Abstract
Background
Various treatment modalities including non-invasive methods such as chemical peels, topical retinoids, microdermabrasion, minimally invasive techniques such as microneedling, fractional lasers, microneedling radiofrequency devices and invasive procedures such as acne scar surgeries and ablative lasers are used for acne scars, each with its own unique advantages and disadvantages. This study is a retrospective assessment of efficacy and safety of microneedling fractional radiofrequency in the treatment of acne scars.Methods
Thirty one patients of skin types III-V with moderate and severe facial acne scarring received four sequential fractional radiofrequency treatments over a period of 6 months with an interval of 6 weeks between each session. Goodman & Baron's acne scar grading system was used for assessment by a side by side comparison of preoperative and post- operative photographs taken at their first visit and at the end of 3 months after the last session.Results
Estimation of improvement with Goodman and Baron's Global Acne Scarring System showed that by qualitative assessment of 31 patients with grade 3 and grade 4 acne scars, 80.64% showed improvement by 2 grades and 19.35% showed improvement by 1 grade. Quantitative assessment showed that 58% of the patients had moderate, 29% had minimal, 9% had good and 3% showed very good improvement. Adverse effects were limited to transient pain, erythema, edema and hyperpigmentation.Conclusion
Microneedling fractional radiofrequency is efficacious for the treatment of moderate and severe acne scars.Free full text

Evaluation of Microneedling Fractional Radiofrequency Device for Treatment of Acne Scars
Abstract
Background:
Various treatment modalities including non-invasive methods such as chemical peels, topical retinoids, microdermabrasion, minimally invasive techniques such as microneedling, fractional lasers, microneedling radiofrequency devices and invasive procedures such as acne scar surgeries and ablative lasers are used for acne scars, each with its own unique advantages and disadvantages. This study is a retrospective assessment of efficacy and safety of microneedling fractional radiofrequency in the treatment of acne scars.
Methods:
Thirty one patients of skin types III-V with moderate and severe facial acne scarring received four sequential fractional radiofrequency treatments over a period of 6 months with an interval of 6 weeks between each session. Goodman & Baron's acne scar grading system was used for assessment by a side by side comparison of preoperative and post- operative photographs taken at their first visit and at the end of 3 months after the last session.
Results:
Estimation of improvement with Goodman and Baron's Global Acne Scarring System showed that by qualitative assessment of 31 patients with grade 3 and grade 4 acne scars, 80.64% showed improvement by 2 grades and 19.35% showed improvement by 1 grade. Quantitative assessment showed that 58% of the patients had moderate, 29% had minimal, 9% had good and 3% showed very good improvement. Adverse effects were limited to transient pain, erythema, edema and hyperpigmentation.
Conclusion:
Microneedling fractional radiofrequency is efficacious for the treatment of moderate and severe acne scars.
INTRODUCTION
Post-acne scarring is a very distressing problem. Atrophic acne scars are dermal depressions commonly caused by destruction of collagen after inflammatory acne.[1] Many therapeutic measures such as chemical peeling, subcision, dermabrasion, fillers and punch techniques have been performed to improve acne scarring but with sub-optimal outcomes.[2,3,4,5,6] Ablative lasers such as Er:YAG lasers or CO2 lasers produce significant improvement at the cost of long recovery times and post-inflammatory hyperpigmentation.[7,8] Recently, newer techniques such as microneedling fractional radiofrequency (MFR) has been shown to be clinically efficient in managing acne scars without causing direct damage to the epidermis.[9]
MFR device works by creating radiofrequency thermal zones without epidermal injury. After damage to the reticular dermis, long-term dermal remodelling, neoelastogenesis, and neocollagenogenesis results in dermal thickening.[10]
MFR device was evaluated over a period of 1 year (Dec 2012 to Nov 2013) in 31 patients of skin type III–V with Grade 3 and 4 atrophic acne scars.
METHODS
A retrospective photographic analysis of 31 patients treated with MFR for facial atrophic acne scarring was done between November 2012 and December 2013. None of the patients had received any previous treatment for their acne scars. Patients were excluded if they had received treatment with any other lasers during treatment or follow-up period. Thirty-one patients (15 male and 16 female) met the inclusion criteria. The mean age was 27.2 years.
Patients had undergone four sessions of MFR treatment for their acne scars with an interval of 6 weeks between each session, since the time for collagen remodelling lasts around 4-6 weeks. Treatment regimen was individualised based on predominant scar type and scar depth. The procedure area was painted with povidone iodine and cleaned with rectified surgical spirit prior to the procedure.
Procedure was performed under topical anaesthesia or nerve blocks, using sterile precautions. Penetration depth was limited to 1.5 mm on forehead, temple areas and areas with bony prominences.
Patients with predominantly ice pick scars and mixed scarring were given a needle depth of 3.5 mm on the first pass, 2.5 mm on the 2nd pass and 1.5 mm on the 3rd pass with minimal or no overlapping.
Higher energy settings (35 W-40 W) at depths of 3.5 mm with successively lower energy levels (30 W-35 W, 25 W-30 W, respectively) were used at lower penetration depths to prevent epidermal coagulation.
Post-procedure pain was managed by oral non steroidal anti-inflammatory drugs (NSAIDs) for 2 to 5 days. Patients were advised strict sun protection along with re-epithelizing agents containing cyclopentasiloxane, cyclohexasiloxone and sodium hyaluronate.
Assessment of efficacy
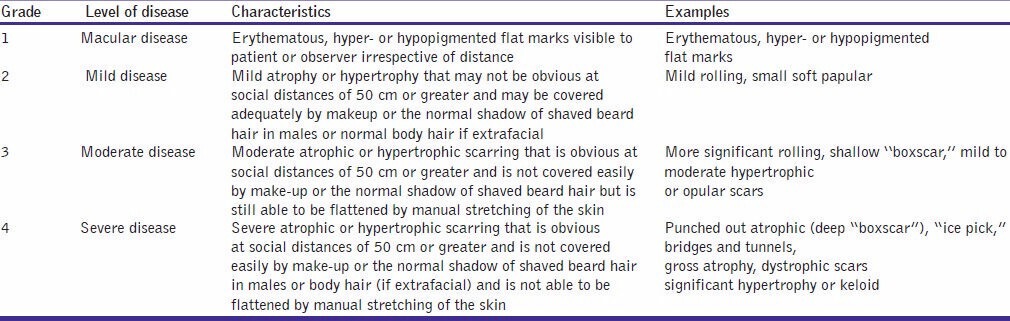
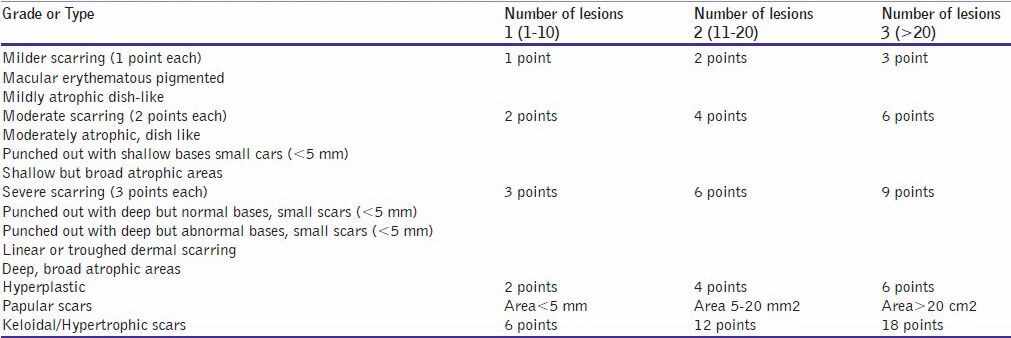
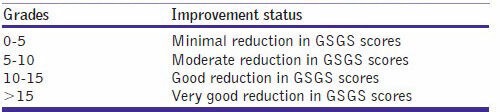
Objective assessment of Physician scores of improvement was determined by global acne scarring classification of Goodman & Baron [Tables [Tables11 and and2a2a and andbb].[11,12]
Table 2
(b) Assessment of improvement using Goodman and Baron's quantitative acne scar grading system
RESULTS
All patients completed the study, including the 3-month follow-ups. Most patients had mixed types of atrophic acne scars, including ice pick, boxcar and rolling scars. MFR was associated with substantial improvement in the appearance of all types of acne scars, which included the softening of scar contours as well as reduction in scar depth.
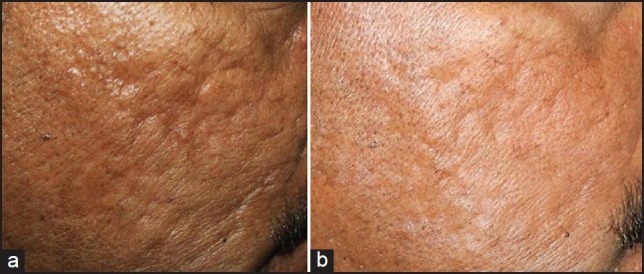
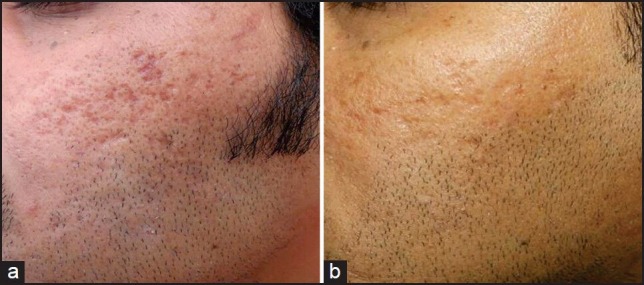
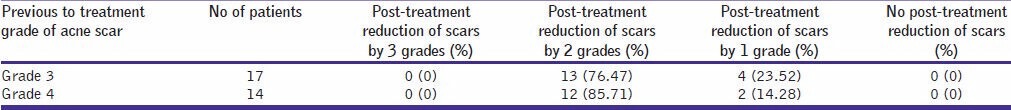
Estimation of improvement with Goodman and Baron's Global qualitative Acne Scarring System was done. Out of 31 patients who completed the treatment, 14 patients had Grade 4, 17 patients had Grade 3 before treatment. The physician's assessment of response to treatment based on Goodman and Baron Qualitative scar grading system is summarised in Table 3. In patients with Grade 4 scars, 12 patients (85.71%) showed improvement by 2 grades, i.e. their scars improved from Grade 4 to Grade 2 of Goodman and Baron scale [Figure 1a and andb].b]. Two patients (14.28%) with Grade 4 scars showed improvement by 1 grade with scars being obvious at social distances of 50 cm or greater. In 17 patients with Grade 3 scars, 13 patients (76.47%) improved by 2 grades [Figure 2a and andb]b] and 4 patients (23.52%) showed improvement by 1 grade [Figure 3a and andb].b]. Rolling and box scars showed better response than ice-pick scars.
Table 3
Physician assessment response based on Goodman and Baron's qualitative acne scar grading
Estimation of improvement with Goodman and Baron's Global quantitative Acne Scarring System showed that 58% of the patients had moderate improvement, 29% had minimal improvement, 9% had good improvement and 3% showed very good improvement [Figure 4].
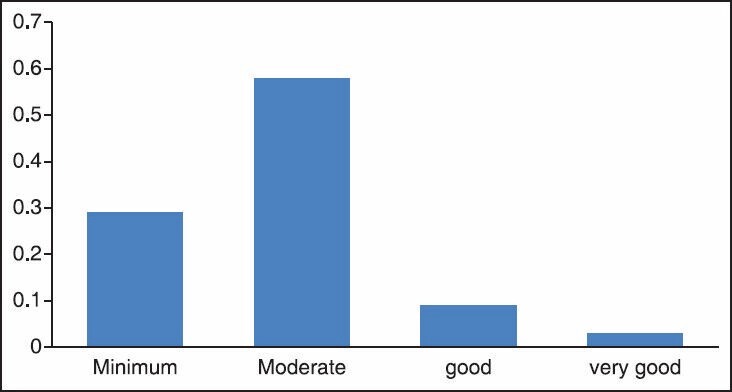
Bar graph representing improvement in acne scars by Goodman and Baron's quantitative acne scar grading system
The treatment was generally well tolerated. All patients underwent treatment-related pain. All patients had reported mild erythema for two days, two patients had oedema for more than three days, five patients reported post inflammatory hyperpigmentation and two patients had track marks of the device probe [Figure 5]. Social activity could commence as early as one day after treatment.
DISCUSSION
Acne scarring occurs subsequent to visible resolution of deep inflammation. Scarring may occur regardless of the severity of acne. Although acne scarring is likely to be associated more often with nodulocystic acne, it may occur in cases with only superficial forms of acne as well, especially when effective treatment is delayed.[13,14]
A study showed that approximately 16% of patients with acne seek proper treatment, and among those seeking such help, 74% wait greater than 12 months, 12% wait for 6 to 12 months, 6% wait for 6 months and only 7% wait for less than 3 months to be seen professionally for therapy of their acne.[15]
Atrophic acne scarring appears to be most common type associated with acne. The major clinical types of atrophic scars are ice pick, rolling or superficial and deep soft scars, and boxcar or depressed fibrotic scars. Although ablative and non-ablative laser skin resurfacing has greatly improved the treatment of atrophic acne scars, they are not without disadvantages.[14,16]
Ablative lasers such as CO2 and Er:YAG laser have efficacy of 25-90% for treatment of acne scars but are associated with erythema for more than 3 months, dyspigmentation and scarring.[17]
Non-ablative lasers such as 1064 nm Nd YAG and 1450 nm diode lasers have an efficacy of 40-50% after a series of treatments, with effect only on shallow box scars with no significant epidermal improvement.[17,18]
In contrast to ablative and non ablative lasers, treatment with the MFR device can be controlled by varying the depth.
Review of technology
A microneedling fractional radiofrequency (RF) device is available for commercial use (Lutronic corporation USA) with a maximum energy output of 50 W and capable of delivering energy in increments of 2.5 W in 20 equally graded energy level settings (Level 1-2.5 W to level 20-50 W).
The duration of each energy pulse can be set from 10 ms to 1,000 ms. A good control over the tissue damage can be achieved by changing the exposure time rather than altering the power level. Although the maximum power is higher than many other devices, the large range of exposure time enables the user to apply safe and consistent levels of coagulation in the dermis to achieve the desired effect. The energy delivery system consists of a disposable tip with 49 gold-plated needles. The entire length of the needle is insulated and it delivers bursts of RF energy through the tip. The depth of the needles can be adjusted from a minimum of 0.5 mm to a maximum of 3.5 mm.[19]
The ability to set multiple needle depths per pass is an advantage, allowing discrete electrothermal coagulation at different layers of the dermis. The insulated needles prevent electrothermal damage from occurring anywhere in the dermis but at the very tip of the needle and never in the epidermis.
The mechanisms involved are neo-collagenogenesis by needle penetration stimulating the release of growth factors and relative sparing of epidermis and adnexal structures which contribute to rapid healing.[19]
Ramesh et al. treated facial acne scars of 30 subjects with a matrix tunable radiofrequency device pretreated with oral antibiotics, topical tretinoin and subcision. The visual analog scale of improvement in scars ranged from 10-50% at end of 2 months to 20-70% at the end of 6 months.[20]
Despite these differences both studies show that fractional radiofrequency is both safe and effective for treatment of acne scars in skin types 3, 4 and 5.
Gold et al., conducted a study where in 13 patients with mild to moderate acne scars were treated with bipolar fractional radiofrequency and concluded that fractional bipolar radiofrequency is safe and an effective treatment for acne scars with 67-92% patients satisfied with the results.[9]
Cho et al. evaluated efficacy of fractional radiofrequency in treatment of 30 patients with mild to moderate acne scars and large facial pores. The grade of acne scars and investigator global assessment of large pores improved in more than 70% of the patients.[21]
The encouraging results prompted us to conduct retrospective analysis of efficacy and safety of MFR to treat atrophic acne scars in patients of Indian ethnicity, skin type 4 and 5.
Estimation of improvement with Goodman and Baron's Global qualitative Acne Scarring System showed that in 14 patients with Grade 4 scars, 85.71% showed improvement by 2 grades, 14.28% showed improvement by 1 grade. In 17 patients with Grade 3 scars, 76.47% improved by 2 grades and 23.52% showed improvement by 1 grade. Of the 31 patients with Grade 3 and Grade 4 acne scars, 80.64% showed improvement by 2 grades and 19.35% showed improvement by 1 grade. Rolling and box scars showed better response than ice-pick scars.
Estimation of improvement with Goodman and Baron's Global quantitative Acne Scarring System showed that 58% of the patients had moderate improvement, 29% had minimal improvement, 9% had good improvement and 3% showed very good improvement Hence, all 31 patients (100%) showed improvement in their scars with no failure rate.
The treatment was well tolerated with transient side effects such as mild erythema, post-inflammatory hyperpigmentation and track marks of the device.
CONCLUSION
MFR treatment can be considered as an effective modality of treatment for moderate to severe acne scars in patients with an added advantage of minimal downtime and effective improvement.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
Articles from Journal of Cutaneous and Aesthetic Surgery are provided here courtesy of Scientific Scholar
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.4103/0974-2077.138328
Article citations
Microneedling in Dermatology: A Comprehensive Review of Applications, Techniques, and Outcomes.
Cureus, 16(9):e70033, 23 Sep 2024
Cited by: 0 articles | PMID: 39449889 | PMCID: PMC11499218
Review Free full text in Europe PMC
Microneedling with Topical Insulin Versus Microneedling with Non-Cross-Linked Hyaluronic Acid for Atrophic Post-Acne Scars: A Split-Face Study.
Dermatol Pract Concept, 14(3), 01 Jul 2024
Cited by: 0 articles | PMID: 39122500 | PMCID: PMC11313770
Comparative study in treatment of acne scars fractional carbon dioxide laser versus micro needling fractional radio frequency - A retrospective study.
J Cutan Aesthet Surg, 17(3):214-218, 01 Jul 2024
Cited by: 0 articles | PMID: 39483656 | PMCID: PMC11494830
Energy-Based Devices for the Treatment of Facial Skin Conditions in Skin of Color.
J Clin Aesthet Dermatol, 17(6):22-32, 01 Jun 2024
Cited by: 0 articles | PMID: 38912197 | PMCID: PMC11189641
Review Free full text in Europe PMC
The Effects of Oral Isotretinoin on Atrophic Acne Scars Measured by Shear-wave Elastography: An Observational, Single-center Study.
J Clin Aesthet Dermatol, 16(9):46-51, 01 Sep 2023
Cited by: 0 articles | PMID: 37720196 | PMCID: PMC10503936
Go to all (30) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Successful Treatment of Facial Atrophic Acne Scars by Fractional Radiofrequency Microneedle in Vietnamese Patients.
Open Access Maced J Med Sci, 7(2):192-194, 17 Jan 2019
Cited by: 4 articles | PMID: 30745955 | PMCID: PMC6364741
An Innovative Approach of Treating Acne Scars Using Bipolar Rotational Stamping and Monopolar Criss-cross Technique with Insulated Microneedling Radiofrequency in Asians.
J Cutan Aesthet Surg, 14(2):191-202, 01 Apr 2021
Cited by: 1 article | PMID: 34566362 | PMCID: PMC8423198
Role of Microneedling in Atrophic Post-Acne Scars: An Experience from a Tertiary Care Hospital.
Cureus, 13(1):e12578, 08 Jan 2021
Cited by: 3 articles | PMID: 33575143 | PMCID: PMC7870110
Energy-based devices in the treatment of acne scars in skin of color.
J Cosmet Dermatol, 22(4):1177-1184, 27 Dec 2022
Cited by: 0 articles | PMID: 36575886
Review