Abstract
Free full text

2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023
Abstract
The American Diabetes Association (ADA) “Standards of Care in Diabetes” includes the ADA’s current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, a multidisciplinary expert committee, are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADA’s clinical practice recommendations and a full list of Professional Practice Committee members, please refer to Introduction and Methodology. Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC.
Classification
Diabetes can be classified into the following general categories:
Type 1 diabetes (due to autoimmune β-cell destruction, usually leading to absolute insulin deficiency, including latent autoimmune diabetes of adulthood)
Type 2 diabetes (due to a non-autoimmune progressive loss of adequate β-cell insulin secretion frequently on the background of insulin resistance and metabolic syndrome)
Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes (such as neonatal diabetes and maturity-onset diabetes of the young), diseases of the exocrine pancreas (such as cystic fibrosis and pancreatitis), and drug- or chemical-induced diabetes (such as with glucocorticoid use, in the treatment of HIV/AIDS, or after organ transplantation)
Gestational diabetes mellitus (diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation)
This section reviews most common forms of diabetes but is not comprehensive. For additional information, see the American Diabetes Association (ADA) position statement “Diagnosis and Classification of Diabetes Mellitus” (1).
Type 1 diabetes and type 2 diabetes are heterogeneous diseases in which clinical presentation and disease progression may vary considerably. Classification is important for determining therapy, but some individuals cannot be clearly classified as having type 1 or type 2 diabetes at the time of diagnosis. The traditional paradigms of type 2 diabetes occurring only in adults and type 1 diabetes only in children are no longer accurate, as both diseases occur in both age groups. Children with type 1 diabetes often present with the hallmark symptoms of polyuria/polydipsia, and approximately half present with diabetic ketoacidosis (DKA) (2–4). The onset of type 1 diabetes may be more variable in adults; they may not present with the classic symptoms seen in children and may experience temporary remission from the need for insulin (5–7). The features most useful in discrimination of type 1 diabetes include younger age at diagnosis (<35 years) with lower BMI (<25 kg/m2), unintentional weight loss, ketoacidosis, and glucose >360 mg/dL (20 mmol/L) at presentation (8). Occasionally, people with type 2 diabetes may present with DKA (9,10), particularly members of ethnic and racial minorities (11). It is important for the health care professional to realize that classification of diabetes type is not always straightforward at presentation and that misdiagnosis is common (e.g., adults with type 1 diabetes misdiagnosed as having type 2 diabetes, individuals with maturity-onset diabetes of the young [MODY] misdiagnosed as having type 1 diabetes). Although difficulties in distinguishing diabetes type may occur in all age groups at onset, the diagnosis becomes more obvious over time in people with β-cell deficiency as the degree of β-cell deficiency becomes clear.
In both type 1 and type 2 diabetes, various genetic and environmental factors can result in the progressive loss of β-cell mass and/or function that manifests clinically as hyperglycemia. Once hyperglycemia occurs, people with all forms of diabetes are at risk for developing the same chronic complications, although rates of progression may differ. The identification of individualized therapies for diabetes in the future will be informed by better characterization of the many paths to β-cell demise or dysfunction (12). Across the globe, many groups are working on combining clinical, pathophysiological, and genetic characteristics to more precisely define the subsets of diabetes that are currently clustered into the type 1 diabetes versus type 2 diabetes nomenclature with the goal of optimizing personalized treatment approaches. Many of these studies show great promise and may soon be incorporated into the diabetes classification system (13).
Characterization of the underlying pathophysiology is more precisely developed in type 1 diabetes than in type 2 diabetes. It is now clear from prospective studies that the persistent presence of two or more islet autoantibodies is a near-certain predictor of clinical diabetes (14). The rate of progression is dependent on the age at first detection of autoantibody, number of autoantibodies, autoantibody specificity, and autoantibody titer. Glucose and A1C levels rise well before the clinical onset of diabetes, making diagnosis feasible well before the onset of DKA. Three distinct stages of type 1 diabetes can be identified (Table 2.1) and serve as a framework for research and regulatory decision-making (12,15). There is debate as to whether slowly progressive autoimmune diabetes with an adult onset should be termed latent autoimmune diabetes in adults (LADA) or type 1 diabetes. The clinical priority with detection of LADA is awareness that slow autoimmune β-cell destruction can occur in adults leading to a long duration of marginal insulin secretory capacity. For the purpose of this classification, all forms of diabetes mediated by autoimmune β-cell destruction are included under the rubric of type 1 diabetes. Use of the term LADA is common and acceptable in clinical practice and has the practical impact of heightening awareness of a population of adults likely to have progressive autoimmune β-cell destruction (16), thus accelerating insulin initiation prior to deterioration of glucose management or development of DKA (6,17).
Table 2.1
| Stage 1 | Stage 2 | Stage 3 | |
|---|---|---|---|
| Characteristics | • Autoimmunity | • Autoimmunity | • Autoimmunity |
| • Normoglycemia | • Dysglycemia | • Overt hyperglycemia | |
| • Presymptomatic | • Presymptomatic | • Symptomatic | |
| Diagnostic criteria | • Multiple islet autoantibodies • No IGT or IFG | • Islet autoantibodies (usually multiple) • Dysglycemia: IFG and/or IGT • FPG 100–125 mg/dL (5.6–6.9 mmol/L) • 2-h PG 140–199 mg/dL (7.8–11.0 mmol/L) • A1C 5.7–6.4% (39–47 mmol/mol) or ≥10% increase in A1C | • Autoantibodies may become absent • Diabetes by standard criteria |
FPG, fasting plasma glucose; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; 2-h PG, 2-h plasma glucose.
The paths to β-cell demise and dysfunction are less well defined in type 2 diabetes, but deficient β-cell insulin secretion, frequently in the setting of insulin resistance, appears to be the common denominator. Type 2 diabetes is associated with insulin secretory defects related to genetics, inflammation, and metabolic stress. Future classification schemes for diabetes will likely focus on the pathophysiology of the underlying β-cell dysfunction (12,13,18–20).
Diagnostic Tests for Diabetes
Diabetes may be diagnosed based on plasma glucose criteria, either the fasting plasma glucose (FPG) value or the 2-h plasma glucose (2-h PG) value during a 75-g oral glucose tolerance test (OGTT) or A1C criteria (21) (Table 2.2).
Table 2.2
Criteria for the diagnosis of diabetes
| FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h.* |
| OR |
| 2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed as described by WHO, using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water.* |
| OR |
| A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay.* |
| OR |
| In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (11.1 mmol/L). |
DCCT, Diabetes Control and Complications Trial; FPG, fasting plasma glucose; OGTT, oral glucose tolerance test; NGSP, National Glycohemoglobin Standardization Program; WHO, World Health Organization; 2-h PG, 2-h plasma glucose.
Generally, FPG, 2-h PG during 75-g OGTT, and A1C are equally appropriate for diagnostic screening. It should be noted that detection rates of different screening tests vary in both populations and individuals. Moreover, the efficacy of interventions for primary prevention of type 2 diabetes has mainly been demonstrated among individuals who have impaired glucose tolerance (IGT) with or without elevated fasting glucose, not for individuals with isolated impaired fasting glucose (IFG) or for those with prediabetes defined by A1C criteria (22,23).
The same tests may be used to screen for and diagnose diabetes and to detect individuals with prediabetes (Table 2.2 and Table 2.5) (24). Diabetes may be identified anywhere along the spectrum of clinical scenarios—in seemingly low-risk individuals who happen to have glucose testing, in individuals screened based on diabetes risk assessment, and in symptomatic patients. For additional details on the evidence used to establish the criteria for the diagnosis of diabetes, prediabetes, and abnormal glucose tolerance (IFG, IGT), see the ADA position statement “Diagnosis and Classification of Diabetes Mellitus” (1) and other reports (21,25,26).
Table 2.5
Criteria defining prediabetes*
| FPG 100 mg/dL (5.6 mmol/L) to 125 mg/dL (6.9 mmol/L) (IFG) |
| OR |
| 2-h PG during 75-g OGTT 140 mg/dL (7.8 mmol/L) to 199 mg/dL (11.0 mmol/L) (IGT) |
| OR |
| A1C 5.7–6.4% (39–47 mmol/mol) |
FPG, fasting plasma glucose; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; OGTT, oral glucose tolerance test; 2-h PG, 2-h plasma glucose.
Fasting and 2-Hour Plasma Glucose
The FPG and 2-h PG may be used to diagnose diabetes (Table 2.2). The concordance between the FPG and 2-h PG tests is imperfect, as is the concordance between A1C and either glucose-based test. Compared with FPG and A1C cut points, the 2-h PG value diagnoses more people with prediabetes and diabetes (27). In people in whom there is discordance between A1C values and glucose values, FPG and 2-h PG are more accurate (28).
A1C
Recommendations
2.1a To avoid misdiagnosis or missed diagnosis, the A1C test should be performed using a method that is certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized to the Diabetes Control and Complications Trial (DCCT) assay. B
2.1b Point-of-care A1C testing for diabetes screening and diagnosis should be restricted to U.S. Food and Drug Administration–approved devices at laboratories proficient in performing testing of moderate complexity or higher by trained personnel. B
2.2 Marked discordance between measured A1C and plasma glucose levels should raise the possibility of A1C assay interference and consideration of using an assay without interference or plasma blood glucose criteria to diagnose diabetes. B
2.3 In conditions associated with an altered relationship between A1C and glycemia, such as hemoglobinopathies including sickle cell disease, pregnancy (second and third trimesters and the postpartum period), glucose-6-phosphate dehydrogenase deficiency, HIV, hemodialysis, recent blood loss or transfusion, or erythropoietin therapy, only plasma blood glucose criteria should be used to diagnose diabetes. B
2.4 Adequate carbohydrate intake (at least 150 g/day) should be assured for 3 days prior to oral glucose tolerance testing as a screen for diabetes. A
The A1C test should be performed using a method that is certified by the NGSP (ngsp.org) and standardized or traceable to the Diabetes Control and Complications Trial (DCCT) reference assay. Point-of-care A1C assays may be NGSP certified and cleared by the U.S. Food and Drug Administration (FDA) for use in monitoring glycemic control in people with diabetes in both Clinical Laboratory Improvement Amendments (CLIA)-regulated and CLIA-waived settings. FDA-approved point-of-care A1C testing can be used in laboratories or sites that are CLIA certified, are inspected, and meet the CLIA quality standards. These standards include specified personnel requirements (including documented annual competency assessments) and participation three times per year in an approved proficiency testing program (29–32). As discussed in Section 6, “Glycemic Targets,” point-of-care A1C assays may be more generally applied for assessment of glycemic stability in the clinic.
A1C has several advantages compared with FPG and OGTT, including greater convenience (fasting not required), greater preanalytical stability, and fewer day-to-day perturbations during stress, changes in nutrition, or illness. However, these advantages may be offset by the lower sensitivity of A1C at the designated cut point, greater cost, limited availability of A1C testing in certain regions of the developing world, and the imperfect correlation between A1C and average glucose in certain individuals. The A1C test, with a diagnostic threshold of ≥6.5% (48 mmol/mol), diagnoses only 30% of the diabetes cases identified collectively using A1C, FPG, or 2-h PG, according to National Health and Nutrition Examination Survey (NHANES) data (33). Despite these limitations with A1C, in 2009, the International Expert Committee added A1C to the diagnostic criteria with the goal of increased screening (21).
When using A1C to diagnose diabetes, it is important to recognize that A1C is an indirect measure of average blood glucose levels and to take other factors into consideration that may impact hemoglobin glycation independently of glycemia, such as hemodialysis, pregnancy, HIV treatment (34,35), age, race/ethnicity, genetic background, and anemia/hemoglobinopathies. (See other conditions altering the relationship of a1c and glycemia below for more information.)
Age
The epidemiologic studies that formed the basis for recommending A1C to diagnose diabetes included only adult populations (33). However, recent ADA clinical guidance concluded that A1C, FPG, or 2-h PG could be used to test for prediabetes or type 2 diabetes in children and adolescents (see screening and testing for prediabetes and type 2 diabetes in children and adolescents below for additional information) (36).
Race/Ethnicity/Hemoglobinopathies
Hemoglobin variants can interfere with the measurement of A1C, although most assays in use in the U.S. are unaffected by the most common variants. Marked discrepancies between measured A1C and plasma glucose levels should prompt consideration that the A1C assay may not be reliable for that individual. For individuals with a hemoglobin variant but normal red blood cell turnover, such as those with the sickle cell trait, an A1C assay without interference from hemoglobin variants should be used. An updated list of A1C assays with interferences is available at ngsp.org/interf.asp.
African American individuals heterozygous for the common hemoglobin variant HbS may have, for any given level of mean glycemia, lower A1C by about 0.3% compared with those without the trait (37). Another genetic variant, X-linked glucose-6-phosphate dehydrogenase G202A, carried by 11% of African American individuals, was associated with a decrease in A1C of about 0.8% in homozygous men and 0.7% in homozygous women compared with those without the variant (38). For example, in Tanzania, where there is a high likelihood of hemoglobinopathies in people with HIV, A1C may be lower than expected based on glucose, limiting its usefulness for screening (39).
Even in the absence of hemoglobin variants, A1C levels may vary with race/ethnicity independently of glycemia (40–42). For example, African American individuals may have higher A1C levels than non-Hispanic White individuals with similar fasting and post–glucose load glucose levels (43). Though conflicting data exist, African American individuals may also have higher levels of fructosamine and glycated albumin and lower levels of 1,5-anhydroglucitol, suggesting that their glycemic burden (particularly postprandially) may be higher (44,45). Similarly, A1C levels may be higher for a given mean glucose concentration when measured with continuous glucose monitoring (46). A recent report in Afro-Caribbean people demonstrated a lower A1C than predicted by glucose levels (47). Despite these and other reported differences, the association of A1C with risk for complications appears to be similar in African American and non-Hispanic White populations (42,48). In the Taiwanese population, age and sex have been reported to be associated with increased A1C in men (49); the clinical implications of this finding are unclear at this time.
Other Conditions Altering the Relationship of A1C and Glycemia
In conditions associated with increased red blood cell turnover, such as sickle cell disease, pregnancy (second and third trimesters), glucose-6-phosphate dehydrogenase deficiency (50,51), hemodialysis, recent blood loss or transfusion, or erythropoietin therapy, only plasma blood glucose criteria should be used to diagnose diabetes (52). A1C is less reliable than blood glucose measurement in other conditions such as the postpartum state (53–55), HIV treated with certain protease inhibitors (PIs) and nucleoside reverse transcriptase inhibitors (NRTIs) (34), and iron-deficient anemia (56).
Confirming the Diagnosis
Unless there is a clear clinical diagnosis (e.g., patient in a hyperglycemic crisis or with classic symptoms of hyperglycemia and a random plasma glucose ≥200 mg/dL [11.1 mmol/L]), diagnosis requires two abnormal screening test results, either from the same sample (57) or in two separate test samples. If using two separate test samples, it is recommended that the second test, which may either be a repeat of the initial test or a different test, be performed without delay. For example, if the A1C is 7.0% (53 mmol/mol) and a repeat result is 6.8% (51 mmol/mol), the diagnosis of diabetes is confirmed. If two different tests (such as A1C and FPG) are both above the diagnostic threshold when analyzed from the same sample or in two different test samples, this also confirms the diagnosis. On the other hand, if a patient has discordant results from two different tests, then the test result that is above the diagnostic cut point should be repeated, with careful consideration of the possibility of A1C assay interference. The diagnosis is made on the basis of the confirmatory screening test. For example, if a patient meets the diabetes criterion of the A1C (two results ≥6.5% [48 mmol/mol]) but not FPG (<126 mg/dL [7.0 mmol/L]), that person should nevertheless be considered to have diabetes.
Each of the screening tests has preanalytic and analytic variability, so it is possible that a test yielding an abnormal result (i.e., above the diagnostic threshold), when repeated, will produce a value below the diagnostic cut point. This scenario is likely for FPG and 2-h PG if the glucose samples remain at room temperature and are not centrifuged promptly. Because of the potential for preanalytic variability, it is critical that samples for plasma glucose be spun and separated immediately after they are drawn. If patients have test results near the margins of the diagnostic threshold, the health care professional should discuss signs and symptoms with the patient and repeat the test in 3–6 months.
People should consume a mixed diet with at least 150 g of carbohydrates on the 3 days prior to oral glucose tolerance testing (58–60). Fasting and carbohydrate restriction can falsely elevate glucose level with an oral glucose challenge.
Diagnosis
In a patient with classic symptoms, measurement of plasma glucose is sufficient to diagnose diabetes (symptoms of hyperglycemia or hyperglycemic crisis plus a random plasma glucose ≥200 mg/dL [11.1 mmol/L]). In these cases, knowing the plasma glucose level is critical because, in addition to confirming that symptoms are due to diabetes, it will inform management decisions. Some health care professionals may also want to know the A1C to determine the chronicity of the hyperglycemia. The criteria to diagnose diabetes are listed in Table 2.2.
Type 1 Diabetes
Recommendations
2.5 Screening for presymptomatic type 1 diabetes using screening tests that detect autoantibodies to insulin, glutamic acid decarboxylase (GAD), islet antigen 2, or zinc transporter 8 is currently recommended in the setting of a research study or can be considered an option for first-degree family members of a proband with type 1 diabetes. B
2.6 Development of and persistence of multiple islet autoantibodies is a risk factor for clinical diabetes and may serve as an indication for intervention in the setting of a clinical trial or screening for stage 2 type 1 diabetes. B
Immune-Mediated Diabetes
This form, previously called “insulin-dependent diabetes” or “juvenile-onset diabetes,” accounts for 5–10% of diabetes and is due to cell-mediated autoimmune destruction of the pancreatic β-cells. Autoimmune markers include islet cell autoantibodies and autoantibodies to GAD (glutamic acid decarboxylase, GAD65), insulin, the tyrosine phosphatases islet antigen 2 (IA-2) and IA-2β, and zinc transporter 8. Numerous clinical studies are being conducted to test various methods of preventing type 1 diabetes in those with evidence of islet autoimmunity (trialnet.org/our-research/prevention-studies) (14,17,61–64). Stage 1 of type 1 diabetes is defined by the presence of two or more of these autoimmune markers. The disease has strong HLA associations, with linkage to the DQB1 and DRB1 haplotypes, and genetic screening has been used in some research studies to identify high-risk populations. Specific alleles in these genes can be either predisposing or protective (Table 2.1).
The rate of β-cell destruction is quite variable, being rapid in some individuals (particularly but not exclusively in infants and children) and slow in others (mainly but not exclusively adults) (65,66). Children and adolescents often present with DKA as the first manifestation of the disease, and the rates in the U.S. have increased dramatically over the past 20 years (2–4). Others have modest fasting hyperglycemia that can rapidly change to severe hyperglycemia and/or DKA with infection or other stress. Adults may retain sufficient β-cell function to prevent DKA for many years; such individuals may have remission or decreased insulin needs for months or years and eventually become dependent on insulin for survival and are at risk for DKA (5–7,67,68). At this later stage of the disease, there is little or no insulin secretion, as manifested by low or undetectable levels of plasma C-peptide. Immune-mediated diabetes is the most common form of diabetes in childhood and adolescence, but it can occur at any age, even in the 8th and 9th decades of life.
Autoimmune destruction of β-cells has multiple genetic factors and is also related to environmental factors that are still poorly defined. Although individuals do not typically have obesity when they present with type 1 diabetes, obesity is increasingly common in the general population; as such, obesity should not preclude testing for type 1 diabetes. People with type 1 diabetes are also prone to other autoimmune disorders such as Hashimoto thyroiditis, Graves disease, celiac disease, Addison disease, vitiligo, autoimmune hepatitis, myasthenia gravis, and pernicious anemia (see Section 4, “Comprehensive Medical Evaluation and Assessment of Comorbidities”). Type 1 diabetes can be associated with monogenic polyglandular autoimmune syndromes, including immune dysregulation, polyendocrinopathy, enteropathy, and X-linked (IPEX) syndrome, which is an early-onset systemic autoimmune, genetic disorder caused by mutation of the forkhead box protein 3 (FOXP3) gene, and another caused by the autoimmune regulator (AIRE) gene mutation (69,70). As indicated by the names, these disorders are associated with other autoimmune and rheumatological diseases.
Introduction of immunotherapy, specifically checkpoint inhibitors, for cancer treatment has led to unexpected adverse events, including immune system activation precipitating autoimmune disease. Fulminant onset of type 1 diabetes can develop, with DKA and low or undetectable levels of C-peptide as a marker of endogenous β-cell function (71,72). Fewer than half of these patients have autoantibodies that are seen in type 1 diabetes, supporting alternate pathobiology. This immune-related adverse event occurs in just under 1% of checkpoint inhibitor-treated patients but most commonly occurs with agents that block the programmed cell death protein 1/programmed cell death ligand 1 pathway alone or in combination with other checkpoint inhibitors (73). To date, the majority of immune checkpoint inhibitor–related cases of type 1 diabetes occur in people with high-risk HLA-DR4 (present in 76% of patients), whereas other high-risk HLA alleles are not more common than those in the general population (73). To date, risk cannot be predicted by family history or autoantibodies, so all health care professionals administering these medications should be mindful of this adverse effect and educate patients appropriately.
Idiopathic Type 1 Diabetes
Some forms of type 1 diabetes have no known etiologies. These individuals have permanent insulinopenia and are prone to DKA but have no evidence of β-cell autoimmunity. However, only a minority of people with type 1 diabetes fall into this category. Individuals with autoantibody-negative type 1 diabetes of African or Asian ancestry may suffer from episodic DKA and exhibit varying degrees of insulin deficiency between episodes (possibly ketosis-prone diabetes) (74). This form of diabetes is strongly inherited and is not HLA associated. An absolute requirement for insulin replacement therapy in affected individuals may be intermittent. Future research is needed to determine the cause of β-cell destruction in this rare clinical scenario.
Screening for Type 1 Diabetes Risk
The incidence and prevalence of type 1 diabetes are increasing (75). People with type 1 diabetes often present with acute symptoms of diabetes and markedly elevated blood glucose levels, and 40–60% are diagnosed with life-threatening DKA (2–4). Multiple studies indicate that measuring islet autoantibodies in relatives of those with type 1 diabetes (15) or in children from the general population (76,77) can effectively identify those who will develop type 1 diabetes. A study reported the risk of progression to type 1 diabetes from the time of seroconversion to autoantibody positivity in three pediatric cohorts from Finland, Germany, and the U.S. Of the 585 children who developed more than two autoantibodies, nearly 70% developed type 1 diabetes within 10 years and 84% within 15 years (14). These findings are highly significant because while the German group was recruited from offspring of parents with type 1 diabetes, the Finnish and American groups were recruited from the general population. Remarkably, the findings in all three groups were the same, suggesting that the same sequence of events led to clinical disease in both “sporadic” and familial cases of type 1 diabetes. Indeed, the risk of type 1 diabetes increases as the number of relevant autoantibodies detected increases (63,78,79). In The Environmental Determinants of Diabetes in the Young (TEDDY) study, type 1 diabetes developed in 21% of 363 subjects with at least one autoantibody at 3 years of age (80). Such testing, coupled with education about diabetes symptoms and close follow-up, has been shown to enable earlier diagnosis and prevent DKA (81,82).
While widespread clinical screening of asymptomatic low-risk individuals is not currently recommended due to lack of approved therapeutic interventions, several innovative research screening programs are available in Europe (e.g., Fr1da, gppad.org) and the U.S. (trialnet.org, askhealth.org). Participation should be encouraged to accelerate development of evidence-based clinical guidelines for the general population and relatives of those with type 1 diabetes. Individuals who test positive should be counseled about the risk of developing diabetes, diabetes symptoms, and DKA prevention. Numerous clinical studies are being conducted to test various methods of preventing and treating stage 2 type 1 diabetes in those with evidence of autoimmunity with promising results (see clinicaltrials.gov and trialnet.org). Delay of overt diabetes development in stage 2 type 1 diabetes with the anti-CD3 antibody teplizumab in relatives at risk for type 1 diabetes was reported in 2019, with an extension of the randomized controlled trial in 2021 (83,84). Based on these data, this agent has been submitted to the FDA for the indication of delay or prevention of clinical type 1 diabetes in at-risk individuals. Neither this agent nor others in this category are currently available for clinical use.
Prediabetes and Type 2 Diabetes
Recommendations
2.7 Screening for prediabetes and type 2 diabetes with an informal assessment of risk factors or validated risk calculator should be done in asymptomatic adults. B
2.8 Testing for prediabetes and/or type 2 diabetes in asymptomatic people should be considered in adults of any age with overweight or obesity (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian American individuals) who have one or more risk factors (Table 2.3). B
Table 2.3
Criteria for screening for diabetes or prediabetes in asymptomatic adults
1. Testing should be considered in adults with overweight or obesity (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian American individuals) who have one or more of the following risk factors:  • First-degree relative with diabetes
• First-degree relative with diabetes • High-risk race/ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander)
• High-risk race/ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander) • History of CVD
• History of CVD • Hypertension (≥130/80 mmHg or on therapy for hypertension)
• Hypertension (≥130/80 mmHg or on therapy for hypertension) • HDL cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L)
• HDL cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L) • Individuals with polycystic ovary syndrome
• Individuals with polycystic ovary syndrome • Physical inactivity
• Physical inactivity • Other clinical conditions associated with insulin resistance (e.g., severe obesity, acanthosis nigricans)
• Other clinical conditions associated with insulin resistance (e.g., severe obesity, acanthosis nigricans)2. People with prediabetes (A1C ≥5.7% [39 mmol/mol], IGT, or IFG) should be tested yearly. 3. People who were diagnosed with GDM should have lifelong testing at least every 3 years. 4. For all other people, testing should begin at age 35 years. 5. If results are normal, testing should be repeated at a minimum of 3-year intervals, with consideration of more frequent testing depending on initial results and risk status. 6. People with HIV CVD, cardiovascular disease; GDM, gestational diabetes mellitus; IFG, impaired fasting glucose; IGT, impaired glucose tolerance.
2.9 For all people, screening should begin at age 35 years. B
2.10 If tests are normal, repeat screening recommended at a minimum of 3-year intervals is reasonable, sooner with symptoms or change in risk (i.e., weight gain). C
2.11 To screen for prediabetes and type 2 diabetes, fasting plasma glucose, 2-h plasma glucose during 75-g oral glucose tolerance test, and A1C are each appropriate (Table 2.2 and Table 2.5). B
2.12 When using oral glucose tolerance testing as a screen for diabetes, adequate carbohydrate intake (at least 150 g/day) should be assured for 3 days prior to testing. A
2.13 In people with prediabetes and type 2 diabetes, identify and treat cardiovascular disease risk factors. A
2.14 Risk-based screening for prediabetes and/or type 2 diabetes should be considered after the onset of puberty or after 10 years of age, whichever occurs earlier, in children and adolescents with overweight (BMI ≥85th percentile) or obesity (BMI ≥95th percentile) and who have one or more risk factors for diabetes. (See Table 2.4 for evidence grading of risk factors.) B
Table 2.4
Risk-based screening for type 2 diabetes or prediabetes in asymptomatic children and adolescents in a clinical setting
Screening should be considered in youth* who have overweight (≥85th percentile) or obesity (≥95th percentile) A and who have one or more additional risk factors based on the strength of their association with diabetes:  • Maternal history of diabetes or GDM during the child’s gestation A
• Maternal history of diabetes or GDM during the child’s gestation A • Family history of type 2 diabetes in first- or second-degree relative A
• Family history of type 2 diabetes in first- or second-degree relative A • Race/ethnicity (Native American, African American, Latino, Asian American, Pacific Islander) A
• Race/ethnicity (Native American, African American, Latino, Asian American, Pacific Islander) A • Signs of insulin resistance or conditions associated with insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic ovary syndrome, or small-for-gestational-age birth weight) B
• Signs of insulin resistance or conditions associated with insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic ovary syndrome, or small-for-gestational-age birth weight) BGDM, gestational diabetes mellitus.
*After the onset of puberty or after 10 years of age, whichever occurs earlier. If tests are normal, repeat testing at a minimum of 3-year intervals (or more frequently if BMI is increasing or risk factor profile deteriorating) is recommended. Reports of type 2 diabetes before age 10 years exist, and this can be considered with numerous risk factors.2.15 People with HIV should be screened for diabetes and prediabetes with a fasting glucose test before starting antiretroviral therapy, at the time of switching antiretroviral therapy, and 3–6 months after starting or switching antiretroviral therapy. If initial screening results are normal, fasting glucose should be checked annually. E
Prediabetes
“Prediabetes” is the term used for individuals whose glucose levels do not meet the criteria for diabetes yet have abnormal carbohydrate metabolism (48,85). People with prediabetes are defined by the presence of IFG and/or IGT and/or A1C 5.7–6.4% (39–47 mmol/mol) (Table 2.5). Prediabetes should not be viewed as a clinical entity in its own right but rather as a risk factor for progression to diabetes and cardiovascular disease (CVD). Criteria for screening for diabetes or prediabetes in asymptomatic adults are outlined in Table 2.3. Prediabetes is associated with obesity (especially abdominal or visceral obesity), dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension. The presence of prediabetes should prompt comprehensive screening for cardiovascular risk factors.
Diagnosis
IFG is defined as FPG levels from 100 to 125 mg/dL (from 5.6 to 6.9 mmol/L) (82,83) and IGT as 2-h PG levels during 75-g OGTT from 140 to 199 mg/dL (from 7.8 to 11.0 mmol/L) (25). It should be noted that the World Health Organization and numerous other diabetes organizations define the IFG lower limit at 110 mg/dL (6.1 mmol/L).
As with the glucose measures, several prospective studies that used A1C to predict the progression to diabetes as defined by A1C criteria demonstrated a strong, continuous association between A1C and subsequent diabetes. In a systematic review of 44,203 individuals from 16 cohort studies with a follow-up interval averaging 5.6 years (range 2.8–12 years), those with A1C between 5.5% and 6.0% (between 37 and 42 mmol/mol) had a substantially increased risk of diabetes (5-year incidence from 9% to 25%). Those with an A1C range of 6.0–6.5% (42–48 mmol/mol) had a 5-year risk of developing diabetes between 25% and 50% and a relative risk 20 times higher compared with A1C of 5.0% (31 mmol/mol) (86). In a community-based study of African American and non-Hispanic White adults without diabetes, baseline A1C was a stronger predictor of subsequent diabetes and cardiovascular events than fasting glucose (87). Other analyses suggest that A1C of 5.7% (39 mmol/mol) or higher is associated with a diabetes risk similar to that of the high-risk participants in the Diabetes Prevention Program (DPP) (88), and A1C at baseline was a strong predictor of the development of glucose-defined diabetes during the DPP and its follow-up (89).
Hence, it is reasonable to consider an A1C range of 5.7–6.4% (39–47 mmol/mol) as identifying individuals with prediabetes. Similar to those with IFG and/or IGT, individuals with A1C of 5.7–6.4% (39–47 mmol/mol) should be informed of their increased risk for diabetes and CVD and counseled about effective strategies to lower their risks (see Section 3, “Prevention or Delay of Type 2 Diabetes and Associated Comorbidities”). Similar to glucose measurements, the continuum of risk is curvilinear, so as A1C rises, the diabetes risk rises disproportionately (86). Aggressive interventions and vigilant follow-up should be pursued for those considered at very high risk (e.g., those with A1C >6.0% [42 mmol/mol]).
Table 2.5 summarizes the categories of prediabetes, and Table 2.3 outlines the criteria for screening for prediabetes. The ADA Diabetes Risk Test is an additional option for assessment to determine the appropriateness of screening for diabetes or prediabetes in asymptomatic adults (Fig. 2.1) (diabetes.org/socrisktest). For additional background regarding risk factors and screening for prediabetes, see screening and testing for prediabetes and type 2 diabetes in asymptomatic adults and also screening and testing for prediabetes and type 2 diabetes in children and adolescents below. For details regarding individuals with prediabetes most likely to benefit from a formal behavioral or lifestyle intervention, see Section 3, “Prevention or Delay of Type 2 Diabetes and Associated Comorbidities.”
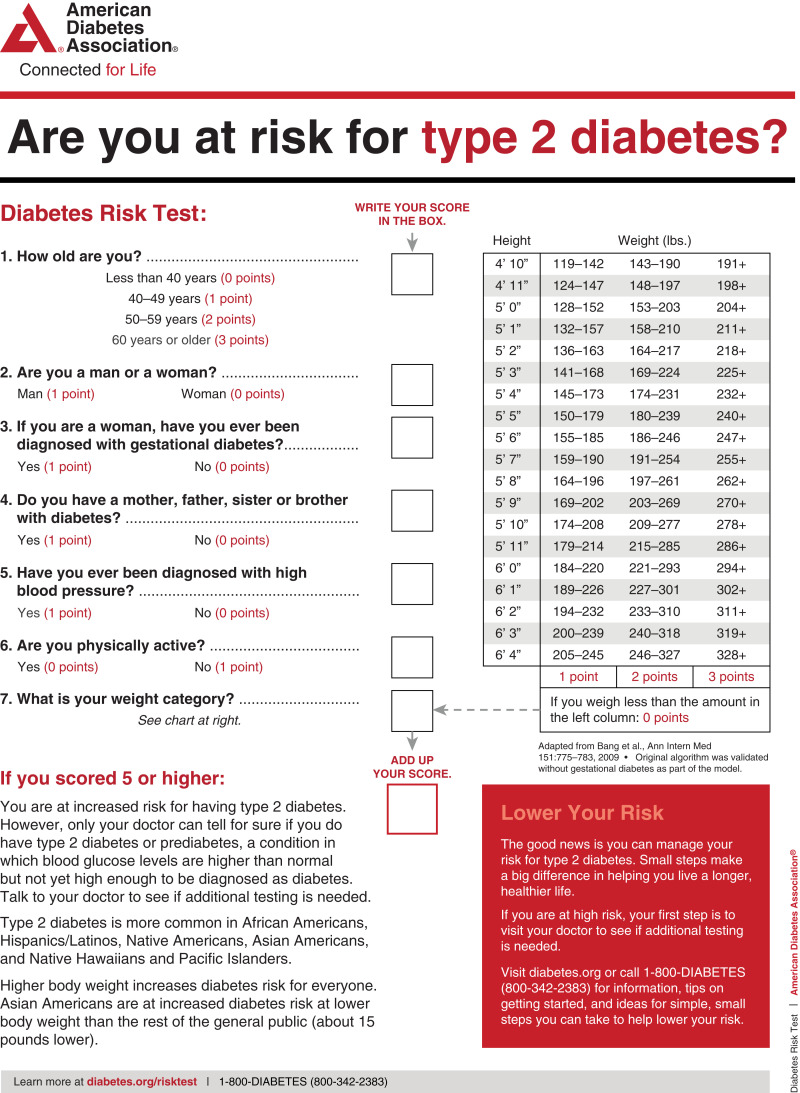
ADA risk test (diabetes.org/socrisktest).
Type 2 Diabetes
Type 2 diabetes, previously referred to as “non-insulin-dependent diabetes” or “adult-onset diabetes,” accounts for 90–95% of all diabetes. This form encompasses individuals who have relative (rather than absolute) insulin deficiency and have peripheral insulin resistance. At least initially, and often throughout their lifetime, these individuals may not need insulin treatment to survive.
There are various causes of type 2 diabetes. Although the specific etiologies are not known, autoimmune destruction of β-cells does not occur, and patients do not have any of the other known causes of diabetes. Most, but not all, people with type 2 diabetes have overweight or obesity. Excess weight itself causes some degree of insulin resistance. Individuals who do not have obesity or overweight by traditional weight criteria may have an increased percentage of body fat distributed predominantly in the abdominal region.
DKA seldom occurs spontaneously in type 2 diabetes; when seen, it usually arises in association with the stress of another illness such as infection or myocardial infarction or with the use of certain drugs (e.g., corticosteroids, atypical antipsychotics, and sodium–glucose cotransporter 2 inhibitors) (90,91). Type 2 diabetes frequently goes undiagnosed for many years because hyperglycemia develops gradually and, at earlier stages, is often not severe enough for the patient to notice the classic diabetes symptoms caused by hyperglycemia, such as dehydration or unintentional weight loss. Nevertheless, even undiagnosed people with diabetes are at increased risk of developing macrovascular and microvascular complications.
People with type 2 diabetes may have insulin levels that appear normal or elevated, yet the failure to normalize blood glucose reflects a relative defect in glucose-stimulated insulin secretion. Thus, insulin secretion is defective in these individuals and insufficient to compensate for insulin resistance. Insulin resistance may improve with weight reduction, physical activity, and/or pharmacologic treatment of hyperglycemia but is seldom restored to normal. Recent interventions with intensive diet and exercise or surgical weight loss have led to diabetes remission (92–98) (see Section 8, “Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes”).
The risk of developing type 2 diabetes increases with age, obesity, and lack of physical activity (99,100). It occurs more frequently in individuals with prior gestational diabetes mellitus (GDM) or polycystic ovary syndrome. It is also more common in people with hypertension or dyslipidemia and in certain racial/ethnic subgroups (African American, Native American, Hispanic/Latino, and Asian American). It is often associated with a strong genetic predisposition or family history in first-degree relatives (more so than type 1 diabetes). However, the genetics of type 2 diabetes are poorly understood and under intense investigation in this era of precision medicine (18). In adults without traditional risk factors for type 2 diabetes and/or of younger age, consider islet autoantibody testing (e.g., GAD65 autoantibodies) to exclude the diagnosis of type 1 diabetes (8).
Screening and Testing for Prediabetes and Type 2 Diabetes in Asymptomatic Adults
Screening for prediabetes and type 2 diabetes risk through an informal assessment of risk factors (Table 2.3) or with an assessment tool, such as the ADA risk test (Fig. 2.1) (online at diabetes.org/socrisktest), is recommended to guide health care professionals on whether performing a diagnostic test (Table 2.2) is appropriate. Prediabetes and type 2 diabetes meet criteria for conditions in which early detection via screening is appropriate. Both conditions are common and impose significant clinical and public health burdens. There is often a long presymptomatic phase before the diagnosis of type 2 diabetes. Simple tests to detect preclinical disease are readily available (101). The duration of glycemic burden is a strong predictor of adverse outcomes. There are effective interventions that prevent progression from prediabetes to diabetes. It is important to individualize risk/benefit of formal intervention for people with prediabetes and consider patient-centered goals. Risk models have explored the benefit, in general finding higher benefit of intervention in those at highest risk (102) (see Section 3, “Prevention or Delay of Type 2 Diabetes and Associated Comorbidities”) and reduce the risk of diabetes complications (103) (see Section 10, “Cardiovascular Disease and Risk Management,” Section 11, “Chronic Kidney Disease and Risk Management,” and Section 12, “Retinopathy, Neuropathy, and Foot Care”). In the most recent National Institutes of Health (NIH) Diabetes Prevention Program Outcomes Study (DPPOS) report, prevention of progression from prediabetes to diabetes (104) resulted in lower rates of developing retinopathy and nephropathy (105). Similar impact on diabetes complications was reported with screening, diagnosis, and comprehensive risk factor management in the U.K. Clinical Practice Research Datalink database (103). In that report, progression from prediabetes to diabetes augmented risk of complications.
Approximately one-quarter of people with diabetes in the U.S. and nearly half of Asian and Hispanic American people with diabetes are undiagnosed (106,107). Although screening of asymptomatic individuals to identify those with prediabetes or diabetes might seem reasonable, rigorous clinical trials to prove the effectiveness of such screening have not been conducted and are unlikely to occur. Clinical conditions, such as hypertension, hypertensive pregnancy, and obesity, enhance risk (108). Based on a population estimate, diabetes in people of childbearing age is underdiagnosed (109). Employing a probabilistic model, Peterson et al. (110) demonstrated cost and health benefits of preconception screening.
A large European randomized controlled trial compared the impact of screening for diabetes and intensive multifactorial intervention with that of screening and routine care (111). General practice patients between the ages of 40 and 69 years were screened for diabetes and randomly assigned by practice to intensive treatment of multiple risk factors or routine diabetes care. After 5.3 years of follow-up, CVD risk factors were modestly but significantly improved with intensive treatment compared with routine care, but the incidence of first CVD events or mortality was not significantly different between the groups (26). The excellent care provided to patients in the routine care group and the lack of an unscreened control arm limited the authors’ ability to determine whether screening and early treatment improved outcomes compared with no screening and later treatment after clinical diagnoses. Computer simulation modeling studies suggest that major benefits are likely to accrue from the early diagnosis and treatment of hyperglycemia and cardiovascular risk factors in type 2 diabetes (112); moreover, screening, beginning at age 30 or 45 years and independent of risk factors, may be cost-effective (<$11,000 per quality-adjusted life year gained—2010 modeling data) (113). Cost-effectiveness of screening has been reinforced in cohort studies (114,115).
Additional considerations regarding testing for type 2 diabetes and prediabetes in asymptomatic individuals include the following.
Age
Age is a major risk factor for diabetes. Testing should begin at no later than age 35 years for all people (116). Screening should be considered in adults of any age with overweight or obesity and one or more risk factors for diabetes.
BMI and Ethnicity
In general, BMI ≥25 kg/m2 is a risk factor for diabetes. However, data suggest that the BMI cut point should be lower for the Asian American population (117,118). The BMI cut points fall consistently between 23 and 24 kg/m2 (sensitivity of 80%) for nearly all Asian American subgroups (with levels slightly lower for Japanese American individuals). This makes a rounded cut point of 23 kg/m2 practical. An argument can be made to push the BMI cut point to lower than 23 kg/m2 in favor of increased sensitivity; however, this would lead to an unacceptably low specificity (13.1%). Data from the World Health Organization also suggest that a BMI of ≥23 kg/m2 should be used to define increased risk in Asian American individuals (119). The finding that one-third to one-half of diabetes in Asian American people is undiagnosed suggests that testing is not occurring at lower BMI thresholds (99,120).
Evidence also suggests that other populations may benefit from lower BMI cut points. For example, in a large multiethnic cohort study, for an equivalent incidence rate of diabetes, a BMI of 30 kg/m2 in non-Hispanic White individuals was equivalent to a BMI of 26 kg/m2 in African American individuals (121).
Medications
Certain medications, such as glucocorticoids, thiazide diuretics, some HIV medications (34), and atypical antipsychotics (92), are known to increase the risk of diabetes and should be considered when deciding whether to screen.
HIV
Individuals with HIV are at higher risk for developing prediabetes and diabetes on antiretroviral (ARV) therapies; a screening protocol is therefore recommended (122). The A1C test may underestimate glycemia in people with HIV; it is not recommended for diagnosis and may present challenges for monitoring (35). In those with prediabetes, weight loss through healthy nutrition and physical activity may reduce the progression toward diabetes. Among people with HIV and diabetes, preventive health care using an approach used in people without HIV is critical to reduce the risks of microvascular and macrovascular complications. Diabetes risk is increased with certain PIs and NRTIs. New-onset diabetes is estimated to occur in more than 5% of individuals infected with HIV on PIs, whereas more than 15% may have prediabetes (123).
PIs are associated with insulin resistance and may also lead to apoptosis of pancreatic β-cells. NRTIs also affect fat distribution (both lipohypertrophy and lipoatrophy), which is associated with insulin resistance. For people with HIV and ARV-associated hyperglycemia, it may be appropriate to consider discontinuing the problematic ARV agents if safe and effective alternatives are available (124). Before making ARV substitutions, carefully consider the possible effect on HIV virological control and the potential adverse effects of new ARV agents. In some cases, antihyperglycemic agents may still be necessary.
Testing Interval
The appropriate interval between screening tests is not known (125). The rationale for the 3-year interval is that with this interval, the number of false-positive tests that require confirmatory testing will be reduced, and individuals with false-negative tests will be retested before substantial time elapses and complications develop (125). In especially high-risk individuals, particularly with weight gain, shorter intervals between screening may be useful.
Community Screening
Ideally, screening should be carried out within a health care setting because of the need for follow-up and treatment. Community screening outside a health care setting is generally not recommended because people with positive tests may not seek, or have access to, appropriate follow-up testing and care. However, in specific situations where an adequate referral system is established beforehand for positive tests, community screening may be considered. Community screening may also be poorly targeted; i.e., it may fail to reach the groups most at risk and inappropriately test those at very low risk or even those who have already been diagnosed (126).
Screening in Dental Practices
Because periodontal disease is associated with diabetes, the utility of screening in a dental setting and referral to primary care as a means to improve the diagnosis of prediabetes and diabetes has been explored (127–129), with one study estimating that 30% of patients ≥30 years of age seen in general dental practices had dysglycemia (129,130). A similar study in 1,150 dental patients >40 years old in India reported 20.69% and 14.60% meeting criteria for prediabetes and diabetes, respectively, using random blood glucose. Further research is needed to demonstrate the feasibility, effectiveness, and cost-effectiveness of screening in this setting.
Screening and Testing for Prediabetes and Type 2 Diabetes in Children and Adolescents
In the last decade, the incidence and prevalence of type 2 diabetes in children and adolescents has increased dramatically, especially in racial and ethnic minority populations (75). See Table 2.4 for recommendations on risk-based screening for type 2 diabetes or prediabetes in asymptomatic children and adolescents in a clinical setting (36). See Table 2.2 and Table 2.5 for the criteria for the diagnosis of diabetes and prediabetes, respectively, that apply to children, adolescents, and adults. See Section 14, “Children and Adolescents,” for additional information on type 2 diabetes in children and adolescents.
Some studies question the validity of A1C in the pediatric population, especially among certain ethnicities, and suggest OGTT or FPG as more suitable diagnostic tests (131). However, many of these studies do not recognize that diabetes diagnostic criteria are based on long-term health outcomes, and validations are not currently available in the pediatric population (132). The ADA acknowledges the limited data supporting A1C for diagnosing type 2 diabetes in children and adolescents. Although A1C is not recommended for diagnosis of diabetes in children with cystic fibrosis or symptoms suggestive of acute onset of type 1 diabetes, and only A1C assays without interference are appropriate for children with hemoglobinopathies, the ADA continues to recommend A1C and the criteria in Table 2.2 for diagnosis of type 2 diabetes in this cohort to decrease barriers to screening (133,134).
Cystic Fibrosis–Related Diabetes
Recommendations
2.16 Annual screening for cystic fibrosis–related diabetes with an oral glucose tolerance test should begin by age 10 years in all people with cystic fibrosis not previously diagnosed with cystic fibrosis–related diabetes. B
2.17 A1C is not recommended as a screening test for cystic fibrosis–related diabetes. B
2.18 People with cystic fibrosis–related diabetes should be treated with insulin to attain individualized glycemic goals. A
2.19 Beginning 5 years after the diagnosis of cystic fibrosis–related diabetes, annual monitoring for complications of diabetes is recommended. E
Cystic fibrosis–related diabetes (CFRD) is the most common comorbidity in people with cystic fibrosis, occurring in about 20% of adolescents and 40–50% of adults (135). Diabetes in this population, compared with individuals with type 1 or type 2 diabetes, is associated with worse nutritional status, more severe inflammatory lung disease, and greater mortality. Insulin insufficiency is the primary defect in CFRD. Genetically determined β-cell function and insulin resistance associated with infection and inflammation may also contribute to the development of CFRD. Milder abnormalities of glucose tolerance are even more common and occur at earlier ages than CFRD. Whether individuals with IGT should be treated with insulin replacement has not currently been determined. Although screening for diabetes before the age of 10 years can identify risk for progression to CFRD in those with abnormal glucose tolerance, no benefit has been established with respect to weight, height, BMI, or lung function. OGTT is the recommended screening test; however, recent publications suggest that an A1C cut point threshold of 5.5% (5.8% in a second study) would detect more than 90% of cases and reduce patient screening burden (136,137). Ongoing studies are underway to validate this approach, and A1C is not recommended for screening (138). Regardless of age, weight loss or failure of expected weight gain is a risk for CFRD and should prompt screening (136,137). The Cystic Fibrosis Foundation Patient Registry (139) evaluated 3,553 people with cystic fibrosis and diagnosed 445 (13%) with CFRD. Early diagnosis and treatment of CFRD was associated with preservation of lung function. The European Cystic Fibrosis Society Patient Registry reported an increase in CFRD with age (increased 10% per decade), genotype, decreased lung function, and female sex (140,141). Continuous glucose monitoring or HOMA of β-cell function (142) may be more sensitive than OGTT to detect risk for progression to CFRD; however, evidence linking these results to long-term outcomes is lacking, and these tests are not recommended for screening outside of the research setting (143).
CFRD mortality has significantly decreased over time, and the gap in mortality between people with cystic fibrosis with and without diabetes has considerably narrowed (144). There are limited clinical trial data on therapy for CFRD. The largest study compared three regimens: premeal insulin aspart, repaglinide, or oral placebo in people with cystic fibrosis and diabetes or abnormal glucose tolerance. Participants all had weight loss in the year preceding treatment; however, in the insulin-treated group, this pattern was reversed, and participants gained 0.39 (± 0.21) BMI units (P = 0.02). The repaglinide-treated group had initial weight gain, but it was not sustained by 6 months. The placebo group continued to lose weight (144). Insulin remains the most widely used therapy for CFRD (145). The primary rationale for the use of insulin in people with CFRD is to induce an anabolic state while promoting macronutrient retention and weight gain.
Additional resources for the clinical management of CFRD can be found in the position statement “Clinical Care Guidelines for Cystic Fibrosis–Related Diabetes: A Position Statement of the American Diabetes Association and a Clinical Practice Guideline of the Cystic Fibrosis Foundation, Endorsed by the Pediatric Endocrine Society” (146) and in the International Society for Pediatric and Adolescent Diabetes 2018 clinical practice consensus guidelines (135).
Posttransplantation Diabetes Mellitus
Recommendations
2.20 After organ transplantation, screening for hyperglycemia should be done. A formal diagnosis of posttransplantation diabetes mellitus is best made once the individual is stable on an immunosuppressive regimen and in the absence of an acute infection. B
2.21 The oral glucose tolerance test is the preferred test to make a diagnosis of posttransplantation diabetes mellitus. B
2.22 Immunosuppressive regimens shown to provide the best outcomes for patient and graft survival should be used, irrespective of posttransplantation diabetes mellitus risk. E
Several terms are used in the literature to describe the presence of diabetes following organ transplantation (147). “New-onset diabetes after transplantation” (NODAT) is one such designation that describes individuals who develop new-onset diabetes following transplant. NODAT excludes people with pretransplant diabetes that was undiagnosed as well as posttransplant hyperglycemia that resolves by the time of discharge (148). Another term, “posttransplantation diabetes mellitus” (PTDM) (148,149), describes the presence of diabetes in the posttransplant setting irrespective of the timing of diabetes onset.
Hyperglycemia is very common during the early posttransplant period, with ~90% of kidney allograft recipients exhibiting hyperglycemia in the first few weeks following transplant (148–151). In most cases, such stress- or steroid-induced hyperglycemia resolves by the time of discharge (151,152). Although the use of immunosuppressive therapies is a major contributor to the development of PTDM, the risks of transplant rejection outweigh the risks of PTDM, and the role of the diabetes care health care professional is to treat hyperglycemia appropriately regardless of the type of immunosuppression (148). Risk factors for PTDM include both general diabetes risks (such as age, family history of diabetes, etc.) as well as transplant-specific factors, such as use of immunosuppressant agents (153–155). Whereas posttransplantation hyperglycemia is an important risk factor for subsequent PTDM, a formal diagnosis of PTDM is optimally made once the patient is stable on maintenance mmunosuppression and in the absence of acute infection (151–153,156). In a recent study of 152 heart transplant recipients, 38% had PTDM at 1 year. Risk factors for PTDM included elevated BMI, discharge from the hospital on insulin, and glucose values in the 24 h prior to hospital discharge (157). In an Iranian cohort, 19% had PTDM after heart and lung transplant (158). The OGTT is considered the gold-standard test for the diagnosis of PTDM (1 year posttransplant) (148,149,159,160). Pretransplant elevation in hs-CRP was associated with PTDM in the setting of renal transplant (161,162). However, screening people with fasting glucose and/or A1C can identify high-risk individuals requiring further assessment and may reduce the number of overall OGTTs required.
Few randomized controlled studies have reported on the short- and long-term use of antihyperglycemic agents in the setting of PTDM (153,163,164). Most studies have reported that transplant patients with hyperglycemia and PTDM after transplantation have higher rates of rejection, infection, and rehospitalization (151,153,165). Insulin therapy is the agent of choice for the management of hyperglycemia, PTDM, and preexisting diabetes and diabetes in the hospital setting. After discharge, people with preexisting diabetes could go back on their pretransplant regimen if they were in good control before transplantation. Those with previously poor glycemic stability or with persistent hyperglycemia should continue insulin with frequent home glucose monitoring to determine when insulin dose reductions may be needed and when it may be appropriate to switch to noninsulin agents.
No studies to date have established which noninsulin agents are safest or most efficacious in PTDM. The choice of agent is usually made based on the side effect profile of the medication and possible interactions with the patient’s immunosuppression regimen (153). Drug dose adjustments may be required because of decreases in the glomerular filtration rate, a relatively common complication in transplant patients. A small short-term pilot study reported that metformin was safe to use in renal transplant recipients (166), but its safety has not been determined in other types of organ transplant. Thiazolidinediones have been used successfully in people with liver and kidney transplants, but side effects include fluid retention, heart failure, and osteopenia (167,168). Dipeptidyl peptidase 4 inhibitors do not interact with immunosuppressant drugs and have demonstrated safety in small clinical trials (169,170). Well-designed intervention trials examining the efficacy and safety of these and other antihyperglycemic agents in people with PTDM are needed.
Monogenic Diabetes Syndromes
Recommendations
2.23 Regardless of current age, all people diagnosed with diabetes in the first 6 months of life should have immediate genetic testing for neonatal diabetes. A
2.24 Children and young adults who do not have typical characteristics of type 1 or type 2 diabetes and who often have a family history of diabetes in successive generations (suggestive of an autosomal dominant pattern of inheritance) should have genetic testing for maturity-onset diabetes of the young. A
2.25 In both instances, consultation with a center specializing in diabetes genetics is recommended to understand the significance of genetic mutations and how best to approach further evaluation, treatment, and genetic counseling. E
Monogenic defects that cause β-cell dysfunction, such as neonatal diabetes and MODY, represent a small fraction of people with diabetes (<5%). Table 2.6 describes the most common causes of monogenic diabetes. For a comprehensive list of causes, see Genetic Diagnosis of Endocrine Disorders (171).
Table 2.6
Most common causes of monogenic diabetes (171)
| Gene | Inheritance | Clinical features | |
|---|---|---|---|
| MODY | HNF1A | AD | HNF1A-MODY: progressive insulin secretory defect with presentation in adolescence or early adulthood; lowered renal threshold for glucosuria; large rise in 2-h PG level on OGTT (>90 mg/dL [5 mmol/L]); sensitive to sulfonylureas |
| HNF4A | AD | HNF4A-MODY: progressive insulin secretory defect with presentation in adolescence or early adulthood; may have large birth weight and transient neonatal hypoglycemia; sensitive to sulfonylureas | |
| HNF1B | AD | HNF1B-MODY: developmental renal disease (typically cystic); genitourinary abnormalities; atrophy of the pancreas; hyperuricemia; gout | |
| GCK | AD | GCK-MODY: higher glucose threshold (set point) for glucose-stimulated insulin secretion, causing stable, nonprogressive elevated fasting blood glucose; typically, does not require treatment; microvascular complications are rare; small rise in 2-h PG level on OGTT (<54 mg/dL [3 mmol/L]) | |
| Neonatal diabetes | KCNJ11 | AD | Permanent or transient: IUGR; possible developmental delay and seizures; responsive to sulfonylureas |
| INS | AD | Permanent: IUGR; insulin requiring | |
| ABCC8 | AD | Permanent or transient: IUGR; rarely developmental delay; responsive to sulfonylureas | |
| 6q24 (PLAGL1, HYMA1) | AD for paternal duplications | Transient: IUGR; macroglossia; umbilical hernia; mechanisms include UPD6, paternal duplication, or maternal methylation defect; may be treatable with medications other than insulin | |
| GATA6 | AD | Permanent: pancreatic hypoplasia; cardiac malformations; pancreatic exocrine insufficiency; insulin requiring | |
| EIF2AK3 | AR | Permanent: Wolcott-Rallison syndrome: epiphyseal dysplasia; pancreatic exocrine insufficiency; insulin requiring | |
| EIF2B1 | AD | Permanent diabetes: can be associated with fluctuating liver function (172) | |
| FOXP3 | X-linked | Permanent: immunodysregulation, polyendocrinopathy, enteropathy X-linked (IPEX) syndrome: autoimmune diabetes, autoimmune thyroid disease, exfoliative dermatitis; insulin requiring |
AD, autosomal dominant; AR, autosomal recessive; IUGR, intrauterine growth restriction; OGTT, oral glucose tolerance test; UPD6, uniparental disomy of chromosome 6; 2-h PG, 2-h plasma glucose.
Neonatal Diabetes
Diabetes occurring under 6 months of age is termed “neonatal” or “congenital” diabetes, and about 80–85% of cases can be found to have an underlying monogenic cause (8,172–175). Neonatal diabetes occurs much less often after 6 months of age, whereas autoimmune type 1 diabetes rarely occurs before 6 months of age. Neonatal diabetes can either be transient or permanent. Transient diabetes is most often due to overexpression of genes on chromosome 6q24, is recurrent in about half of cases, and may be treatable with medications other than insulin. Permanent neonatal diabetes is most commonly due to autosomal dominant mutations in the genes encoding the Kir6.2 subunit (KCNJ11) and SUR1 subunit (ABCC8) of the β-cell KATP channel. A recent report details a de novo mutation in EIF2B1 affecting eIF2 signaling associated with permanent neonatal diabetes and hepatic dysfunction, similar to Wolcott-Rallison syndrome but with few severe comorbidities (176). The recent ADA-European Association for the Study of Diabetes type 1 diabetes consensus report recommends that regardless of current age, individuals diagnosed under 6 months of age should have genetic testing (8). Correct diagnosis has critical implications because 30–50% of people with KATP-related neonatal diabetes will exhibit improved blood glucose levels when treated with high-dose oral sulfonylureas instead of insulin. Insulin gene (INS) mutations are the second most common cause of permanent neonatal diabetes, and while intensive insulin management is currently the preferred treatment strategy, there are important genetic counseling considerations, as most of the mutations that cause diabetes are dominantly inherited.
Maturity-Onset Diabetes of the Young
MODY is frequently characterized by onset of hyperglycemia at an early age (classically before age 25 years, although diagnosis may occur at older ages). MODY is characterized by impaired insulin secretion with minimal or no defects in insulin action (in the absence of coexistent obesity). It is inherited in an autosomal dominant pattern with abnormalities in at least 13 genes on different chromosomes identified to date (177). The most commonly reported forms are GCK-MODY (MODY2), HNF1A-MODY (MODY3), and HNF4A-MODY (MODY1).
For individuals with MODY, the treatment implications are considerable and warrant genetic testing (178,179). Clinically, people with GCK-MODY exhibit mild, stable fasting hyperglycemia and do not require antihyperglycemic therapy except commonly during pregnancy. Individuals with HNF1A- or HNF4A-MODY usually respond well to low doses of sulfonylureas, which are considered first-line therapy; in some instances, insulin will be required over time. Mutations or deletions in HNF1B are associated with renal cysts and uterine malformations (renal cysts and diabetes [RCAD] syndrome). Other extremely rare forms of MODY have been reported to involve other transcription factor genes, including PDX1 (IPF1) and NEUROD1.
Diagnosis of Monogenic Diabetes
A diagnosis of one of the three most common forms of MODY, including HFN1A-MODY, GCK-MODY, and HNF4A-MODY, allows for more cost-effective therapy (no therapy for GCK-MODY; sulfonylureas as first-line therapy for HNF1A-MODY and HNF4A-MODY). Additionally, diagnosis can lead to identification of other affected family members. Genetic screening is increasingly available and cost-effective (176,178).
A diagnosis of MODY should be considered in individuals who have atypical diabetes and multiple family members with diabetes not characteristic of type 1 or type 2 diabetes, although admittedly, “atypical diabetes” is becoming increasingly difficult to precisely define in the absence of a definitive set of tests for either type of diabetes (173–175,178–184). In most cases, the presence of autoantibodies for type 1 diabetes precludes further testing for monogenic diabetes, but the presence of autoantibodies in people with monogenic diabetes has been reported (185). Individuals in whom monogenic diabetes is suspected should be referred to a specialist for further evaluation if available, and consultation can be obtained from several centers. Readily available commercial genetic testing following the criteria listed below now enables a cost-effective (186), often cost-saving, genetic diagnosis that is increasingly supported by health insurance. A biomarker screening pathway, such as the combination of urinary C-peptide/creatinine ratio and antibody screening, may aid in determining who should get genetic testing for MODY (187). It is critical to correctly diagnose one of the monogenic forms of diabetes because these individuals may be incorrectly diagnosed with type 1 or type 2 diabetes, leading to suboptimal, even potentially harmful, treatment plans and delays in diagnosing other family members (188). The correct diagnosis is especially critical for those with GCK-MODY mutations, where multiple studies have shown that no complications ensue in the absence of glucose-lowering therapy (189). The risks of microvascular and macrovascular complications with HNFIA- and HNF4A-MODY are similar to those observed in people with type 1 and type 2 diabetes (190,191). Genetic counseling is recommended to ensure that affected individuals understand the patterns of inheritance and the importance of a correct diagnosis and addressing comprehensive cardiovascular risk.
The diagnosis of monogenic diabetes should be considered in children and adults diagnosed with diabetes in early adulthood with the following findings:
Diabetes diagnosed within the first 6 months of life (with occasional cases presenting later, mostly INS and ABCC8 mutations) (172,192)
Diabetes without typical features of type 1 or type 2 diabetes (negative diabetes-associated autoantibodies, no obesity, lacking other metabolic features, especially with strong family history of diabetes)
Stable, mild fasting hyperglycemia (100–150 mg/dL [5.5–8.5 mmol/L]), stable A1C between 5.6% and 7.6% (between 38 and 60 mmol/mol), especially if no obesity
Pancreatic Diabetes or Diabetes in the Context of Disease of the Exocrine Pancreas
Pancreatic diabetes includes both structural and functional loss of glucose-normalizing insulin secretion in the context of exocrine pancreatic dysfunction and is commonly misdiagnosed as type 2 diabetes. Hyperglycemia due to general pancreatic dysfunction has been called “type 3c diabetes,” and, more recently, diabetes in the context of disease of the exocrine pancreas has been termed pancreoprivic diabetes (1). The diverse set of etiologies includes pancreatitis (acute and chronic), trauma or pancreatectomy, neoplasia, cystic fibrosis (addressed elsewhere in this chapter), hemochromatosis, fibrocalculous pancreatopathy, rare genetic disorders (193), and idiopathic forms (1); as such, pancreatic diabetes is the preferred umbrella terminology.
Pancreatitis, even a single bout, can lead to postpancreatitis diabetes mellitus (PPDM). Both acute and chronic pancreatitis can lead to PPDM, and the risk is highest with recurrent bouts. A distinguishing feature is concurrent pancreatic exocrine insufficiency (according to the monoclonal fecal elastase 1 test or direct function tests), pathological pancreatic imaging (endoscopic ultrasound, MRI, computed tomography), and absence of type 1 diabetes-associated autoimmunity (194–199). There is loss of both insulin and glucagon secretion and often higher-than-expected insulin requirements. Risk for microvascular complications appears to be similar to that of other forms of diabetes. In the context of pancreatectomy, islet autotransplantation can be done to retain insulin secretion (200,201). In some cases, autotransplant can lead to insulin independence. In others, it may decrease insulin requirements (202).
Gestational Diabetes Mellitus
Recommendations
2.26a In individuals who are planning pregnancy, screen those with risk factors B and consider testing all individuals of childbearing potential for undiagnosed diabetes. E
2.26b Before 15 weeks of gestation, test individuals with risk factors B and consider testing all individuals E for undiagnosed diabetes at the first prenatal visit using standard diagnostic criteria if not screened preconception.
2.26c Individuals of childbearing potential identified as having diabetes should be treated as such. A
2.26d Before 15 weeks of gestation, screen for abnormal glucose metabolism to identify individuals who are at higher risk of adverse pregnancy and neonatal outcomes, are more likely to need insulin, and are at high risk of a later gestational diabetes mellitus diagnosis. B Treatment may provide some benefit. E
2.26e Screen for early abnormal glucose metabolism using fasting glucose of 110–125 mg/dL (6.1 mmol/L) or A1C 5.9–6.4% (41–47 mmol/mol). B
2.27 Screen for gestational diabetes mellitus at 24–28 weeks of gestation in pregnant individuals not previously found to have diabetes or high-risk abnormal glucose metabolism detected earlier in the current pregnancy. A
2.28 Screen individuals with gestational diabetes mellitus for prediabetes or diabetes at 4–12 weeks postpartum, using the 75-g oral glucose tolerance test and clinically appropriate nonpregnancy diagnostic criteria. B
2.29 Individuals with a history of gestational diabetes mellitus should have lifelong screening for the development of diabetes or prediabetes at least every 3 years. B
2.30 Individuals with a history of gestational diabetes mellitus found to have prediabetes should receive intensive lifestyle interventions and/or metformin to prevent diabetes. A
Definition
For many years, GDM was defined as any degree of glucose intolerance that was first recognized during pregnancy (86), regardless of the degree of hyperglycemia. This definition facilitated a uniform strategy for detection and classification of GDM, but this definition has serious limitations (203). First, the best available evidence reveals that many cases of GDM represent preexisting hyperglycemia that is detected by routine screening in pregnancy, as routine screening is not widely performed in nonpregnant individuals of reproductive age. It is the severity of hyperglycemia that is clinically important with regard to both short- and long-term maternal and fetal risks.
The ongoing epidemic of obesity and diabetes has led to more type 2 diabetes in people of reproductive age, with an increase in the number of pregnant individuals with undiagnosed type 2 diabetes in early pregnancy (204–206). Ideally, undiagnosed diabetes should be identified preconception in individuals with risk factors or in high-risk populations (207–212), as the preconception care of people with preexisting diabetes results in lower A1C and reduced risk of birth defects, preterm delivery, perinatal mortality, small-for-gestational-age birth weight, and neonatal intensive care unit admission (213). If individuals are not screened prior to pregnancy, universal early screening at <15 weeks of gestation for undiagnosed diabetes may be considered over selective screening (Table 2.3), particularly in populations with high prevalence of risk factors and undiagnosed diabetes in people of childbearing age. Strong racial and ethnic disparities exist in the prevalence of undiagnosed diabetes. Therefore, early screening provides an initial step to identify these health disparities so that they can begin to be addressed (209–212). Standard diagnostic criteria for identifying undiagnosed diabetes in early pregnancy are the same as those used in the nonpregnant population (Table 2.2). Individuals found to have diabetes by the standard diagnostic criteria used outside of pregnancy should be classified as having diabetes complicating pregnancy (most often type 2 diabetes, rarely type 1 diabetes or monogenic diabetes) and managed accordingly.
Early abnormal glucose metabolism, defined as fasting glucose threshold of 110 mg/dL (6.1 mmol/L) or an A1C of 5.9% (39 mmol/mol), may identify individuals who are at higher risk of adverse pregnancy and neonatal outcomes (preeclampsia, macrosomia, shoulder dystocia, perinatal death), are more likely to need insulin treatment, and are at high risk of a later GDM diagnosis (214–220). An A1C threshold of 5.7% has not been shown to be associated with adverse perinatal outcomes (221,222).
If early screening is negative, individuals should be rescreened for GDM between 24 and 28 weeks of gestation (see Section 15, “Management of Diabetes in Pregnancy”). The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) GDM diagnostic criteria for the 75-g OGTT, as well as the GDM screening and diagnostic criteria used in the two-step approach, were not derived from data in the first half of pregnancy and should not be used for early screening (223). To date, most randomized controlled trials of treatment of early abnormal glucose metabolism have been underpowered for outcomes. Therefore, the benefits of treatment for early abnormal glucose metabolism remain uncertain. Nutrition counseling and periodic “block” testing of glucose levels weekly to identify individuals with high glucose levels are suggested. Testing frequency may proceed to daily, and treatment may be intensified, if the fasting glucose is predominantly >110 mg/dL prior to 18 weeks of gestation.
Both the fasting glucose and A1C are low-cost tests. An advantage of the A1C is its convenience, as it can be added to the prenatal laboratories and does not require an early-morning fasting appointment. Disadvantages include inaccuracies in the presence of increased red blood cell turnover and hemoglobinopathies (usually reads lower) and higher values with anemia and reduced red blood cell turnover (224). A1C is not reliable to screen for GDM or for preexisting diabetes at 15 weeks of gestation or later. See Recommendation 2.3 above.
GDM is often indicative of underlying β-cell dysfunction (225), which confers marked increased risk for later development of diabetes, generally but not always type 2 diabetes, in the mother after delivery (226,227). As effective prevention interventions are available (228,229), individuals diagnosed with GDM should receive lifelong screening for prediabetes to allow interventions to reduce diabetes risk and for type 2 diabetes to allow treatment at the earliest possible time (230).
Diagnosis
GDM carries risks for the mother, fetus, and neonate. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study (231), a large-scale multinational cohort study completed by more than 23,000 pregnant individuals, demonstrated that risk of adverse maternal, fetal, and neonatal outcomes continuously increased as a function of maternal glycemia at 24–28 weeks of gestation, even within ranges previously considered normal for pregnancy. For most complications, there was no threshold for risk. These results have led to careful reconsideration of the diagnostic criteria for GDM.
GDM diagnosis (Table 2.7) can be accomplished with either of two strategies:
The “one-step” 75-g OGTT derived from the IADPSG criteria, or
The older “two-step” approach with a 50-g (nonfasting) screen followed by a 100-g OGTT for those who screen positive based on the work of Carpenter-Coustan’s interpretation of the older O’Sullivan and Mahan (232) criteria.
Table 2.7
Screening for and diagnosis of GDM
| One-step strategy |
| Perform a 75-g OGTT, with plasma glucose measurement when patient is fasting and at 1 and 2 h, at 24–28 weeks of gestation in individuals not previously diagnosed with diabetes. |
| The OGTT should be performed in the morning after an overnight fast of at least 8 h. |
| The diagnosis of GDM is made when any of the following plasma glucose values are met or exceeded: |
 • Fasting: 92 mg/dL (5.1 mmol/L) • Fasting: 92 mg/dL (5.1 mmol/L) |
 • 1 h: 180 mg/dL (10.0 mmol/L) • 1 h: 180 mg/dL (10.0 mmol/L) |
 • 2 h: 153 mg/dL (8.5 mmol/L) • 2 h: 153 mg/dL (8.5 mmol/L) |
| Two-step strategy |
| Step 1: Perform a 50-g GLT (nonfasting), with plasma glucose measurement at 1 h, at 24–28 weeks of gestation in individuals not previously diagnosed with diabetes. |
| If the plasma glucose level measured 1 h after the load is ≥130, 135, or 140 mg/dL (7.2, 7.5, or 7.8 mmol/L, respectively), proceed to a 100-g OGTT. |
| Step 2: The 100-g OGTT should be performed when the patient is fasting. |
| The diagnosis of GDM is made when at least two* of the following four plasma glucose levels (measured fasting and at 1, 2, and 3 h during OGTT) are met or exceeded (Carpenter-Coustan criteria [251]): |
 • Fasting: 95 mg/dL (5.3 mmol/L) • Fasting: 95 mg/dL (5.3 mmol/L) |
 • 1 h: 180 mg/dL (10.0 mmol/L) • 1 h: 180 mg/dL (10.0 mmol/L) |
 • 2 h: 155 mg/dL (8.6 mmol/L) • 2 h: 155 mg/dL (8.6 mmol/L) |
 • 3 h: 140 mg/dL (7.8 mmol/L) • 3 h: 140 mg/dL (7.8 mmol/L) |
GDM, gestational diabetes mellitus; GLT, glucose load test; OGTT, oral glucose tolerance test.
Different diagnostic criteria will identify different degrees of maternal hyperglycemia and maternal/fetal risk, leading some experts to debate, and disagree on, optimal strategies for the diagnosis of GDM.
One-Step Strategy
The IADPSG defined diagnostic cut points for GDM as the average fasting, 1-h, and 2-h PG values during a 75-g OGTT in individuals at 24–28 weeks of gestation who participated in the HAPO study at which odds for adverse outcomes reached 1.75 times the estimated odds of these outcomes at the mean fasting, 1-h, and 2-h PG levels of the study population. This one-step strategy was anticipated to significantly increase the incidence of GDM (from 5–6% to 15–20%), primarily because only one abnormal value, not two, became sufficient to make the diagnosis (233). Many regional studies have investigated the impact of adopting the IADPSG criteria on prevalence and have seen a roughly one- to threefold increase (234). The anticipated increase in the incidence of GDM could have a substantial impact on costs and medical infrastructure needs and has the potential to “medicalize” pregnancies previously categorized as normal. A recent follow-up study of individuals participating in a blinded study of pregnancy OGTTs found that 11 years after their pregnancies, individuals who would have been diagnosed with GDM by the one-step approach, as compared with those without, were at 3.4-fold higher risk of developing prediabetes and type 2 diabetes and had children with a higher risk of obesity and increased body fat, suggesting that the larger group of individuals identified by the one-step approach would benefit from the increased screening for diabetes and prediabetes that would accompany a history of GDM (235,236). The ADA recommends the IADPSG diagnostic criteria with the intent of optimizing gestational outcomes because these criteria are the only ones based on pregnancy outcomes rather than end points such as prediction of subsequent maternal diabetes.
The expected benefits of using IADPSG criteria to the offspring are inferred from intervention trials that focused on individuals with lower levels of hyperglycemia than identified using older GDM diagnostic criteria. Those trials found modest benefits including reduced rates of large-for-gestational-age births and preeclampsia (237,238). It is important to note that 80–90% of participants being treated for mild GDM in these two randomized controlled trials could be managed with lifestyle therapy alone. The OGTT glucose cutoffs in these two trials overlapped the thresholds recommended by the IADPSG, and in one trial (238), the 2-h PG threshold (140 mg/dL [7.8 mmol/L]) was lower than the cutoff recommended by the IADPSG (153 mg/dL [8.5 mmol/L]).
No randomized controlled trials of treating versus not treating GDM diagnosed by the IADPSG criteria but not the Carpenter-Coustan criteria have been published to date. However, a recent randomized trial of testing for GDM at 24–28 weeks of gestation by the one-step method using IADPSG criteria versus the two-step method using a 1-h 50-g glucose loading test (GLT) and, if positive, a 3-h OGTT by Carpenter-Coustan criteria identified twice as many individuals with GDM using the one-step method compared with the two-step method. Despite treating more individuals for GDM using the one-step method, there was no difference in pregnancy and perinatal complications (239). However, concerns have been raised about sample size estimates and unanticipated suboptimal engagement with the protocol with regard to screening and treatment. For example, in the two-step group, 165 participants who did not get counted as having GDM were treated for isolated elevated fasting glucose >95 mg/dL (240). The high prevalence of prediabetes in people of childbearing age may support the more inclusive IADPSG criteria. NHANES data demonstrate a 21.5% prevalence of prediabetes in people of reproductive age 20–44 years, which is comparable to or higher than the prevalence of GDM diagnosed by the one-step method (241).
The one-step method identifies the long-term risks of maternal prediabetes and diabetes and offspring abnormal glucose metabolism and adiposity. Post hoc GDM in individuals diagnosed by the one-step method in the HAPO cohort was associated with higher prevalence of IGT; higher 30-min, 1-h, and 2-h glucoses during the OGTT; and reduced insulin sensitivity and oral disposition index in their offspring at 10–14 years of age compared with offspring of mothers without GDM. Associations of mother’s fasting, 1-h, and 2-h values on the 75-g OGTT were continuous with a comprehensive panel of offspring metabolic outcomes (236,242). In addition, HAPO Follow-up Study (HAPO FUS) data demonstrate that neonatal adiposity and fetal hyperinsulinemia (cord C-peptide), both higher across the continuum of maternal hyperglycemia, are mediators of childhood body fat (243).
Data are lacking on how the treatment of mother’s hyperglycemia in pregnancy affects her offspring’s risk for obesity, diabetes, and other metabolic disorders. Additional well-designed clinical studies are needed to determine the optimal intensity of monitoring and treatment of individuals with GDM diagnosed by the one-step strategy (244,245).
Two-Step Strategy
In 2013, the NIH convened a consensus development conference to consider diagnostic criteria for diagnosing GDM (246). The 15-member panel had representatives from obstetrics and gynecology, maternal-fetal medicine, pediatrics, diabetes research, biostatistics, and other related fields. The panel recommended a two-step approach to screening that used a 1-h 50-g GLT followed by a 3-h 100-g OGTT for those who screened positive. The American College of Obstetricians and Gynecologists (ACOG) recommends any of the commonly used thresholds of 130, 135, or 140 mg/dL for the 1-h 50-g GLT (247). Updated from 2014, a 2021 U.S. Preventive Services Task Force systematic review continues to conclude that one-step versus two-step screening is associated with increased likelihood of GDM (11.5% vs. 4.9%) but without improved health outcomes. It reports that the oral glucose challenge test using 140 or 135 mg/dL thresholds had sensitivities of 82% and 93% and specificities of 82% and 79%, respectively, against Carpenter-Coustan criteria. Fasting plasma glucose cutoffs of 85 mg/dL or 90 mg/dL had sensitivities of 88% and 81% and specificities of 73% and 82%, respectively, against Carpenter-Coustan criteria (248). The use of A1C at 24–28 weeks of gestation as a screening test for GDM does not function as well as the GLT (249).
Key factors cited by the NIH panel in their decision-making process were the lack of clinical trial data demonstrating the benefits of the one-step strategy and the potential negative consequences of identifying a large group of individuals with GDM, including medicalization of pregnancy with increased health care utilization and costs. Moreover, screening with a 50-g GLT does not require fasting and therefore is easier to accomplish for many individuals. Treatment of higher-threshold maternal hyperglycemia, as identified by the two-step approach, reduces rates of neonatal macrosomia, large-for-gestational-age births (250), and shoulder dystocia without increasing small-for-gestational-age births. ACOG currently supports the two-step approach but notes that one elevated value, as opposed to two, may be used for the diagnosis of GDM (247). If this approach is implemented, the incidence of GDM by the two-step strategy will likely increase markedly. ACOG recommends either of two sets of diagnostic thresholds for the 3-h 100-g OGTT–Carpenter-Coustan or National Diabetes Data Group (251,252). Each is based on different mathematical conversions of the original recommended thresholds by O’Sullivan and Mahan (232), which used whole blood and nonenzymatic methods for glucose determination. A secondary analysis of data from a randomized clinical trial of identification and treatment of mild GDM (253) demonstrated that treatment was similarly beneficial in people meeting only the lower thresholds per Carpenter-Coustan (251) and in those meeting only the higher thresholds per National Diabetes Data Group (252). If the two-step approach is used, it would appear advantageous to use the Carpenter-Coustan lower diagnostic thresholds, as shown in step 2 in Table 2.7.
Future Considerations
The conflicting recommendations from expert groups underscore the fact that there are data to support each strategy. A systematic review of economic evaluations of GDM screening found that the one-step method identified more cases of GDM and was more likely to be cost-effective than the two-step method (254). The decision of which strategy to implement must therefore be made based on the relative values placed on factors that have yet to be measured (e.g., willingness to change practice based on correlation studies rather than intervention trial results, available infrastructure, and importance of cost considerations).
The IADPSG criteria (“one-step strategy”) have been adopted internationally as the preferred approach. Data comparing population-wide outcomes with one-step versus two-step approaches have been inconsistent to date (239,255–257). In addition, pregnancies complicated by GDM per the IADPSG criteria, but not recognized as such, have outcomes comparable to pregnancies with diagnosed GDM by the more stringent two-step criteria (258,259). There remains strong consensus that establishing a uniform approach to diagnosing GDM will benefit patients, caregivers, and policymakers. Longer-term outcome studies are currently underway.
Footnotes
Disclosure information for each author is available at https://doi.org/10.2337/dc23-SDIS.
Suggested citation: ElSayed NA, Aleppo G, Aroda VR, et al., American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2023;46(Suppl. 1):S19–S40
References
 months following diagnosis of type 1 diabetes: an ADDRESS-2 (After Diagnosis Diabetes Research Support System-2) study analysis. Diabetes Res Clin Pract
2019;155:107789. [Abstract] [Google Scholar]
months following diagnosis of type 1 diabetes: an ADDRESS-2 (After Diagnosis Diabetes Research Support System-2) study analysis. Diabetes Res Clin Pract
2019;155:107789. [Abstract] [Google Scholar]Articles from Diabetes Care are provided here courtesy of American Diabetes Association
Full text links
Read article at publisher's site: https://doi.org/10.2337/dc23-s002
Read article for free, from open access legal sources, via Unpaywall:
https://diabetesjournals.org/care/article-pdf/46/Supplement_1/S19/696898/dc23s002.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/140157908
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.2337/dc23-s002
Article citations
The combined predictive power of the atherogenic index of plasma and serum glycated albumin for cardiovascular events in postmenopausal patients with acute coronary syndrome after percutaneous coronary intervention.
Lipids Health Dis, 23(1):352, 30 Oct 2024
Cited by: 0 articles | PMID: 39478539 | PMCID: PMC11523790
Gut microbiota predict retinopathy in patients with diabetes: A longitudinal cohort study.
Appl Microbiol Biotechnol, 108(1):497, 28 Oct 2024
Cited by: 0 articles | PMID: 39466432 | PMCID: PMC11519154
Bibliometric and visual analysis of SGLT2 inhibitors in cardiovascular diseases.
Front Pharmacol, 15:1437760, 30 Oct 2024
Cited by: 0 articles | PMID: 39539627 | PMCID: PMC11557488
Association between the weight-adjusted-waist index and testosterone deficiency in adult males: a cross-sectional study.
Sci Rep, 14(1):25574, 26 Oct 2024
Cited by: 0 articles | PMID: 39462140 | PMCID: PMC11513048
Is pulmonary vascular remodeling an intermediate link between hyperglycemia and adverse outcomes in patients with idiopathic pulmonary arterial hypertension? Insights from a multi-center cohort study.
Cardiovasc Diabetol, 23(1):384, 28 Oct 2024
Cited by: 0 articles | PMID: 39468502 | PMCID: PMC11520901
Go to all (523) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2024.
Diabetes Care, 47(suppl 1):S20-S42, 01 Jan 2024
Cited by: 141 articles | PMID: 38078589
Review
17. Diabetes Advocacy: Standards of Care in Diabetes-2023.
Diabetes Care, 46(suppl 1):S279-S280, 01 Jan 2023
Cited by: 0 articles | PMID: 36507643 | PMCID: PMC9810458
Review Free full text in Europe PMC
7. Diabetes Technology: Standards of Care in Diabetes-2023.
Diabetes Care, 46(suppl 1):S111-S127, 01 Jan 2023
Cited by: 93 articles | PMID: 36507635 | PMCID: PMC9810474
Review Free full text in Europe PMC
6. Glycemic Targets: Standards of Care in Diabetes-2023.
Diabetes Care, 46(suppl 1):S97-S110, 01 Jan 2023
Cited by: 200 articles | PMID: 36507646 | PMCID: PMC9810469
Review Free full text in Europe PMC




