yen) | |||||||
 <300 <300 | 143 | 5.2 | 136 | 95.1 | 7 | 4.9 | 0.154 |
 ≥300 and <700 ≥300 and <700 | 1539 | 56.5 | 1504 | 97.7 | 35 | 2.3 | |
 ≥700 ≥700 | 1043 | 38.3 | 1014 | 97.2 | 29 | 2.8 | |
| Educational level | |||||||
 Junior high school/high school/ Junior high school/high school/ junior college/vocational school graduate junior college/vocational school graduate | 1440 | 52.8 | 1394 | 96.8 | 46 | 3.2 | 0.041 |
 University/graduate school graduate University/graduate school graduate | 1285 | 47.2 | 1260 | 98.1 | 25 | 1.9 | |
| Cervical cancer screening before pregnancy | |||||||
 Within 2 Within 2 years years | 1974 | 72.4 | 1933 | 97.9 | 41 | 2.1 | 0.005 |
 Others Others | 751 | 27.6 | 721 | 96.0 | 30 | 4.0 | |
| HPV vaccination* | |||||||
 Yes (1–3 times) Yes (1–3 times) | 207 | 7.6 | 200 | 96.6 | 7 | 3.4 | 0.506 |
 No No | 2191 | 80.4 | 2134 | 97.4 | 57 | 2.6 | |
 No answer No answer | 327 | 12.0 | 320 | 97.9 | 7 | 2.1 | |
| Sampling instruments of cervical cytology# | |||||||
 Cotton swab Cotton swab | 547 | 20.1 | 537 | 98.2 | 10 | 1.8 | 0.044 |
 Spatula/brush Spatula/brush | 719 | 26.4 | 692 | 96.2 | 27 | 3.8 | |
 Unknown Unknown | 1459 | 53.5 | 1425 | 97.7 | 34 | 2.3 | |
*Analyzed with a yes or no answer; #analyzed with a cotton swab or spatula/brush answer.
NILM, negative for intraepithelial lesion or malignancy; ASC-US+, atypical squamous cells of undetermined significance or higher grade; HPV, human papillomavirus.
Table 2 shows the results of cytological tests according to the tool used for sampling. The overall detection rate of ASC-US+ was 2.9%. The rate of cytological abnormalities appeared to be higher in the spatula/brush group than in the cotton swab group, regardless of the degree of cytological abnormality.
Table 2.
Cervical cytological results by sampling instruments.
| Sampling instruments | ||||||
|---|---|---|---|---|---|---|
| Overall | Cotton swab | Spatula/brush | ||||
n = = 1266 1266 | n = = 547 547 | n = = 719 719 | ||||
| n | % | n | % | n | % | |
| NILM | 1229 | 97.1 | 537 | 98.2 | 692 | 96.2 |
| ASC-US | 21 | 1.7 | 6 | 1.1 | 15 | 2.1 |
| LSIL | 9 | 0.7 | 2 | 0.4 | 7 | 1.0 |
| HSIL | 3 | 0.2 | 1 | 0.2 | 2 | 0.3 |
| ASC-H | 3 | 0.2 | 1 | 0.2 | 2 | 0.3 |
| AGC | 1 | 0.1 | 0 | 0.0 | 1 | 0.1 |
| SCC, AIS, or ADCA | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| ASC-US+ | 37 | 2.9 | 10 | 1.8 | 27 | 3.8 |
| LSIL+ | 16 | 1.3 | 4 | 0.7 | 12 | 1.7 |
| HSIL+ | 7 | 0.6 | 2 | 0.4 | 5 | 0.7 |
NILM, negative for intraepithelial lesion or malignancy; ASC-US, atypical squamous cells of undetermined significance; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade squamous intraepithelial lesion; ASC-H, atypical squamous cells cannot exclude HSIL; AGC, atypical glandular cells; SCC, squamous cell carcinoma; AIS, adenocarcinoma in situ; ADCA, adenocarcinoma.
ASC-US+: ASC-US, LSIL, HSIL, ASC-H, AGC, SCC, AIS, and ADCA.
LSIL+: LSIL, HSIL, ASC-H, AGC, SCC, AIS, and ADCA.
HSIL+: HSIL, ASC-H, AGC, SCC, AIS, and ADCA.
A multivariable logistic regression analysis was performed to identify the factors associated with detecting ASC-US+ (Table 3). A total of 1110 participants (1077 participants in the NILM group and 33 participants in the ASC-US+ group) were analyzed. We excluded those with an unknown HPV vaccination status from the 1266 participants with known cytological results and sampling tools. The explanatory variables chosen using the backward-stepwise approach based on the Akaike information criteria were age, pre-pregnancy smoking, and the sampling tool. Pre-pregnancy smoking (smoker: adjusted OR, 2.99 [95% CI: 1.41–6.33]; p <
< 0.05) and the sampling tool used (sampling by a spatula/brush: adjusted OR, 2.46 [95% CI: 1.09–5.53]; p
0.05) and the sampling tool used (sampling by a spatula/brush: adjusted OR, 2.46 [95% CI: 1.09–5.53]; p <
< 0.05) were independent explanatory variables associated with the detection of ASC-US+.
0.05) were independent explanatory variables associated with the detection of ASC-US+.
Table 3.
Multivariable logistic regression analysis of ASC-US+.
| OR (95% confidence interval) | p value | |
|---|---|---|
| Age at enrollment (years) | ||
 20–29 20–29 | Reference | 0.09 |
 30+ 30+ | 0.52 (0.25–1.09) | |
| Smoking before pregnancy | ||
 No No | Reference | <0.05 |
 Yes Yes | 2.99 (1.41–6.33) | |
| Sampling instruments of cervical cytology | ||
 Cotton swab Cotton swab | Reference |  <0.05 <0.05 |
 Spatula/brush Spatula/brush | 2.46 (1.09–5.53) | |
ASC-US+, atypical squamous cells of undetermined significance or higher grade (atypical squamous cells of undetermined significance, low-grade squamous intraepithelial lesion, high-grade squamous intraepithelial lesion, atypical squamous cells cannot exclude a high-grade squamous intraepithelial lesion, atypical glandular cells, squamous cell carcinoma, adenocarcinoma in situ, and adenocarcinoma).
To determine whether the pregnant women were aware of their abnormal test results, the following question was asked: “During this pregnancy, did you have abnormal cervical cytology?” Of the 59 participants who responded “Yes (abnormality in cervical cytological results),” 43 showed abnormalities in an actual cytological test, which indicated that the positive predictive value of self-reporting was 72.9% (Table 4). In contrast, despite the presence of abnormalities in the cytological test, 28 participants responded “No (no abnormalities).” Among these 28 participants, 20 had ASC-US (HPV-positive, 0; HPV-negative, 12; and unknown HPV status, 8), 4 had LSIL (CIN1 by biopsy, 3; repeated NILM after childbirth, 1), 3 had HSIL (1 participant had undergone cervical conization for CIN3 during pregnancy, 1 had CIN2 and was monitored during pregnancy, and 1 underwent a repeated cytological test and was further evaluated with colposcopy during pregnancy), and 1 had AGC (1 participant had an AIS-type AGC and underwent cervical conization during pregnancy). Among the 43 participants who recognized their abnormal cytological result correctly, 7 of 19 with ASC-US tested positive for HPV, 4 tested negative for HPV, and 8 had unknown results. Among 16 participants who were thought to have abnormal results, despite an actual normal cytological result, 6 had a history of cytological abnormalities or CIN. No association was found between knowledge of cervical cancer and the cytological results by evaluation between cytological abnormal results and the answer to the question “Did you know that most cervical cancer is caused by HPV infection?” Incidentally, two cases of conization during pregnancy resulted in term vaginal deliveries. There were no significant difference between the mode of delivery and cytological results (data not shown).
Table 4.
Pregnant women’s awareness of cervical cancer.
| Cervical cytological results | |||||||
|---|---|---|---|---|---|---|---|
| Overall | NILM | ASC-US + | p value | ||||
n = = 2725 2725 | n = = 2654 2654 | n = = 71 71 | |||||
| n | % | n | % | n | % | ||
| During this pregnancy, did you have an abnormal cervical cytology? | |||||||
 Yes Yes | 59 | 2.2 | 16 | 27.1 | 43 | 72.9 | <0.001 |
 No No | 2666 | 97.8 | 2638 | 98.9 | 28 | 1.1 | |
| Did you know that most cervical cancer is caused by HPV infection? | |||||||
 Yes Yes | 1202 | 44.1 | 1164 | 96.8 | 38 | 3.2 |  0.107* 0.107* |
 No No | 1479 | 54.3 | 1447 | 97.8 | 32 | 2.2 | |
 No answer No answer | 44 | 1.6 | 43 | 97.7 | 1 | 2.3 | |
*Analyzed with a yes or no answer.
NILM, negative for intraepithelial lesion or malignancy; ASC-US+, atypical squamous cells of undetermined significance or higher grade; HPV, human papillomavirus.
Discussion
In Japan, cervical cytology during pregnancy is an important screening opportunity that adds to the cervical cancer screening rate. In this study, we conducted a questionnaire-based survey in pregnant women to determine the actual status of cervical cancer screening among Japanese pregnant women. The test result data obtained from the attending physicians were compared with results of the questionnaire by participants to evaluate the characteristics of the population of women who showed abnormalities on actual cervical cytology. The risk factors for detecting ASC-US+ cytological abnormalities were age, pre-pregnancy smoking, educational background, cervical cancer screening history, and the sampling tool used for cytology as shown by the univariate analysis. The multivariable analysis including these factors identified cytological sampling by a spatula or brush and pre-pregnancy smoking as factors that contributed to the high detection rate of ASC-US+.
Currently, 64.2% of institutions in Japan use cotton swabs for cervical cancer sampling in pregnant women. 8 According to the Japanese clinical practice guidelines 2020, 12 in the general population, the use of a spatula/brush is more desirable, and the use of a cotton swab alone is not generally recommended. However, the use of cotton swabs is permitted to avoid the risk of bleeding, while sampling with spatulas and brushes can result in high cell counts. Many of the instruction manuals of sampling tools commonly used in Japan contain warning labels that prohibit their application for pregnant women. However, a study on 300 pregnant women showed no difference in the risk of severe pregnancy adverse events by a cervical cytological sampling device including a brush and spatula compared with cotton swabs. 13 However, the number of cells obtained for cervical cytology is greater with a sampling device including a brush and spatula than with cotton swabs in pregnant and non-pregnant women.13,14 In a univariate analysis of Japanese pregnant women, 8 the detection rate of ASC-US+ was higher when a spatula/brush was used during sampling than with a cotton swab. The multivariable analysis in this study also indicated the accuracy of spatula/brush sampling. We are currently conducting a retrospective cohort study as part of a multicenter joint study investigating the detection rate of ASC-H+ using sampling tools suitable for pregnant women.
This study showed an association between cervical cytological abnormalities and smoking. These results support the results of a previous study, which reported that smokers had a higher risk of developing CIN2+ than non-smokers. 15 In studies of Japanese women, smoking was found to be a risk factor for cervical cancer.16,17 The risk of developing cervical cancer is higher in smokers than in non-smokers, and this risk is further increased by the number of cigarettes smoked and the age at starting smoking. 17
The misunderstanding of abnormal cytological results by patients may be the cause of interruption of follow-up visits; therefore, the communication of accurate results and related information is important. In a Japanese study, the detection rate of abnormal cytology was higher in pregnant women who considered themselves healthy than in pregnant women who considered themselves with a poor health status. 18
In a previous study, 42 of 70 pregnant women with abnormal cytology during pregnancy were histologically diagnosed as CIN1+, but 5 (7.2%) women discontinued follow-up of their own accord from delivery to 6 months post-delivery.
10
These results indicate that creating an environment for continuous follow-up and increasing the awareness of pregnant women and health care providers are important.
months post-delivery.
10
These results indicate that creating an environment for continuous follow-up and increasing the awareness of pregnant women and health care providers are important.
In the present study, 28 of 71 (39.4%) participants with ASC-US+ detected during pregnancy thought that they had “no abnormalities in the test results.” The test results during pregnancy may not have been accurately communicated to the patient or the results may have been forgotten.
In this study, participants who misidentified cytological results as normal included those with ASC-US and negative HPV tests. There is a concern that this perception of normality may lead to a decline in postpartum screening rates. Cervical cytology during pregnancy may not be accurate; therefore, postpartum follow-up is important.
10
Health care providers and pregnant women need to share appropriate information on test results. Additionally, pregnant women should take preventive actions, such as regular cervical cancer examinations, and recognize that even if they have no subjective symptoms and consider themselves healthy, they are at risk of contracting cervical cancer at any time. In this study, 44.1% of pregnant women responded that “Most cervical cancer is caused by HPV infection,” and this level of awareness was not different between the ASC-US+ and NILM groups. Among young women, 16% to 65%19–21 are aware of the association between HPV infection and cervical cancer. In one Japanese survey,
21
the regular cervical cancer screening rate was approximately 30% for women with knowledge of cervical cancer, HPV, vaccines, and screening, while <
< 10% for those without this knowledge. Based on a questionnaire-based survey administered to 618 women aged 20 to 21 years,
22
the common reasons for not undergoing screening were as follows: “I have no symptoms,” “It’s costly to go to the hospital,” “I can’t be bothered to go to the hospital,” and “I’m afraid of what cancer screening is like.” Non-medical workers obtained information from the Internet, social media, television, advertisements of medical institutions, and educational curricula, which were considered important tools for providing knowledge. Women missed the opportunity to receive vaccinations and undergo medical examinations because of a lack of knowledge. Even if a medical checkup reveals an abnormality, these women may not perceive it as anything serious. The prevention, early diagnosis, and timely treatment of cervical cancer and enhancing knowledge about cervical cancer among women in Japan are important.
10% for those without this knowledge. Based on a questionnaire-based survey administered to 618 women aged 20 to 21 years,
22
the common reasons for not undergoing screening were as follows: “I have no symptoms,” “It’s costly to go to the hospital,” “I can’t be bothered to go to the hospital,” and “I’m afraid of what cancer screening is like.” Non-medical workers obtained information from the Internet, social media, television, advertisements of medical institutions, and educational curricula, which were considered important tools for providing knowledge. Women missed the opportunity to receive vaccinations and undergo medical examinations because of a lack of knowledge. Even if a medical checkup reveals an abnormality, these women may not perceive it as anything serious. The prevention, early diagnosis, and timely treatment of cervical cancer and enhancing knowledge about cervical cancer among women in Japan are important.
This study has some limitations. We only conducted a questionnaire-based survey. Approximately 60% of the study population completed the web survey, which may not reflect the overall situation. Additionally, those who preferred university hospitals or general hospitals for childbirth and agreed to participate in the study may have had a higher health literacy than the general population. Sampling instruments and abnormal cytological positivity rates were examined, but the sampling instruments were unknown in approximately half of all cases.
HPV testing is going to be introduced in Japan as part of cervical cancer screening. However, cervical cytology is still necessary for verification or risk classification of the HPV-positive population in pregnant women.
Conclusion
Japanese women have a low cervical cancer screening rate and a low HPV vaccination rate. In Japan, cervical cancer screening remains part of an initial examination during prenatal checkups because pregnancy is considered an opportunity for women to undergo cervical cancer screening. This study shows that pre-pregnancy smoking and cytological sampling tools are factors that may contribute to the detection of ASC-US+. Some pregnant women have an incorrect understanding of cytological abnormalities. Consequently, communicating test results more accurately and ensuring that women have a follow-up are important.
Acknowledgements
We thank Edanz for editing a draft of this manuscript.
Author contributions: All authors: Substantial contributions to the conception of the work, acquisition, and interpretation of data; drafting the work or revising it critically for important intellectual content; final approval of the version published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated.
EU: Investigation, writing original draft, validation, and editing.
TM: Review, editing, and supervision.
AS: Methodology and validation.
YS: Statistical analysis.
KK: Methodology and validation.
AI: Methodology and validation.
SA: Methodology and validation.
YU: Methodology and validation.
MS: Methodology and validation.
EM: Review, editing, and supervision.
The authors declare that they have no conflict of interest.
Funding: This work was supported by a Health Labour Sciences Research Grant from 2018 to 2020.
ORCID iD: Taichi Mizushima https://orcid.org/0000-0002-3505-4717
Data availability statement
The datasets used in the analyses of the current study are available from the corresponding author on reasonable request.
References
Articles from The Journal of International Medical Research are provided here courtesy of SAGE Publications
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Cervical cytopathological changes in pregnancy: An experience from a low resource setting.
Ann Afr Med, 20(3):212-221, 01 Jul 2021
Cited by: 2 articles | PMID: 34558451 | PMCID: PMC8477285
Diagnosis of Cervical Precancers by Endocervical Curettage at Colposcopy of Women With Abnormal Cervical Cytology.
Obstet Gynecol, 130(6):1218-1225, 01 Dec 2017
Cited by: 19 articles | PMID: 29112672 | PMCID: PMC5709212
Current status of cervical cytology during pregnancy in Japan.
PLoS One, 16(1):e0245282, 07 Jan 2021
Cited by: 3 articles | PMID: 33411854 | PMCID: PMC7790376
A Groundbreaking Work Which Laid the Foundation for Mass Screening in Cervical Cytology in Japan.
Acta Cytol, 61(4-5):299-304, 11 Jul 2017
Cited by: 1 article | PMID: 28693014
Review
Funding
Funders who supported this work.

 1
1