Abstract
Background
100 years after the first description, Alzheimer's disease is one of the most disabling and burdensome health conditions worldwide. We used the Delphi consensus method to determine dementia prevalence for each world region.Methods
12 international experts were provided with a systematic review of published studies on dementia and were asked to provide prevalence estimates for every WHO world region, for men and women combined, in 5-year age bands from 60 to 84 years, and for those aged 85 years and older. UN population estimates and projections were used to estimate numbers of people with dementia in 2001, 2020, and 2040. We estimated incidence rates from prevalence, remission, and mortality.Findings
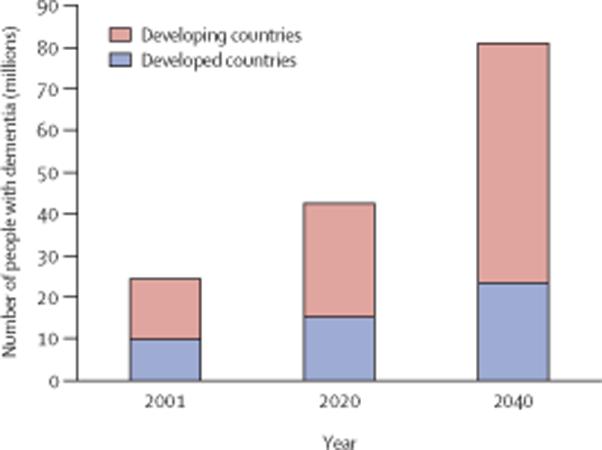
Evidence from well-planned, representative epidemiological surveys is scarce in many regions. We estimate that 24.3 million people have dementia today, with 4.6 million new cases of dementia every year (one new case every 7 seconds). The number of people affected will double every 20 years to 81.1 million by 2040. Most people with dementia live in developing countries (60% in 2001, rising to 71% by 2040). Rates of increase are not uniform; numbers in developed countries are forecast to increase by 100% between 2001 and 2040, but by more than 300% in India, China, and their south Asian and western Pacific neighbours.Interpretation
We believe that the detailed estimates in this paper constitute the best currently available basis for policymaking, planning, and allocation of health and welfare resources.Free full text

Global prevalence of dementia: a Delphi consensus study
Summary
Background
100 years after the first description, Alzheimer's disease is one of the most disabling and burdensome health conditions worldwide. We used the Delphi consensus method to determine dementia prevalence for each world region.
Methods
12 international experts were provided with a systematic review of published studies on dementia and were asked to provide prevalence estimates for every WHO world region, for men and women combined, in 5-year age bands from 60 to 84 years, and for those aged 85 years and older. UN population estimates and projections were used to estimate numbers of people with dementia in 2001, 2020, and 2040. We estimated incidence rates from prevalence, remission, and mortality.
Findings
Evidence from well-planned, representative epidemiological surveys is scarce in many regions. We estimate that 24·3 million people have dementia today, with 4·6 million new cases of dementia every year (one new case every 7 seconds). The number of people affected will double every 20 years to 81·1 million by 2040. Most people with dementia live in developing countries (60% in 2001, rising to 71% by 2040). Rates of increase are not uniform; numbers in developed countries are forecast to increase by 100% between 2001 and 2040, but by more than 300% in India, China, and their south Asian and western Pacific neighbours.
Interpretation
We believe that the detailed estimates in this paper constitute the best currently available basis for policymaking, planning, and allocation of health and welfare resources.
Introduction
Auguste D, a patient of Alois Alzheimer, was a 51-year-old woman with a 5-year history of progressive cognitive impairment, hallucinations, delusions, and severely impaired social functioning. After her death on April 8, 1906, Alzheimer identified in her brain amyloid plaques, neurofibrillary tangles, and arteriosclerotic changes. World Alzheimer's Day, Sept 21, 2006, marks the centenary of the identification and naming of the clinico-pathological entity that we now recognise to be the main cause of dementia syndrome, and one of the most burdensome conditions of later life.
According to the Global Burden of Disease estimates for the 2003 World Health Report,1 dementia contributed 11·2% of years lived with disability in people aged 60 years and older; more than stroke (9·5%), musculoskeletal disorders (8·9%), cardiovascular disease (5·0%), and all forms of cancer (2·4%). The disability weight for dementia, estimated by an international and multidisciplinary expert consensus, was higher than for almost any other health condition, apart from spinal-cord injury and terminal cancer. Although people with dementia are heavy consumers of health services, direct costs in developed countries arise mostly from community and residential care. Knapp and colleagues2 estimated that in the UK, 224 000 of the 461 000 elderly people with cognitive impairment live in institutions at a cost of £4·6 billion (US$8·2 billion) every year, or 0·6% of the UK gross domestic product. Family caregivers remain the cornerstone of support for people with dementia, experiencing substantial psychological, practical, and economic strain.3,4 Dementia care is particularly time intensive, and many caregivers need to cut back on work. In the USA, the annual cost of informal care was $18 billion per year in 1998 dollars.5
Such estimates of burden are critically dependent on the accuracy of the estimates of people living with the disease, which in turn depend on evidence from epidemiological surveys that are representative and well organised. For dementia in many world regions, such evidence is either incomplete or scanty in its coverage. Even when a wider evidence base is available for country or region-specific figures, these estimates are sometimes generated from single studies with little regard for their generalisability. Previous estimates of the number of people worldwide with dementia have tended to apply a uniform age-specific prevalence, assuming no important geographic variation.6,7 Prevalence has been noted to be lower in developing countries,8 strikingly so in some studies.9,10
Alzheimer's Disease International, the umbrella organisation for national Alzheimer's associations, convened an international group of experts to generate up-to-date evidence-based estimates for the prevalence and numbers of people with dementia in all regions of the world. Such figures would provide an authoritative and consistent foundation for global policymaking, and would assist national Alzheimer's associations to raise awareness of the size of the challenge faced by this and future generations.
Methods
Study design
We selected a Delphi consensus approach, guided by a systematic review of the published work on the prevalence of dementia from around the world. The essence of the Delphi consensus method is to derive quantitative estimates through the qualitative assessment of evidence. Studies of widely different design and quality can be assessed, much more than is usual in systematic reviews. When published information is scarce, experts can make inferences using other data from comparable contexts. Experts' estimates are aggregated and fed back anonymously to all participants, who then review their initial responses in view of group-wide choices.11,12 The group does not need to meet. This practice confers anonymity and allows opinions to be expressed free from peer-group pressure.
We sought consensus on dementia prevalence for all regions of the world, in 5-year age bands from 60 to 84 years, and for those aged 85 years and older. We combined the sexes, and focused on dementia prevalence rather than subtypes such as Alzheimer's disease because most prevalence data was neither gender-specific nor distinguished by subtype. WHO has divided the countries of the world into 14 regions based on geography (AMRO [the Americas], EURO [Europe], EMRO [north Africa and the middle east], AFRO [Africa], SEARO [south Asia] and WPRO [western Pacific]) and patterns of child and adult mortality, from A (lowest) to E (highest).
The panel was selected to achieve global coverage. The 12 experts had done studies on the prevalence of dementia, meta-analyses on regional or global dementia prevalence or incidence, or were able to bring a global perspective to the exercise. Investigators who worked together gave only one combined estimate, since it would have been difficult for them to avoid interacting. Thus, we obtained ten prevalence estimates per age-group per region.
CF and MP did a systematic review of published work from around the world on the prevalence of dementia to assist the panel's decision making. This review consisted of a MEDLINE search covering the period from 1980 to 2004. Studies were identified with the terms: dementia, Alzheimer's disease, prevalence, and cross-sectional. Secondary references and review papers were also examined. Consensus panel members were asked to identify any omissions. The only inclusion criterion was that the study should be population-based. Although studies varied widely in quality, methodology, and dementia outcome definition, the evidence contributed by all could be judged and weighted appropriately by the expert panel.
The studies were examined and a detailed document synthesising the research evidence for the 14 WHO regions was sent to each expert. This consisted of methodological details (setting, sample size, one-phase or two-phase survey, implementation of two-phase design, response rates for both phases, diagnostic criteria) and a table that summarised the age-specific prevalence estimates from every study. 95% CIs were included where they were given in the paper, or could be calculated from information provided. CF and MP highlighted any apparent methodological deficiencies, most of which related to the design, conduct, and analysis of two-phase surveys. All information was given separately for each of the 14 WHO regions.
Procedures
Participants reviewed the document combining the research evidence and gave their own estimates for dementia prevalence in the 14 WHO regions, for men and women combined, in 5-year bands from 60 to 64 years up to 85 years and older. We did not specify how estimates were to be derived, although when regional data were not available, we requested that the participants make inferences where possible from data from other regions. We did provide information about factors of potential relevance, namely the development status and child and adult mortality of the regions. Participants could also comment on the rationale for their decision.
The ten estimates of age-specific prevalence were entered into a spreadsheet for every region. Individual responses were made anonymous so that the experts could identify their own responses but not those of others. The group response was summarised as the mean prevalence estimate. These spreadsheets were then returned to the members of the panel who were invited to reconsider in the light of their colleagues' prevalence estimates and any accompanying comments. If they chose to alter their estimates, they could see the effect of this change on the group mean. All participants responded in the second round.
Analysis
The levels of agreement between participants in the first and second round of the exercise were assessed with intraclass correlation coefficient (ICC) within age-groups for every region. The mean prevalence estimate and its SD were calculated for each age-group and each WHO region. These means were applied to the current age-specific population estimates for the 14 WHO world regions to arrive at total numbers affected worldwide and by region. Population projections (demographic statistics available from the UN) were used to estimate numbers likely to be affected in 2020 and 2040. These projections assume that current prevalence would be constant over time. The Global Burden of Disease project DISMOD-II software was used to derive estimated incidence rates for the year 2001 from prevalence, remission, and mortality.13 Remission was assumed to be zero, and cause-specific mortality was modelled in terms of relative risks identified in EURODEM: RR of 2·38 up to age 89, declining to 1·8 in women aged 90 and older and 1·6 in men aged 90 and older.14
Role of the funding source
The sponsor had no role in study design, data collection, data analysis, data interpretation, or the writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
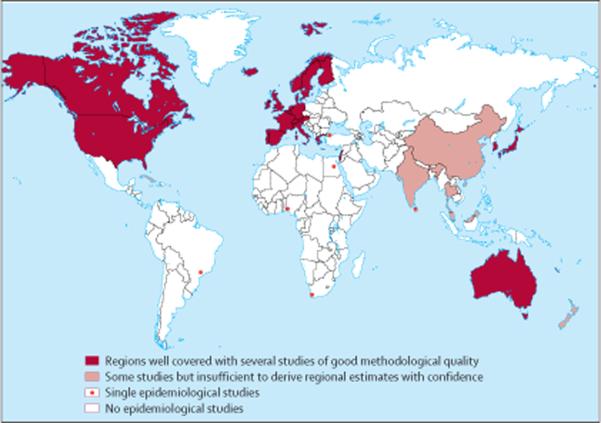
Figure 1 shows the extent of the global research evidence on the prevalence of dementia. The world regions coloured in red (North America, Europe, Japan, and Australia) are well covered with several studies of good methodological quality. Some epidemiological studies have been done in the regions coloured in pink, but they are insufficient in quality or quantity to provide representative estimates of the regional prevalence of dementia. Regions marked in white are completely or almost completely lacking in epidemiological studies; in these regions sites of single studies are marked with a red dot.
Agreement for AFRO E was poor in the first round (ICC=0·62 [95% CI 0·17–0·94]) but improved to 0·80 (0·56–0·96) in the second round. Otherwise, ICCs ranged from 0·88 to 0·99 in the first round, and from 0·95 to 0·99 in the second. There was an improvement in agreement for every region, other than EURO A and EURO C, for which agreement was already excellent (0·99) in the first round. Table 1 shows the mean and SD for the ten final prevalence estimates given by the 12 participants for all age-groups and the 14 WHO regions. The lowest estimates for all age-groups were given for AFRO D region followed by SEARO D, SEARO B, and AFRO E. DISMOD estimated that yearly incidence rates naturally follow the same regional pattern. When applying the prevalence figures from table 1 to the 2001 world population the estimated number of people with dementia worldwide is 24·3 million (table 2). Applying the DISMOD estimated incidence rates, we estimate 4.6 million new cases of dementia every year (about one new case every 7 s). The number of people living with dementia will almost double every 20 years, to 42·3 million in 2020 and 81·1 million in 2040. Although the expert consensus was for a higher prevalence of dementia in developed regions than developing regions, it is China and its developing western-Pacific neighbours that have the highest number of people with dementia (6 million), followed by western Europe with 4·9 million, and North America with 3·4 million. In 2001, 60·1% of all people with dementia lived in developing countries, rising to 64·5% in 2020 and 71·2% in 2040 (figure 2). At country level, the seven countries with the largest number of people with dementia in 2001 were: China (5·0 million), the European Union (5·0 million), USA (2·9 million), India (1·5 million), Japan (1·1 million), Russia (1·1 million), and Indonesia (1·0 million).
Table 1
Group mean consensus estimates (SD) for prevalence of dementia (%) for each region and age-group
| Age-group (years) | ||||||
|---|---|---|---|---|---|---|
| 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | ≥85 | |
| EURO A | 0·9 (0·1) | 1·5 (0·2) | 3·6 (0·2) | 6·0 (0·2) | 12·2 (0·8) | 24·8 (1·0) |
| EURO B | 0·9 (0·1) | 1·3 (0·1) | 3·2 (0·3) | 5·8 (0·3) | 12·2 (0·3) | 24·7 (2·3) |
| EURO C | 0·9 (0·1) | 1·3 (0·1) | 3·2 (0·2) | 5·8 (0·2) | 11·8 (0·5) | 24·5 (1·8) |
| AMRO A | 0·8 (0·1) | 1·7 (0·1) | 3·3 (0·3) | 6·5 (0·5) | 12·8 (0·5) | 30·1 (1·1) |
| AMRO B | 0·8 (0·1) | 1·7 (0·1) | 3·4 (0·2) | 7·6 (0·4) | 14·8 (0·6) | 33·2 (3·5) |
| AMRO D | 0·7 (0·1) | 1·5 (0·3) | 2·8 (0·4) | 6·2 (1·1) | 11·1 (2·0) | 28·1 (5·2) |
| EMRO B | 0·9 (0·3) | 1·8 (0·1) | 3·5 (0·3) | 6·6 (0·2) | 13·6 (0·8) | 25·5 (2·3) |
| EMRO D | 1·2 (0·3) | 1·9 (0·2) | 3·9 (0·3) | 6·6 (0·4) | 13·9 (1·3) | 23·5 (2·3) |
| WPRO A | 0·6 (0·1) | 1·4 (0·1) | 2·6 (0·3) | 4·7 (0·6) | 10·4 (1·2) | 22·1 (3·5) |
| WPRO B | 0·6 (0·1) | 1·8 (0·2) | 3·7 (0·4) | 7·0 (0·9) | 14·4 (1·9) | 26·2 (3·9) |
| SEARO B | 1·0 (0·1) | 1·7 (0·2) | 3·4 (0·2) | 5·7 (0·5) | 10·8 (1·2) | 17·6 (2·7) |
| SEARO D | 0·4 (0·1) | 0·9 (0·1) | 1·8 (0·2) | 3·7 (0·4) | 7·2 (1·2) | 14·4 (2·7) |
| AFRO D | 0·3 (0·1) | 0·6 (0·1) | 1·3 (0·2) | 2·3 (0·5) | 4·3 (1·0) | 9·7 (1·9) |
| AFRO E | 0·5 (0·3) | 1·0 (0·4) | 1·9 (0·9) | 3·8 (1·7) | 7·0 (3·6) | 14·9 (7·2) |
Table 2
Number of people with dementia in 2001, projections for 2020 and 2040, and percentage increases, by WHO region
| Population (millions), aged ≥60 years (2001) | Consensus dementia prevalence (%) at age ≥60 years | Estimated annual incidence per 1000 | New dementia cases (millions) per year, 2001 | Number of people (millions) with dementia, aged ≥60 years | Proportionate increase (%) in number of people with dementia | ||||
|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2020 | 2040 | 2001–2020 | 2001–2040 | |||||
| Western Europe (EURO A) | 89·6 | 5·4 | 8·8 | 0·79 | 4·9 | 6·9 | 9·9 | 43 | 102 |
| Eastern Europe low adult mortality (EURO B) | 27·4 | 3·8 | 7·7 | 0·21 | 1·0 | 1·6 | 2·8 | 51 | 169 |
| Eastern Europe high adult mortality (EURO C) | 44·6 | 3·9 | 8·1 | 0·36 | 1·8 | 2·3 | 3·2 | 31 | 84 |
| North America (AMRO A) | 53·1 | 6·4 | 10·5 | 0·56 | 3·4 | 5·1 | 9·2 | 49 | 172 |
| Latin America (AMRO B/D) | 40·1 | 4·6 | 9·2 | 0·37 | 1·8 | 4·1 | 9·1 | 120 | 393 |
| North Africa and Middle Eastern Crescent (EMRO B/D) | 27·5 | 3·6 | 7·6 | 0·21 | 1·0 | 1·9 | 4·7 | 95 | 385 |
| Developed western Pacific (WPRO A) | 34·5 | 4·3 | 7·0 | 0·24 | 1·5 | 2·9 | 4·3 | 99 | 189 |
| China and developing western Pacific (WPRO B) | 151·1 | 4·0 | 8·0 | 1·21 | 6·0 | 11·7 | 26·1 | 96 | 336 |
| Indonesia, Thailand, and Sri Lanka (SEARO B) | 23·7 | 2·7 | 5·9 | 0·14 | 0·6 | 1·3 | 2·7 | 100 | 325 |
| India and south Asia (SEARO D) | 93·1 | 1·9 | 4·3 | 0·40 | 1·8 | 3·6 | 7·5 | 98 | 314 |
| Africa (AFRO D/E) | 31·5 | 1·6 | 3·5 | 0·11 | 0·5 | 0·9 | 1·6 | 82 | 235 |
| TOTAL | 616·2 | 3·9 | 7·5 | 4·6 | 24·3 | 42·3 | 81·1 | 74 | 234 |
Projections for growth in the number of people with dementia indicate that regions fall into three broad groups (table 2). Developed regions start from a high base, but will experience a moderate proportionate increase (around 100% between 2001 and 2040). Latin America and Africa start from a low base but will experience a rapid increase in numbers (235–393%). India, China, and their south Asian and western-Pacific neighbours start from a high base and will experience rapid growth (314–336%). The consequences are striking. We predict that by 2040 China and its western-Pacific neighbours will have three times more people living with dementia than western Europe. Latin American countries today have half as many people with dementia (1·8 million) as North America (3·4 million), but by 2040 the numbers will be very similar (9·1 million and 9·2 million, respectively).
Discussion
We have generated expert consensus estimates of age-specific dementia prevalence for different world regions using the Delphi technique. We estimate that 24 million people have dementia today and that this amount will double every 20 years to 42 million by 2020 and 81 million by 2040, assuming no changes in mortality, and no effective prevention strategies or curative treatments. Of those with dementia, 60% live in developing countries, with this number rising to 71% by 2040. The rate of increase in numbers of people with dementia is predicted to be three to four times higher in developing areas than in developed regions.
In 1997, Prince6 estimated that 18 million people would be living with dementia today. He assumed the same prevalence in all regions and did not allow for regional differences in age distribution in the older population. Wimo and colleagues7, however, estimated a similar total number of people with dementia worldwide as our Delphi consensus; 25 million in 2000 rising to 63 million by 2030 and 114 million by 2050. They assumed the age-specific prevalence of dementia to be the same worldwide. They also calculated continent-specific numbers on the basis of published reviews. Wimo's figures differ substantially from our consensus for some regions; for example they estimate that there are 1·25 million people with dementia in Africa, but we estimated only 0·49. Compared with previous estimates, our consensus should be more sensitive to regional variation; the expert group reviewed all available evidence and its quality, and considered relevant regional characteristics.
The suggestion of a lower prevalence of dementia in developing regions than in developed regions8 is reinforced by the consensus judgment of our panel. Our experts seemed to be strongly influenced by the one study of good methodological quality from sub-Saharan Africa,10 for which the reported prevalence was very much lower than in developed countries. For south Asia (SEARO D), more weight seemed to be given to the similarly low estimates from the Ballabgarh rural north Indian study9 than to studies in more developed sites in south India,15,16 for which the reported prevalences are closer to those in Europe and North America. More research is needed to establish the generalisability of existing data and to explore differences between urban and rural areas.
Methodological factors might also be relevant; mild dementia could have been underdetected in the least developed regions because of difficulties in establishing social impairment. For China and its neighbours (WPRO B) the consensus prevalence estimates were very similar to those for Europe and North America. This finding is consistent with recent prevalence data from four Chinese cities, published after we had completed our consensus exercise.17 The lower prevalence in Africa and south Asia, if genuine, might be partly explained by lower survival with dementia rather than lower incidence. However, incidence estimates in Nigeria and India are also much lower than in developed countries.18,19 Differences in level of exposure to environmental risk factors might have contributed, with low levels of cardiovascular risk18 and hypolipidaemia19 in some developing countries both having been advanced as explanations. However, other risk factors, for example anaemia found to be associated with Alzheimer's disease in rural India,20 will be more prevalent in developing countries. High levels of mortality in early life could also be implicated; constitutional and genetic factors that confer survival advantage in early years might go on to protect against neurodegeneration or delay its clinical manifestations.
Our estimates have limitations. Although the expert panel achieved high levels of consensus, this was often on the basis of scant epidemiological evidence. Some of the estimates, particularly for developing regions with few studies, may be reliable but invalid. Figure 1 signifies the need for much more epidemiological research on dementia, particularly in Latin America, Russia and eastern Europe, the middle east, and Africa. Our projections should be interpreted with caution for several reasons. First, these relied on demographic statistics, which might not be accurate for many parts of the world, especially for older age-groups. Second, we assumed that age-specific prevalence in each region would remain constant over time. In fact, changes in risk exposure might increase or decrease incidence. Improved medical and social care might reduce case mortality and increase prevalence. Interventions that delay onset would have substantial potential for reducing age-specific prevalence. Irrespective of any such effects, it seems probable that as early and late life patterns of morbidity and mortality converge with those of the developed west, dementia prevalence levels will do likewise.21,22 The implication is that our projections for dementia in developing regions might be conservative. Efforts need to be made in all regions to monitor secular trends in incidence and prevalence associated with the epidemiological transition, and with changes in medical and social care.
We believe that the detailed estimates contained in this paper are the best currently available basis for policymaking, planning, and allocation of health and welfare resources. Primary prevention should focus on targets suggested by current evidence; risk factors for vascular disease, including hypertension, smoking, type 2 diabetes, and hyperlipidaemia.23 The epidemic of smoking in developing countries and the high rising prevalence of type 2 diabetes in Asia are particular causes of concern. More work is needed to identify further modifiable risk factors.
Achieving progress with dementia care in developing countries has much to do with creating the climate for change. Poor awareness is a key public-health problem with important consequences: affected people do not seek help, and if they do health-care services tend not to meet their needs;4 dementia is stigmatised, and sufferers can be excluded from residential care and denied admission to hospital;24–26 no constituency is available to lobby government; and families tend to have less support or understanding from others and experience substantial strain.4
National Alzheimer's associations help to raise awareness and create a framework for positive engagement between policymakers, clinicians, researchers, caregivers, and people with dementia. Most of Alzheimer Disease International's 75 members are associations in developing countries. Their advocacy, empowered by evidence of prevalence, effect, and need will foster the development of more responsive services. For many low-income countries the most cost-effective approach will be community primary care to support and advise family caregivers.4,24,26 Day care and residential respite care are expensive but important elements of a community service. Residential care is unlikely to be a government priority, but private nursing and residential care homes are already opening to meet the new demand. If government policies are well formulated and planned with the projections described in this paper in mind, the inevitable shift of resource expenditure towards older people can be predicted and its consequences mitigated.27 The health and social care needs of the large and rapidly growing numbers of frail, dependent older people should be a matter of great concern for policymakers in developing regions.
Acknowledgments
C Ferri and M Scazufca were fully supported by the Wellcome Trust (grant code GR066133MA) during the development of this work.
References
Full text links
Read article at publisher's site: https://doi.org/10.1016/s0140-6736(05)67889-0
Read article for free, from open access legal sources, via Unpaywall:
https://revistascientificas.cuc.edu.co/culturaeducacionysociedad/article/download/954/pdf_174
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/101728566
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1016/s0140-6736(05)67889-0
Article citations
Arterial stiffness measured by pulse wave velocity correlated with cognitive decline in hypertensive individuals: a systematic review.
BMC Neurol, 24(1):393, 16 Oct 2024
Cited by: 0 articles | PMID: 39415095 | PMCID: PMC11481605
Review Free full text in Europe PMC
Machine learning-based personalized composite score dissects risk and protective factors for cognitive and motor function in older participants.
Front Aging Neurosci, 16:1447944, 15 Oct 2024
Cited by: 0 articles | PMID: 39474283 | PMCID: PMC11518739
Destabilisation of Alzheimer's amyloid-β protofibrils by Baicalein: mechanistic insights from all-atom molecular dynamics simulations.
Mol Divers, 08 Oct 2024
Cited by: 0 articles | PMID: 39379662
Neuroprotective effects of magnesium: implications for neuroinflammation and cognitive decline.
Front Endocrinol (Lausanne), 15:1406455, 25 Sep 2024
Cited by: 0 articles | PMID: 39387051 | PMCID: PMC11461281
Review Free full text in Europe PMC
Poor sleep quality, dementia status and their association with all-cause mortality among older US adults.
Aging (Albany NY), 16(17):12138-12167, 04 Sep 2024
Cited by: 0 articles | PMID: 39237306 | PMCID: PMC11424588
Go to all (2,446) article citations
Other citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.
Cochrane Database Syst Rev, 2(2022), 01 Feb 2022
Cited by: 12 articles | PMID: 36321557 | PMCID: PMC8805585
Review Free full text in Europe PMC
The global prevalence of dementia: a systematic review and metaanalysis.
Alzheimers Dement, 9(1):63-75.e2, 01 Jan 2013
Cited by: 2032 articles | PMID: 23305823
Review
Estimating the number of people living with dementia at different stages of the condition in India: A Delphi process.
Dementia (London), 23(3):438-451, 05 Jun 2023
Cited by: 0 articles | PMID: 37272749 | PMCID: PMC11041066
Epidemiology of Alzheimer's disease and other forms of dementia in China, 1990-2010: a systematic review and analysis.
Lancet, 381(9882):2016-2023, 01 Jun 2013
Cited by: 350 articles | PMID: 23746902
Review
Funding
Funders who supported this work.
NIA NIH HHS (2)
Grant ID: R01 AG009956
Grant ID: R01 AG009956-14S1