Abstract
Background
The unprecedented increase in critically ill patients due to the COVID-19 pandemic mandated rapid training in critical care for redeployed staff to work safely in intensive care units (ICU).Methods
The COVID-19 ICU Remote-Learning Course (CIRLC) is a remote delivery course developed in response to the pandemic. This was a one-day course focused on the fundamentals of Intensive Care. The course used blended learning with recorded lectures and interactive tutorials delivered by shielding and frontline ICU trained professionals. The course was developed within one week and piloted at three NHS Trusts. It was then made publicly available free of charge to redeployed healthcare professionals across the UK and Ireland. An iterative cycle of improvement was used to update the course content weekly. A course confidence questionnaire with quantitative and qualitative questions was used to evaluate effectiveness. Data is reported as n (%), means (SD) and thematic analysis was used for the open questions.Results
1,269 candidates from 171 organisations completed the course, with 99 volunteer trainers. 96% of respondents rated the course as very or extremely useful. 86% rated the online platform as excellent. Overall confidence improved from 2.7/5 to 3.9/5. Qualitative data showed that the course was pitched at the appropriate level, accessible and built clinicians confidence to work in intensive care.Conclusion
This model of educational delivery with a rapid iteration cycle was a pragmatic, effective solution to knowledge-based training under social distancing measures. Whilst full course evaluation was not possible, we believe that this work demonstrates practical guidance on educational response in a pandemic as well as highlighting the altruistic nature of the critical care community.Free full text
Covid-19 ICU remote-learning course (CIRLC): Rapid ICU remote training for frontline health professionals during the COVID-19 pandemic in the UK
Abstract
Background
The unprecedented increase in critically ill patients due to the COVID-19 pandemic mandated rapid training in critical care for redeployed staff to work safely in intensive care units (ICU).
Methods
The COVID-19 ICU Remote-Learning Course (CIRLC) is a remote delivery course developed in response to the pandemic. This was a one-day course focused on the fundamentals of Intensive Care. The course used blended learning with recorded lectures and interactive tutorials delivered by shielding and frontline ICU trained professionals. The course was developed within one week and piloted at three NHS Trusts. It was then made publicly available free of charge to redeployed healthcare professionals across the UK and Ireland. An iterative cycle of improvement was used to update the course content weekly. A course confidence questionnaire with quantitative and qualitative questions was used to evaluate effectiveness. Data is reported as n (%), means (SD) and thematic analysis was used for the open questions.
Results
1,269 candidates from 171 organisations completed the course, with 99 volunteer trainers. 96% of respondents rated the course as very or extremely useful. 86% rated the online platform as excellent. Overall confidence improved from 2.7/5 to 3.9/5. Qualitative data showed that the course was pitched at the appropriate level, accessible and built clinicians confidence to work in intensive care.
Conclusion
This model of educational delivery with a rapid iteration cycle was a pragmatic, effective solution to knowledge-based training under social distancing measures. Whilst full course evaluation was not possible, we believe that this work demonstrates practical guidance on educational response in a pandemic as well as highlighting the altruistic nature of the critical care community.
Background
The COVID-19 pandemic pushed healthcare services to their limit with 6.4 million confirmed cases, and 383,262 deaths worldwide 1 within six months. This led to 12,086 intensive care unit (ICU) admissions in the United Kingdom (UK) alone during that period. 2 However, the UK has one of the lowest numbers of ICU beds per capita in Europe, with only 6.6 beds per 100,000 in 2012, compared to an average of 11.5 per 100,000. 3 This surge demanded an increased ICU capacity requiring appropriately trained staff. The workforce expansion included redeployment of non-ICU health professionals, creating a substantial need for rapid, effective training. Conventional face-to-face training was challenging due to social distancing measures, the lack of available trainers, and demand urgency.
Concurrently, experienced ICU staff with a wealth of knowledge were confined to their homes due to government guidance on self-isolation and shielding. The objective of the presented programme was to rapidly develop and scale an interactive distance learning programme that was compliant with social distancing, but also harnessed the unique opportunities and expertise it serendipitously afforded.
Methods
On 18th March 2020 authors EC, AMo and MC from Brunel University London
(www.brunel.ac.uk) and 33 N Ltd. (https://33n.co.uk/home) had a
virtual meeting to discuss how both organisations may be able to assist in the COVID
response following collaboration with the Northwest London Critical Care Network
(NWLCCN). We recognised that there was a high work burden of in-house training for
redeployed staff that was being implemented within local hospitals by frontline
clinicians. Concurrently, scores of highly skilled critical care staff were
shielding at home unable to work on the frontline. We identified that mobilising
these staff to assist in teaching frontline clinicians using a remote format may
help to off load the work burden of frontline clinicians whilst allowing educational
delivery that conformed to social distancing rules.
N Ltd. (https://33n.co.uk/home) had a
virtual meeting to discuss how both organisations may be able to assist in the COVID
response following collaboration with the Northwest London Critical Care Network
(NWLCCN). We recognised that there was a high work burden of in-house training for
redeployed staff that was being implemented within local hospitals by frontline
clinicians. Concurrently, scores of highly skilled critical care staff were
shielding at home unable to work on the frontline. We identified that mobilising
these staff to assist in teaching frontline clinicians using a remote format may
help to off load the work burden of frontline clinicians whilst allowing educational
delivery that conformed to social distancing rules.
The result was the rapid development of a 1-day online course developed and delivered by clinicians and academics specialising in intensive care. The process and principles that resulted in this development are detailed below.
Underpinning educational principles
Computer-based technology using online learning content is widely used in undergraduate and postgraduate medical education. For example, to support training for healthcare professionals, the NHS has invested heavily in a web-based e-learning platform http://www.e-lfh.org.uk. Educational packages with a “drill-and-practice” approach can be highly efficient for skill-based training such as x-ray interpretation and drug prescribing. 4 However, without interaction with the teacher and other students, learners may feel unmotivated and unsupported. Moreover, the typical lecture followed by homework elements of a course can make the learning experience isolating and impersonal.
Blended learning offers a solution to these problems by combining pre-recorded lectures to be watched by students and assimilation of knowledge through focused group discussion lead by field experts. This ‘flipped classroom’ model contrasts with the traditional model of learning where first exposure to knowledge occurs inside the classroom with further consolidation and application of knowledge achieved through individual learning. 5 The ‘flipped’ approach not only promotes a more personalised learning experience with expert support readily available, but also encourages peer interaction and collaboration.4,6
The overall development of the course was also guided by general standards of course design (e.g. Quality Matters rubric https://www.qualitymatters.org/qa-resources/rubric-standards/higher-ed-rubric) including consideration and alignment of course overview, learning objectives, instructional material, learner interactions, course technology and usability and learner support. Due to the nature of the pandemic and pressure on staff time, assessment of knowledge and implementation in practice was not practicable and subsequently not included.
Content development
The first step was to identify the target audience for the course and to develop the
core content. We liaised with local NHS trusts to identify the staff groups that
were being redeployed- in the early days of the pandemic this was theatre nurses,
operating department technicians, junior doctors and surgeons. We contacted NWLCCN,
practice educators and frontline clinicians to determine the essential
knowledge aspects of critical care that the course could
address. These were: an introduction to COVID-19, ICU monitoring, mechanical
ventilation, acute respiratory distress syndrome (ARDS), basics of good ICU care,
and sedation and vasoactive medication. As time progressed physiotherapists were
also being redeployed at haste, so further meetings with clinical specialist
physiotherapists (n =
= 7) took place to establish core physiotherapy content and the
latter two topics were replaced with physiotherapy assessment, and physiotherapy
management of the COVID-19 patient. This resulted in three course streams aimed at
nurses, doctors and physiotherapists. A second course which focused on
rehabilitation was added at a later date but is not reported here.
7) took place to establish core physiotherapy content and the
latter two topics were replaced with physiotherapy assessment, and physiotherapy
management of the COVID-19 patient. This resulted in three course streams aimed at
nurses, doctors and physiotherapists. A second course which focused on
rehabilitation was added at a later date but is not reported here.
Session plans and learning objectives for each topic and for each profession were developed by the core faculty (MC, AMo, AW and EC) comprised of lecturers in critical care from nursing and physiotherapy backgrounds and intensive care doctors, EC, MC and AW are also Fellows of the Higher Education Academy. An example of the learning objectives for the nursing course is shown in Table 1.
Table 1.
Learning objectives for nursing specific course.
| Topic | Learning objective |
|---|---|
| ICU monitoring and interpretation | • Know what monitoring ICU patients will need Know what monitoring ICU patients will need•  Know how
to incorporate the monitoring into my assessment Know how
to incorporate the monitoring into my assessment•  Know
what essential parameters to act upon Know
what essential parameters to act upon |
Basics of good ICU care | • Know what basic care needs should be addressed
daily Know what basic care needs should be addressed
daily•  Know what tools and bundles I can use in
ICU Know what tools and bundles I can use in
ICU•  Know how I will work within the ICU team
effectively Know how I will work within the ICU team
effectively |
Basics of ventilation | • Know what to look for when assessing a patient on a
ventilator Know what to look for when assessing a patient on a
ventilator•  How to look at a ventilator and change its
setting How to look at a ventilator and change its
setting•  Know what interventions I can consider Know what interventions I can consider |
ARDS management | • Know the basic pathophysiology of ARDS Know the basic pathophysiology of ARDS •  Know what the
key areas of ARDS management are Know what the
key areas of ARDS management are•  Know what you can do
to monitor for deterioration and help optimize the
management Know what you can do
to monitor for deterioration and help optimize the
management |
Vasoactive and sedative drugs | • Know how to use and deliver the common vasoactive
drugs Know how to use and deliver the common vasoactive
drugs•  Know how to use and deliver the common sedative
drugs Know how to use and deliver the common sedative
drugs•  Know how to monitor sedation levels Know how to monitor sedation levels |
To address these learning objectives, we used a blended learning model combining a
series of online lectures written and pre-recorded by topic experts (PS, AW, JB, TM,
EC, MJ and AH). These were followed by case-based interactive tutorials on the same
topic delivered to profession-specific tutorial groups of up to 20 by experienced
volunteer ICU staff. Lectures and tutorials lasted around 30 minutes each.
minutes each.
Technical set up
The course utilised technology donated by Blackboard Learn Online (BBL) (https://www.blackboard.com/teaching-learning/learning-management/blackboard-learn) integrating pre-recorded lectures recorded on panopto™ software (https://www.panopto.com/), with online resources, and ‘collaborate’ room function. The collaborate rooms enabled candidates to speak directly to tutors and each other using audio or text functions. This allowed candidates to consolidate their learning whilst drawing on the tutors’ practical expertise.
Administrative support was provided from 33 N Ltd., and the technological support
from Brunel University London.
N Ltd., and the technological support
from Brunel University London.
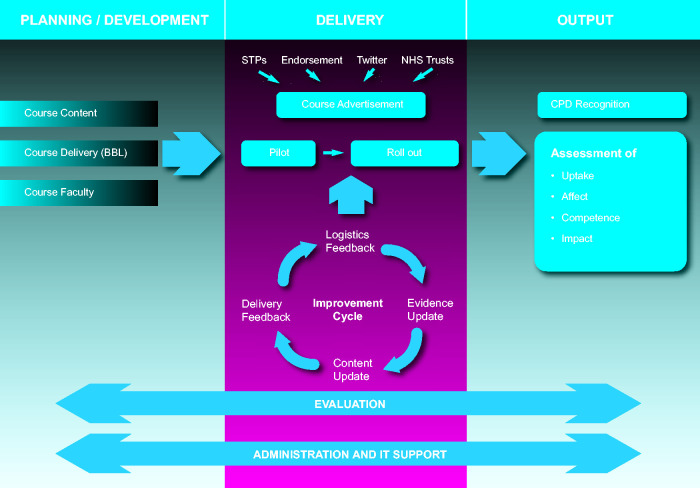
Course registration and advertising
There were two routes to both register for the course and to volunteer as a tutor.
Marketing material was developed and distributed via formal and informal networks to
recruit candidates and faculty. Formal networks included liaising directly with NHS
Trusts and Sustainability and Transformation Partnerships (STPs), and advertising
via the Intensive Care Society and The Association of Physiotherapists in
Respiratory Care. In addition, we launched a course Twitter™ account (@IcuRemote)
which has n =
= 1,098 followers to date to advertise for both tutors and
candidates.
1,098 followers to date to advertise for both tutors and
candidates.
A total of 99 experienced ICU staff consisting of frontline, self-isolating or shielding clinicians and academics taught on the course. To maintain high standards, we reviewed tutors’ credentials and used a train the trainer system to teach on the course. In order to teach on the course, we requested that all physiotherapists and nurses worked at Senior (Agenda for Change Band 6) level or above in ICU or had an academic role delivering ICU education. All tutors were registered with their professional body. All doctors had at least 3 years’ experience working in an ICU. Demographics of the tutors are shown in Table 2.
Table 2.
Demographics of course tutors (n =
= 99).
99).
| Job role | n | % |
|---|---|---|
| Consultant in anaesthesia/emergency medicine | 6 | 5.94 |
| Band 7 physiotherapist | 17 | 16.83 |
| Band 6 physiotherapist | 1 | 0.99 |
| Band 8 nurse | 1 | 0.99 |
| Band 7 nurse | 3 | 2.97 |
| Band 6 nurse | 1 | 0.99 |
| Band 8 nurse | 2 | 1.98 |
| Core trainee in anaesthetics | 4 | 3.96 |
| Specialist trainee 3–4 in anaesthetics | 2 | 1.98 |
| Specialist trainee 5+ in anaesthetics | 5 | 4.95 |
| 11 | 10.89 | |
| 9 | 8.91 | |
| 8 | 7.92 | |
| Professor of nursing | 2 | 1.98 |
| Senior lecturer – critical care | 5 | 4.95 |
| Lecturer – critical care | 1 | 0.99 |
| Practice development nurse/practice educator | 5 | 4.95 |
| Resuscitation officer | 1 | 0.99 |
| Critical care nurse (band not available) | 8 | 7.92 |
| Critical care doctor (band not available) | 5 | 4.95 |
| ‘ICU trust grade’ | 1 | 0.99 |
| ‘ICU registrar’ | 1 | 0.99 |
All new tutors were paired with core faculty or experienced tutors to observe the tutorials first before delivering them themselves. They were then observed by experienced faculty delivering the sessions. All sessions had two tutors for quality assurance and in case of sickness absence. If any concerns were noted about the quality of tutoring then the tutors were removed from the faculty.
Organisational structure
A course team was created to manage ongoing organisational refinement including
administration, IT support, content and tutors. Continual engagement with Trusts and
social media facilitated the training of large cohorts of staff. The course was
endorsed by the Intensive Care Society (https://www.ics.ac.uk/). The
course was a multi-organisational collaboration between Brunel University London,
33 N Ltd, and Blackboard, and piloted within a week of its conception.
N Ltd, and Blackboard, and piloted within a week of its conception.
Improvement cycle
The rapidly emerging information during the pandemic, and the course format, required a rapid cycle of iteration. Daily interactive feedback sessions with tutors and candidates were used to enable rapid improvement of course structure, user interface and administration. Course content leads were appointed for each stream to review and update the course material weekly to reflect candidate feedback and new clinical guidance. For example, prone positioning of the awake patient was integrated into the course content as this treatment strategy emerged during the pandemic.
Delegate evaluation methodology
From the outset, candidates were asked to give a global score on the course usefulness and use of platform via an online form. After two weeks a more formal evaluation was undertaken with a course questionnaire administered before and after the course (online Appendix A). Its development was informed by Sitzman & Weinhardt, 7 focusing on training utilization (including demographic data on course attendees), training affect and performance indicators (specifically confidence of application to practice). Candidates were given timetabled time during the course to complete this. The questionnaire was hosted on onlinesurveys.ac.uk and submissions were anonymized.
The questionnaire data were predominantly analysed using descriptive statistics. Open comments were invited regarding participants experience of the course and this qualitative data were transferred onto a word document. They were analysed through inductive descriptive thematic analysis. 8 This is an atheoretical approach suitable for a pragmatic evaluation. The process included familiarization of the data, line coding, collation of subthemes and thematic development. Analysis was completed by one experienced researcher who was independent to the teaching of the course (MN). The candidate themes were discussed with other members of the evaluation team who were involved in verbal feedback from participants to ensure resonance prior to confirmation.
The process of course development, delivery and evaluation is displayed diagrammatically in Figure 1.
Funding
The course was provided free to all participants. The organisations donated their
employees’ time and software to design, build and hold the structure of the course,
at an estimated combined cost of £102,700. The course was then delivered through
approximately 3,808 hours of volunteer tutors time, approximating a value of
£88,148. The course was designed in a modular fashion to enable rapid scalability,
with the estimated cost at between £60 and £100 per person.
hours of volunteer tutors time, approximating a value of
£88,148. The course was designed in a modular fashion to enable rapid scalability,
with the estimated cost at between £60 and £100 per person.
The outcome
Demographics and course attendance
The course ran 36 times from 25th of March 2020 to 27th of May 2020 and was accessed by 1,269 candidates from 171 healthcare organisations in the UK and Ireland. Attendance ranged from 60-200 candidates/day. Of these, 1,027 completed basic demographic data demonstrating a professional spread of 476 (46%) Physiotherapists, 249 (24%) Doctors, 234 (23%) Nurses, and 68 (7%) unspecified.
More detailed demographic information was available from the 210 participants who completed the pre-post questionnaire and these are shown in Table 3. Of note 32 areas of clinical specialty were represented and 154 (73%) of candidates had either no or <6 months experience on ICU/HDU.
Table 3.
Candidate demographic data.
| Number | % | |
|---|---|---|
| Profession | ||
 Doctor Doctor | 27 | 12.86 |
 Nurse Nurse | 70 | 33.33 |
 Physiotherapist Physiotherapist | 102 | 48.57 |
 Other Other | 11 | 5.24 |
| Area of practice | ||
 Acute internal medicine Acute internal medicine | 14 | 6.67 |
 Anaesthetics Anaesthetics | 5 | 2.38 |
 Cardio-thoracic surgery Cardio-thoracic surgery | 9 | 4.29 |
 Cardiology Cardiology | 9 | 4.29 |
 Emergency medicine Emergency medicine | 6 | 2.86 |
 General (internal) medicine General (internal) medicine | 8 | 3.81 |
 General practice General practice | 3 | 1.43 |
 General surgery General surgery | 17 | 8.10 |
 Geriatric medicine Geriatric medicine | 10 | 4.76 |
 Infectious diseases Infectious diseases | 5 | 2.38 |
 Intensive care medicine Intensive care medicine | 20 | 9.53 |
 Neurology Neurology | 21 | 10.00 |
 Neurosurgery Neurosurgery | 5 | 2.38 |
 Rehabilitation medicine Rehabilitation medicine | 13 | 6.19 |
 Respiratory medicine Respiratory medicine | 36 | 17.14 |
 Sport and exercise medicine Sport and exercise medicine | 3 | 1.43 |
 Trauma and orthopaedic surgery Trauma and orthopaedic surgery | 9 | 4.29 |
 Othera Othera | 17 | 8.15 |
| Clinical grade | ||
 Band 1–4 Band 1–4 | 3 | 1.44 |
 Band 5 Band 5 | 99 | 47.14 |
 Band 6 Band 6 | 63 | 30.00 |
 Band 7 Band 7 | 15 | 7.14 |
 Band 8 Band 8 | 4 | 1.90 |
 Foundation trainee Foundation trainee | 21 | 1.00 |
 ST1–2ST3-4 ST1–2ST3-4 | 3 | 1.43 |
 ST5+ ST5+ | 2 | 0.95 |
 Consultant Consultant | 1 | 0.48 |
| Prior experience in ICU/HDU | ||
 Nil Nil | 72 | 34.30 |
 <6 <6 months months | 82 | 39.04 |
 6 6 months–2 months–2 years years | 29 | 13.81 |
 >2 >2 years years | 27 | 12.86 |
| Last worked in ICU/HDU | ||
 <1 <1 year ago year ago | 92 | 43.81 |
 1–2 1–2 years ago years ago | 20 | 9.52 |
 3–5 3–5 years ago years ago | 7 | 3.33 |
 >5 >5 years ago years ago | 11 | 5.24 |
 Never Never | 80 | 38.10 |
| New proposed role | ||
 ICU/HDU in my current hospital ICU/HDU in my current hospital | 166 | 79.05 |
 ICU/HDU at a Nightingale hospital ICU/HDU at a Nightingale hospital | 1 | 0.48 |
 ICU/HDU in another hospital ICU/HDU in another hospital | 8 | 3.81 |
 Other Other | 35 | 16.67 |
aOther included: obstetrics & gynaecology, occupational medicine, maxillofacial surgery, otolaryngology, paediatric cardiology, paediatrics, plastic surgery, public health medicine, clinical genetics, clinical neurophysiology, clinical pharmacology and therapeutics, clinical psychiatry and heamatology, clinical oncology.
Evaluation results
Quantitative data
Of the 1,027 candidates who completed the global evaluation, 96% of respondents rated the overall course as very or extremely useful. 86% rated the online platform as excellent.
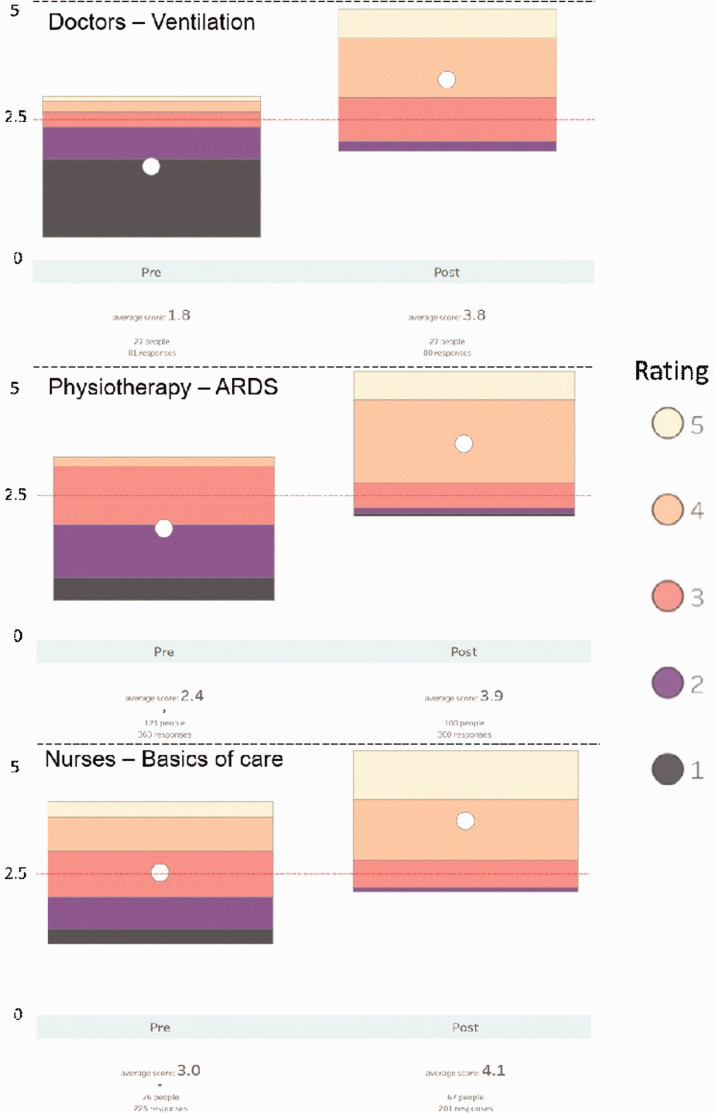
The questionnaire results, from 210 participants, demonstrate increased overall confidence for all professions- pre-course mean confidence of 2.7/5, post-course mean 3.9/5 (Table 4). While this pattern was broadly replicated differences in topic and profession were noted (Figure 2).
Table 4.
Changes in confidence by topic and profession.
| Before, group mean (SD) | After, group mean (SD) | Mean difference | |
|---|---|---|---|
| Doctors’ confidence increase in Likert scale by topic | |||
 Monitoring and interpretation in ICU Monitoring and interpretation in ICU | 3.15 (1.0) | 4.17 (0.62) | 1.02 |
 Basics of good ICU Care Basics of good ICU Care | 2.66 (1.07) | 4.04 (0.66) | 1.38 |
 Ventilation Ventilation | 1.81 (1.12) | 3.76 (0.84) | 1.95 |
 ARDS ARDS | 2.09 (1.12) | 3.68 (0.77) | 1.58 |
 Vasoactive and sedative drugs in ICU Vasoactive and sedative drugs in ICU | 2.17 (1.24) | 3.85 (0.78) | 1.68 |
| Nurses’ confidence increase in Likert scale by topic | |||
 Basics of good ICU Care Basics of good ICU Care | 3.08 (1.00) | 3.94 (0.76) | 0.85 |
 Monitoring and interpretation in ICU Monitoring and interpretation in ICU | 3.02 (1.14) | 4.09 (0.81) | 1.07 |
 Ventilation Ventilation | 2.67 (1.00) | 3.70 (0.83) | 1.03 |
 ARDS ARDS | 2.39 (1.11) | 3.45 (0.77) | 1.06 |
 Vasoactive and sedative drugs in ICU Vasoactive and sedative drugs in ICU | 2.60 (1.15) | 3.64 (0.96) | 1.04 |
| Physiotherapists’ confidence increase in Likert scale by topic | |||
 Monitoring and interpretation in ICU Monitoring and interpretation in ICU | 3.07 (0.89) | 4.22 (0.73) | 1.15 |
 Physiotherapy assessment of critically ill patients Physiotherapy assessment of critically ill patients | 3.06 (0.83) | 4.26 (0.74) | 1.20 |
 Physiotherapy management Physiotherapy management | 2.38 (0.84) | 3.90 (0.81) | 1.52 |
 Ventilation Ventilation | 3.47 (0.89) | 4.40 (0.68) | 0.93 |
 ARDS ARDS | 2.91 (0.84) | 4.26 (0.73) | 1.35 |
| Likert scale confidence increase by prior ICU experience (all professions and topics) | |||
 None None | 2.61 (1.15) | 3.90 (0.88) | 1.29 |
 Less than 6 Less than 6 months months | 2.77 (1.00) | 3.99 (0.79) | 1.22 |
 6 6 months to 2 months to 2 years years | 2.91 (1.07) | 4.10 (0.75) | 1.19 |
 More than 2 More than 2 years years | 4.30 (0.97) | 4.43 (0.65) | 0.13 |
Qualitative questionnaire results
Themes included the pitch of the material, tutor expertise, forum accessibility including BBL, the approachability of the tutors, building confidence in practice and the course as a platform for further learning. Details of each theme and supporting quotes are shown in Table 5.
Table 5.
Derived these from open questions.
| Theme | Subthemes | Example quotes |
|---|---|---|
| Pitched at an appropriate level | Previous exposure helps engagement | “I found the course very informative and I feel would benefit all of us who have had no experience in ICU but have been working within that environment. To me it was enough without going over board.” |
| Led by experts in the field | “Very informative and well led. Amazing lectures and team”
“Really enjoyed the course and all speakers were very knowledgeable and were able to clearly explain content.” “Excellent course. Superb resources. Experts in their field. “ “The facilitators of the physio tutorials were excellent - demonstrated an amazing knowledge and keen for group discussion” “All tutors were very knowledgeable and explained things very clearly!” | |
| Accessible forum | BBL generally easy to engage with | “I cannot tell you how brilliant this has been for me and I
honestly think I am converted to web based training and
would consider an annual course like this as part of
maintaining my respiratory competencies” “I found the Blackboard software very easy to use and didn't have any issues.” “It's a great way of learning, I stopped a couple of the presentations to make notes, so I never missed bits and rewind things I didn't understand” |
| Useful to have later access | “Worked well, good to have information available for a
number of months to recap during this time, good to have
opportunity to ask questions.” “Very full day but super helpful to have the resources available for after” “I will go back at lectures to re visit especially the ventilator lecture as this is where my knowledge is slightly weaker.” | |
| A few technical issues could be overcome | “Day ran smoothly, with minor technical issues but these are to be expected” | |
| Approachable staff | “Enjoyed the open discussions. I never once felt uncomfortable to answer a question.” | |
| Building confidence in practice | “This course has been extremely beneficial. I am able to put
theory to my practice.” “Overall I found the course extremely helpful and will use the knowledge in my future practice.” “This course given me a new insight into ICU monitoring and caring for the critically ill. As a redeployed nurse to ICU due to COVID I am feeling more confident now.” “This definitely will improve the quality of care for my patient and give me more confidence working in ICU” | |
| Platform for further learning | “It really has reduced my apprehension about possibly having to work on ITU and given me a starting framework for learning about ITU assessment, ventilation and ARDS management. Most of this information was very foreign to me as this is not my area of practice, but look forward to building on what I have learnt” |
Discussion
The COVID-19 pandemic mandated rapid cross skilling of healthcare professionals to be able to manage, treat and care for critically ill patients in the ICU environment. This created extra workload for frontline staff. The CIRLC course demonstrated that during the current and future pandemics, learning technologies can be utilised to create solutions to educate, whilst reducing training burden on frontline clinicians, maintaining social distancing measures and facilitating rapid iteration, in both formal and informal education.
This course was successful in terms of speed of set up and engagement. The results also demonstrated improved confidence in the taught topics and building confidence to practice. This ICS endorsed course has been adopted by Health Education England to be delivered pan-London to address the training needs required to maintain a flexible critical care workforce.
Key lessons and limitations
Utilizing shielding faculty was feasible and enabled recruitment of experts in their field. This optimized use of the available workforce, and gave shielding staff a role in the pandemic.
The online blended learning format allowed learners to access the educational material, consider it at their own pace, and check their understanding through the interactive tutorials. This was highly valued by candidates. The novel format could be replicated for induction and training in the post COVID era. However, it is accepted that this approach does not allow for any practical teaching relating to patient management. Future iterations could consider potential follow-up sessions on site to evaluate the translation of learning to practice.
The rapid cycle of iteration was essential due to the nature of the technology, new working relationships, multiple educators, and emerging clinical guidance. This process is a useful consideration for any course that needs rapid development and implementation and requires human resources in each area to enact changes in a timely manner.
The range of educators required support to ensure quality delivery and up-to-date messaging. Careful consideration of organization and senior faculty support is required to sustain quality.
Due to constraints of the pandemic a pragmatic approach to the course evaluation was used. It was not feasible to evaluate in-practice competence of the course participants. This is a major limitation of this work.
We estimate that the course cost £60–100/candidate. The cost of running the course needs to be considered for ongoing sustainability and we would recommend costs being factored into professional development funding as part of the pandemic response.
Supplemental Material
Supplemental material, sj-pdf-1-inc-10.1177_1751143720972630 for Covid-19 ICU remote-learning course (CIRLC): Rapid ICU remote training for frontline health professionals during the COVID-19 pandemic in the UK by Matthew Camilleri, Xiaoxi Zhang, Meriel Norris, Alex Monkhouse, Alex Harvey, Allison Wiseman, Pratik Sinha, Alex Hemsley, Sophie Tang, Arun Menon, Smruti Sinmayee, Mandy Jones, Jim Buckley, Ruth Johnson, Thomas Medici and Evelyn Corner in Journal of the Intensive Care Society
Acknowledgments
We would like to acknowledge the contribution of all 99 course tutors, and the administration and IT teams involved in the delivery of the course. We would also like to acknowledge Brunel University London, 33N, CLEAR and Blackboard Learn online for providing staff time and software free of charge to allow the delivery of this course.
Footnotes
Competing interests/declarations: The author(s) declared the following potential conflicts of interest with respect
to the research, authorship, and/or publication of this article: 33N is a
private limited company specialising in healthcare data analytics and training.
It is run by working NHS clinicians and provides the Clinically Led Workforce
and Activity Redesign Programme. 33 N provided resources for CIRLC for free with
no charges or monetary gains.
N provided resources for CIRLC for free with
no charges or monetary gains.
Blackboard International B.V: Blackboard provides educational services to support teaching & learning solutions. Blackboard’s EdTech platform ‘Learn Ultra’ was provided for CIRLC for free with no charges or monetary gains.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jim Buckley https://orcid.org/0000-0001-8110-5135
Evelyn Corner https://orcid.org/0000-0002-5611-8118
Supplemental material: Supplemental material for this article is available online.
References
Articles from Journal of the Intensive Care Society are provided here courtesy of SAGE Publications
Full text links
Read article at publisher's site: https://doi.org/10.1177/1751143720972630
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9125447
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1177/1751143720972630
Article citations
Knowledge, Attitude, and Practice of Physiotherapists in COVID-19 ICUs: A National Survey.
ScientificWorldJournal, 2024:9918558, 17 Jan 2024
Cited by: 0 articles | PMID: 38268747
Challenges, obstacles, and unknowns in implementing principles of modern intensive care medicine in low-resource settings: an insider's perspective.
Intensive Care Med, 50(1):141-143, 14 Dec 2023
Cited by: 4 articles | PMID: 38095698
Critical care and pandemic preparedness and response.
Br J Anaesth, 131(5):847-860, 14 Sep 2023
Cited by: 1 article | PMID: 37689541 | PMCID: PMC10636520
Review Free full text in Europe PMC
Nursing workforce deployment and intensive care unit strain during the COVID-19 pandemic in Victoria, Australia.
Aust Crit Care, 36(1):84-91, 12 Dec 2022
Cited by: 2 articles | PMID: 36572575 | PMCID: PMC9742212
Strengthening the ICUs' human resource-related responses to Covid-19: A rapid review of the experience during the first year of public health emergency.
Int J Health Plann Manage, 38(1):22-39, 27 Sep 2022
Cited by: 3 articles | PMID: 36164939 | PMCID: PMC9538981
Review Free full text in Europe PMC
Go to all (7) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Mixed methods evaluation of the impact of the COVID-19 ICU remote-learning rehabilitation course for frontline health professionals during the COVID-19 pandemic in the UK.
J Intensive Care Soc, 23(4):485-491, 23 Sep 2021
Cited by: 1 article | PMID: 36751346 | PMCID: PMC9679894
Rapid cycle training for non-critical care physicians to meet intensive care unit staff shortage at an academic training center in a developing country during the COVID-19 pandemic.
BMC Med Educ, 23(1):493, 05 Jul 2023
Cited by: 1 article | PMID: 37403115 | PMCID: PMC10320933
Service evaluation of a COVID-19 critical care orientation programme.
Br J Nurs, 31(8):452-458, 01 Apr 2022
Cited by: 0 articles | PMID: 35439073
Impact of COVID-19 on rheumatology practice in the UK-a pan-regional rheumatology survey.
Clin Rheumatol, 40(6):2499-2504, 25 Jan 2021
Cited by: 14 articles | PMID: 33495972 | PMCID: PMC7832421
Review Free full text in Europe PMC
 4,14
4,14