Abstract
Background
During the first wave of COVID-19, many Iranians were poisoned by ingesting hand sanitizers and/or alcoholic beverages to avoid viral infection. To assess whether the COVID-19 pandemic resulted in an increased prevalence of accidental hand sanitizer/alcoholic beverage exposure in children and adolescents, we compared pediatric hospitalization rates during COVID-19 and the previous year. For poisoning admissions during COVID-19, we also evaluated the cause by age and clinical outcomes.Methods
This retrospective data linkage study evaluated data from the Legal Medicine Organization (reporting mortalities) and hospitalization data from nine toxicology referral centers for alcohol-poisoned patients (age 0 to 18 years) for the study period (February 23 to June 22, 2020) and the pre-COVID-19 reference period (same dates in 2019).Results
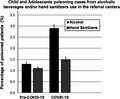
Hospitalization rates due to ethanol and methanol exposure were significantly higher in 2020 (n = 375) than 2019 (n = 202; OR [95% CI] 1.9 [1.6, 2.2], p < 0.001). During COVID-19, in patients ≤15 years, the odds of intoxication from hand sanitizers were significantly higher than from alcoholic beverages, while in 15- to 18-year-olds, alcoholic beverage exposure was 6.7 times more common (95% CI 2.8, 16.1, p < 0.001). Of 375 children/adolescents hospitalized for alcoholic beverage and hand sanitizer exposure in 2020, six did not survive. The odds of fatal outcome were seven times higher in 15- to 18-year-olds (OR (95% CI) 7.0 (2.4, 20.1); p < 0.001).Conclusion
The Iranian methanol poisoning outbreak during the first wave of COVID-19 was associated with significantly increased hospitalization rates among children and adolescents-including at least six pediatric in-hospital deaths from poisoning. Public awareness needs to be raised of the risks associated with ingesting alcoholic hand sanitizers.Free full text
COVID‐19 pandemic and methanol poisoning outbreak in Iranian children and adolescents: A data linkage study
Abstract
Background
During the first wave of COVID‐19, many Iranians were poisoned by ingesting hand sanitizers and/or alcoholic beverages to avoid viral infection. To assess whether the COVID‐19 pandemic resulted in an increased prevalence of accidental hand sanitizer/alcoholic beverage exposure in children and adolescents, we compared pediatric hospitalization rates during COVID‐19 and the previous year. For poisoning admissions during COVID‐19, we also evaluated the cause by age and clinical outcomes.
Methods
This retrospective data linkage study evaluated data from the Legal Medicine Organization (reporting mortalities) and hospitalization data from nine toxicology referral centers for alcohol‐poisoned patients (age 0 to 18 years) for the study period (February 23 to June 22, 2020) and the pre‐COVID‐19 reference period (same dates in 2019).
Results
Hospitalization rates due to ethanol and methanol exposure were significantly higher in 2020 (n = 375) than 2019 (n = 202; OR [95% CI] 1.9 [1.6, 2.2], p < 0.001). During COVID‐19, in patients ≤15 years, the odds of intoxication from hand sanitizers were significantly higher than from alcoholic beverages, while in 15‐ to 18‐year‐olds, alcoholic beverage exposure was 6.7 times more common (95% CI 2.8, 16.1, p < 0.001). Of 375 children/adolescents hospitalized for alcoholic beverage and hand sanitizer exposure in 2020, six did not survive. The odds of fatal outcome were seven times higher in 15‐ to 18‐year‐olds (OR (95% CI) 7.0 (2.4, 20.1); p < 0.001).
Conclusion
The Iranian methanol poisoning outbreak during the first wave of COVID‐19 was associated with significantly increased hospitalization rates among children and adolescents—including at least six pediatric in‐hospital deaths from poisoning. Public awareness needs to be raised of the risks associated with ingesting alcoholic hand sanitizers.
Abstract
During the first wave of COVID‐19 pandemic, Iran experienced the worldwide biggest methanol outbreak recorded to date. The outbreak triggered by consumption of toxic alcoholic beverages or hand sanitizers, partially motivated by the belief that ingestion would protect against COVID‐19 infection. Our study shows that children and adolescents were also affected, with 22 deaths due to methanol exposure recorded in 2020. These were significantly higher in Feb‐June 2020 (during COVID‐19), compared to the corresponding time period in 2019.
INTRODUCTION
On February 19, 2020, Iran reported the first confirmed case of COVID‐19 infection in Qom, almost a month before the World Health Organization declared a global pandemic on March 11, 2020 (Soltaninejad, 2020; WHO, 2020a, 2020b). Lack of adequate diagnostic tools, prior training of healthcare professionals and the community on how to manage airborne viruses, and measures to prevent the viral spread facilitated a sharp increase in the rate of COVID‐19 infections in Iran. By March 28, 2020, about 35,408 COVID‐19 cases had been reported, including 2517 deaths (Soltaninejad, 2020).
The United States Centers for Disease Control and Prevention (CDC) recommended hand sanitization as the first method of disease prevention (CDC, 2019). Also, guidelines recommended the disinfection of frequently touched surfaces and objects to prevent the spread of the virus (CDC, 2019; Emmanuel et al., 2020), resulting in high demand for hand sanitizers in the general population.
In Iran, this led to a serious shortage of these products (Kampf, et al., 2020), and counterfeit and nonstandardized hand sanitizers entered the black market, some of which contained less than 60% ethanol (EtOH) or contained methanol (Jairoun et al., 2021). This coincided with the rapid spread of COVID‐19 misinformation via social media at the beginning of the COVID‐19 pandemic.
One of the misleading suggestions via social media was to drink or gargle alcoholic beverages to disinfect the mouth and prevent COVID‐19 infection (Delirrad & Mohammadi, 2020; Soltaninejad, 2020). Other recommendations involved household cleaning agents and disinfectants, leading to excessive exposure. This COVID‐19 misinformation caused a steep increase in household poisonings, including a major methanol poisoning outbreak in the population (Gharpure et al., 2020; Hassanian‐Moghaddam et al., 2020; Chang et al., 2020).
The Iranian methanol poisoning outbreak in adults involved 5876 hospitalizations and about 800 deaths registered by the Legal Medicine Organization (LMO) between February and May 2020, equivalent to an estimated mortality rate of 9 to 14% (Hassanian‐Moghaddam et al., 2020). This outbreak was five times greater than the second largest methanol outbreak in history, with 1066 hospitalizations reported in Libya in March 2013 (Rostrup et al., 2016). However, the scale of methanol poisoning during COVID‐19 in children and adolescents is unknown to date. To address this gap in the literature, we conducted a multicenter data linkage study of pediatric hospitalization and mortality data.
We aimed to compare the prevalence rates during the first wave of COVID‐19 versus the previous year (2019; “pre‐COVID”) for children and adolescents hospitalized with EtOH and methanol poisoning. For pediatric poisoning during COVID‐19, we also aimed to evaluate the cause of exposure by age and the clinical outcome.
METHODS
Design
This retrospective linkage study was carried out based on administrative data obtained from the LMO (see below) as well as hospitalization data collected from participating referral toxicology centers.
Setting
The study period was February 23 until June 22, 2020, which represents the initial 4 months of the COVID‐19 pandemic in Iran. Hospitalization and mortality data on alcoholic beverage and hand sanitizer exposure during the reference period, that is, the same period in the previous year (February 23 to June 22, 2019), were also obtained from both data sources for comparison.
Hospitalization data
Twelve major clinical toxicology centers across Iran were invited to participate in this study, among which nine referral toxicology centers across five cities accepted to contribute. These nine centers are all affiliated with local medical universities and are based in Tehran (Loghman Hakim Hospital), Isfahan (Khorshid, Alzahra, and Imam Hossein Hospitals), Mashhad (Imam Reza Hospital), Qazvin (Qods and Booali‐Sina Hospitals), and Ahvaz (Razi and Aboozar Hospitals).
Mortality data
The LMO is the national body responsible for conducting autopsies and issuing death certificates for any unnatural deaths, including poisoning cases. As such, the LMO conducts autopsies (and collects data) on corpses referred from toxicology centers, general hospitals, and the community (Kordrostami et al., 2017).
Participants
Inclusion criteria
All children and adolescents aged 0 to 18 years (McGoldrick, 1991) with (a) hospitalization due to alcohol (EtOH or methanol) exposure and/or (b) postmortem diagnosis of methanol poisoning during the study period were included.
Hospitalized cases at the nine referral toxicology centers were eligible if they had taken the sold product of alcoholic beverages usually used for recreational purposes and/or hand sanitizers used in an attempt to disinfect the body. History obtained from the patient or accompanying relatives determined the product that the patient was exposed to. In‐hospital diagnosis of EtOH poisoning was based on history and clinical presentation, as serum EtOH concentration cannot be routinely measured in an emergency condition.
The LMO established postmortem diagnosis of methanol poisoning (toxic alcohol) based on two criteria: (a) a serum methanol level >6.24 mmol/L (20 mg/dl) and/or (b) a high clinical suspicion of methanol exposure (gastrointestinal symptoms, visual disturbances, dyspnea, central nervous system signs/symptoms) with pH < 7.3 and serum bicarbonate <20 mmol/L (Hassanian‐Moghaddam et al., 2019).
Exclusion criteria
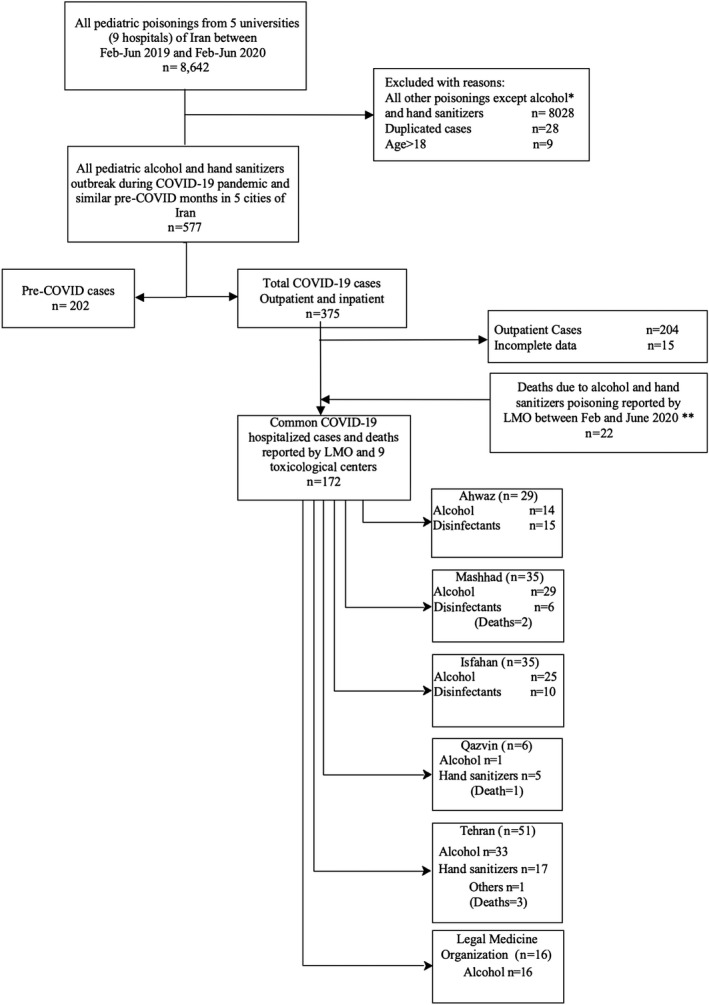
Patients with caustic ingestion and consumption of unknown substances were excluded. Hospitalized cases with duplicate, inaccurate, and missing data as well as outpatients with alcohol exposure were excluded (Figure (Figure1,1, see below).
Case matching
To identify fatal cases among those hospitalized, LMO data were matched to data from the clinical toxicology centers using the following patient identifiers: name, date of birth, and national identification number. Cases that could not be matched were either (1) out‐of‐hospital deaths (LMO data only) or (2) patients who were discharged from hospital (toxicology center data only) and thus survivors.
Comparator and interventions
Comparator
Data on alcoholic beverage and hand sanitizer exposures registered from February 23 to June 22, 2019 (“reference period”), were collected from toxicology referral centers and LMO.
Interventions
All hospitalized patients were managed for EtOH and methanol exposure based on the national guidelines and received hemodialysis treatment, if necessary.
Measures
Data from the two databases (LMO and clinical toxicology referral centers; see Table Table1;1; Figure Figure1)1) were extracted using a purpose‐developed study instrument which contained 21 items. The following data were recorded: patients’ demographic characteristics (including age, gender, city), the type of consumed substance (alcoholic beverage or hand sanitizer), route of exposure, and cause of exposure (accidental/recreational, suicidal). We also recorded the clinical manifestations on admission: Glasgow Coma Scale (GCS), vital signs, and routine laboratory tests, including venous blood gas (VBG) analyses. In terms of treatment, we recorded the need for intubation, the duration of hospital stay, and the final outcome (death, recovery with sequela, or complete recovery; Table Table22).
TABLE 1
Referrals of child and adolescent poisoning cases (pre‐ vs. during COVID‐19) from alcoholic beverages and/or hand sanitizer use in the poisoning referral centers (n = 8605)
| Center (cases) | Period |
Alcohol n (%) |
Other poisoning n (%) | p |
Hand sanitizer n (%) |
Other poisoning n (%) | p |
Alcohol + hand sanitizer n (%) |
Other poisoning n (%) | p |
OR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tehran (n = 1893) | Pre‐COVID‐19 | 46 (2.4) | 931 (49.2) | <0.001 | 7 (0.4) | 970 (51.2) | 0.195 | 53 (2.8) | 924 (48.8) | <0.001 |
2.4 [1.7, 3.4] |
| COVID‐19 | 99 (5.2) | 817 (43.2) | 12 (0.6) | 904 (47.8) | 111 (5.9) | 805 (42.5) | |||||
| Isfahan (n = 4020) | Pre‐COVID‐19 | 21 (0.5) | 1882 (46.8) | 0.025 | 48 (1.2) | 1855 (46.8) | 0.484 | 69 (1.7) | 1834 (45.6) | 0.053 | – |
| COVID‐19 | 42 (1.1) | 2075 (51.6) | 61 (1.5) | 2056 (51.1) | 103 (2.6) | 2014 (50.1) | |||||
| Ghazvin (n = 181) | Pre‐COVID‐19 | 11 (6.1) | 79 (43.6) | 0.311 | 21 (11.6) | 69 (38.1) | 0.334 | 32 (17.7) | 58 (32.0) | 0.110 | – |
| COVID‐19 | 16 (8.8) | 75 (41.4) | 27 (14.9) | 64 (35.4) | 43 (23.8) | 48 (26.5) | |||||
| Mashhad (n = 736) | Pre‐COVID‐19 | 17 (2.3) | 432 (58.7) | <0.001 | 9 (1.2) | 440 (59.8) | 0.693 | 26 (3.5) | 423 (57.5) | <0.001 | 2.6 [1.5,4.3] |
| COVID‐19 | 32 (4.3) | 255 (34.6) | 7 (1.0) | 280 (38.0) | 39 (5.3) | 248 (33.7) | |||||
| Ahwaz (n = 1775) | Pre‐COVID‐19 | 16 (0.9) | 790 (44.5) | <0.001 | 6 (0.3) | 800 (45.1) | 0.01 | 22 (1.2) | 784 (44.2) | <0.001 | 3.2 [2,5.1] |
| COVID‐19 | 57 (3.2) | 912 (51.3) | 22 (1.2) | 947 (53.4) | 79 (4.5) | 890 (50.1) | |||||
| Total (n = 8605) | Pre‐COVID‐19 | 111 (1.3) | 4114 (47.8) | <0.001 | 91 (1.1) | 4164 (48.2) | 0.017 | 202 (2.3) | 4023 (46.8) | <0.001 | 1.9 [1.6, 2.2] |
| COVID‐19 | 246 (2.9) | 4134 (48.0) | 129 (1.5) | 4251 (49.2) | 375 (4.4) | 4005 (46.5) | |||||
| Total | 357 (4.2) | 8248 (95.8) | – | 220 (2.6) | 8415 (97.4) | – | 577 (6.7) | 8028 (93.3) | – | – |
TABLE 2
Patient data during COVID‐19 pandemic considering ingestion source
| Variable | Alcohols (n = 118) | Sanitizers (n = 54) | p‐value |
|---|---|---|---|
| Gender | |||
| Male n (%) | 82.0 (69.5) a | 30.0 (55.6) | 0.075 |
| Female n (%) | 36.0 (30.5) | 24.0 (44.4) | |
| Age | |||
| <15 years n (%) | 59.0 (50.0) | 47.0 (87.0) | <0.001* |
| 15 to 18 years n (%) | 59.0 (50.0) | 7.0 (13.0) | |
| Outcome | |||
| Deaths n (%) | 21.0 (17.8) | 1.0 (3.6) | 0.002** |
| Discharge n (%) | 97.0 (82.2) | 53.0 (96.4) | |
| Systolic blood pressure (mmHg) | 110.0 [100.0 to 110.0] b | 100.0 [100.0 to 110.0] | 0.24 |
| Diastolic blood pressure (mmHg) | 70.0 [70.0 to 80.0] | 70.0 [60.0 to 71.2] | 0.09 |
| Respiratory rate (per min) | 18.0 [19.0 to 23.0] | 21.0 [18.0 to 24.0] | 0.18 |
| Pulse rate (per min) | 94.23±14.27 | 99.77±20.05 | 0.12 |
| O2 saturation of room air | 95.0 [95.0 to 98.0] | 95.0 [95.0 to 97.0] | 0.39 |
| Cr (umol/L) | 70.72 [53.04 to 10.61] | 61.88 [53.36 to 70.72] | 0.14 |
| Urea (mmol/L) | 6.78 [4.28 to 10.53] | 3.57 [3.21 to 9.28] | 0.02 |
| pH | 7.3 [7.1 to 7.4] | 7.3 [7.2 to 7.4] | 0.19 |
| Hco3 (mmol/L) | 20.4 [12.9 to 24.0] | 23.5 [21.0 to 26.0] | 0.02 |
| Na (mmol/L) | 139.0 [136.0 to 141.0] | 138.0 [136.0 to 138.0] | 0.41 |
| K (mmol/L) | 4.2 [3.9 to 4.8] | 4.2 [3.8 to 5.3] | 0.99 |
| Glucose (mmol/L) | 5.52 [4.76 to 6.58] | 5.88 [4.38 to 9.66] | 0.98 |
| Ca (mmol/L) | 8.65±1.45 c | 9.34±0.61 | 0.36 |
| pCO2 (kPa) | 4.56±1.33 | 5.07±1.33 | 0.07 |
Alcohol beverage exposure cases only
For cases of alcohol beverage poisoning (i.e., nonhand sanitizer exposure cases), we also recorded the time elapsed between consumption and hospital presentation (if available), previous history of alcohol consumption, serum methanol and EtOH levels (if available), the need for hemodialysis, and the number of hemodialysis sessions required per patient.
Data analysis
Data were analyzed using R3.3.1 software (R Foundation for Statistical Computing). For quantitative variables, the distribution of the data was examined using Shapiro–Wilk test. Independent T‐test was applied if variables were normally distributed. Mann–Whitney U test was used for nonnormally distributed data. For qualitative data, Chi‐square or Fisher's exact test was applied, all at a point of significance of p < 0.05. Odds ratio (95% CI) was applied to show the measures of association and related precision.
Ethics approval
This study was approved by our local ethics committee in Shahid Beheshti University of Medical Sciences (reference code: IR.SBMU.RETECH.REC. 1399.1336; project code: 24276). All study procedures were performed in accordance with relevant guidelines and regulations.
RESULTS
Identification of eligible cases
We assessed patients for their eligibility after receiving data from the 9 referral centers and LMO (see Table Table1).1). During the study period (2020, during COVID‐19) and the reference period (2019, pre‐COVID‐19), a total of n = 8605 pediatric poisoning cases were reported, including 577 alcoholic beverage and hand sanitizer exposures (6.7%; Table Table1).1). Out of these 577 cases, 375 cases occurred in during the 2020 study period and 202 cases during the 2019 reference period.
In total, the LMO reported 23 deaths from methanol poisoning, of which 22 deaths occurred in 2020 and one in 2019.
Among the 22 deaths that occurred in 2020, six deaths could be matched to the hospital records. Among the remaining 16 methanol poisoning deaths that were registered by LMO in 2020, two deaths happened at home, and 14 occurred in other hospitals in the country (see Table Table2;2; Figure Figure11).
Among these 375 alcoholic beverage exposures, which occurred during COVID‐19, full records (hospital data and LMO) were available for 172 cases (150 survivals + 22 deaths) and included in the study. For these 172 cases, hospital data only were available for the 150 surviving cases. For six deaths (matched cases), hospital and LMO data were available, whereas for the remaining 16 deaths hospital records were not available to us (i.e., did not occur at the nine referral centers).
Comparison of prevalence rates during COVID‐19 versus pre‐COVID data
The number of alcoholic beverage and hand sanitizer exposures was significantly higher (OR 1.9; 95% CI 1.6, 2.2; p < 0.001) during the COVID‐19 pandemic (n = 375) compared to the 2019 reference period (n = 202; Table Table11).
In addition, the number of alcoholic beverage exposures during the first 2 months of COVID‐19 pandemic (February 23 to April 22; n = 99) was significantly higher (p < 0.001) than during the last 2 months of the study period (April 23 to June 22; n = 19; see Table Table3).3). The rates of hand sanitizer exposures did not differ by month.
TABLE 3
Time‐dependent hospitalizations and deaths in nine referral poisoning hospitals and LMO during the COVID‐19 outbreak (February‐June 2020, n = 172)
| Time period | Alcohols (n = 118) | Hand sanitizers (n = 54) | p‐value | Deaths (n = 22) | Discharge (n = 150) | p‐value |
|---|---|---|---|---|---|---|
|
02/23 to 03/22 n (%) | 60.0 (50.8%) | 18.0 (33.4%) | <0.001 | 11.0 (50.0%) | 64.0 (42.6%) | 0.14 |
|
03/23 to 04/22 n (%) | 39.0 (33.1%) | 10.0 (18.5%) | 9.0 (40.9%) | 39.0 (26.0%) | ||
|
04/23 to 05/22 n (%) | 11.0 (9.3%) a , b | 14.0 (25.9%) | 1.0 (4.5%) | 28.0 (18.7%) | ||
|
05/23 to 06/22 n (%) | 8.0 (6.8%) a , b | 12.0 (22.2%) | 1.0 (4.5%) | 19.0 (12.7%) |
Route, amount, and cause of exposure
Out of the 172 included cases for the 2020 study period (see above), all exposures were due to ingestion. 118 were classified as alcoholic beverage exposure, and 54 were as hand sanitizer cases (Table (Table22).
Most cases (72; 57.1%) were considered accidental exposure. Six (4.8%) cases reported suicidal intent, of whom five were in the 15 to 18 years age category. The aim of ingestion was not declared in the remaining 46 cases.
Hospital records indicated that supermarkets (44 cases), street vendors (23 cases), and pharmacies (17 cases) were the three most common sources where parents/guardians had purchased the alcoholic beverages or hand sanitizers involved in pediatric exposure.
The amount of ingestion was available in 54 cases. Of whom the median [IQR] (min, max) volume was 10 ml [5, 20] (2, 500) in youngers and 275 [200, 500] (50, 1500) in 15 to 18 years age (p < 0.001).
Previous history of alcohol consumption was available in 100 cases. Of whom 22 (22%) have mentioned the history of alcohol drinking in which only two children were <15 years old with odds (95% CI) of 037 (0.008, 0.171, p < 0.001).
Cause of exposure by age
The mean age of the patients was 10.1 ± 6.8 years, ranging from 6 months to 18 years, during the COVID‐19 pandemic. Among the included 172 cases, 106 cases (61.6%) were younger than 15 years old, and 66 cases (38.4%) fell into the 15 to 18 years of age category.
The odds of hand sanitizer exposure were 6.7 times higher (95% CI 2.8, 16.1) among patients younger than 15 years of age (p < 0.001; see Table Table2)2) when compared to 15‐ to 18‐year‐old cases.
Presentation and clinical manifestations
The time between exposure and hospital admission was available in 67 cases, with a median [IQR] (min, max) time elapsed of 6 h [2, 24] (1, 72). The median [IQR] time elapsed was significant shorter among <15‐year‐olds compared to 15‐ to 18‐year‐olds (3 h [2, 8] (range 1, 72) vs. 20 h [6, 24] (range 1, 72), respectively, p < 0.001).
Among the sample of 172 patients, 64 (37.2%) cases had gastrointestinal symptoms. Of the GI symptoms, nausea and/or vomiting were predominant, observed in 57 of the 64 (89.1%), while abdominal pain was claimed in 18 of the 64 (28.1%). Twenty‐four patients (14%) complained of visual disturbances on arrival to medical facilities (of whom one was discharged with visual sequelae and one died due to methanol toxicity).
GCS data were available for only 113 (66.0%) of the 172 included cases. Of the 113 GCS recorded data, 101 (89.4%) patients were fully awake on presentation, while the remaining 12 patients had GCS scores between 3 and 12. Of whom seven patients underwent tracheal intubation.
Laboratory findings
Laboratory testing revealed significant differences only in the urea and HCO3 levels between alcohol‐poisoned and disinfectant‐poisoned patients (both p values were 0.02; Table Table2).2). Of note, there were significant differences in creatinine, urea, pH, HCO3, serum potassium, and serum glucose between the patients who recovered and those who died due to intoxication. Nonsurvivors had elevated mean glucose level (11.99 vs. 5.90 mmol/L), a lower pH, HCO3 and pulse rate, and a higher level of potassium, urea, and creatinine compared to the survivors (Table (Table44).
TABLE 4
Patients’ data during the COVID‐19 pandemic by outcome
| Variable | Deaths (n = 22) | Discharge (n = 150) | p‐value |
|---|---|---|---|
| Gender | |||
| Male n (%) | 16.0 (72.7) a | 96.0 (64.0) | 0.423 |
| Female n (%) | 6.0 (27.3) | 54.0 (36.0) | |
| Age | |||
| <15 years n (%) | 5.0 (22.7) | 101.0 (67.3) | <0.001* |
| 15 to 18 years n (%) | 17.0 (77.3) | 49.0 (32.7) | |
| Systolic blood pressure (mmHg) | 110.0 [92.5 to 128.5] b | 100.0 [100.0 to 110.0] | 0.38 |
| Diastolic blood pressure (mmHg) | 72.5 [67.5 to 81.2] | 70.0 [70.0 to 75.0] | 0.36 |
| Pulse rate (per min) | 82.0 ± 12.26 | 96.68 ± 16.02 | 0.03 |
| Respiratory rate (per min) | 19.33 ± 5.89 | 21.26 ± 4.45 | 0.32 |
| O2 saturation of room air | 94.5 [92.5 to 97.2] | 95.0 [95.0 to 97.0] | 0.31 |
| Cr (μmol/L) | 167.96 [123.76 to 344.76] | 61.88 [53.04 to 97.24] | <0.001 |
| Urea (mmol/L) | 14.99 [12.39 to 24.88] | 6.07 [3.57 to 9.28] | <0.001 |
| pH | 6.9 [6.5 to 7.1] | 7.3 [7.2 to 7.4] | <0.001 |
| HCO3 (mmol/L) | 5.1 [3.6 to 12.8] | 22.7 [15.0 to 24.0] | <0.001 |
| pCO2 (kPa) | 3.80 ± 2.55 | 4.71 ± 1.25 | 0.42 |
| K (mmol/L) | 4.9 [4.5 to 5.7] | 4.2 [3.8 to 4.6] | 0.02 |
| Na (mmol/L) | 144.33 ± 17.17 c | 138.03 ± 3.11 | 0.41 |
| Glucose (mmol/L) | 11.99 ± 1.42 | 5.90 ± 1.73 | <0.001 |
| Ca (mmol/L) | 8.20 ± 1.35 | 9.30 ± 0.59 | 0.15 |
Due to the lack of laboratory facilities in our hospitals, methanol and EtOH concentrations were recorded in only 35 and 12 cases, respectively. The median [IQR] levels were 0.27 [0.02, 0.92] (range: 0 to 6.36) mmol/L methanol and 1.95 [1.52, 11.50] (range: 0.65 to 37.97) mmol/L EtOH. Fatal cases had a higher level of methanol concentration compared to survivors (median [IQR] of 1.86 [0.48, 5.02] (range: 0 to 6.36) and 0.22 [0.02, 0.64] (range: 0.09 to 3.74) mmol/L; p = 0.017).
Treatment and follow‐up
Thirty‐one out of 156 hospitalized patients (19.9%) were dialyzed, of whom six were dialyzed twice due to persistent metabolic acidosis or visual disturbances concomitant with metabolic acidosis. The majority (25 cases; 80.6%) of hemodialysis was done on 15‐ to 18‐year‐old cases with an odds (95% CI) of 12.0 (4.3, 34.0; p < 0.001).
Intubation was done in seven cases, of whom six died. All 150 survivors were discharged with no sequelae, except for two cases. In one case, gastrointestinal hemorrhage occurred, and the other case had visual sequela. Patients younger than 15 years (101; 67.3%) were more likely to recover completely and be discharged than 15‐ to 18‐year‐olds (49.0; 32.7%; p < 0.001).
Clinical outcome
During the study period, 22 patients died. Twenty‐one cases died from methanol poisoning (due to alcoholic beverage ingestion), while 1 case died from ingestion of hand sanitizers. Fatal outcome was 11.5 times more common (95% CI 1.5, 87.7) in those who were exposed to alcohols rather than those exposed to hand sanitizers (p < 0.001, Table Table2).2). Two of the 22 deaths recorded by LMO occurred in the prehospital setting, that is, at home before receiving any medical care. Six deaths occurred among 156 patients treated in the nine referral toxicological centers in this study (case fatality rate of 3.8%), of whom two had no opportunity to undergo hemodialysis as they deteriorated extremely fast after admission. One other in‐hospital death occurred in a patient who was referred fully awake with headache and visual disturbances, but his condition gradually worsened, resulting in death.
Median [IQR] (min, max) duration of hospital stay was 24 h [12, 48] (6, 72).
The number of dead cases was 17 (77.3%) in 15‐ to 18‐year‐olds versus 5 (22.7%) in 0‐ to 15‐year‐olds (Table (Table44).
DISCUSSION
Our findings show that the rate of pediatric exposure from ingestion of alcoholic beverages and hand sanitizers was significantly increased in Iran during the first 4 months of the COVID‐19 pandemic, compared to the same period in the previous year. In total, 22 children and adolescents died of methanol poisoning during the COVID‐19 pandemic in Iran, of whom 20 died in hospitals and two died in the community before arriving at a treatment center.
Methanol outbreaks during the COVID‐19 pandemic were not confined to Iran. In the United States, the CDC reported that between May and June 2020, 15 adult patients in Arizona and New Mexico had ingested alcohol‐based hand sanitizers and were subsequently admitted to a hospital. Four patients died and three were discharged with vision impairment (Yip et al., 2020). There were also reports of a methanol poisoning outbreak in Turkey with 63 deaths within 11 days, likely from counterfeit alcohol (Dağ & Kara Aydın, 2020). However, to the best of our knowledge, no pediatric cases of methanol poisoning during COVID‐19 have been reported outside of Iran.
The pediatric exposures in our study co‐occurred with the spread of misinformation on Iranian social media at the start of the pandemic, suggesting that ingesting alcohol or hand sanitizers to “wash” the gastrointestinal tract could protect against COVID‐19. Most poisoned children and adolescents were referred during the initial 2 months of the COVID‐19 epidemic in Iran (February 23 to April 22), and, not surprisingly, most patients died during this period. The prevalence of exposures decreased after the Iranian methanol outbreak (which affected adults, adolescents, and children) received substantial media attention in March/April 2020.
Among the pediatric exposure cases in our study, almost two‐thirds (62%) were younger than 15 years old, with the remainder (38%) being 15 to 18 years old. The odds of hand sanitizer exposure were higher in those younger than 15 years, whereas alcohol poisoning and fatal outcome were more common in 15‐ to 18‐year‐olds.
Our high rates of hand sanitizer exposure among under 15‐year‐olds may reflect the fact that households were stockpiling hand sanitizers at the start of COVID‐19, which may have posed increased risk for unintentional toxicity among children (Hakimi & Armstrong, 2020). Disinfectant represents a common source of pediatric exposure, as many hand sanitizers contain up to 60 to 95% EtOH or isopropyl alcohol and often have artificially added scents that might be appealing to young children (Santos et al., 2017). For instance, a total of 70,669 hand sanitizer exposures in children aged ≤12 years were reported to the National Poison Data System in the United States during 2011 to 2014 (Santos et al., 2017).
Children are prone to experiencing complications from unintentional/accidental poisoning. Children are naturally curious and unaware of the consequences of exposure to toxic agents. Compared to adults (and adolescents), young children generally have a lower body weight and are therefore more vulnerable to exposure to such products, resulting in more severe intoxications (Peden et al., 2008; Yip et al., 2020).
It is generally assumed that young children, including infants, are at greater risk of developing complications from alcohol intoxication than older children and teenagers. Young children have decreased liver glycogen stores, which increase their risk of developing hypoglycemia, and have various pharmacokinetic parameters that make them more susceptible to development of alcohol toxicity (Madsen, 1990).
However, in our study, 15‐ to 18‐year‐olds, although fewer in number, had worse prognosis than under 15‐year‐olds. This is possibly because under 15‐year‐olds were exposed unintentionally to a lower amount of hand sanitizers and admitted sooner as they were under the care of adults, whereas 15‐ to 18‐year‐olds deliberately ingested alcoholic beverages (and in larger volume) and were admitted later. These prognostic factors have already been discussed in the literature (Kalkan et al., 2003). We could detect only 1 death due to hand sanitizers in the current study. The possibility of more EtOH concentrations in hand sanitizers, less ingested volume, and early admission through caring parents may explain lower mortality rate in nine referral centers (one out of 103 = 1%) in children under 15.
Accordingly, five out of the six cases who reported suicidal intent were in the 15‐ to 18‐year age category, including one fatal case (age: 17 years). The fatality rate of this group was five out of 53 cases (9.4%), which is similar to the average mortality of 9 to 14% in the current outbreak in the whole population (Hassanian‐Moghaddam et al., 2020). The higher metabolic acidosis in older children, the more evidence in favor of methanol poisoning with need for hemodialysis and higher mortality rate.
Our results support early findings by Gormley et al. who showed that older children were more likely to report intentional ingestion and to have adverse health effects and worse outcomes compared to younger children (Gormley et al., 2012).
Our study has several limitations. We requested data from 12 academic centers, but only nine centers agreed to cooperate with us. Our data are therefore likely not representative of the entire country. Also, due to the retrospective nature of the study, we had to contend with missing data. Another limitation concerned the lack of measurement of serum methanol and EtOH levels in most cases, even though we tried to compensate by evaluating VBGs and patients’ clinical presentation.
Acute methanol and EtOH intoxication may be indistinguishable early on, which suggests a risk of misclassification bias. Future research should focus on how monitoring of alcohol products and early warning systems can be established to prevent further toxic alcohol outbreaks.
CONCLUSION
COVID‐19 misinformation at the start of the pandemic in Iran was associated with poisonings from alcoholic beverage and hand sanitizers in children and adolescents, resulting in at least 22 fatalities in this age group. Parents need to be educated about the correct use of alcoholic sanitizers, with adult supervision and proper child safety precautions to prevent unintended adverse consequences.
Physicians should be trained to recognize the clinical manifestations of poisoning from toxic alcohols in order to initiate timely treatment and prevent long‐term morbidity or mortality.
ACKNOWLEDGMENTS
We would also like to show our gratitude to Somayeh Sohrabi, Social Determinants of Health Research Center, for her assistance with data entry. We wish to thank Legal Medicine Research Center for matching the death cases against hospital data.
Notes
Mahdavi, S. A. , Kolahi, A.‐A. , Akhgari, M. , Gheshlaghi, F. , Gholami, N. , Moshiri, M. , Mohtasham, N. , Ebrahimi, S. , Ziaeefar, P. , McDonald, R. , Tas, B. , Kazemifar, A. M. , Amirabadizadeh, A. , Ghadirzadeh, M. , Jamshidi, F. , Dadpour, B. , Mirtorabi, S. D. , Farnaghi, F. , Zamani, N. , & Hassanian‐Moghaddam, H. (2021). COVID‐19 pandemic and methanol poisoning outbreak in Iranian children and adolescents: A data linkage study. Alcoholism: Clinical and Experimental Research, 45, 1853–1863. 10.1111/acer.14680 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
REFERENCES
- CDC . (2019) How to Protect Yourself and Others Know how It Spreads, pp. 18–19. Available from: https://www.cdc.gov/coronavirus/2019‐ncov/prevent‐getting‐sick/prevention‐H.pdf [Accessed 22nd April 2021].
- Chang, A. , Schnall, A.H. , Law, R. , Bronstein, A.C. , Marraffa, J.M. , Spiller, H.A. et al. (2020) Cleaning and disinfectant chemical exposures and temporal associations with COVID‐19—National Poison Data System, United States, January 1, 2020–March 31, 2020. Morbidity and Mortality Weekly Report, 69, 496–498. [Europe PMC free article] [Abstract] [Google Scholar]
- Dağ, B. & Kara Aydın, H. (2020) Turkey: Police Seize Bootleg Alcohol, Nab 10 Suspects. [online] Aa.com.tr. Available from: https://www.aa.com.tr/en/turkey/turkey‐police‐seize‐bootleg‐alcohol‐nab‐10‐suspects/2011943 [Accessed 22nd April 2021].
- Delirrad, M. & Mohammadi, A.B. (2020) New methanol poisoning outbreaks in Iran following COVID‐19 pandemic. Alcohol and Alcoholism, 55, 347–348. [Europe PMC free article] [Abstract] [Google Scholar]
- Emmanuel, J. , Sriram, N. & Muthukaruppan, R. (2020) The COVID‐19 outbreak action plan for endoscopy services in a tertiary hospital in East Malaysia. Asian Journal of Research and Reports in Gastroenterology, 4, 1–7. [Google Scholar]
- Gharpure, R. , Hunter, C.M. , Schnall, A.H. , Barrett, C.E. , Kirby, A.E. , Kunz, J. et al. (2020) Knowledge and practices regarding safe household cleaning and disinfection for COVID‐19 prevention—United States, May 2020. Morbidity and Mortality Weekly Report, 69, 705–709. [Europe PMC free article] [Abstract] [Google Scholar]
- Gormley, N.J. , Bronstein, A.C. , Rasimas, J.J. , Pao, M. , Wratney, A.T. , Sun, J. et al. (2012) The rising incidence of intentional ingestion of ethanol‐containing hand sanitizers. Critical Care Medicine, 40, 290–294. [Europe PMC free article] [Abstract] [Google Scholar]
- Hakimi, A.A. & Armstrong, W.B. (2020) Hand Sanitizer in a Pandemic: Wrong Formulations in the Wrong Hands. Journal of Emergency Medicine, 59, 668–672. [Europe PMC free article] [Abstract] [Google Scholar]
- Hassanian‐Moghaddam, H. , Zamani, N. , Roberts, D.M. , Brent, J. , McMartin, K. , Aaron, C. et al. (2019) Consensus statements on the approach to patients in a methanol poisoning outbreak. Clinical Toxicology, 57, 1129–1136. [Abstract] [Google Scholar]
- Hassanian‐Moghaddam, H. , Zamani, N. , Kolahi, A.A. , McDonald, R. & Hovda, K.E. (2020) Double trouble: methanol outbreak in the wake of the COVID‐19 pandemic in Iran—a cross‐sectional assessment. Critical Care, 24, 10–12. [Europe PMC free article] [Abstract] [Google Scholar]
- Jairoun, A.A. , Al‐Hemyari, S.S. & Shahwan, M. (2021) The pandemic of COVID‐19 and its implications for the purity and authenticity of alcohol‐based hand sanitizers: The health risks associated with falsified sanitisers and recommendations for regulatory and public health bodies. Research in Social and Administrative Pharmacy, 17, 2050–2051. 10.1016/j.sapharm.2020.04.014 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Kalkan, S. , Cevik, A.A. , Cavdar, C. , Aygoren, O. , Akgun, A. , Ergun, N. , & Tuncok, Y. (2003) Acute methanol poisonings reported to the Drug and Poison Information Center in Izmir, Turkey. Vet Hum Toxico, 45(6), 334–337. PMID: 14640491. [Abstract] [Google Scholar]
- Kampf, G. , Scheithauer, S. , Lemmen, S. , Saliou, P. & Suchomel, M. (2020) COVID‐19‐associated shortage of alcohol‐based hand rubs, face masks, medical gloves and gowns–proposal for a risk‐adapted approach to ensure patient and healthcare worker safety. Journal of Hospital Infection, 105, 424–427. [Europe PMC free article] [Abstract] [Google Scholar]
- Kordrostami, R. , Akhgari, M. , Ameri, M. , Ghadipasha, M. & Aghakhani, K. (2017) Forensic toxicology analysis of self‐poisoning suicidal deaths in Tehran, Iran; trends between 2011–2015. DARU Journal of Pharmaceutical Sciences, 25, 15. [Europe PMC free article] [Abstract] [Google Scholar]
- Madsen, L.P. (1990) Acute alcohol intoxication in children. Diagnosis, treatment and complications. Ugeskrift for Laeger, 152, 2362–2364. [Abstract] [Google Scholar]
- McGoldrick, D. (1991) The United Nations Convention on the rights of the Child. International Journal of Law, Policy and the Family, 5, 132–169. [Google Scholar]
- Peden, M. , Oyegbite, K. , Ozanne‐Smith, J. et al. (Eds.). (2008) World report on child injury prevention. Geneva: World Health Organization. 6, Poisoning. Available from: https://www.ncbi.nlm.nih.gov/books/NBK310644/ [Accessed 22nd April 2021]. [Abstract] [Google Scholar]
- Rostrup, M. , Edwards, J.K. , Abukalish, M. , Ezzabi, M. , Some, D. , Ritter, H. et al. (2016) The methanol poisoning outbreaks in Libya 2013 and Kenya 2014. PLoS One, 11, 1–10, e0152676. [Europe PMC free article] [Abstract] [Google Scholar]
- Santos, C. , Kieszak, S. , Wang, A. , Law, R. , Schier, J. & Wolkin, A. (2017) Reported adverse health effects in children from ingestion of alcohol‐based hand sanitizers—United States, 2011–2014. Morbidity and Mortality Weekly Report, 66, 223–226. [Europe PMC free article] [Abstract] [Google Scholar]
- Soltaninejad, K. (2020) Methanol mass poisoning outbreak, a consequence of COVID‐19 pandemic and misleading messages on social media. International Journal of Occupational and Environmental Medicine, 11, 148–150. [Europe PMC free article] [Abstract] [Google Scholar]
- WHO . (2020a) Coronavirus Disease 2019 Situation Report 51—11th March 2020’, WHO Bulletin, 2019 (March), p. 2633. Available from: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019 [Accessed 22nd April 2021].
- World Health Organization . (2020b) Weekly epidemiological and operational updates September 2020. Coronavirus disease 2019 (COVID‐19). Retrieved from: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports [Accessed 22nd April 2021].
- Yip, L. , Bixler, D. , Brooks, D.E. , Clarke, K.R. , Datta, S.D. , Dudley, S. Jr. et al. (2020) Serious adverse health events, including death, associated with ingesting alcohol‐based hand sanitizers containing methanol—Arizona and New Mexico, May–June 2020. Morbidity and Mortality Weekly Report, 69, 1070–1073. [Europe PMC free article] [Abstract] [Google Scholar]
Full text links
Read article at publisher's site: https://doi.org/10.1111/acer.14680
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8653331
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/113085733
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1111/acer.14680
Article citations
Suicide Risk Factors in High School Students.
Int J Environ Res Public Health, 21(8):1055, 12 Aug 2024
Cited by: 0 articles | PMID: 39200665 | PMCID: PMC11354979
Beyond misinformation: developing a public health prevention framework for managing information ecosystems.
Lancet Public Health, 9(6):e397-e406, 20 Apr 2024
Cited by: 3 articles | PMID: 38648815 | PMCID: PMC11369959
Review Free full text in Europe PMC
An Outbreak of Home Distillation Methanol Poisoning in Turkey During the COVID-19 Pandemic: A Single Center Experience.
Arch Iran Med, 27(3):151-158, 01 Mar 2024
Cited by: 0 articles | PMID: 38685840 | PMCID: PMC11097313
Changes in emergency department visits and mortality during the COVID-19 pandemic: a retrospective analysis of 956 hospitals.
Arch Public Health, 82(1):5, 12 Jan 2024
Cited by: 3 articles | PMID: 38216989 | PMCID: PMC10785366
Mobile Apps Aimed at Preventing and Handling Unintentional Injuries in Children Aged <7 Years: Systematic Review.
Interact J Med Res, 12:e45258, 06 Sep 2023
Cited by: 0 articles | PMID: 37672312 | PMCID: PMC10512123
Review Free full text in Europe PMC
Go to all (13) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
A cross-sectional multicenter linkage study of hospital admissions and mortality due to methanol poisoning in Iranian adults during the COVID-19 pandemic.
Sci Rep, 12(1):9741, 13 Jun 2022
Cited by: 2 articles | PMID: 35697919 | PMCID: PMC9189800
Serious Adverse Health Events, Including Death, Associated with Ingesting Alcohol-Based Hand Sanitizers Containing Methanol - Arizona and New Mexico, May-June 2020.
MMWR Morb Mortal Wkly Rep, 69(32):1070-1073, 14 Aug 2020
Cited by: 43 articles | PMID: 32790662 | PMCID: PMC7440116
Death by hand sanitizer: syndemic methanol poisoning in the age of COVID-19.
Clin Toxicol (Phila), 59(11):1009-1014, 23 Mar 2021
Cited by: 6 articles | PMID: 33755514
Awareness raising and dealing with methanol poisoning based on effective strategies.
Environ Res, 228:115886, 16 Apr 2023
Cited by: 1 article | PMID: 37072082
Review
Funding
Funders who supported this work.
Shahid Beheshti University of Medical Sciences (1)
Grant ID: 24276
 2
,
12
2
,
12