Abstract
Aim
To evaluate our experience in endoscopic retrograde cholangio-pancreatography (ERCP) in terms of fulfilling the ASGE guidelines in indications, positive findings, and complications in the post-magnetic resonance cholangiopancreatography (MRCP) era.Methods
Between November 2001 and February 2003, consecutive ERCP cases were prospectively evaluated with regard to the indications, findings, cannulation techniques, devices used during the procedure, sedation given, duration of procedure, and complications. These data were entered in a database for subsequent processing and analysis.Results
Of 336 cases, 21.4% were diagnostic and 78.6% therapeutic ERCP. The indications for ERCP fulfilled the ASGE guidelines in 323 cases (96.1%). Suspected bile duct stone was the most frequent indication (26.8%), and this was followed by cholangitis (24.4%), dilated common bile duct (14.9%), and cholestatic jaundice (13.4%). Cannulation success rate was 94%. Biliary sphincterotomy was performed in 175 (52.1%) patients. Repeated ERCP was performed on 31.5% of the patients. Overall, the complication rate was 9.8% with 0.3% being procedure-related mortality. The complications were pancreatitis (5.4%), bleeding (0.8%), cholangitis (2.4%) and others (1.5%). No significant difference was observed between the complication rate and the type of ERCP performed.Conclusion
Our study showed that post-ERCP complication rate was comparable with the other large prospective studies and there was no difference in the complication between the diagnostic and therapeutic ERCP.Free full text

Complications of endoscopic retrograde cholangiography in the post-MRCP era: A tertiary center experience
Abstract
AIM: To evaluate our experience in endoscopic retrograde cholangio-pancreatography (ERCP) in terms of fulfilling the ASGE guidelines in indications, positive findings, and complications in the post-magnetic resonance cholangiopancreatography (MRCP) era.
METHODS: Between November 2001 and February 2003, consecutive ERCP cases were prospectively evaluated with regard to the indications, findings, cannulation techniques, devices used during the procedure, sedation given, duration of procedure, and complications. These data were entered in a database for subsequent processing and analysis.
RESULTS: Of 336 cases, 21.4% were diagnostic and 78.6% therapeutic ERCP. The indications for ERCP fulfilled the ASGE guidelines in 323 cases (96.1%). Suspected bile duct stone was the most frequent indication (26.8%), and this was followed by cholangitis (24.4%), dilated common bile duct (14.9%), and cholestatic jaundice (13.4%). Cannulation success rate was 94%. Biliary sphincterotomy was performed in 175 (52.1%) patients. Repeated ERCP was performed on 31.5% of the patients. Overall, the complication rate was 9.8% with 0.3% being procedure-related mortality. The complications were pancreatitis (5.4%), bleeding (0.8%), cholangitis (2.4%) and others (1.5%). No significant difference was observed between the complication rate and the type of ERCP performed.
CONCLUSION: Our study showed that post-ERCP complication rate was comparable with the other large prospective studies and there was no difference in the complication between the diagnostic and therapeutic ERCP.
INTRODUCTION
Endoscopic retrograde cholangio-pancreatography (ERCP) is the most complex endoscopic procedure. It is the preferred treatment for the majority of pancreatico-biliary diseases. Since its introduction in 1968[1], ERCP has evolved from a purely diagnostic to a therapeutic procedure because noninvasive imaging techniques such as magnetic resonance cholangio-pancreatography (MRCP) is increasingly being used for the diagnosis of conditions, otherwise previously diagnosed only by ERCP. Endobiliary sphincterotomy (ES) has become a common procedure in the era of endoscopic management of biliary and pancreatic diseases. However, these procedures carry certain mortality and morbidity[2-5] with acute pancreatitis, being the most common complication. The purpose of this study was to evaluate our experience in ERCP in terms of fulfilling acceptable ASGE guidelines[6] in indications, positive findings, and complications in the post-MRCP era.
MATERIALS AND METHODS
Study population
A prospective study was conducted at the National University Hospital, Singapore from November 2001 to February 2003. A total of 336 consecutive ERCPs were performed during the study period. All patients signed an informed consent for the procedures, after receiving an explanation on the risks, benefits and alternatives of ERCP and associated therapeutic procedures. Patients were given topical pharyngeal spray with 10% lignocaine spray, and sedated with midazolam and pethidine or fentanyl. All procedures were performed by Olympus duodenoscope JF200 or JF 240. Prophylactic antibiotics were routinely given to all patients.
Data on patients’ characteristics, ERCP indications and findings, cannulation techniques, devices used during the procedure, sedation given, duration of procedure and complications were collected prospectively during the procedure, recovery period and hospitalization. These data were entered in a database for subsequent processing and analysis.
ERCP complications
Post-ERCP complications were defined as any adverse effect related to the ERCP that prolonged hospitalization or required readmission for previously discharged patients. The complications were defined according to the previously published criteria[6]. Acute pancreatitis was defined as a new onset of abdominal pain with a rise in the level of amylase at least three times the upper limit of normal at more than 24 h after the procedure, requiring more than one night of hospitalization. Bleeding was defined as a clinical evidence of hemorrhage with decrease in hemoglobin greater than 2 g/dL or the need for a blood transfusion. Cholangitis was defined as a fever greater than 38 °C for more than 24 h that was thought to have biliary causes. Additional procedure-interrupting events such as hypoxia (decrease in oxygen saturation to below 90% for 2 min), duodenal tear and bradycardia (decrease in heart rate to less than 50 beats per minute for 2 min) were considered as post-ERCP complications. Any intensive care unit admission after procedure was graded as a severe complication.
ERCP was defined as therapeutic, where endoscopic sphincterotomy, precut, drainage, stricture dilatation, stent exchange, sphincter of Oddi manometry or biliary stone removal had been performed singularly or in combination.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Science (SPSS) version 10.0[9]. Comparison of diagnostic and therapeutic ERCP complications were evaluated using the χ2- or Fisher’s exact test. All tests of significance were two-tailed and a P value <0.05 was considered significant.
RESULTS
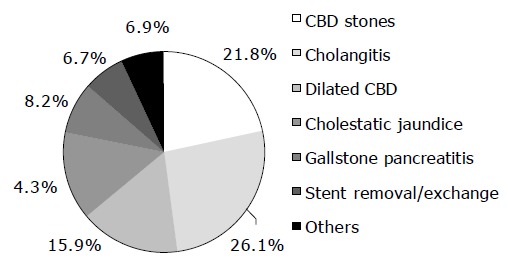
A total of 336 ERCPs were performed during the study period. Median age of the patients was 65 years (range 17-93 years). There were an equal number of males and females (167 men and 169 women). The ethnic distribution was Chinese in 78.3%, Malay in 11.3%, Indian in 5.7% and others in 4.8%. Indications of ERCP were suspected choledocholithiasis (26.8%), cholangitis (24.4%), dilated common bile duct (14.9%), cholestatic jaundice (13.4%), gallstone pancreatitis (7.7%), stent-related problems (6.3%) and others (6.5%, Figure Figure1).1). These indications fulfilled ASGE guidelines in 323 (96.1%) patients.
One hundred and seventy-three (51.5%) patients had co-morbidity such as diabetes mellitus with renal impairment, ischemic heart disease, heart failure, old stroke, atrial fibrillation, chronic renal failure and others. Twenty-seven (8%) patients were on anticoagulation or antiplatelet drugs for their underlying diseases. Anesthetist assistance (general anesthesia) was required in 8 patients (2.4%), whereas the endoscopic team assisted in sedation for all the remaining patients. Midazolam (dose 0.5-10 mg) was used in 97.6%, pethidine (dose 7-125 mg) in 97% and fentanyl (dose 20-75 μg) in 0.6% of all patients. Prophylactic antibiotics were routinely given to all patients.
ERCP failed in 20 patients (6%) because of unsuccessful cannulation and/or suboptimal ductal opacification whereas in 21 patients (6.3%), only shallow cannulation was achieved preventing further therapeutic procedure. Successful cannulation of the desired duct was obtained in 295 patients (87.7%).
Biliary sphincterotomy was performed in 175 patients (52.1%). Indications for sphincterotomy were common bile duct stones in 119 cases (68%), suspected passed biliary stone in 27 (15.4%), and biliary drainage in 11 (6.3%). Overall, therapeutic procedures were performed in 264 patients (78.6%). Sphincterotomy was the most common therapeutic procedure (66.5%) and this was followed by stenting (33.3%) and stone extraction (27.7%). Sphincter of Oddi manometry was performed in two (0.6%) patients (Table (Table11).
Table 1
Therapeutic procedure in 264 patients
| Type of procedure | n | % |
| Sphincterotomy alone | 40 | 11.9 |
| Sphincterotomy+stone extraction | 86 | 25.6 |
| Sphincterotomy+biliary stenting | 42 | 12.5 |
| Stricture dilatation±sphincterotomy | 3 | 0.9 |
| Nasobiliary drainage±sphincterotomy | 2 | 0.6 |
| Biliary stenting/stent removal alone | 73 | 21.7 |
| Stone extraction alone | 7 | 2.1 |
| Dilatation and stenting | 5 | 1.5 |
| SOD manometry | 2 | 0.6 |
| Biopsy/cytology | 4 | 1.2 |
Of 336 patients undergoing ERCP, 33 complications (9.8%) were reported (Table (Table2).2). Eighteen cases were immediate and 16 cases were delayed complications. Post-ERCP pancreatitis was the most frequent complication and occurred in 18 patients (5.4%). Pancreatitis was mild in 15 patients (4.5%), moderate in 2 patients (0.6%) and severe in 1 patient (0.3%). Bleeding occurred in three patients (0.8%); two bled immediately after sphincterotomy (mild hemorrhage) and one had delayed hemorrhage (moderate hemorrhage), after dilatation and biopsy of malignant biliary stricture. All three of them were successfully treated with endoscopic therapy and only one required blood transfusion. Cholangitis occurred in eight patients (2.4%); mild cholangitis in four patients, moderate in three patients and severe in one patient. The cholangitis occurred after plastic stenting for biliary stricture or stones in three patients, after biliary stone extraction in another three, after biopsy of biliary stricture in one, and after diagnostic ERCP in the other. One patient had a duodenal tear (0.3%) sustained during intubation of a Bilroth 2 anatomy, one (0.3%) developed choledocho-duodenal fistula due to forceful cannulation, one (0.3%) had subcapsular liver perforation due to vigorous biliary stenting, one (0.3%) desaturated during the procedure, and one (0.3%) developed bradycardia. These patients were treated conservatively and recovered well with no ill sequelae. Six (1.8%) patients died within 1 mo of the procedure, but only one was deemed procedure-related (0.3%). This post-ERCP death was due to severe cholangitis 2 d after sphincterotomy and stone extraction for biliary stones. Four died of underlying severe cholangitis on presentation and one died of cardiac arrest 8 d after the procedure. No significant difference was observed between the complication rate and the type of ERCP performed (Table (Table22).
Table 2
Major complications in 336 patients: comparison between diagnostic and therapeutic ERCP
| Complication | Diagnostic ERCP | Therapeutic ERCP | P |
| n = 72 (%) | n = 264 (%) | ||
| Pancreatitis | 5 (6.9) | 13 (4.9) | 0.5 |
| Cholangitis | 1 (1.4) | 8 (3) | 0.53 |
| Hemorrhage | 0 | 3 (1.1) | 0.36 |
| Other complications | 2 (2.8) | 3 (1.1) | 0.31 |
| Total | 8 (11.1) | 26 (9.8) | 0.68 |
DISCUSSION
In recent years, ERCP had evolved from a purely diagnostic to a therapeutic procedure with the introduction of non-invasive investigative tools such as MRCP. Most of the ERCP procedures in the present series, were therapeutic (78.6%) compared to earlier studies[7-9] in which therapeutic ERCP only comprised 40-55% of the total number of procedures. The post-ERCP complication rate in the present series was no different compared to other studies[9-13]. The overall complication rate was 9.8%. There was no significant difference in the complication rate between diagnostic and therapeutic ERCP. This finding is consistent with that of a retrospective US survey by Male et al[14], but was in contrast with those from a British survey[15] and an Italian study[16] in which therapeutic ERCP was associated with three- to four-fold higher complication rates.
The reported incidences of post-ERCP pancreatitis ranged 0-40%[17] but were commonly quoted as 2-7%[10,18,19]. The variation is likely due to the difference in definition of pancreatitis, method of data collection and indications for ERCP. In the present study, acute pancreatitis was the most common complication (5.4% of patients) and most cases were mild. This finding is comparable with those of two recently published large prospective studies by Freeman et al[10], and Loperfido et al[16]. In the former study, which only considered therapeutic procedure, the overall complication rate was 9.8%. Procedure-related pancreatitis occurred in 5.4% of patients; mild in 2.3%, moderate in 2.8% and severe in 0.4%. In the latter survey which also included diagnostic procedure (one-third of procedures), reported major complication rate was 4%, and pancreatitis (moderate and severe only) occurred in 1.3%. The risk of pancreatitis was similar for diagnostic and therapeutic ERCP in our study. This is similar to the finding from a prospective study from Boston[9] even though some studies[20,21] reported higher pancreatitis complication rates in therapeutic ERCP. Risk factors of procedure-related pancreatitis identified were factors related to patients characteristics such as younger age[10,16,22], suspected dysfunction of sphincter of Oddi[10], history of ERCP-related pancreatitis[9], recurrent pancreatitis[9] and factors related to endoscopic technique such as pancreatic duct opacification[16,19], small bile duct[16,23], multiple cannulation attempt[9] or difficult cannulation[10], development of abdominal pain during the procedure[9], precut sphincterotomy[10,22] and pancreatic duct brushing for cytology[9]. ERCP-induced pancreatitis remains an important clinical problem even in diagnostic ERCP.
Incidence of post-ERCP hemorrhage varies between 0.65% and 4% in earlier retrospective studies[24,25]. In our study, procedure-related hemorrhage was only 0.8%. This low figure is similar to those from a few large prospective studies[9,10,16,22]. Cholangitis is an uncommon complication in ERCP, ranged 0.5-1.1%[9,10,16,22]. However, cholangitis seems to be slightly higher (2.3%) in our study, even though routine antibiotics were given before starting the procedure. Three patients with cholangitis had stent migration after plastic stenting for biliary stricture or stones (one required repeat ERCP), three had cholangitis after biliary stone extraction (one had incomplete stone removal and required the ERCP repeat for stones clearance and one who had severe cholangitis subsequently died), one developed cholangitis after biopsy of biliary stricture and one after diagnostic ERCP. Most of the patients with cholangitis resolved after one course of antibiotics.
Our study showed that post-ERCP complication rate was comparable with those of other large prospective studies and there was no difference in the complication rates between the diagnostic and therapeutic ERCP. In line with the current post-MRCP, most of our ERCPs were therapeutic (78.6%). Future research should focus on developing clinical pathways to guide clinicians in selecting patients who should undergo ERCP or MRCP as the initial investigation and those who would benefit from MRCP followed by ERCP.
Footnotes
Science Editor Li WZ Language Editor Elsevier HK
References
Articles from World Journal of Gastroenterology are provided here courtesy of Baishideng Publishing Group Inc
Full text links
Read article at publisher's site: https://doi.org/10.3748/wjg.v11.i33.5209
Free to read at www.wjgnet.com
http://www.wjgnet.com/downpdf.asp?url=/1007-9327/11/5209
Free to read at www.wjgnet.com
http://www.wjgnet.com/abstract.asp?url=/1007-9327/11/5209
Free to read at www.wjgnet.com
http://www.wjgnet.com/1007-9327/11/5209.asp
Citations & impact
Impact metrics
Citations of article over time
Article citations
Non-Invasive Prediction of Choledocholithiasis Using 1D Convolutional Neural Networks and Clinical Data.
Diagnostics (Basel), 14(12):1278, 17 Jun 2024
Cited by: 0 articles | PMID: 38928692
Evaluation of therapeutic efficacy, safety and economy of ERCP and LTCBDE in the treatment of common bile duct stones.
Front Physiol, 13:949452, 25 Aug 2022
Cited by: 0 articles | PMID: 36091409 | PMCID: PMC9452837
Oral effervescent agent improving magnetic resonance cholangiopancreatography.
Quant Imaging Med Surg, 12(9):4414-4423, 01 Sep 2022
Cited by: 1 article | PMID: 36060576 | PMCID: PMC9403601
A Novel Cause of Biliary Peritonitis after Endoscopic Retrograde Cholangiopancreatography: Case Report and Literature Review.
Case Rep Gastrointest Med, 2021:3814080, 21 Oct 2021
Cited by: 1 article | PMID: 34721910 | PMCID: PMC8553500
Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches.
World J Gastroenterol, 27(28):4536-4554, 01 Jul 2021
Cited by: 43 articles | PMID: 34366622 | PMCID: PMC8326257
Review Free full text in Europe PMC
Go to all (35) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Surgeon-performed endoscopic retrograde cholangiopancreatography. Outcomes of 2392 procedures at two tertiary care centers.
Surg Endosc, 32(6):2871-2876, 22 Dec 2017
Cited by: 9 articles | PMID: 29273876 | PMCID: PMC5957783
NIH state-of-the-science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy.
NIH Consens State Sci Statements, 19(1):1-26, 01 Jan 2002
Cited by: 41 articles | PMID: 14768653
Review
Efficacy of endoscopic nasobiliary drainage for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis and cholangitis after repeated clearance of common bile duct stones: experience from a Chinese center.
Dig Endosc, 25(4):453-458, 20 Dec 2012
Cited by: 10 articles | PMID: 23363031
Feasibility of endoscopic retrograde cholangiopancreatography-related procedures in hemodialysis patients.
J Gastroenterol Hepatol, 29(3):648-652, 01 Mar 2014
Cited by: 18 articles | PMID: 23869844