Abstract
Free full text

Towards optimal design of cancer nanomedicines: Multi-stage nanoparticles for the treatment of solid tumors
Abstract
Conventional drug delivery systems for solid tumors are composed of a nano-carrier that releases its therapeutic load. These two-stage nanoparticles utilize the Enhanced Permeability and Retention (EPR) effect to enable preferential delivery to tumor tissue. However, the size-dependency of the EPR, the limited penetration of nanoparticles into the tumor as well as the rapid binding of the particles or the released cytotoxic agents to cancer cells and stromal components inhibit the uniform distribution of the drug and the efficacy of the treatment. Here, we employ mathematical modeling to study the effect of particle size, drug release rate and binding affinity on the distribution and efficacy of nanoparticles to derive optimal design rules. Furthermore, we introduce a new multistage delivery system. The system consists of a 20-nm primary nanoparticle, which releases 5-nm secondary particles, which in turn release the chemotherapeutic drug We found that tuning the drug release kinetics and binding affinities leads to improved delivery of the drug. Our results also indicate that multi-stage nanoparticles are superior over two-stage nano-carriers provided they have a faster drug release rate and for high binding affinity drugs. Furthermore, our results suggest that smaller nanoparticles achieve better treatment outcome.
Introduction
To eradicate cancer cells, nanoparticle formulations have first to reach the tumor site through the tumor blood vessels and extravasate from the relatively leaky regions of the tumor vasculature into the tumor microenvironment. Subsequently, nanoparticles release their drug in many cases in a controlled fashion while they stay put at the perivascular space or to some extent travel in the interior of the tumor. Drug molecules diffuse into the tumor a little further and can bind to cancer cells and/or components of the tumor microenvironment. Finally, they get internalized by cells. The successful delivery of the drug depends in large part on the amount of nanoparticles that reaches the tumor, the ability of the nanoparticles to penetrate deep into the tissue to achieve uniform distribution and the release kinetic and binding affinity of the drug 11.
Parameters of the tumor microenvironment that inhibit the delivery of nanoparticles into the tumor include the size-dependency of the transport both across the tumor vessel wall and then through the tumor interstitial space 4-6, 11. Transport across the tumor vessel wall is determined by the relative size of the particle compared to the size of the pores of the vessel wall. We have calculated with the use of mathematical modeling that nanoparticles larger than 60% of the pores of the vessel wall cannot extravasate due to steric and hydrodynamic interactions of the particle with the vessel wall 6. As a result, large nanoparticles can only extravasate from highly abnormal vessels with extremely large pores in the vessel wall. This might explain in some part why Doxil®, a 100 nm pegylated liposomal doxorubicin, has failed to treat pancreatic cancers, which have moderately leaky vessels 10. However, recently the new liposome MM-398, of approximately the same size as Doxil, did lead to a 1.9 months survival advantage in pancreatic cancers (http://investors.merrimackpharma.com/releasedetail.cfm?ReleaseID=844390). Therefore, not only the size but also other parameters, such as the drug release kinetics might play a crucial role in the outcome of the therapy 24, 30, 35.
Once through the vessel wall, the next step in delivery, interstitial transport, is determined by the relative size of the particle compared to the pores of the dense network of extracellular matrix. If the size of the particle is comparable to the size of the pores, the nanoparticle cannot penetrate into the tumor but it is concentrated in the perivascular regions of the leaky vessels 18, 34. Heterogeneous distribution of the nano-carriers results in heterogeneous release of the chemotherapy and despite the fact that chemotherapeutic agents should diffuse rapidly into the tumor interior owing to their small size, there is a competition between rapid diffusion and binding of the drug from nearby cancer cells 13, 24. Therefore, reduced and heterogeneous delivery of nano-carriers and high binding affinities to cancer cells and stromal components can hinder the uniform distribution of chemotherapy, reducing its tumoricidal potential 11,28.
In previous research, in order to optimize intratumoral distribution of nano-carriers, we developed a multi-stage nanoparticle delivery system that shrinks in size when it enters the tumor interstitial space 33. We synthesized 100-nm particles (similar in size to Doxil®) using gelatin that can extravasate from leaky tumor blood vessels and be exposed to the tumor microenvironment. The primary gelatin particle was then degraded by matrix metalloproteinases (MMP-2) that are over-expressed in the interior of many tumors and released secondary, 10-nm particles, which could contain therapeutic or diagnostic agents. The secondary particles penetrated deeper and more homogeneously into the tumor interstitial space than the primary particles, and thus, they were able to cover more effectively the large avascular regions of a tumor, providing better distribution. We tested this multi-stage delivery system in vivo in mice bearing tumors and proved their superior penetration into the tumor microenvironment compared with non-degradable particles of the same primary size. However, limited extravasation of 100-nm particles remains a cause for reduced delivery to tumors with poorly or moderately leaky vessels Recently, we found that the ideal nanoparticle size that optimizes transvascular transport (i.e., extravasation) to tumor tissue and at the same time prevents extravasation to normal tissues, is within the range of 12-20 nm 6. Therefore, a muti-stage delivery system with primary nanoparticles in this size range appears to be optimal.
In this work, we employ a mathematical model of fluid flow and drug delivery to solid tumors 26. We first investigate under what conditions our 100-nm multi-stage delivery system has better efficacy compared with conventional two-stage delivery systems composed of a same size primary particle and the drug. Subsequently, we repeat simulations for a 20-nm multi-stage delivery system that releases 5-nm secondary particles, which contain the chemotherapy. We compare this formulation with a 20-nm two-stage nanoparticle and derive conclusions about the effect of particle size, drug release rate and binding affinity on the efficacy of nanoparticles and provide design guidelines for both two-stage and multi-stage delivery systems.
Materials and Methods
The mathematical model builds on our previous work 26, 28 and involves coupling of fluid flow and nanoparticle transport in the vascular and interstitial spaces of the tumor as well as the controlled release of the drug and its binding and internalization by cancer cells. A 2-dimensional percolation network at the percolation threshold is employed to represent the chaotic, multi-scale heterogeneity of the tumor vasculature 1 (Supplementary Fig. 1 in the Supporting Material), but our methodology can be applied to any vascular geometry in 2 or 3-dimensions. Vascular flow is taken to be steady, laminar and axial as governed by Poiseuille's equation 19 (a detailed set of equations is presented at the Supporting Material). Fluid exchange between the vascular and interstitial space is calculated with the use of Starling's approximation for semipermeable membranes, and interstitial flow is governed by the solution of Darcy's law for flow through porous media 3. Transport of particles in the vascular network is assumed to be driven by convection only, transvascular flux was calculated by Starling's approximation and interstitial transport was determined by the solution of the convection-diffusion equation taking into account the release of the drug and of the secondary particle when applicable 3, 28. The equations for the transport of the different delivery systems are presented in the Supporting Material along with the model parameters employed in our analysis (Supplementary Table 1). We have successfully validated this model by comparison with in vivo data for the delivery of nanoparticles of different sizes in murine mammary carcinomas 6. Owing to the stochastic nature of percolation networks, we repeated the simulations for five random network realizations and the average values are presented.
We model three different delivery systems following bolus injection: i) a one-stage, chemotherapy system, ii) a conventional two-stage delivery system consisting of the nano-carrier and the chemotherapy, and iii) a multi-stage delivery system consisting of a primary nanoparticle, a secondary nanoparticle and the chemotherapy (Fig. 1). The chemotherapy in the first case or the nano-carrier in the other two cases is delivered to the tumor site through the tumor blood vessels, then they cross the tumor vessel wall and subsequently, they travel the remaining distance from the vessel wall to the cancer cells. For the two-stage and multi-stage systems, the nanoparticles release their payload once they enter the tumor interstitium and the free molecules of chemotherapy (drug) can bind to cell surface receptors, unbind or get internalized. The vascular transport of the drug or the nano-carrier is characterized by the blood half-life Kd, the release of the chemotherapy from the nano-carrier by the release rate constant Kel, whereas for the multi-stage system two release rate constants appear, Kel1 for the release of the secondary particle from the primary and Kel2 for the release of the chemotherapy from the secondary particle. To reduce the number of model parameters, we assume that the two release rate constants are the same, unless otherwise stated. Finally, the drug-cell interactions are described by the binding/unbinding rate constants Kon/Koff and the internalization rate constant, Kint (Fig. 1). It is also possible, the drug to be taken up by cancer cells without binding to cell surface receptors. In this case, we could simply ignore the binding/unbinding step. We calculate the intratumoral distribution of the drug, its amount that is taken up by cancer cells and the fraction of cells killed by the drug.

Schematic shows the three different delivery strategies considered in the study: chemotherapy alone (one-stage), conventional two-stage nanoparticle delivery system consisting of the nano-carrier and the drug and the new multi-stage nanoparticle delivery system consisting of the primary nano-carrier, the secondary nanoparticle and the drug.
We simulate a bolus injection and we adjust the concentration of the delivery systems at the inlet of the vasculature so that all three systems contain the same amount of chemotherapy. Therefore, the load capacity of the two-stage and multi-stage nanoparticles does not have any effect on our calculations. Parameters that affect drug delivery are: the size of the primary and secondary particles, their circulation time in the blood and their diffusivity in the tumor extravascular space, and the release kinetics of the drug and its binding affinity to cell surface receptors. Blood circulation time and interstitial diffusivity are determined based on the size of the particles and published experimental measurements 14, 16, 18, whereas the rate constant of drug release and the rate constant of binding are varied parametrically to create optimization contour plots The efficacy of the delivery strategies was quantified by calculating the fraction of cells killed following a methodology by El-Kareh and Secomb 9 and Eikenberry 8. According to this methodology the fraction of cells killed is related to the concentration of the chemotherapy that is taken up by the cells through a mathematical expression. We used an exponential decay function according to 8.
Selection of optimal release and binding rates can be guided by numerical solutions of the full model and by insights drawn from analytical solutions of a simplified one-dimensional model (see Supporting Material). Including effects of diffusion, convection and release and binding kinetics, we find that the concentrations of the nanoparticles and drug in free and bound forms decrease with distance from the vessel wall, x approximately as Aie−x/Li with each stage's characteristic length scale given by
where Di is the diffusivity of stage i, Ki is the stage's rate of release or binding and v is the interstitial fluid velocity away from the vessel. Convection by the interstitial fluid can aid (v > 0) or hinder (v < 0) distribution of the drug. In the absence of significant interstitial flow, the characteristic lengths simplify further to Li =(Di/Ki)0.5. Roughly speaking, the distance to which the drug penetrates beyond the vessel wall scales as the sum of the characteristic lengths from each stage with longer lengths generally providing more uniform drug distribution, but potentially at the cost of lower absolute concentrations of internalized drug when the multipliers Ai are taken into account.
Results
Large, 100-nm delivery systems have modest efficacy due to limited penetration into the tumor
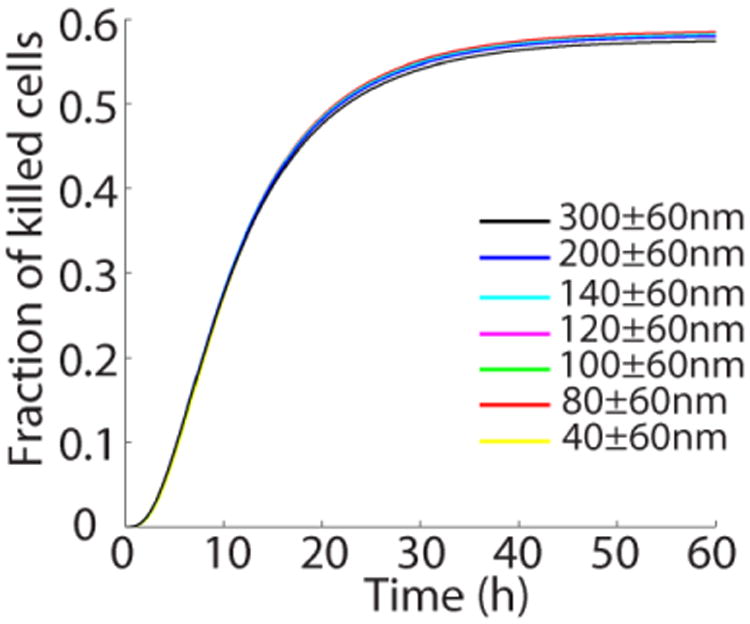
Contour plots of the 100-nm two-stage and multi-stage delivery systems are presented in Fig. 2. The concentration of the drug that is taken-up by cancer cells for the three different delivery scenarios is shown in Fig. 3A. Figure 3A suggests that the concentration of internalized drug is higher when chemotherapy is delivered directly, without the use of a nano-carrier. Because of its small size, the chemotherapy reaches the tumor in larger amounts and thus, it is internalized in larger concentrations 5, 17. However, improved internalization is not necessarily related to better distribution because drug molecules more effectively bind to cells in the vicinity of the tumor blood vessels preventing the drug from penetrating deep into the tumor tissue (Fig. 3B). As a result, two-stage and multi-stage systems can be more efficient than chemotherapy alone (Fig. 3C). Specifically, the optimization contour plots in Fig. 2 suggest that a two- stage system is more effective in a wider range of release kinetics than a multi-stage system, but the latter is superior for relatively high release rate constants and particularly for high binding affinities of the drug with the cells. In both cases, however, the efficacy of nanoparticles is modest. Furthermore, the efficacy depends strongly on the permeability of the vessels. In Fig. 4, the fraction of killed cells is presented as a function of time for different distributions of vessel wall pore sizes (mean ± standard deviation). Decreasing the size of the pores, the efficacy of both delivery systems reduces drastically as a result of the size-dependency of the transvascular transport.
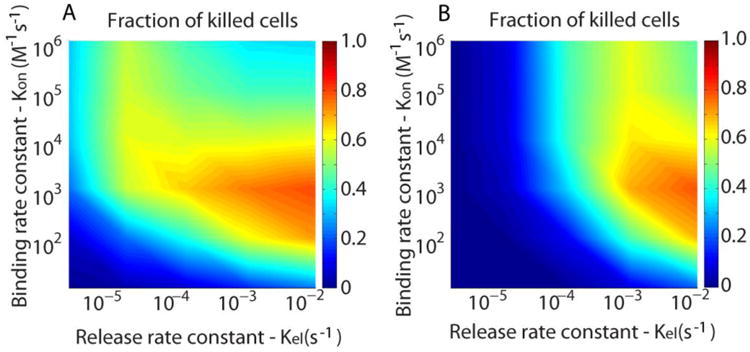
Optimization contour plots of the fraction of cells killed as a function of binding rate constant (Kon) and rate constant of release (Kel) for the two-stage (A) and multi-stage (B) 100 nm drug delivery systems. The blood half-life, Kd, was set to 10 h.
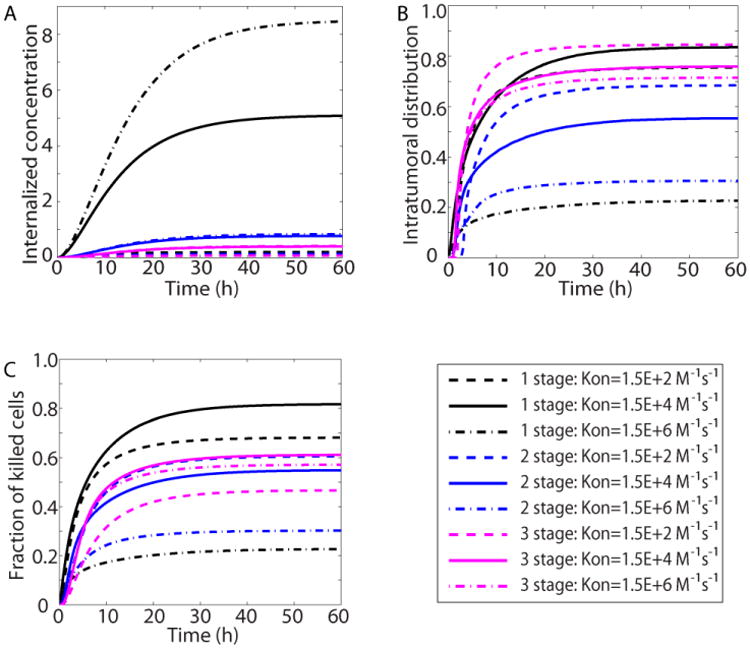
Comparison of the three delivery strategies. (A) intracellular (internalized) chemotherapy concentration as a function of time for chemotherapy alone (1 stage), the 100 nm two-stage delivery system (2 stage) and for the 100 nm multi-stage system (3 stage). (B) Intratumoral distribution of chemotherapy as a function of time, and (C) fraction of killed cells as a function of time. Three values of the binding rate constant Kon (M-1 s-1) were employed, whereas the rate constant of release, Kel was set to the physiologically relevant value of 1×10-3 s-1 based on experimental data. Concentration became dimensionless with division with the initial concentration at the entrance of the vascular network. Intratumoral distribution is the area fraction of the tumor where the drug has reached in concentrations above 5% of the concentration at the inlet of the vascular network.
Small, 20-nm multi-stage delivery systems optimize treatment efficacy for rapid release kinetics and high binding affinities
Optimization contour plots for the efficacy of a 20-nm multi-stage delivery system as well as a conventional two-stage system of the same primary size are presented in Figs. 5A&B. Comparison of Figures 1 and 5A&B shows that the smaller the particle, the more effective the treatment becomes. Additionally, Figs. 5A and 5B suggest that multi-stage systems are associated with a higher fraction of killed cells when the rate constant of release is suitably adjusted to relatively high values (See also Supplementary Figs. 2 and 3).
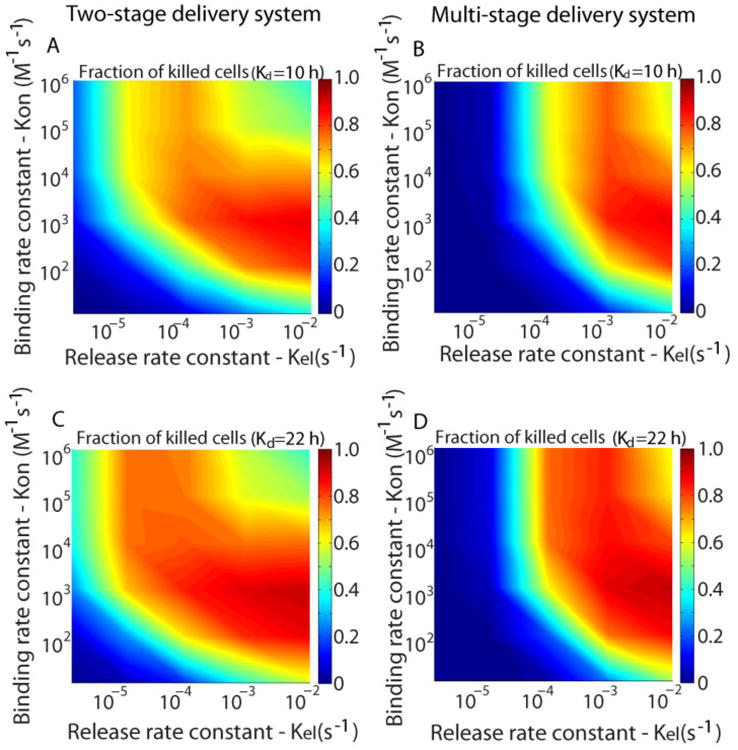
Optimization contour plots of the fraction of killed cells as a function of binding rate constant (Kon) and rate constant of release (Kel) for the 20 nm two-stage (A) and multi-stage (B) nanoparticles for blood half-life Kd=10 h. Results of the two-stage (C) and multi-stage (D) delivery systems for Kd=22h.
Apart from the release kinetics and binding affinity, another design parameter that can be modulated is the blood half-life of the particle. In our analysis thus far, we assumed 100- and 20-nm particles to have the same blood half-life but there is experimental evidence for a size-dependency. Particles less than 6 nm in size clear very fast from the blood stream 7. For larger particles blood half-life decreases as we move from 12-nm to 125-nm particles, provided the surface chemistry remains the same 14, 18. Therefore, a 20-nm particle is expected to circulate in the blood for a longer time compared with a 100-nm particle, which further improves the efficacy of smaller delivery systems. This is confirmed in Figs. 5C and 5D, which presents the efficacy of the 20-nm particles for a blood half-life value (Kd = 22 h), taken from the literature for particles of similar size (10).
Delivery of 20-nm multi-stage systems is independent from the permeability of tumor vessels
In normal tissues the size of the pores of the blood vessels is less than 12 nm in diameter 23. Therefore, nanoparticles with a size of 20 nm are not only large enough so that they will not extravasate to normal tissues but at the same time they can ensure unhindered transvascular flux into the tumor tissue due to the leakiness of the tumor vessels 27. As shown in Fig. 6, the efficacy of the 20-nm multi-stage delivery system is not affected by a decrease in the size of the pores of the vessel wall and thus, it is expected that it will be effective even for tumors with poorly permeable vessels, such as pancreatic cancers. This finds clinical confirmation in the case of nab-paclitaxel (a 125-nm particle that reduces rapidly to 10 nm in size following disintegration in the blood), which can improve the overall survival of pancreatic adenocarcinoma patients 31.
Discussion
Examination of the results reveals features that can guide design of nanomedicines. The combination of parameters that lead to the optimal kill of cancer cells achieves two goals. First, the free drug must be available to as much of the tumor volume as possible. Otherwise, uniform binding and ultimately internalization cannot occur. And second, the free drug must bind rapidly enough to avoid being carried out of the tumor before binding can occur. The first goal of maximizing the distance from the blood vessels that the free drug penetrates is achieved by maximizing the sum of the characteristic lengths (ΣLi), that is, matching low release rates and low binding rates with small, highly diffusive particles (i.e., large Li =(Di/Ki)0.5), however, a design based solely on maximizing depth of penetration for the free drug would be misguided. We note that the characteristic lengths are maximized when the release and binding rates tend to zero, which clearly does not allow any drug to be released or internalized. If instead, we focus on rapid release and internalization, we lose depth of penetration and uniformity of drug distribution. Clearly, a compromise between too rapid and too slow kinetics best balances the challenges of distribution and internalization.
To strike a balance between binding kinetics and penetration depth, we propose a new design of nanomedicines that can optimize the amount and distribution of the drug inside the tumor and the efficacy of the treatment. The essential characteristics of the new multi-stage drug delivery system are i) its relatively small primary size, on the order of 20 nm, which ensures effective extravasation even from vessels of poorly permeable tumors, ii) the relatively fast release of the secondary particle and of the drug, and iii) the penetration and uniform distribution of the secondary particles within the tumor. This new delivery system is expected to be effective in a wider range of binding affinities compared with conventional two-stage systems. In the two-stage systems rapid binding of the chemotherapy to cancer cells prevents their penetration and distribution into the tumor, causing effects limited to the vicinity of the blood vessels near the tumor periphery. In the multi-stage system, the addition of an intermediate stage between the primary particle and the chemotherapy delays the interactions of the drug with the cancer cells, whereas the release of the secondary, 5-nm particle that contains the chemotherapy permits the unhindered and rapid transfer of the drug deep into the tumor micro-environment. The size of both the primary and secondary particles is important, because the size of the primary determines the amount of the drug that extravasates into the tumor and the size of the secondary particle determines the penetration and uniform distribution of the drug.
We propose that 20 nm is an ideal size for drug delivery systems. Particles of this size still retain the EPR effect and thus, the selective delivery to tumor tissue and moreover, due to their relatively small size they can extravasate faster and penetrate deep into the tumor interstitial space. This finding is in agreement and confirms published experimental studies 6, 18. Despite the fact that small size might be associated with increased toxicity, current nanoparticle formulations of 20-30 nm size (e.g. CRLX101 and NC-6004) have already gone through a phase I clinical trial, showing low toxicity 17, 32. Therefore, in general particles of this size should not be considered to be toxic.
Two-stage nanoparticle formulations exist that are equipped with targeting ligands on their surface to specifically recognize cancer cells 12, 22. In Supplementary Fig. 4, we repeated the simulations to account for nanoparticle binding. The results suggest that binding of the nanoparticle to cancer cells does not improve significantly the survival benefit, in accordance with published experimental studies 15. Our results suggest that nanoparticle binding is beneficial when a high binding affinity of the nanoparticle is combined with a slow release of the chemotherapy. Furthermore, it is also possible the nanoparticle to be taken up by the cells and then to release its drug. Our model can be easily modified to account for such cases by replacing binding with the internalization step. In this case, however, the main conclusion of this study is not affected, i.e., without binding, high internalization rates will still pose a barrier to the penetration and uniform distribution of the nano-carrier and the characteristic penetration length will still be given by Eq. 1 as before. It is also possible, the drug to be taken up by cancer cells without binding to cell surface receptors. Our modeling framework is general, and in this case, the binding step can be omitted allowing the drug to be internalized with a rate constant, Kint. Again, the main conclusion described by Eq. 1 does not change and ignoring convection the characteristic penetration length will be scaled as L = (D/Kint)0.5.Another model limitation is that our analysis did not account for release of the drug in the vascular network. Even though nanoparticles can selectively accumulate in the tumor tissue due to their relatively large size and the EPR effect, release of the drug in the vasculature causes severe adverse effects10. Therefore, nanoparticle delivery systems must be designed to release their therapeutic load after they have entered the tumor tissue. This can be achieved with stimuli-responsive nanoparticles, where drug release is triggered by a property of the tumor microenvironment (e.g. pH or enzyme responsive particles) or by external stimuli (e.g. magnetic field, ultrasound, heat or light). In our manuscript, since drug-loaded secondary nanoparticles are protected by the primary nanoparticles, drug release of multi-stage particles in the vascular space is considered minimum. Drug release in the vascular system can be incorporated into our modeling framework based on previous models 2, 36. Finally, the model does not account for antivascular effects caused by the well-known highest concentration of the drug near blood vessels, which can result in killing of endothelial cells and changes in vascular structure and geometry. The effect of vascular architecture on drug delivery was discussed in a previous publication 28.
Our work is novel compared to our previous research in that the mathematical model has been extended with incorporation of nanoparticle transport inside the tumor taking into account the release of the chemotherapy and its binding and uptake by cancer cells. Furthermore, a new 1-dimensional model is presented, which is used to derive general conclusions about the characteristic length scale of the penetration of a delivery system into the tumor as a function of its size, binding affinity and release kinetic. Additionally, in previous research 33, we had presented for first time a 100-nm multistage particle, which released secondary 10-nm particles following enzymatic degradation. The scope of the current work was i) to present under what conditions (release and binding kinetics and particle size) a multi-stage nanoparticle delivery system is advantageous over conventional two-stage delivery systems, ii) to optimize the size of the multi-stage system and also to highlight the importance of the particle size for both two-stage and multi-stage systems, and finally, iii) to derive a simple expression for the selection of optimal release and binding rates that optimize the penetration of the drug in the tumor. Even though derived for nanoparticles, the results of this research can be applied to other cancer therapeutics, such as chemotherapy.
In our analysis for the multi-stage system, we assumed the same rate constant of release for the secondary particle and the drug. This was a simplification to reduce the number of model parameters and create the corresponding contour plots. In Supplementary Fig. 5, we repeated simulations for the multi-stage system fixing one of the release rate constants while varying the other. The results show that decreasing one of the two rate constants drastically reduces the efficacy of the nanoparticle. Therefore, it is desirable for the release of both the secondary particle and the drug to be fast. In our previous study (11), we calculated the release rate constant of the secondary particle to be in the range of 10-4 to 10-3 s-1, which is within the range of effectiveness of the multi-stage particles according to the contour plots of Figs. 2 and and5.5. Additionally, we did not account in our simulations for the internalization of the particles by cancer cells. Indeed, we assumed that only the drug (chemotherapy) is internalized and we performed simulations (Supplementary Fig. 4) to account for the effect of nanoparticle binding/internalization.
In a recent study, a new 100-nm liposome carrying the drug irinotecan showed a 1.9 month survival benefit in a phase III trial for pancreatic ductal adenocarcinomas in combination with 5-FU and leucovarin versus treatment with 5-FU and leucovarin alone (ClinicalTrials.gov identifier: NCT01494506). Our results (Figs. 2, ,33 and Supplementary Fig. 2) suggest that under certain conditions of the drug release kinetics, a 100-nm nanoparticle can be more effective than chemotherapy alone. In the particular clinical study, irinotecan is a very toxic drug and incorporating this drug into a liposome reduces its toxicity, and this could improve overall survival. Therefore, tuning of the drug release kinetics and reduction of toxicity can be sufficient even for a large, 100-nm nanoparticle to improve treatment outcome compared with monotherapy.
Model parameters (Supplementary Table 1) were carefully selected from the literature and our predictions have been shown to be consistent with available pre-clinical and clinical data 6, 28. The current model is limited in that it is two-dimensional and does not account for the heterogeneous distribution of vessel diameters and hematocrit and for the formation of vascular shunts 20, 21. Another parameter not accounted for here is the rheology of blood. Plasma leakage might result in local hemoconcentration, which can increase blood viscosity and flow resistance 25, 29. Finally, the effect of nanoparticle material, shape and surface charge were not considered in the current study but can vary considerably among different nanoparticle designs. Our model predictions are better suited for spherical, neutral (e.g. PEGylated) nanoparticles, but even for elongated particles the penetration length can be described by Eq. 1.
Acknowledgments
Simulations were performed at the high performance computer systems of the Cancer Biophysics laboratory at the University of Cyprus and of the Partners Healthcare System at Massachusetts General Hospital. This work was supported by the European Commission with a Marie-Curie Reintegration Grant (FP7-PIRG08-GA-2010-276894) to TS and the National Cancer Institute (P01-CA080124, R01-CA126642, R01-CA115767, R01-CA096915, R01-CA085140, R01-CA098706, Federal Share Income Grant), and a DoD Breast Cancer Research Innovator award (W81XWH-10-1-0016) to RKJ.
Footnotes
Conflict of interest: R.K.J. received research grants from Dyax, MedImmune and Roche; consultant fees from Enlight, Ophthotech, SynDevRx and Zyngenia; owns equity in Enlight, Ophthotech, SynDevRx and XTuit, serves on the Board of Directors of XTuit and Board of Trustees of Tekla Healthcare Investors, Tekla Life Sciences Investors and Tekla Healthcare Opportunities Fund. No reagents or funding from these companies was used in these studies. Therefore, there is no significant financial or other competing interest in the work.
References
Full text links
Read article at publisher's site: https://doi.org/10.1007/s10439-015-1276-9
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc4519365?pdf=render
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1007/s10439-015-1276-9
Article citations
Accumulation of liposomes in metastatic tumor sites is not necessary for anti-cancer drug efficacy.
J Transl Med, 22(1):621, 03 Jul 2024
Cited by: 0 articles | PMID: 38961395 | PMCID: PMC11223361
Recent developments in cancer diagnosis and treatment using nanotechnology.
Ann Med Surg (Lond), 86(8):4541-4554, 17 Jun 2024
Cited by: 1 article | PMID: 39118776 | PMCID: PMC11305775
Review Free full text in Europe PMC
In Situ Formation of Fibronectin-Enriched Protein Corona on Epigenetic Nanocarrier for Enhanced Synthetic Lethal Therapy.
Adv Sci (Weinh), 11(19):e2307940, 14 Mar 2024
Cited by: 2 articles | PMID: 38482976 | PMCID: PMC11109615
Development of an ultrasound-mediated nano-sized drug-delivery system for cancer treatment: from theory to experiment.
Nanomedicine (Lond), 19(13):1167-1189, 09 May 2024
Cited by: 0 articles | PMID: 38722104
Radiopharmaceutical transport in solid tumors via a 3-dimensional image-based spatiotemporal model.
NPJ Syst Biol Appl, 10(1):39, 12 Apr 2024
Cited by: 0 articles | PMID: 38609421 | PMCID: PMC11015041
Go to all (35) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Clinical Trials
- (1 citation) ClinicalTrials.gov - NCT01494506
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
EPR: Evidence and fallacy.
J Control Release, 190:451-464, 30 Apr 2014
Cited by: 275 articles | PMID: 24794900
Review
Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy.
Eur J Pharm Biopharm, 93:52-79, 23 Mar 2015
Cited by: 570 articles | PMID: 25813885
Review
A pharmacokinetic model for quantifying the effect of vascular permeability on the choice of drug carrier: a framework for personalized nanomedicine.
J Pharm Sci, 104(3):1174-1186, 12 Jan 2015
Cited by: 9 articles | PMID: 25583443
Antitumor efficacy of cisplatin-loaded glycol chitosan nanoparticles in tumor-bearing mice.
J Control Release, 127(1):41-49, 26 Dec 2007
Cited by: 159 articles | PMID: 18234388
Funding
Funders who supported this work.
NCI NIH HHS (13)
Grant ID: P01-CA080124
Grant ID: R01-CA085140
Grant ID: R01 CA085140
Grant ID: R01 CA115767
Grant ID: T32-CA073479
Grant ID: R01 CA098706
Grant ID: T32 CA073479
Grant ID: P01 CA080124
Grant ID: R01 CA126642
Grant ID: R01-CA096915
Grant ID: R01-CA115767
Grant ID: R01 CA096915
Grant ID: R01-CA126642