Abstract
Free full text

Haemodynamic definitions and updated clinical classification of pulmonary hypertension
Abstract
Since the 1st World Symposium on Pulmonary Hypertension (WSPH) in 1973, pulmonary hypertension (PH) has been arbitrarily defined as mean pulmonary arterial pressure (mPAP) ≥25 mmHg at rest, measured by right heart catheterisation. Recent data from normal subjects has shown that normal mPAP was 14.0±3.3 mmHg. Two standard deviations above this mean value would suggest mPAP >20 mmHg as above the upper limit of normal (above the 97.5th percentile). This definition is no longer arbitrary, but based on a scientific approach. However, this abnormal elevation of mPAP is not sufficient to define pulmonary vascular disease as it can be due to an increase in cardiac output or pulmonary arterial wedge pressure. Thus, this 6th WSPH Task Force proposes to include pulmonary vascular resistance ≥3 Wood Units in the definition of all forms of pre-capillary PH associated with mPAP >20 mmHg. Prospective trials are required to determine whether this PH population might benefit from specific management.
Regarding clinical classification, the main Task Force changes were the inclusion in group 1 of a subgroup “pulmonary arterial hypertension (PAH) long-term responders to calcium channel blockers”, due to the specific prognostic and management of these patients, and a subgroup “PAH with overt features of venous/capillaries (pulmonary veno-occlusive disease/pulmonary capillary haemangiomatosis) involvement”, due to evidence suggesting a continuum between arterial, capillary and vein involvement in PAH.
Short abstract
State of the art and research perspectives of haemodynamic definitions and clinical classification of pulmonary hypertension http://ow.ly/TJeR30mgWKj
Introduction
The main objectives of our Task Force were to reassess haemodynamic definitions and the clinical classification of pulmonary hypertension (PH).
Regarding definitions, we addressed two questions:
1) Should we redefine PH and pre-capillary PH?
2) Should exercise PH be reintroduced as part of the PH definition?
The other topic was to update the clinical classification, adopting some basic principles: 1) to maintain the general architecture of the current classification of PH for adults and children, 2) to provide only relevant modifications, and 3) to simplify the core of the classification
Haemodynamic definitions
Definition of PH
In 1961, a report of the World Health Organization (WHO) Expert Committee on Chronic Cor Pulmonale mentioned clearly that the mean pulmonary arterial pressure (mPAP) does not normally exceed 15 mmHg when the subject is at rest in a lying position, and that the value was little affected by age and never exceeded 20 mmHg [1].
Since the 1st World Symposium on Pulmonary Hypertension (WSPH) organised by the WHO in Geneva in 1973, PH has been defined as mPAP ≥25 mmHg measured by right heart catheterisation (RHC) in the supine position at rest [2]. The Geneva WHO meeting was devoted to primary PH, a severe form of PH, some years after an outbreak related to the intake of the anorexic drug aminorex [3]. In the report of the meeting, it was recognised that this upper limit of normal mPAP of 25 mmHg was somewhat empirical and arbitrarily defined [2]. However, this conservative cut-off value allowed physicians to discriminate severe PH due to primary PH from other forms of PH (mainly due to lung diseases) characterised by a lower mPAP. This definition remained unchanged during the subsequent WSPH meetings from 1998 to 2013 [4–6], at least in part to preclude potential overdiagnosis and overtreatment of PH.
What is actually the upper limit of normal mPAP?
In 2009, Kovacs et al. [7] analysed all available data obtained by RHC studies in healthy individuals to determine normal values of mPAP at rest and exercise. Data from 1187 normal subjects from 47 studies were analysed. mPAP at rest was 14.0±3.3 mmHg; this value was independent of sex and ethnicity, and was only slightly influenced by age and posture. Considering this mPAP of 14 mmHg, two standard deviations would suggest mPAP >20 mmHg as above the upper limit of normal (i.e. above the 97.5th percentile). This definition is, therefore, no longer arbitrary, but based on a scientific approach.
A value of mPAP used in isolation is not accurate enough to characterise a clinical condition
Whatever the mPAP cut-off value considered for defining PH (≥25 or >20 mmHg), it is important to emphasise that this value used in isolation cannot characterise a clinical condition and does not define the pathological process per se. PAP elevation may indeed have several different causes with different management and outcomes, including increase in cardiac output (CO), left-to-right cardiac shunts, elevation of pulmonary arterial wedge pressure (PAWP) in left heart disease (LHD) and hyperviscosity. This abnormal elevation may also be due to pulmonary vascular disease (PVD) associated with structural changes of small pulmonary arteries. In the present clinical classification of PH, pre-capillary PH concerns patients from groups 1, 3 and 4, some patients from group 5, and rarely patients from group 2 with combined pre- and post-capillary PH.
To identify pre-capillary PH suggesting the presence of PVD, an above normal elevation of pulmonary vascular resistance should be included in the definition
Including pulmonary vascular resistance (PVR=(mPAP–PAWP)/CO) in the definition of pre-capillary PH is essential, allowing discrimination of elevation of PAP due to PVD from those due to elevation of PAWP or due to high CO. Since the 3rd WSPH held in 2003, pre-capillary PH of group 1 (pulmonary arterial hypertension (PAH)) has been defined by the presence of mPAP ≥25 mmHg with a normal PAWP ≤15 mmHg and elevated PVR ≥3 Wood Units (WU) [4–6]. This cut-off value of PVR ≥3 WU is also quite arbitrary since some recent data suggest that PVR >2 WU could be also considered abnormal [6]. In this sense, the use of a cut-off value of PVR ≥3 WU is conservative, suggesting the presence of a manifest pre-capillary PH. This value of PVR ≥3 WU is considered clinically relevant in different clinical situations, suggesting the presence of a significant PVD, e.g. it is already used as the threshold value for which the correction of congenital systemic-to-pulmonary shunts becomes questionable [8]. Moreover, it has been shown that elevated PVR ≥3 WU was associated with a poor survival after heart transplantation [9]. During the 6th WSPH in 2018, for patients of group 2, the Task Force on PH due to LHD recommended a PVR cut-off value ≥3 WU to define patients with a pre-capillary component [10], so-called combined pre- and post-capillary PH, that is associated with a worse prognosis.
We propose including PVR ≥3 WU not only in the definition of pre-capillary PH of group 1, but also in the definition of all forms of pre-capillary PH.
In patients with PH due to chronic obstructive pulmonary disease, those with severe PH (>40 mmHg) have a marked increase in PVR (around 10 WU); more often these patients have a mild PH (mPAP 20–30 mmHg), associated with lower PVR but remaining generally >3 WU [11], and this is also the case for patients with idiopathic pulmonary fibrosis [12]. In these different chronic lung diseases, even a modest elevation in mPAP (20–29 mmHg) was associated with a poor prognosis [13].
In chronic thromboembolism (group 4), a large international registry reported haemodynamic findings of severe pre-capillary PH with a mPAP of 47 mmHg and a mean PVR of 8.9 WU [14]. In this setting, even in patients with mild elevation of mPAP (20–24 mmHg), PVR is generally >3 WU.
Outcome of patients with PVD and mPAP 21–24 mmHg
Accumulating data indicate that many patients with PVD associated with an increase in mPAP but below the former threshold value defining PH (≥25 mmHg) are at risk of disease progression.
In systemic sclerosis, outcome data of patients with mPAP at diagnosis between 21 and 24 mmHg have been recently published. In 2013, a single-centre cohort study of 228 patients with systemic sclerosis who underwent RHC for suspicion of PH was reported [15]. mPAP 21–24 mmHg was documented in 86 patients at baseline; of these, 38 underwent a second RHC during the follow-up (median follow-up 48±35 months) and 16 of these (42%) developed overt PH (mPAP ≥25 mmHg). The mean mPAP and PVR at baseline of these 16 patients was 22±2 mmHg and 2.9±0.6 WU, respectively; at follow-up, mean mPAP and PVR increased to 31±6 mmHg and 6.9±1.7 WU, respectively. Patients with so-called borderline mPAP at diagnosis were more likely to develop overt PAH than patients with mPAP ≤20 mmHg (p<0.001; hazard ratio (HR) 3.7). Incident development of PAH was not benign in this cohort, with five deaths during follow-up despite the subsequent introduction of dual oral combination therapy and/or i.v. prostacyclin.
More recently, a two-centre cohort study identified 21 patients with systemic sclerosis and a mPAP at baseline of 21–24 mmHg [16]; these patients underwent a second RHC with a median follow-up of 3 years. At baseline, mean mPAP and PVR were 22±1 mmHg and 2.3±0.8 WU, respectively. At follow-up, mPAP and PVR increased to 25±4 mmHg and 3.2±1.6 WU, respectively. Among them, seven patients (33%) developed overt PH (three PAH, three pre-capillary PH associated with interstitial lung disease and one PH due to LHD) (J.G. Coghlan, Cardiology Dept, Royal Free Hospital, London, UK; personal communication).
In 2017, an Austrian group [17] published a series of 547 patients with unexplained dyspnoea and/or at risk of PH who underwent RHC. Manifest PH (mPAP ≥25 mmHg) was confirmed in 290 patients, borderline PH (mPAP 21–24 mmHg) in 64 cases and 193 cases were considered as “normal” with mPAP ≤20 mmHg; among them, 137 patients were defined as “lower normal” with mPAP ≤15 mmHg. The median follow-up time of this cohort was 45.9 months; overall 161 patients (29%) died during the follow-up. In the multivariate model, considering age and comorbidities, both borderline PH and manifest PH were significantly associated with poor survival compared with the “lower normal” group with HR 2.37 (95% CI 1.14–4.97; p=0.022) and HR 5.05 (95% CI 2.79–9.12; p<0.001), respectively. At baseline, the group with mPAP 21–24 mmHg had a median PVR of 2.7 WU and 36% of these patients had PVR >3 WU.
Another instance where pre-capillary PH can be diagnosed at an earlier stage is chronic thromboembolism, as in this setting exercise limitation can occur in the absence of overt PH at rest due to the increase in dead-space ventilation resulting in a decreased ventilatory efficiency. Recently, two cohorts of 42 and 23 patients, respectively, have been reported with extensive persistent thromboembolic occlusions but without PH [18, 19]. At diagnosis, mPAP was 15–24 mmHg and PVR was 2–3 WU. These patients underwent pulmonary endarterectomy (PEA) and experienced significant improvement in WHO Functional Class, exercise capacity and quality of life, with no in-hospital mortality at 6 months. This form of chronic thromboembolism corresponded to 4% and 7% of the overall population treated with PEA in these two centres.
Summary and perspectives
A mPAP of 20 mmHg should be considered as the upper limit of normal value. This new definition has been recently proposed by others [20–22]. However, this abnormal elevation of mPAP in isolation is not sufficient to define PVD as it can be due to an increase in CO or PAWP.
Pre-capillary PH is best defined by the concomitant presence of mPAP >20 mmHg, PAWP ≤15 mmHg and PVR ≥3 WU (table 1), emphasising the need for RHC with mandatory measurement of CO and accurate measurement of PAWP.
TABLE 1
Haemodynamic definitions of pulmonary hypertension (PH)
| Definitions | Characteristics | Clinical groups# |
| Pre-capillary PH | mPAP >20 mmHg | 1, 3, 4 and 5 |
| PAWP ≤15 mmHg | ||
| PVR ≥3 WU | ||
| Isolated post-capillary PH (IpcPH) | mPAP >20 mmHg | 2 and 5 |
| PAWP >15 mmHg | ||
| PVR <3 WU | ||
| Combined pre- and post-capillary PH (CpcPH) | mPAP >20 mmHg | 2 and 5 |
| PAWP >15 mmHg | ||
| PVR ≥3 WU |
mPAP: mean pulmonary arterial pressure; PAWP: pulmonary arterial wedge pressure; PVR: pulmonary vascular resistance; WU: Wood Units. #: group 1: PAH; group 2: PH due to left heart disease; group 3: PH due to lung diseases and/or hypoxia; group 4: PH due to pulmonary artery obstructions; group 5: PH with unclear and/or multifactorial mechanisms.
For many years, the diagnosis of PH was based on an arbitrary value of mPAP ≥25 mmHg, probably because of understandable concern about overdiagnosis and overtreatment. Actually, the main cause of overdiagnosis and treatment of pre-capillary PH is the failure to confirm the diagnosis by RHC.
Conversely, the other side of this dilemma could be to undertreat some patients with abnormal elevation of PAP but not meeting the classical definition of PH. Today, there is growing evidence that in some PVDs (mainly PAH associated with systemic sclerosis, chronic thromboembolism and chronic lung diseases) patients with even a modest elevation in mPAP (21–24 mmHg) are symptomatic with exercise limitation and may have poor outcome. Nevertheless, a change in the haemodynamic definition of PH due to PVDs does not imply treating these additional patients, but highlights the importance of close monitoring in this population. Prospective trials are required to determine whether this PH population might benefit from specific management.
Definition of exercise PH
In 2004, PH was defined as resting mPAP >25 mmHg or exercise mPAP >30 mmHg [8]. At the 4th WSPH in 2008, however, the “exercise” part of the definition was removed [23]. This was largely due to uncertainties concerning the interrelationships between normal ageing, CO changes with exercise and pulmonary vascular physiology. This question was revisited again at the 6th WSPH in 2018.
Why might exercise PH be relevant?
A rise in resting PH pressure is a late event in the natural history of PVDs, because of microvascular “reserves”. PAP rises only when ≥50% of the microcirculation has been lost [24]. Much effort has been directed towards detecting PVD at an earlier (and potentially more treatable) stage. Intuitively, “unmasking” PVD by increasing CO to demonstrate increased resistance is a logical idea. Furthermore, PH patients first develop symptoms on exercise.
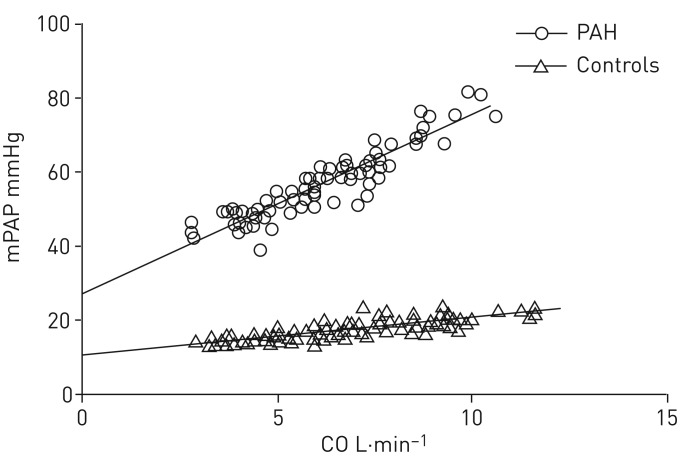
A number of studies have tried to unmask PVD by “stressing” the pulmonary circulation, by lung flow redistribution with upright posture [25] or by increasing CO [26]. This has led to the concept of “multipoint mPAP–CO” curves, where the rate of rise of mPAP with increasing CO has been informative (figure 1). In general, mPAP rises by ≥1 mmHg per litre of CO in normal subjects; PVD patients have a rise of ≥3 mmHg per litre of CO, reflecting increased resistance [27]. Generating such data is, however, challenging as exercise RHC measurements are time consuming, difficult, and potentially complicated by errors due to rapid respiratory cycles and inaccuracies in exercise CO and PAWP measures. Thus, generating mPAP–CO graphs for individual patients is impractical as a clinical routine.
Why might defining exercise PH and PAH be difficult?
A number of variables impact on the “normal” change of mPAP with exercise, which in turn complicates any attempt to establish a threshold for “exercise PH” as a pathological condition. Physiological changes occur with normal ageing [7] and mPAP also does rise with increasing CO; therefore in subjects (e.g. elite athletes) who can raise their CO to 30–40 L·min−1 at peak exercise, mPAP can exceed previous “upper limits” of normal [28]. The greatest difficulty, however, is in using exercise to deduce the presence of PVD, because exercise also causes a rise in PAWP. Thus, if PVR=(mPAP–PAWP)/CO, one must measure exercise PAWP to deduce the pathogenesis of an abnormally high exercise-related PAP. As LHD is the commonest cause of resting PH and left atrial pressure rises abnormally with exercise in subjects with LHD, measuring changes in PAWP (or left atrial pressure) with exercise becomes the critical determinant for assessing PVR, in breathless patients with exercise PH.
This lack of diagnostic discrimination power (whether exercise PH is due to LHD or to PVD) has been explored by Herve et al. [29]. Although total pulmonary resistance >3 mmHg per litre of CO distinguished healthy controls from those with LHD or PVD, it was impossible to distinguish LHD from PVD patients with confidence (figure 2). It should be noted that accurate measurement of exercise PAWP is technically challenging, related to the exaggerated respiratory swings in PAWP and in part to difficulties in “wedging” a balloon catheter adequately during vigorous exertion.
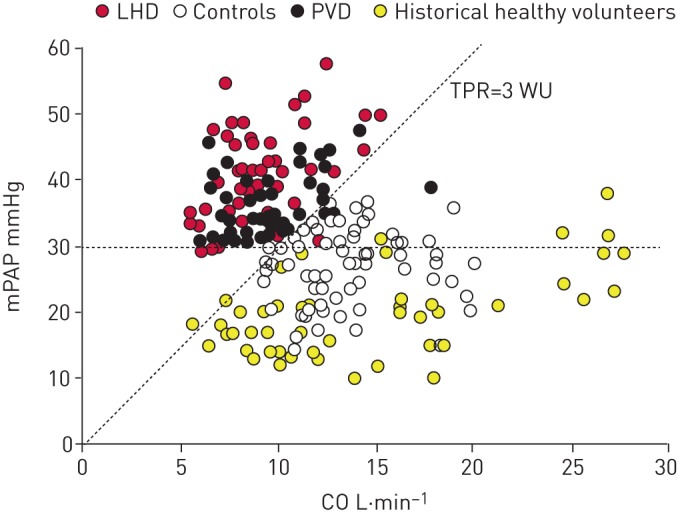
Knowledge of the mean pulmonary arterial pressure (mPAP)–cardiac output (CO) relationship does not allow distinction between left heart disease (LHD) and pulmonary vascular disease (PVD) patients; knowledge of exercise pulmonary arterial wedge pressure is also required. TPR: total pulmonary resistance; WU: Wood Units. Reproduced from [29] with permission.
Summary and perspectives
Although there is intuitive appeal to measuring exercise haemodynamics to detect PVD at an earlier stage than can be revealed by measurements at rest, too many uncertainties persist to allow the reintroduction of a clinically useful definition of exercise PH. More information is required concerning normal changes with ageing, high CO and especially about distinguishing exercise-elated changes in PAWP (due to LHD) from changes due to PVD. We believe that these will be fruitful areas for future investigation.
Updated clinical classification of PH
The general purpose of clinical classification of PH is to categorise clinical conditions associated with PH based on similar pathophysiological mechanisms, clinical presentation, haemodynamic characteristics and therapeutic management. A comprehensive and simplified version of the clinical classification of PH in children and adults is presented in table 2. For patients with PAH associated with congenital heart disease, the four subgroups (Eisenmenger syndrome, left-to-right shunts, coincidental or small defects and post-operative/closed defects) remain the same [30] as the indications for defect closure (see the Task Force article in this issue of the European Respiratory Journal [31]). The updates of groups 2, 3 and 4 are presented in the respective Task Force articles in this issue of the European Respiratory Journal [10, 32, 33].
TABLE 2
| 1 PAH |
 1.1 Idiopathic PAH 1.1 Idiopathic PAH |
 1.2 Heritable PAH 1.2 Heritable PAH |
 1.3 Drug- and toxin-induced PAH (table 3) 1.3 Drug- and toxin-induced PAH (table 3) |
 1.4 PAH associated with: 1.4 PAH associated with: |
  1.4.1 Connective tissue disease 1.4.1 Connective tissue disease |
  1.4.2 HIV infection 1.4.2 HIV infection |
  1.4.3 Portal hypertension 1.4.3 Portal hypertension |
  1.4.4 Congenital heart disease 1.4.4 Congenital heart disease |
  1.4.5 Schistosomiasis 1.4.5 Schistosomiasis |
 1.5 PAH long-term responders to calcium channel blockers (table 4) 1.5 PAH long-term responders to calcium channel blockers (table 4) |
 1.6 PAH with overt features of venous/capillaries (PVOD/PCH) involvement (table 5) 1.6 PAH with overt features of venous/capillaries (PVOD/PCH) involvement (table 5) |
 1.7 Persistent PH of the newborn syndrome 1.7 Persistent PH of the newborn syndrome |
| 2 PH due to left heart disease |
 2.1 PH due to heart failure with preserved LVEF 2.1 PH due to heart failure with preserved LVEF |
 2.2 PH due to heart failure with reduced LVEF 2.2 PH due to heart failure with reduced LVEF |
 2.3 Valvular heart disease 2.3 Valvular heart disease |
 2.4 Congenital/acquired cardiovascular conditions leading to post-capillary PH 2.4 Congenital/acquired cardiovascular conditions leading to post-capillary PH |
| 3 PH due to lung diseases and/or hypoxia |
 3.1 Obstructive lung disease 3.1 Obstructive lung disease |
 3.2 Restrictive lung disease 3.2 Restrictive lung disease |
 3.3 Other lung disease with mixed restrictive/obstructive pattern 3.3 Other lung disease with mixed restrictive/obstructive pattern |
 3.4 Hypoxia without lung disease 3.4 Hypoxia without lung disease |
 3.5 Developmental lung disorders 3.5 Developmental lung disorders |
| 4 PH due to pulmonary artery obstructions (table 6) |
 4.1 Chronic thromboembolic PH 4.1 Chronic thromboembolic PH |
 4.2 Other pulmonary artery obstructions 4.2 Other pulmonary artery obstructions |
| 5 PH with unclear and/or multifactorial mechanisms (table 7) |
 5.1 Haematological disorders 5.1 Haematological disorders |
 5.2 Systemic and metabolic disorders 5.2 Systemic and metabolic disorders |
 5.3 Others 5.3 Others |
 5.4 Complex congenital heart disease 5.4 Complex congenital heart disease |
PAH: pulmonary arterial hypertension; PVOD: pulmonary veno-occlusive disease; PCH: pulmonary capillary haemangiomatosis; LVEF: left ventricular ejection fraction.
Update of group 1: PAH
Group 1.3: Drug- and toxin-induced PAH
We propose simplifying the characterisation of PAH associated with drugs and toxins into two subgroups to help physicians to identify drugs requiring specific surveillance. “Definite association” includes drugs with data based on outbreaks, epidemiological case–control studies or large multicentre series. “Possible association” is suggested by multiple case series or cases with drugs with similar mechanisms of action. Based on recent data, the association of PAH with two drugs and toxins (amphetamines/methamphetamines and dasatinib) is now considered definite (table 3).
TABLE 3
Updated classification of drugs and toxins associated with PAH
| Definite | Possible |
| Aminorex | Cocaine |
| Fenfluramine | Phenylpropanolamine |
| Dexfenfluramine | l-tryptophan |
| Benfluorex | St John's wort |
| Methamphetamines | Amphetamines |
| Dasatinib | Interferon-α and -β |
| Toxic rapeseed oil | Alkylating agents |
| Bosutinib | |
| Direct-acting antiviral agents against hepatitis C virus | |
| Leflunomide | |
| Indirubin (Chinese herb Qing-Dai) |
Zamanian et al. [34] reported a large series of 90 cases of PAH associated with methamphetamine-associated PAH; these subjects were less likely to be female, had more haemodynamic compromise at diagnosis and had poorer outcomes than IPAH. This analysis confirmed an association between methamphetamine/amphetamine use and PAH-related hospitalisation (relative risk 2.64, 95% CI 2.18–3.2; p<0.001). Interestingly, pathological assessment demonstrated characteristic vascular changes similar to IPAH, including angiomatoid plexiform lesions, but also proliferative capillaries, as described in pulmonary capillary haemangiomatosis (PCH) or pulmonary veno-occlusive disease (PVOD). Dasatinib is a second-generation tyrosine kinase inhibitor and has been reported to be associated with PAH; the lowest estimate of incident PAH occurring in patients exposed to dasatinib in France was 0.45% [35]. Dasatinib-induced PAH frequently improves after discontinuation, but persists in over one-third of patients [35, 36].
Over the last 5 years, new drugs have been identified or suspected as potential risk factors for PAH. Several cases of deterioration or relapse of dasatinib-associated PAH after bosutinib initiation have been reported [37–39]; these cases were also characterised by an improvement of PAH after withdrawal of bosutinib. Cases of severe portopulmonary hypertension have occurred with novel strategies of direct-acting antivirals, including sofosbuvir for hepatitis C virus infection [40, 41]. Leflunomide, a disease-modifying antirheumatic drug, has been associated with several cases of PAH [42–44]. Recently, cases of potentially reversible PAH associated with natural indigo (Qing-Dai), an unapproved Chinese herbal drug, have been reported from the Japan Pulmonary Hypertension Registry [45, 46]. The active pharmaceutical ingredient of Qing-Dai is indirubin, which could induce apoptosis of pulmonary endothelial cells in vitro [46].
Group 1.5: PAH long-term responders to calcium channel blockers
Although remodelling of small pulmonary arteries is the main pathological finding in PAH, pulmonary vasoconstriction also plays an important role in PAH pathophysiology, particularly in vasoreactive patients.
In a series of 64 patients published in 1992, Rich et al. [47] reported that patients with an acute vasodilator response to calcium channel blockers (CCBs) had dramatically improved survival when treated with long-term CCBs. In 2005, Sitbon et al. [48] demonstrated in a large series of 557 PH patients that acute vasodilator response may be observed in 12.5% of idiopathic PAH (IPAH), and overall 6.8% of patients have a long-term clinical and haemodynamic improvement on CCBs. This study identified the best criteria to identify acute vasodilator response, i.e. a reduction of mPAP ≥10 mmHg to reach an absolute value of mPAP ≤40 mmHg with an increased or unchanged CO. For vasoreactivity testing, inhaled nitric oxide at 10–20 ppm is the preferred agent, but i.v. epoprostenol, i.v. adenosine or inhaled iloprost can be used as alternatives (table 4). Long-term response to CCBs was defined by clinical improvement (New York Heart Association Functional Class I or II) and sustained haemodynamic improvement after at least 1 year on CCBs only (same or better than achieved in the acute test and usually to obtain mPAP <30 mmHg with an increased or normal CO) (table 4). Pulmonary vasoreactivity testing for identification of patients suitable for CCB treatment is recommended only for patients with IPAH, heritable PAH or drug-induced PAH. In all other forms of PAH and PH the results can be misleading and long-term responders are rare [49].
TABLE 4
Definitions of acute and long-term response
| Acute pulmonary vasoreactivity# for patients with idiopathic, hereditable or drug-induced PAH | Reduction of mPAP ≥10 mmHg to reach an absolute value of mPAP ≤40 mmHg |
| Increased or unchanged cardiac output | |
| Long-term response to CCBs | New York Heart Association Functional Class I/II |
| With sustained haemodynamic improvement (same or better than achieved in the acute test) after at least 1 year on CCBs only |
PAH: pulmonary arterial hypertension; mPAP: mean pulmonary arterial pressure; CCB: calcium channel blocker. #: nitric oxide (10–20 ppm) is recommended for performing vasoreactivity testing, but i.v. epoprostenol, i.v. adenosine or inhaled iloprost can be used as alternatives.
Pathophysiology of PAH with vasoreactivity is largely unknown. Recently, Hemnes and co-workers have shown that PAH with vasoreactivity was characterised by a specific blood signature (microarray of cultured lymphocytes) and different gene variants (whole exome sequencing) compared with IPAH [50, 51]. These results suggest a specific entity with a distinct clinical course, characterised by significantly better prognosis, unique management and different pathophysiology (table 2).
Group 1.6: PAH with overt features of venous/capillaries (PVOD/PCH) involvement
Significant pulmonary venous and/or capillary involvement has been reported in many conditions which are known causes of PAH, such as systemic sclerosis. In the previous classification, PVOD/PCH was characterised as a distinct subgroup.
PVOD/PCH and PAH share similar causes and associated conditions even if some of them are more frequently associated with more pronounced venous/capillary involvement (table 5). Heritable forms of PVOD/PCH have been recognised in consanguineous families with a recessive transmission, due to biallelic mutations in the eukaryotic translation initiation factor 2α kinase 4 (EIF2AK4) gene [52–54]. Occupational exposure to organic solvents, particularly to trichloroethylene, has been associated with the development of pre-capillary PH with significant venous and capillary involvement [55].
TABLE 5
Signs evocative of venous and capillary (pulmonary veno-occlusive disease/pulmonary capillary haemangiomatosis) involvement
| Pulmonary function tests | Decreased DLCO (frequently <50%) |
| Severe hypoxaemia | |
| Chest HRCT | Septal lines |
| Centrilobular ground-glass opacities/nodules | |
| Mediastinal lymph node enlargement | |
| Response to PAH therapy | Possible pulmonary oedema |
| Genetic background | Biallelic EIF2AK4 mutations |
| Occupational exposure | Organic solvent (trichloroethylene) |
DLCO: diffusing capacity of the lung for carbon monoxide; HRCT: high-resolution computed tomography; PAH: pulmonary arterial hypertension.
Diagnosis of significant pulmonary venous/capillary involvement (PVOD/PCH) may be strongly suspected based on pulmonary function tests (decreased diffusion capacity of the lung for carbon monoxide (DLCO) frequently <50% of theoretical values), arterial blood gases (severe hypoxaemia) and high-resolution computed tomography of the chest (septal lines, centrilobular ground-glass opacities/nodules and mediastinal lymph node enlargement) (table 5) [53, 54, 56]. More pronounced pulmonary venous/capillary involvement is associated with a poor prognosis, a limited response to PAH therapy and a risk of pulmonary oedema with these treatments [53, 57].
PAH and PVOD/PCH usually share a broadly similar haemodynamic profile and clinical presentation. Of note, significant pulmonary arterial remodelling has been described in biallelic EIF2AK4 mutation carriers [58] and muscular remodelling of pulmonary septal veins can be observed in BMPR2 (bone morphogenetic protein receptor type 2) mutation carriers [59]. What matters in practice are the clinical consequences of pulmonary venous/capillary involvement in pre-capillary PH. We therefore suggest that PAH and PVOD/PCH belong to a spectrum of PVDs rather than representing two clear-cut distinct entities. We propose including “PAH with overt features of venous/capillaries (PVOD/PCH) involvement” in the revised PAH (group 1) of the updated PH classification (table 2).
Update of group 5: PH with unclear and/or multifactorial mechanisms
Since the basis of our classification system was established in 1998, group 5 has passed through significant changes. Initially describing “disorders directly affecting the pulmonary vasculature”, then named “miscellaneous” during the 3rd WSPH in 2003 [60], and finally reaching its current presentation, this group includes forms of PH with unclear and/or multifactorial mechanisms [30, 61]. From the beginning, this group has represented less-studied forms of PH, in comparison with other groups; nevertheless, many of the PH forms currently in group 5 represent a significant part of the yet unrecognised worldwide burden of PH [62].
One of the central characteristics of the clinical conditions included in group 5 is that there is no identified predominant mechanism driving the development of PH and there may be multiple pathophysiological phenomena involved in this process (table 7). In this update of the classification, changes were considered only for the subtypes in which a definite relocation was supported by the available literature.
TABLE 7
Pulmonary hypertension with unclear and/or multifactorial mechanisms
| 5.1 Haematological disorders | Chronic haemolytic anaemia |
| Myeloproliferative disorders | |
| 5.2 Systemic and metabolic disorders | Pulmonary Langerhans cell histiocytosis |
| Gaucher disease | |
| Glycogen storage disease | |
| Neurofibromatosis | |
| Sarcoidosis | |
| 5.3 Others | Chronic renal failure with or without haemodialysis |
| Fibrosing mediastinitis | |
| 5.4 Complex congenital heart disease | See the Task Force article by Rosenzweig et al. [31] in this issue of the European Respiratory Journal |
TABLE 6
Pulmonary hypertension (PH) due to pulmonary artery obstructions
| 4.1 Chronic thromboembolic PH | |
| 4.2 Other pulmonary artery obstructions | |
 4.2.1 Sarcoma (high or intermediate grade) or angiosarcoma 4.2.1 Sarcoma (high or intermediate grade) or angiosarcoma | |
 4.2.2 Other malignant tumours 4.2.2 Other malignant tumours Renal carcinoma Renal carcinoma Uterine carcinoma Uterine carcinoma Germ cell tumours of the testis Germ cell tumours of the testis Other tumours Other tumours | |
 4.2.3 Non-malignant tumours 4.2.3 Non-malignant tumours Uterine leiomyoma Uterine leiomyoma | |
 4.2.4 Arteritis without connective tissue disease 4.2.4 Arteritis without connective tissue disease | |
 4.2.5 Congenital pulmonary artery stenoses 4.2.5 Congenital pulmonary artery stenoses | |
 4.2.6 Parasites 4.2.6 Parasites
 Hydatidosis Hydatidosis |
Group 5.1: Haematological disorders
Chronic haemolytic anaemia is clearly associated with an increased risk of PH [63]. Since the 5th WSPH in 2013, little has been added to the current understanding of the numerous presentations of PH in sickle cell disease (SCD). However, it is clear that in this setting PH is frequently multifactorial, including elevated CO, LHD, thromboembolic disease, altered blood viscosity and PVD due to endothelial dysfunction, mainly due to nitric oxide depletion [64–67]. More recently, restrictive cardiomyopathy has been better recognised and described in clinical and experimental studies [68]. These data reinforce the utmost importance of this particular form of PH and the need for continuous investigation in this field [64, 65]. In addition, over recent years, significant data have been generated regarding another important chronic haemolytic anaemia, i.e. β-thalassaemia. A better understanding about the risk factors for major complications of the disease, including PH, has been derived from significant cohorts [69]. Furthermore, Derchi et al. [70] evaluated the prevalence of PH through invasive haemodynamic evaluation, similarly to what has been done in SCD [71–73]. In their cohort of 1309 patients that underwent screening evaluation, pre-capillary PH was confirmed in 2.1% of the cases, while a post-capillary profile was found in 0.3% [70]. Older age and splenectomy were clear risk factors associated with PH. Although this study provided important information regarding the significance of PH in this clinical condition, more data concerning the histopathology of vascular involvement as well as about pathophysiological mechanisms of PH development in these patients are still needed to better address potential management strategies.
Splenectomy deserves particular discussion. Following the first association of splenectomy and PH [74], it was not clear whether it represented a risk factor or a particular condition. Since then, splenectomy has been associated with the development of PH in many haematological conditions, as in the aforementioned β-thalassaemia [69, 70]. Most importantly, it has been strongly associated with the development of chronic thromboembolic PH [75]. Nevertheless, no other particular phenotype or change in clinical behaviour has been associated with the presence of splenectomy, suggesting that it should be better considered as a risk factor for PH instead of a particular condition deserving a specific classification.
Group 5.2: Systemic and metabolic disorders
It is important to emphasise that the concept supporting the classification of a clinical condition with systemic manifestations and a clear risk for PH into group 5 is, again, the lack of robust data allowing a definite recognition of predominant pathophysiological mechanisms, or describing the histopathological findings or yet, describing management strategies. For this reason, several conditions have been classified in this group, including sarcoidosis, lymphangioleiomyomatosis (LAM), pulmonary Langerhans cell histiocytosis, thyroid disorders, Gaucher disease, glycogen storage disease and neurofibromatosis
Regarding LAM, a recent screening study [76], in a significant cohort of more than 100 LAM patients, reinforced that PH in LAM is usually mild, as previously described [77]. From six patients (5.7%) presenting with pre-capillary PH, none had mPAP >30 mmHg. Moreover, the presence of PH was associated with poor pulmonary function, suggesting that the rise in pulmonary pressure is associated with parenchymal involvement, which was further reinforced by a more recent echocardiographic study [78]. Based on these findings, PH in LAM seem to be better classified together with other parenchymal lung diseases, in group 3.
Sarcoidosis is a more challenging situation, given the fact that PH might develop as a consequence of significantly different factors, from parenchymal lung disease to extrinsic compression of pulmonary vessels, direct myocardial involvement or even granulomatous arteriopathy [79]. Significant lung parenchymal disease is a highly prevalent condition in patients with sarcoidosis-associated PH [80, 81], although the presence of left ventricular dysfunction cannot be neglected [80]. It is difficult, however, to solely consider lung parenchymal involvement to reclassify sarcoidosis, given the multiplicity of other factors yet to be clarified, including the different histopathological pattern of the pulmonary vessels commonly seen in sarcoidosis, with granuloma formation in some cases [79], as opposed to other diseases in group 3. While these features are better studied, sarcoidosis remains classified into group 5.
There is a strong rationale for the concomitance of thyroid diseases and PH, from autoimmunity to the presence of high or low CO, left ventricular dysfunction, or even an angioproliferation profile. The prevalence of thyroid disorders is increased in patients with PAH [82, 83]; furthermore, the level of thyroid dysfunction is also associated with prognosis in this setting [84]. Nevertheless, similarly to splenectomy, the presence of thyroid dysfunction does not necessarily characterise a specific clinical condition; it behaves more like a risk factor or a comorbidity that should be specifically controlled during the course of PH management. Until novel data prove otherwise, it was a consensus to withdraw thyroid disorders from the classification as a specific entity and better discuss their role as risk factors and/or associated comorbidities.
Many different conditions associated with PH still need better designed studies that add to the understanding of disease development. We propose that changes be made only after the generation of robust data to support such reclassification.
Conclusions
This Task Force first revisited the definition of PH, suggesting a new pressure level to define an abnormal elevation in the mPAP >20 mmHg and the need for PVR ≥3 WU to define the presence of pre-capillary PH. Furthermore, the Task Force proposed to simplify the core of the clinical classification of PH (table 2) which has been developed in additional tables. The two main changes in group 1 (PAH) include 1) the designation of a subgroup “PAH long-term responders to CCBs” and 2) the inclusion of the subgroup “PAH with overt features of venous/capillaries (PVOD/PCH) involvement”. Group 5 (PH with unclear and/or multifactorial mechanisms) was simplified with 1) the removal of splenectomy and thyroid disorders, and 2) the classification of LAM-associated PH together with other parenchymal lung diseases in group 3. Important new insights for groups 2, 3 and 4 have been addressed by the respective Task Forces in this issue of the European Respiratory Journal [10, 32, 33].
Footnotes
Number 4 in the series “Proceedings of the 6th World Symposium on Pulmonary Hypertension” Edited by N. Galiè, V.V. McLaughlin, L.J. Rubin and G. Simonneau
Conflict of interest: G. Simonneau reports grants, personal fees and non-financial support from Actelion Pharmaceuticals, Bayer Healthcare, Merck and GSK, outside the submitted work.
Conflict of interest: D. Montani reports grants, personal fees and non-financial support from Actelion Pharmaceuticals, Bayer Healthcare, Merck and GSK, outside the submitted work.
Conflict of interest: D.S. Celermajer is an investigator on two clinical trials sponsored by Actelion.
Conflict of interest: C.P. Denton reports grants and personal fees from Actelion and Roche, grants from GSK, and personal fees from Bayer and Boehringer Ingelheim, during the conduct of the study; grants and personal fees from Inventiva and CSL Behring, and personal fees from Leadiant, outside the submitted work.
Conflict of interest: M.A. Gatzoulis reports personal fees for steering committee membership from Actelion Pharmaceuticals, and grants from Actelion Global, Pfizer and GSK, during the conduct of the study.
Conflict of interest: M. Krowka is a steering committee member for PORTICO (Macitentan for Portopulmonary Hypertension Study), which is sponsored by Actelion, outside the submitted work.
Conflict of interest: P.G. Williams received personal fees for advisory board meetings from Aspen SA and GSK, outside the submitted work.
Conflict of interest: R. Souza reports lecture and consultancy fees from Actelion, Bayer, GSK and Pfizer, outside the submitted work.
References
Full text links
Read article at publisher's site: https://doi.org/10.1183/13993003.01913-2018
Read article for free, from open access legal sources, via Unpaywall:
https://erj.ersjournals.com/content/erj/53/1/1801913.full.pdf
Citations & impact
Impact metrics
Article citations
Multiple serum biomarkers associate with mortality and interstitial lung disease progression in systemic sclerosis.
Rheumatology (Oxford), 63(11):2981-2988, 01 Nov 2024
Cited by: 0 articles | PMID: 38366632 | PMCID: PMC11534140
Emerging multimodality imaging techniques for the pulmonary circulation.
Eur Respir J, 64(4):2401128, 31 Oct 2024
Cited by: 0 articles | PMID: 39209480 | PMCID: PMC11525339
Review Free full text in Europe PMC
Vitamin D receptor and its antiproliferative effect in human pulmonary arterial hypertension.
Sci Rep, 14(1):27445, 10 Nov 2024
Cited by: 0 articles | PMID: 39523384 | PMCID: PMC11551162
Management and outcomes in pulmonary arterial hypertension patients with sepsis.
BMC Pulm Med, 24(1):538, 28 Oct 2024
Cited by: 0 articles | PMID: 39468558 | PMCID: PMC11520816
Treatment algorithm for pulmonary arterial hypertension.
Eur Respir J, 64(4):2401325, 31 Oct 2024
Cited by: 3 articles | PMID: 39209476 | PMCID: PMC11525349
Review Free full text in Europe PMC
Go to all (1,533) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Definition, classification and diagnosis of pulmonary hypertension.
Eur Respir J, 64(4):2401324, 31 Oct 2024
Cited by: 3 articles | PMID: 39209475 | PMCID: PMC11533989
[Diagnosis and classification of pulmonary hypertension].
Presse Med, 39 Suppl 1:1S3-15, 01 Jun 2010
Cited by: 0 articles | PMID: 20732615
[Hemodynamic Definition of Pulmonary Hypertension: Commentary on the Proposed Change by the 6th World Symposium on Pulmonary Hypertension].
Dtsch Med Wochenschr, 144(19):1367-1372, 05 Jul 2019
Cited by: 5 articles | PMID: 31277079
Pulmonary arterial hypertension.
Orphanet J Rare Dis, 8:97, 06 Jul 2013
Cited by: 152 articles | PMID: 23829793 | PMCID: PMC3750932
Review Free full text in Europe PMC