Abstract
Free full text

Lung epithelial cells are essential effectors of inducible resistance to pneumonia
Abstract
Infectious pneumonias are a leading cause of death worldwide, particularly among immunocompromised patients. Therapeutic stimulation of the lungs’ intrinsic defenses with a unique combination of inhaled Toll-like receptor agonists broadly protects mice against otherwise lethal pneumonias. As the survival benefit persists despite cytotoxic chemotherapy-related neutropenia, the cells required for protection were investigated. The inducibility of resistance was tested in mice with deficiencies of leukocyte lineages due to genetic deletions and in wild type mice with leukocyte populations significantly reduced by antibodies or toxins. Surprisingly, these serial reductions in leukocyte lineages did not appreciably impair inducible resistance, but targeted disruption of Toll-like receptor signaling in the lung epithelium resulted in complete abrogation of the protective effect. Isolated lung epithelial cells were also induced to kill pathogens in the absence of leukocytes. Proteomic and gene expression analyses of isolated epithelial cells and whole lungs revealed highly congruent antimicrobial responses. Taken together, these data indicate that lung epithelial cells are necessary and sufficient effectors of inducible resistance. These findings challenge conventional paradigms about the role of epithelia in antimicrobial defense and offer a novel potential intervention to protect patients with impaired leukocyte-mediated immunity from fatal pneumonias.
INTRODUCTION
Lower respiratory tract infections constitute a tremendous worldwide public health threat, affecting hundreds of millions of people annually.1–4 Patients with hematologic malignancies, those with advanced HIV disease, and certain transplant recipients face extreme pneumonia risks due to impaired leukocyte-mediated immunity.5–7 In fact, in the transfusion era, pneumonia is the primary cause of death among patients with leukemia.8,9
We have previously reported that the lungs’ mucosal defenses can be stimulated to protect mice against otherwise lethal pneumonias.10–14 This phenomenon, known as inducible resistance, results from inhaled treatments targeting pattern recognition receptors in the lungs and yields broad protection against bacterial, viral and fungal pathogens.10,13,15–17 Most recently, we showed that robust pneumonia protection could be induced by a single inhaled treatment consisting of a unique, synergistic combination of Toll-like receptor (TLR) agonists: a diacylated lipopeptide ligand for TLR2/6, Pam2CSK4; and a class C unmethylated 2′-deoxyribo cytidine-phosphate-guanosine (CpG) ligand for TLR9, ODN M362 (hereafter, “Pam2-ODN”).15,17
Notably, while we have shown that onset of protection temporally correlates with treatment-induced neutrophil influx into the lungs, we have also demonstrated persistent protection, despite profound depletion of neutrophils and macrophages.10,11,15 As these leukocytes are widely considered the primary mediators of mucosal immunity in the lungs, these findings raised the question of which cells are principally required for inducible resistance.
Although the airway and alveolar epithelia are often regarded as passive airflow conduits and inert gas exchange barriers, it is evident that they possess intrinsic antimicrobial capacity that contributes to pathogen clearance under physiologic conditions.12,18–22 The current work supports an essential role for the lung epithelium in the therapeutic induction of resistance,10–12,15 but surprisingly, does not clearly identify any individual leukocyte lineages that are required for protection. These findings not only challenge conventional paradigms about the role of the lung epithelium in antimicrobial defense, but offer the potential to protect vulnerable patients with impaired leukocyte-dependent immunity.
RESULTS
Pam2-ODN-induced resistance to pneumonia persists despite reductions in numerous leukocyte lineages
Leukocytes are generally viewed as the principle (or sole) mediators of pulmonary innate immunity. However, since we have reported durable anti-pneumonia protection following leukodepleting therapies,10,15 we serially depleted leukocyte lineages in an effort to determine which cell types were required for inducible resistance.
Consistent with previous observations using myeloablative therapies,15 depletion of neutrophils to undetectable levels in both blood and bronchoalveolar lavage (BAL) fluid (Supplemental Figure 1A) failed to impair Pam2-ODN-induced protection against otherwise lethal infections with Pseudomonas aeruginosa and Streptococcus pneumoniae (Figures 1A and 1B). Further, neutrophil-depleted lungs could still be induced to kill bacteria by a single inhaled Pam2-ODN treatment. While complete absence of neutrophils is not assumed to occur following antibody-mediated depletion, no recruitable neutrophils were detected in the lungs of antibody-treated mice in the first 12 h after pathogen challenge, despite the observed differences in pathogen burden starting immediately after infection. By 24 h after pathogen challenge, rare neutrophils could be detected in the lungs of surviving mice by flow cytometry, though at a greatly reduced level compared to undepleted mice (Supplemental Figure 1B).
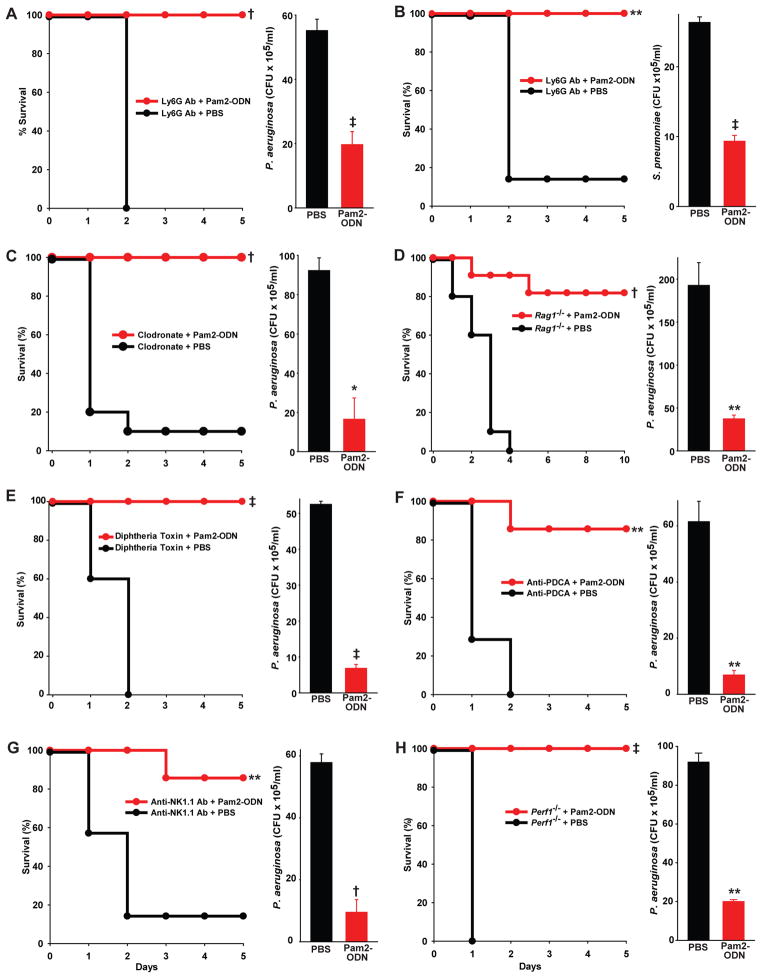
(A) Wild type C57BL/6J mice were depleted of neutrophils by intraperitoneal injection of anti-Ly6G Ab then inhalationally challenged with P. aeruginosa grown to mid-log phase following aerosolized Pam2CSK4 and ODN M362 (Pam2-ODN) or PBS (sham) treatment of the mice 24 h prior to the infectious challenge. (B) Neutrophil-depleted mice were inhalationally challenged with S. pneumoniae in mid-log phase with or without aerosolized Pam2-ODN pretreatment 24 h prior to infection. (C) Wild type mice were depleted of alveolar macrophages by two intratracheal treatments with liposomal clodronate prior to challenge with P. aeruginosa with or without aerosolized Pam2-ODN pretreatment 24 h prior to infection. (D) Rag1−/− mice were challenged with P. aeruginosa with or without aerosolized Pam2-ODN pretreatment 24 h prior to infection. (E) Mice expressing the diphtheria toxin receptor under the CD11c promotor received repetitive intratracheal doses of diphtheria toxin prior to challenge with P. aeruginosa with or without aerosolized Pam2-ODN pretreatment 24 h prior to infection. (F) Wild type mice were depleted of plasmacytoid dendritic cells by intraperitoneal injection with anti-PDCA Ab, prior to challenge with P. aeruginosa with or without aerosolized Pam2-ODN pretreatment 24 h prior to infection. (G) Wild type mice were depleted of natural killer cells by intraperiotneal injection with anti-NK1.1 Ab, prior to challenge with P. aeruginosa with or without aerosolized Pam2-ODN pretreatmen 24 h prior to infection t. (H) Perf1−/− mice were challenged with P. aeruginosa with or without aerosolized Pam2-ODN pretreatment 24 h prior to infection. For all experiments, the left panel displays pneumonia survival (N = 8–10 mice/group for all experiments), the right panel displays the lung pathogen burden immediately after the infectious challenge as assessed by serial dilution culture of whole lung homogenates (N = 3–6 mice/group for all experiments). Panels shown are representative of at least three separate experiments. All survival groups were followed for at least 14 d, no deaths occurred outside the presented periods. (*p<0.03, **p<0.005, †p<0.0006, ‡p<0.00001 relative to PBS-treated control)
To address the role of alveolar macrophages in inducible resistance, mice were treated with intratracheal liposomal clodronate, resulting in 70 to 80% reductions in alveolar macrophages in the airways of treated mice compared to untreated mice or mice treated with control liposomes. Mice depleted of alveolar macrophages in this manner displayed no impairment in either Pam2-ODN-induced protection or rapid intrapulmonary pathogen killing (Figure 1C). Similarly, mice lacking functionally mature lymphocytes (Figure 1D) displayed no impairment of inducible resistance.
Dendritic cells have been reported to critically participate in modulation of mucosal defense in the lungs and elsewhere,23,24 and they express abundant TLRs.25,26 Therefore, these lineages were viewed as likely to be required for Pam2-ODN-induced resistance. However, despite substantial reductions in the number of conventional dendritic cells with diphtheria toxin or antibody-mediated depletion of plasmacytoid dendritic cells (Supplemental Figure 2), mice were still protected against lethal Pseudomonas pneumonia (Figure 1E and 1F). Protection was equally inducible by Pam2-ODN in mice substantially depleted of dendritic cells mice and sham-depleted mice.
Given their microbicidal role in innate immunity,27,28 natural killer (NK) cells were also investigated as potential mediators of inducible resistance. However, mice significantly depleted of NK cells with antibodies (Supplemental Figure 2) and mice lacking functional NK cells due to perforin deficiency similarly displayed no impairment of Pam2-ODN-induced resistance (Figures 1G and 1H).
In addition to exerting directly microbicidal effects on infecting pathogens, leukocytes also express interleukin 22 (IL-22) in response to infections, promoting antimicrobial responses from nonhematopoietic cells at environmental interfaces.29 Consistent with the leukocyte depletion studies, IL-22 knockout mice were fully protected by Pam2-ODN against P. aeruginosa pneumonia (Figure 2). Taken together, these studies fail to demonstrate a single, critically important leukocyte effector of inducible resistance.
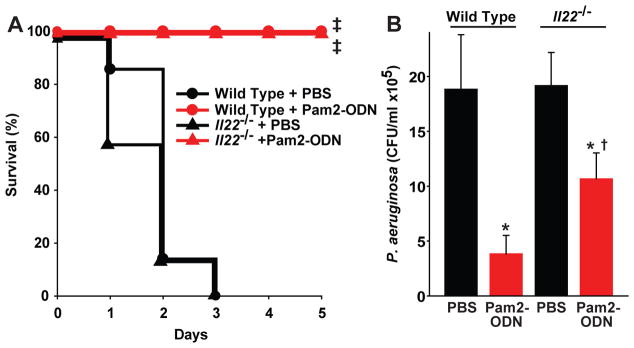
Il22−/− mice and wild type littermates were inhalationally challenged with P. aeruginosa grown to mid-log phase with or without aerosolized Pam2-ODN pretreatment 24 h prior to the infectious challenge. (A) Survival of pneumonia (N = 8 mice/group), (B) lung pathogen burden immediately after the infectious challenge as assessed by serial dilution culture of whole lung homogenates (N = 3 mice/group). (*p < 0.01 vs. PBS-treated wild type; **p < 0.03 vs. PBS-treated Il22−/−; †p > 0.09 vs. Pam2-ODN-treated wildtype; ‡ p < 0.0001 vs. PBS-treated syngeneic mice)
Pam2-ODN-induced resistance requires canonical TLR signaling pathway activation
As no individual tested leukocyte lineage was confirmed to be a central effector cell of inducible resistance, an alternate effector cell was needed to explain the protective response induced by Pam2-ODN. We have hypothesized that lung epithelial cells might serve an effector function in inducible resistance.11,13,15 However, unlike the tested leukocytes, anatomic depletion of the lung epithelium is incompatible with host survival. So, it was necessary to identify a means to functionally disrupt the epithelium without impairing gas exchange.
TLR2/6:Pam2 and TLR9:ODN-initiated signaling events are described to require the Toll/Interleukin 1 receptor (TIR) adaptor MyD88. However, given the unanticipated synergy observed with Pam2-ODN, it was important to confirm that the Pam2-ODN-induced protection actually required signal propagation via known MyD88 pathways. As shown in Figure 3A, while wild type mice were fully protected against P. aeruginosa pneumonia by a single inhaled Pam2-ODN treatment on the day prior to infection, MyD88-deficient littermates could not be similarly protected. Consonantly, Pam2-ODN induced rapid pathogen killing in the lungs of Pseudomonas-challenged wild type mice, but had no such effect in MyD88-deficient mice.
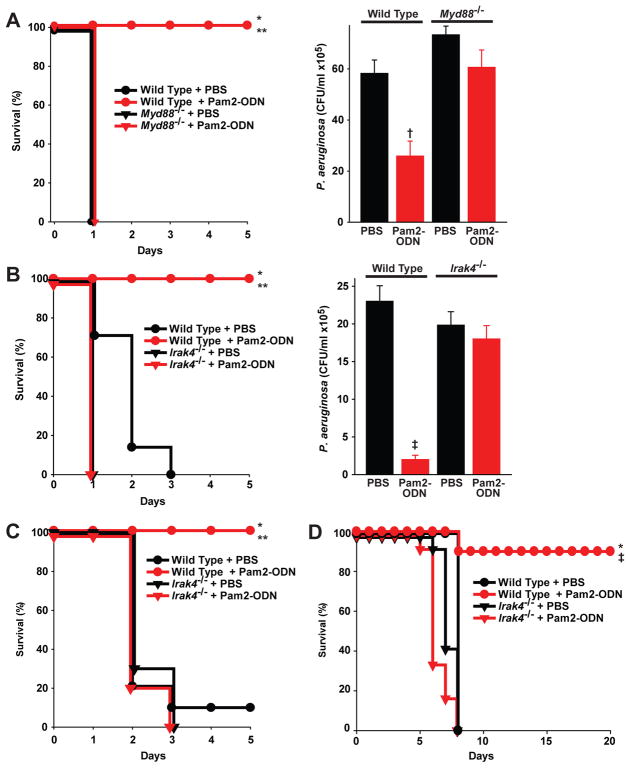
(A) Myd88−/− and wild type littermates were inhalationally challenged with P. aeruginosa grown to mid-log phase with or without aerosolized Pam2-ODN treatment 24 h prior to infection. Left, survival (N = 10 mice/group); right, lung bacterial burden immediately after infection (N = 3 mice/group). (B) Irak4−/− and wild type mice inhalationally challenged with P. aeruginosa with or without Pam2-ODN pretreatment 24 h prior to infection. Left, survival (N = 10 mice/group); right, lung bacterial burden immediately after infection (N = 3 mice/group). (C) Irak4−/− and wild type mice inhalationally challenged with S. pneumoniae with or without Pam2-ODN pretreatment 24 h prior to infection. (D) Irak4−/− and wild type mice inhalationally challenged with influenza A virus (H3N2) with or without Pam2-ODN pretreatment 24 h prior to infection. (* p < 0.0001 wild type + Pam2-ODN vs. knockout + Pam2-ODN; ** p < 0.0001 wild type + PBS vs. wild type + Pam2-ODN; † p < 0.02 wild type + PBS vs. wild type + Pam2-ODN)
Recent structural and functional analyses indicate that MyD88-dependent TLR signaling is propagated by formation of giant signalosomes (“Myddosomes”) following recruitment of IRAK4.34–37 Given the novel synergy observed with Pam2-ODN, we sought to further test whether inducible resistance utilized this classically described TLR-MyD88-IRAK4 pathway. Figure 3B confirms that IRAK4-deficient mice phenocopy mice lacking MyD88, resulting in total abrogation of the protective Pam2-ODN effect against P. aeruginosa pneumonia and failing to induce pathogen killing in the lungs.
Although we have described broad protection following Pam2-ODN treatment, it is conceivable that protection against different pathogens occurs via different mechanisms. To confirm that protection against non-Pseudomonas pathogens proceeds via recruitment of the same proximal signaling molecules, we also attempted to induce protection against a Gram-positive bacterium and a virus by Pam2-ODN inhalation in IRAK4-deficient mice. As shown, Pam2-ODN protects wild type mice against lethal challenge with these pathogens, but IRAK4 deficiency resulted in complete loss of inducible resistance against S. pneumoniae (Figure 3C) and influenza A (Figure 3D).
Lung epithelial cells are necessary and sufficient for inducible resistance
The requirement for canonical TLR-MyD88-IRAK4 signaling following Pam2-ODN inhalation afforded an opportunity to functionally disrupt the epithelium without requiring cellular depletion. So, MyD88 was conditionally deleted in lung epithelial cells. As observed in experiments with full MyD88 knockout mice (Figure 3A), inhaled Pam2-ODN treatment conferred no significant protection to lung epithelium-specific Myd88SPCΔ/Δ mice challenged with P. aeruginosa (Figure 4A), nor could intrapulmonary pathogen killing be induced by the TLR treatment (Figure 4B). Similarly, as shown in Figure 4C, protection against lethal influenza pneumonia by Pam2-ODN was also found to be highly dependent on lung epithelial MyD88. Together, these studies confirm that MyD88-dependent signaling in the lung epithelium is required for Pam2-ODN-induced resistance to pneumonia.
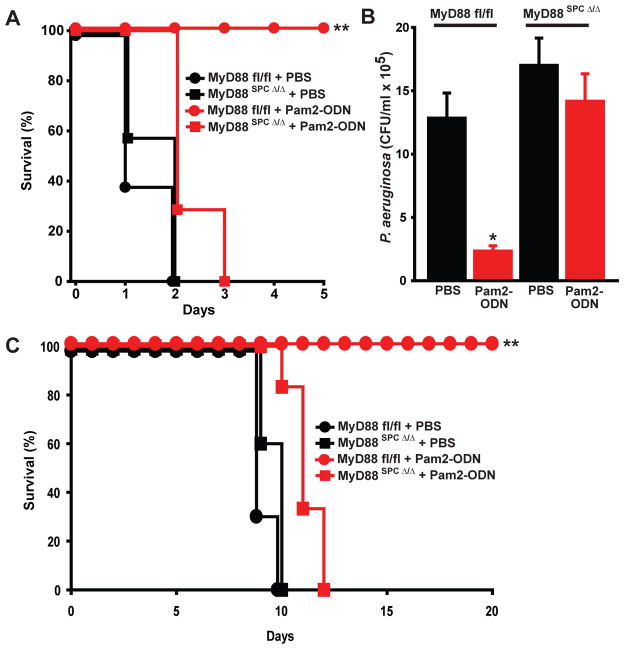
Mice conditionally-deficient in lung epithelial Myd88 (Myd88SPCΔ/Δ) and littermate controls (Myd88fl/fl) were inhalationally challenged with P. aeruginosa grown to mid-log phase with or without aerosolized Pam2-ODN pretreatment 24 h prior to the infectious challenge: (A) pneumonia survival (N = 8 mice/group), (B) lung pathogen burden immediately after the infectious challenge (N = 3 mice/group). (C) Survival of influenza pneumonia in lung epithelial Myd88 deletants and littermate controls with or without aerosolized Pam2-ODN pretreatment 24 h prior to the infectious challenge. (* p < 0.0005 vs. PBS-treated Myd88fl/fl; ** p < 0.0001 vs. Pam2-ODN-treated Myd88SPCΔ/Δ)
Pam2-ODN-induced protection is described as inducible resistance, rather than inducible tolerance, because the survival benefit is consistently associated reductions in pathogen burden. Remarkably, inducible pathogen killing is even evident immediately after delivery of an infectious challenge. As shown in Figure 5A, the lungs of Pam2-ODN-treated wild type mice contained one log fewer P. aeruginosa CFU/ml than did sham-treated mice immediately after inhalational challenge. 24 h after infection, the lung pathogen burden of the sham treated mice had again doubled, whereas Pam2-ODN-treated mouse lungs demonstrated a bacterial burden reduced by another two logs compared to Pam2-ODN-treated mice at 0 h. By 48 h after infection, the Pam2-ODN-treated mice cleared the remaining pathogens, whereas the sham-treated mice had all succumbed to infection. Together, these data suggest that generation of a microbicidal environment is an important, ongoing process in effective inducible resistance.
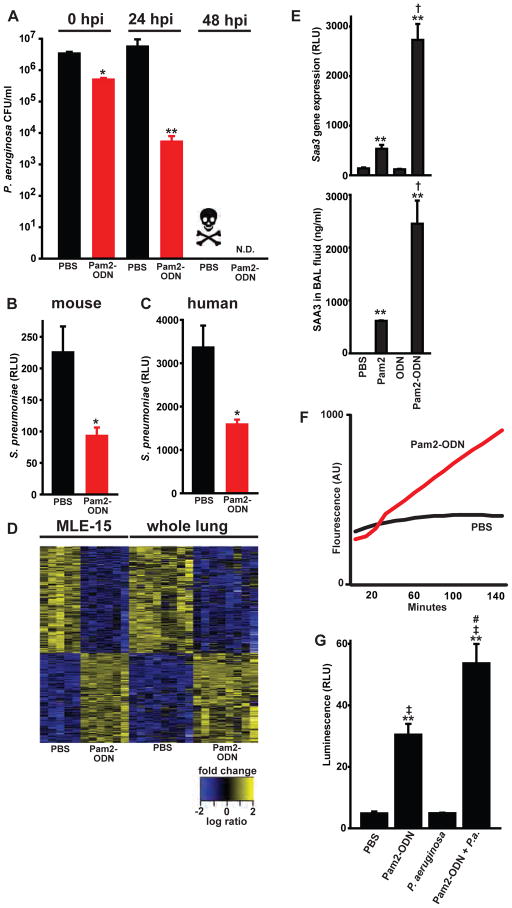
(A) Wild type mice were inhalationally challenged with P. aeruginosa grown to mid-log phase with or without aerosolized Pam2-ODN treatment 24 h prior to infection. Lungs were harvested at the indicated times after infection, homogenized in 1 ml PBS, and submitted to serial dilution culture. All sham-treated mice died before the 48 h harvest. (n = 3–6 mice/group) (B). Primary mouse tracheal epithelial cell cultures were inoculated with luminescent S. pneumoniae after 4 h pretreatment with Pam2-ODN or PBS, then the culture pathogen burden was assessed by luminescence intensity. (C) Pathogen burden of HBEC3-KT cultures infected with luminescent S. pneumoniae 4 h after pretreatment with Pam2-ODN or PBS. (D) Heatmap of differentially-expressed genes in MLE-15 cells or whole mouse lung homogenates 4 h after treatment with Pam2-ODN, shown as standardized log ratios of fold change. (E) Saa3 mRNA levels in whole lung homogenates (upper panel) and SAA3 protein concentration in BAL fluid (lower panel). (F) Reactive oxygen species generation by MLE-15 cells following treatment with PBS or Pam2-ODN, detected by H2DCF-DA. (G) Reactive oxygen species generation by intact lungs, assessed by luminescence detection of BAL fluid following lavage with L-012-containing PBS. (hpi, hours post-infection; N.D., none detected; * p < 0.04 vs. PBS-treated; ** p < 0.008 vs. PBS-treated; † p < 0.008 vs. Pam2-treated; ‡ p < 0.001 vs. P. aeruginosa infected; # p < 0.035 vs. Pam2-ODN-treated, uninfected)
Testing the sufficiency of lung epithelial cells to generate such a microbicidal environment, isolated lung epithelial cells were stimulated with Pam2-ODN for 4 h prior to bacterial infection. Pam2-ODN-treated primary mouse tracheal epithelial cells infected with luminescent S. pneumoniae demonstrated significantly lower pathogen burdens than did PBS-treated controls, as assessed by luminescence intensity (Figure 5B). We and others have previously reported that culture luminescence correlates with an extremely high degree of certainty (R2 > 0.998) with pathogen burden as assessed by serial dilution cultures, and allows for detection of free, bound and internalized pathogens.15,38,39 Thus, Pam2-ODN-treated epithelial cells appeared to autonomously reduce the pathogen burden. However, because it is virtually impossible to exclude the possibility of leukocyte contamination in primary epithelial cultures, we also tested a model system that allowed for no such contamination. Using the human bronchial epithelial cell line HBEC3-KT,40 we observed comparable induction of pathogen killing by epithelial cells in the absence of any leukocytes (Figure 5C).
Further exploring the capacity of epithelial cells to mediate the observed protective response, we compared Pam2-ODN-induced gene expression in isolated mouse lung epithelial cells (MLE-15) to that of whole mouse lung homogenates. By hypergeometric testing,41,42 the two gene sets were found to significantly overlap (p < 10−10), indicating that lung epithelial cells (in the absence of leukocytes) respond to Pam2-ODN exposure in a manner that was statistically similar to intact mouse lungs treated with Pam2-ODN. Figure 5D shows the 585 congruently differentially expressed transcripts, not surprisingly heavily enriched for TLR signaling and antimicrobial defense genes (individually reported in Supplemental Table 1).
Previous proteomic analyses demonstrate antimicrobial peptide production following inhalation of bacterial lysates.10 However, we have not previously confirmed that Pam2-ODN-induced defense transcript enrichment translated into antimicrobial peptide production. Serum amyloid A3 (Saa3) is among the most strongly induced transcripts following lysate11 or Pam2-ODN exposure,15 and it is the single most synergistically induced gene product (i.e., greatest mRNA induction following combined Pam2-ODN treatment relative to the sum of the effects of Pam2 and ODN administered alone). As shown in Figure 5E, Saa3 gene expression correlates tightly with BAL concentrations of SAA3 protein, demonstrating both the translation of the gene expression signal and the similarity to lysate-induced resistance. Similar responses were observed for isolated MLE-15 cells (not shown).
In addition to protein mediators of resistance, we have speculated that reactive oxygen species (ROS) are generated in response to Pam2-ODN treatment, but have not previously demonstrated this element of the response. Using 2′,7′-dichlorodihydrofluoresceindiacetate acetyl ester (H2DCF-DA) to detect ROS generation, we found significant induction from MLE-15 cells within minutes of Pam2-ODN treatment (Figure 5F). To determine whether this phenomenon extended to the intact lung, we devised a novel strategy to assess for volatile ROS. Mice underwent BAL with the ROS-detecting agent L-012 added to the PBS lavagate. As shown in Figure 5G, ROS levels were significantly elevated 24 h after Pam2-ODN inhalation, and this was further enhanced in the presence of P. aeruginosa (but not by the infectious challenge alone).
DISCUSSION
Pneumonia remains a leading cause of death in virtually all populations worldwide. Our recent reports have described the novel strategy of therapeutically stimulating the lungs’ intrinsic defenses as a means to counter this threat. While we have previously hypothesized that the epithelium could play an important role in facilitating inducible resistance, we have heretofore been unable to conclusively demonstrate the contribution of the epithelia to inducible resistance. The data presented here allow us, for the first time, to convincingly demonstrate an essential role for lung epithelial cells as essential effectors of inducible resistance.
Therapy-induced leukocyte infiltration of the lungs, particularly neutrophil influx, has been temporally associated with the onset inducible resistance. However, we previously identified instances where protection persisted despite neutrophil depletion.10,15 In the current study, serial reductions of several leukocyte populations did not reveal any individual hematopoietic cell types that were definitely required for Pam2-ODN-induced resistance. As the antibody- and toxin-dependent leukocyte-depleting techniques used may fail to achieve complete absence of their target populations, it is difficult to conclusively infer the role of individual leukocytes from the depletion studies when considered in isolation. Moreover, we hypothesize that leukocytes, when present, likely provide a reinforcing signal that promotes inducible resistance, at a minimum. Nonetheless, it is notable that protection can still be induced in mice substantially depleted of multiple leukocyte types.
This finding is of potentially great importance to numerous immunocompromised patient populations. Many patients with hematologic malignancies, autoimmune diseases, advanced HIV disease and solid organ or stem cell transplants face elevated risks of pneumonia due to quantitative or qualitative leukocyte deficiency. If inducible resistance relied heavily on these deficient cells, aggressive inhalational stimulation with Pam2-ODN would be unlikely to benefit the most vulnerable patients. Therefore, leukocyte independence of the protective response would be a highly favorable characteristic for these immunocompromised populations.
Potentially limiting the interpretation of these results is that, in most experiments, only one leukocyte lineage was depleted at a time. While most conditions do not present with pan-leukocyte depletion, it is conceivable that concurrently depleting multiple cell types could result in an uncompensatable defect or otherwise impair the Pam2-ODN response. Further, it is possible that differences in the duration and means of leukodepletion might influence a defect of inducible resistance, and this is an area of ongoing research. However, as IL-22 has been shown to be a critical means for leukocyte mediated stimulation of epithelia and we have found IL-22 to be dispensable for inducible resistance, it is appears less likely that a combination of leukocyte deficiencies would further impair this epithelial response. Moreover, the demonstration of antimicrobial responses from isolated epithelial cells emphasizes the importance of leukocyte-independent epithelial responses in Pam2-ODN-induced protection.
The identification of the epithelium as a critical mediator of inducible resistance is also a favorable finding from the perspective of protecting immunocompromised patients. Suppression of leukocyte-mediated immunity, as in hematologic malignancies and/or cytotoxic chemotherapy, does not obviate the lungs’ intrinsic responses to infection. Rather, profoundly immunosuppressed patients generate striking inflammatory responses to pulmonary infections.43 Perhaps more importantly, lung epithelial cells’ capacity to generate antimicrobial responses are uniquely spared the effects of immunosuppressive therapy,44 probably reflecting their slow cellular turnover rate, as contrasted with rapidly replaced gut epithelial cells that display loss of barrier and antimicrobial function with cytotoxic therapies.45,46 Thus, inducible epithelial resistance may liberate many patients from reliance on leukocyte-mediated immunity as their sole defense against pneumonia by engaging cells that are relatively impervious to the immunosuppressive and cytotoxic therapies they require for their underlying diseases.
We are not the first group to demonstrate active participation of epithelial cells in host defense. In fact, Mijares and colleagues have reported that lung epithelial MyD88 contributes to mouse survival in a model of P. aeruginosa pneumonia.47 However, to our knowledge we are the first to show that loss of MyD88 in the lung epithelium results in loss of protective immunity in the presence of an intact leukocyte-mediated immune system. Further, unlike other studies investigating TLR-signaling in the lungs, we have shown a requirement for epithelial function for therapeutic enhancement of mucosal immunity, whereas others have focused on modulating baseline susceptibility to infection. While the confirmation of MyD88-dependent signaling advances our understanding of inducible resistance, based on the unique synergy of two reportedly MyD88-dependent TLR ligands, we hypothesize that MyD88-independent events also contribute to the protective phenomenon. For instance, the current studies have not excluded the possibility of Pam2-ODN-induced signaling via TRIF or inflammasome-associated pathways.
Another unique aspect of these studies is the demonstration of direct antimicrobial responses from the lung epithelium following Pam2-ODN treatment. Regardless of organ, previous reports of epithelial stimulation by TLR ligands almost all identify leukocytes as the primary TLR target cells, with subsequent (leukocyte-derived) cytokines driving epithelial responses. By apparently obviating the need for an intermediary leukocyte, this may expand the pool of potentially benefitting patients to include those without functional leukocytes, and could afford an immense targetable surface area (~100 m2) for delivery of the inhaled therapeutic.
Pam2-ODN-enhanced survival of pneumonia consistently correlates with the generation of an antimicrobial environment, resulting in rapid induction of pathogen killing at the time of infection. As shown in Figures 1–5, lungs of Pam2-ODN treated mice harvested immediately after delivery of an infectious challenge demonstrate significantly lower pathogen burdens than lungs of sham treated mice. Whether the relatively modest differential between the initial pathogen burdens of Pam2-ODN treated and sham treated lungs fully accounts for the survival benefit is unknown, but it is suspected that this initial antimicrobial response is only one contributor to protection. Whereas these earliest antimicrobial effects may reflect release of preformed stores of effector molecules and/or activation of existing ROS generators, later effects may reflect transcriptionally regulated production of microbicidal molecules, modulation of host molecules that facilitate pathogen adherence or invasion, enhancements of mechanical barrier function and increased mucociliary clearance of pathogens and noxious debris. Ongoing pathogen killing, containment, and clearance are suggested by the dramatic widening of the pathogen differential in the lungs at later time points (Figure 5A), and the prevention of septicemia by Pam2-ODN treatment (Supplemental Table 2).
While we have demonstrated production of both antimicrobial peptides and ROS by the epithelium, the current studies do not attempt to ascertain which molecules are required for the antimicrobial response. However, our identification of a required cellular compartment is expected to facilitate the necessary studies to discover the critical effector molecules, particularly when integrated with novel mutant mouse models presently in development. We have reported SAA3 to be the most synergistically induced antimicrobial molecule in the lung following Pam2-ODN treatment. Previously, we reported that the inducible SAA proteins also comprised three of the four most upregulated transcripts following resistance-inducing treatment with inhaled bacterial lysates.11 Locally-produced SAA proteins have been reported to exert direct antimicrobial effects, to promote ROS generation, to facilitate the phagocytosis of certain bacteria, to promote the recruitment and activation of myeloid cells, and to polarize Th17 immune responses.48–51 Consequently, lung epithelial induction of SAA3 is an attractive target for therapeutic manipulation and may be an important contributor to Pam2-ODN-induced protection.
Together, these data provide critical insights into the mechanisms of inducible resistance. By establishing the central role of lung epithelial cells in the antimicrobial response, these data provide an opportunity to develop more accurate models to explore the means by which the lungs’ inherent defenses can be exploited to kill pathogens. More urgently, these data provide hope that we can utilize this technology to protect our patients during periods of peak vulnerability.
MATERIALS AND METHODS
Animals and reagents
All general reagents were obtained from Sigma-Aldrich (St. Louis, MO), except as indicated. All mice were handled in accordance with the Institutional Animal Care and Use Committee of The University of Texas MD Anderson Cancer Center. Mouse experiments were performed with 5–8 week old mice. Unless indicated, C57BL/6J mice (The Jackson Laboratory, Bar Harbor, ME) were used. To eliminate intergroup variability, all mice in each experiment were of a single gender. Rag1−/−, CD11c-DTR, and Perf1−/− mice were purchased from Jackson. Myd88−/− mice52 were provided by Shizuo Akira. Irak4−/− mice53 were provided by Wen-Chen Yeh (Amgen, Thousand Oaks, CA). Il22−/− mice54 were provided by Wenjun Ouyang (Genentech, South San Francisco, CA). Mice with LoxP sites flanking exon 3 of Myd8855 were provided by Anthony L. DeFranco. Sftpc-Cre mice56 were provided by Brigid L. M. Hogan.
Aerosol treatments
S-[2,3-bis(palmitoyloxy)-propyl]-(R)-cysteinyl-(lysyl) 3-lysine (Pam2CSK4) and ODN M362 (InvivoGen, San Diego, CA) were reconstituted in endotoxin-free water and suspended in sterile PBS. As described,15 The Pam2-ODN was placed in an Aerotech II nebulizer (Biodex Medical Systems, Shirley, NY) driven by 10 l/min air supplemented with 5% CO2 for 20 min. The nebulizer was connected by polyethylene tubing to a polyethylene exposure chamber.
Infection models
As described,10,11,13,15 mice were challenged inhalationally with bacterial inocula targeted to LD90-LD100. Frozen stock of Pseudomonas aeruginosa strain PA103 (American Type Culture Collection, Manassas, VA) was incubated for 16 h in 200 ml Luria-Bertani medium at 37 C in 5% CO2, then diluted in 1.5 l fresh broth, and grown at 37°C to an OD600 of 0.5, yielding 1–4 × 1010 CFU/ml. Frozen stock of a mouse-adapted clinical isolate of Streptococcus pneumonia serotype 4 was incubated for 16 h in 200 ml Todd-Hewitt broth at 37°C in 5% CO2, then diluted in 1.5 l fresh broth, and grown to an OD600 target of approximately 0.5, yielding 2–6 × 1011 CFU/ml. The bacterial suspensions were centrifuged, washed, resuspended in 10 ml PBS, and aerosolized over a period of 60 min in the exposure chamber. To determine lung pathogen burdens, mouse lungs were harvested under anesthesia immediately after infections and homogenized in 1 ml sterile PBS with 1 g of sterile glass beads using a Mini-Beadbeater-1 (Biospec, Bartlesville, OK). Serial dilutions of challenge inocula and lung homogenates were plated on tryptic soy agar (TSA) plates (Becton Dickinson), incubated at 37°C for 16 h, and bacterial CFUs were counted.
Frozen stock (2.8 × 107 TCID50/ml) of mouse adapted influenza A/Hong Kong/8/68 (H3N2; Mouse Lung Pool 1-17-12 provided by Brian E. Gilbert)57 was diluted 1:250 in 0.05% gelatin in Eagle’s minimal essential medium and aerosolized for 20 min to achieve LD90–LD100 (target 100 TDIC50/mouse). Viral concentrations in the nebulizer before and after aerosolization were determined by hemagglutination assay of infected MDCK cells.58
Leukocyte depletion models
Neutrophils were depleted by injecting 100 μl anti-Ly6G mAb (clone RB6-8C5) i.p. one day prior to Pam2-ODN treatment. Alveolar macrophages were depleted by intratracheal administration of 50 μl liposomal clodronate (0.25 g/ml, provided by Nico van Roojen) on days -3 and -2 prior to infection. Conventional dendritic cells and CD11c-expressing monocytes/macrophages were depleted in the lungs by administering 50 μl diphtheria toxin intranasally to CD11c-DTR mice on days -2 and -1 prior to infection. Plasmacytoid dendritic cells were depleted by injecting 100 μl anti-PDCA mAb (clone JF05-1C2.4.1, Miltenyi, Bergisch Gladbach, Germany) i.p. on days -2 and -1 prior to Pam2-ODN treatment. NK cells were depleted by injecting 100 μl anti-Nk1.1 mAb (clone PK136, Pierce Antibodies, Rockford, IL) i.p. on days -2 and -1 prior to Pam2-ODN treatment.
To confirm peripheral depletion of neutrophils, blood samples were obtained from the inferior vena cavae of anesthetized mice using 1 ml syringes containing sodium citrate. To confirm depletion of CD11c+ cells, plasmacytoid dendritic cells, and NK cells, mouse lungs were harvested, minced, and disaggregated with collagenase and DNase 1. Blood and lung samples were then treated with red blood cell lysis buffer prior to flow cytometry using a Becton Dickinson LSR II Laser Flow Cytometer. As described,10,11,59 For BAL cytology, fluid was obtained by instilling and collecting two aliquots of 1 ml each of PBS through a luer stub adapter cannula (Becton Dickinson) inserted through rings of the exposed trachea at indicated time points. Total leukocyte count was determined with a hemacytometer (Hauser Scientific, Horsham, PA), and differential count by cytocentrifugation of 300 μl of BAL fluid followed by Wright-Giemsa staining.
In vitro pathogen killing assays
To test pathogen killing by epithelial cells, mouse tracheal epithelial cells (mTEC) were isolated as described.60 Briefly, mouse tracheas were digested overnight with 0.15% pronase (Roche). Disaggregated cells were incubated in Ham’s F12/DMEM (Invitrogen) containing 4 mM glutamine (Invitrogen), 10 units penicillin-streptomycin, 0.25μg/ml amphotericin B (Fisher Scientific), and 50 μg/ml gentamicin (Fisher Scientific) at 37°C in 5% CO2 for 5 h. After incubation, floating cells were collected and 3.8 × 105 cells/well were plated on collagen I/III coated 24-well tissue culture plates in Ham’s F12/DMEM containing 5% heated inactivated FCS, 4mM glutamine, 10 units penicillin-streptomycin, 0.25 μg/ml amphotericin B, 50 μg/ml gentamicin, 10 μg/ml insulin, 30 μg/ml bovine pituitary extract (Lonza), 5 μg/ml human transferrin (Fisher Scientific), 0.1 μg/ml cholera toxin, 25 ng/ml epidermal growth factor (Fisher Scientific) and 10−8 M retinoic acid. The cells were then incubated at 37°C in 5% CO2 for 3–4 days until confluent. To test killing by human epithelial cells, HBEC3-KT cells40 (provided by John Minna) were grown in monolayer to ~80% confluence in Keratinocyte-SFM media (Invitrogen) containing bovine pituitary extract, epidermal growth factor and 1% penicillin-streptomycin.
Epithelial cells were treated with 20 μl PBS or 20 μl of ODN M362 (20 μg/ml) and Pam2CSK4 (10 μg/ml) in antibiotic-free mTEC culture media. Four hours later, the wells were infected with 150 CFU luminescent S. pneumoniae (provided by Jon McCullers). Culture luminescence was measured after infection by a Synergy 2 plate reader (Biotek, Winooski, VT).
Gene expression analysis
For in vitro analyses, MLE-15 cells were and grown in monolayer to approximately 80% confluence, the designated treatments were added to the culture media for 4 h, and the cells were collected by scraping. For in vivo analyses, wild type mice were exposed by aerosol to the designated treatments, then euthanized after 4 h. The lungs were sterilely-resected and mechanically homogenized. Total RNA was isolated using RNeasy Mini kit (QIAGEN). cRNA was then synthesized and amplified using Ilumina TotalPrep RNA amplification kits (Ambion), labeled and hybridized onto Illumina Mouse Ref-8 v 2.0 Expression BeadChips, then scanned on an Illunima iScan. mRNA and cRNA quality was confirmed using an Agilent 2100 Bioanalyzer. Consistent with minimum information about a microarray experiment (MIAME) standards, all primary microarray data were deposited at the NCBI Gene Expression Omnibus (GEO) (http://www.ncbi.nlm.nih.gov/geo/, GEO Accession GSE26864, in vitro, and GSE28994, in vivo). Primary signal intensity was normalized between and within samples, and differentially expressed genes were identified based on signal change and inter-sample variation.
Statistical analysis
Statistical analysis was performed using SPSS v19 (SAS Institute). Student’s t-test was used to compare the lung bacterial burdens between groups. Error bars shown in all figures represent technical replicates within the displayed experiment, rather than aggregation of experimental replicates. Percentage of mice surviving pathogen challenges was compared using Fisher’s exact test on the final day of observation, and the log-rank test was used to compare the survival distribution estimated by the Kaplan-Meier method. One-way ANOVA with Dunnett’s post hoc test was used to compare the BAL fluid differential counts.
Gene expression data were background corrected using the robust microarray averaging (RMA) method, then transformed by taking the base-two logarithm, and quantile normalized. Analysis of the microarray output was performed using a gene-by-gene class comparison ANOVA to identify treatment-induced changes. To adjust for multiple testing, we used a beta-uniform mixture (BUM) model to estimate the false discovery rate (FDR). Tukey honestly significant difference (HSD) test was used to compare the differences between each pair of means with appropriate adjustment for multiple testing on the level of individual genes.
Serum Amyloid A3 ELISA
ELISA kits for measuring mouse SAA3 were from Millipore (Billerica, MA). All assays were performed in duplicate according to manufacturer’s instructions. Reported concentrations are in ng/ml from undiluted BALF samples (PBS and ODN) or from BALF samples diluted 1:10 in assay buffer (Pam2 and Pam2-ODN).
Supplementary Material
1-2
Supplemental Table 1. Differentially expressed genes shown in Figure 6.
mRNA was harvested from C56BL/6 mouse lung homogenates (“Lung”) or from MLE-15 cells (“Cell”) 4 h after treatment with Pam2-ODN or PBS, then submitted to microarray analysis. Shown are fold change transcript levels comparing PBS-treated samples to Pam2-ODN-treated samples for the designated sample type. Tukey honestly significant difference (HSD) test was used to compare the differences between each pair of means with appropriate adjustments for multiple testing. A false discovery rate of <0.05 was used, and p value comparing means of PBS-treated to Pam2-ODN-treated samples was <0.0006 for all reported transcripts.
Supplemental Table 2. Time course of pathogen burden.
Mice were treated by aerosol with PBS (sham) or Pam2-ODN 24 h prior to infection with P. aeruginosa. The lungs, spleens and livers of infected mice were harvested under sterile conditions at designated time points, homogenized in 1 ml sterile PBS, and submitted to serial dilution culture. Reported are CFU/ml. All PBS-treated mice died prior to the 48 h harvest. (n = 3–6 mice/condition)
Acknowledgments
This work is supported by NIH U01 AI82226, the MD Anderson Physician-Scientist Program, NIH P30 CA016672 Cancer Center Support Grant, and NIH P50 CA100632 Leukemia SPORE.
Footnotes
Conflict of Interest:
MJT and SEE are authors on a related United States patent application entitled “Stimulation of Innate Resistance of the Lungs to Infection with Synthetic Ligands.” MJT and SEE own stock in Pulmotect, Inc., which holds the commercial options on these patent disclosures. The other authors declare no financial conflicts of interest.
References
Full text links
Read article at publisher's site: https://doi.org/10.1038/mi.2013.26
Read article for free, from open access legal sources, via Unpaywall:
http://www.mucosalimmunology.org/article/S193302192201025X/pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1038/mi.2013.26
Article citations
Is There a Role for Immunostimulant Bacterial Lysates in the Management of Respiratory Tract Infection?
Biomolecules, 14(10):1249, 02 Oct 2024
Cited by: 0 articles | PMID: 39456182 | PMCID: PMC11505618
Review Free full text in Europe PMC
The aging lung: microenvironment, mechanisms, and diseases.
Front Immunol, 15:1383503, 02 May 2024
Cited by: 1 article | PMID: 38756780 | PMCID: PMC11096524
Review Free full text in Europe PMC
Effect of epithelial-specific MyD88 signaling pathway on airway inflammatory response to organic dust exposure.
J Immunotoxicol, 20(1):2148782, 01 Dec 2023
Cited by: 1 article | PMID: 36538286
Antimicrobial mitochondrial reactive oxygen species induction by lung epithelial immunometabolic modulation.
PLoS Pathog, 19(9):e1011138, 11 Sep 2023
Cited by: 0 articles | PMID: 37695784 | PMCID: PMC10522048
Redox-Dependent Activation of Lung Epithelial STAT3 Is Required for Inducible Protection against Bacterial Pneumonia.
Am J Respir Cell Mol Biol, 68(6):679-688, 01 Jun 2023
Cited by: 1 article | PMID: 36826841 | PMCID: PMC10257071
Go to all (54) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
GEO - Gene Expression Omnibus (2)
- (1 citation) GEO - GSE28994
- (1 citation) GEO - GSE26864
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Inducible Lung Epithelial Resistance Requires Multisource Reactive Oxygen Species Generation To Protect against Viral Infections.
mBio, 9(3):e00696-18, 15 May 2018
Cited by: 24 articles | PMID: 29764948 | PMCID: PMC5954225
Inducible lung epithelial resistance requires multisource reactive oxygen species generation to protect against bacterial infections.
PLoS One, 14(2):e0208216, 22 Feb 2019
Cited by: 16 articles | PMID: 30794556 | PMCID: PMC6386317
Inducible epithelial resistance protects mice against leukemia-associated pneumonia.
Blood, 128(7):982-992, 17 Jun 2016
Cited by: 19 articles | PMID: 27317793 | PMCID: PMC4990857
Lung epithelial cells: therapeutically inducible effectors of antimicrobial defense.
Mucosal Immunol, 11(1):21-34, 16 Aug 2017
Cited by: 118 articles | PMID: 28812547 | PMCID: PMC5738267
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NCI NIH HHS (2)
Grant ID: P50 CA100632
Grant ID: P30 CA016672
NHLBI NIH HHS (3)
Grant ID: DP2 HL123229
Grant ID: R01 HL107291
Grant ID: R01 HL117976
NIAID NIH HHS (3)
Grant ID: R01 AI020624
Grant ID: U01 AI82226
Grant ID: U01 AI082226





