Abstract
Free full text

Predicting Prediabetes and Diabetes
Atherosclerosis begins in youth, and the extent of coronary lesions in adolescents is associated with individual and combined levels of risk factors including lipids, smoking, blood pressure, obesity, and—the focus of this editorial—hyperglycemia.1,2 These risk factors tend to track from childhood to adulthood; children with elevated risk factor levels tend to retain them as they grow, thus becoming adults at higher risk of cardiovascular disease.
Of these risk factors, hyperglycemia is a special case. Hyperglycemia heralds diabetes. Diabetes is not only a risk factor for heart and stroke but, because of its myriad vascular and neurologic effects, it is also a major cause of renal disease, blindness, amputations, dental disease, pregnancy complications, peripheral neuropathy, and sexual dysfunction.3 With the obesity epidemic, type 2 diabetes is becoming more common in the pediatrician’s office in the West, and probably will soon in the developing world, where rates of adult diabetes are skyrocketing.4
Hyperglycemia is special for another reason, too. Unlike the continuous and graded relationship between most risk factors and heart disease, the association between glucose level and some diabetic complications exhibits a threshold. Risk of retinopathy, for example, rises steeply above a glycosylated hemoglobin (A1c) level of between 6.0% and 6.5%. These observations underlie the new international recommendations to use hemoglobin A1c level to screen for diabetes in children and adults, with 6.5% as the diagnostic cutoff point.5 Over time, hemoglobin A1c level is likely to replace the inconvenient fasting glucose (diabetes cutoff point, 126 mg/dL, [to convert to millimoles per liter, multiply by 0.0555]) and the cumbersome oral glucose tolerance test.
While type 2 diabetes is becoming more common, it still affects less than 1% of adolescents in the United States.6 More common is prediabetes, reflected in glucose levels that don’t quite reach diabetic status, either as impaired fasting glucose or as impaired glucose tolerance on the basis of oral glucose tolerance testing. This is where deciding the right cutoff point gets tricky. In adults, predicting who will develop diabetes itself using glucose levels is not so clear because the relationship is continuous. The farther from 126 mg/dL or 6.5%, the lower the risk of subsequent diabetes, with no apparent threshold.5 This is why, when an expert committee decided 6 years ago to lower the cutoff point for impaired fasting glucose from 110 to 100 mg/dL, there was a hue and cry from some quarters.7
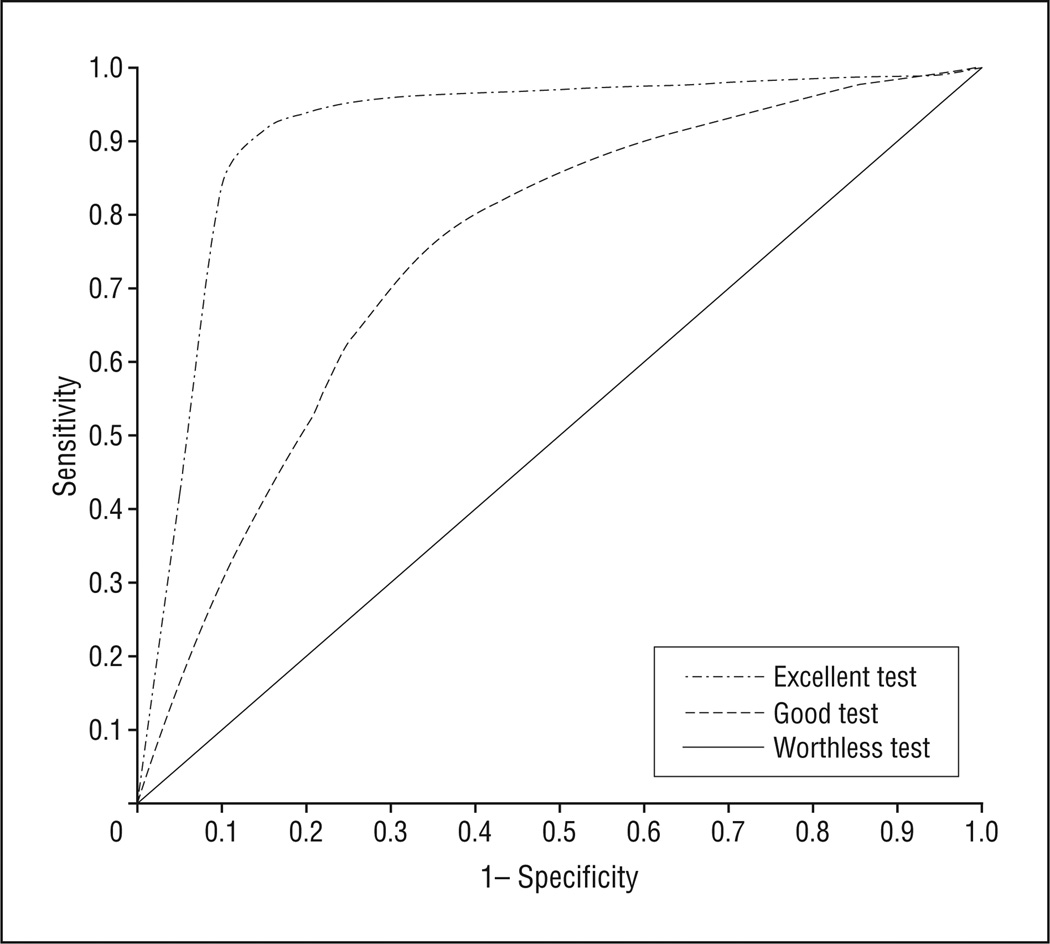
Setting cutoff points for screening tests that are continuous variables is an unenviable task. No test predicts outcomes perfectly. We typically estimate how well a test performs with sensitivity and specificity. The unpleasant reality is that if we choose a cutoff point that increases sensitivity (can’t miss all those kids who might be at risk), we necessarily lower specificity (that’s a lot of kids to evaluate to find 1 who will actually get diabetes). Analogously, increasing the specificity will lower sensitivity.
One way to display sensitivity and specificity together is the receiver operating characteristic curve (Figure). The higher and more to the left the curve is, the better the test. The problem is that most receiver operating characteristic practitioners assume that the point on the curve closest to the upper left corner represents the ideal cutoff point because, generally, it simultaneously maximizes sensitivity and specificity.
In reality, however, the ideal cutoff point would minimize cost and risk while maximizing benefit.8,9 The math is tractable, but finding values for these parameters is often challenging. It is difficult, for example, to account for all of the downstream consequences of falsely (or even truly) labeling a child as prediabetic. They include not only the cost of the initial test, but also costs of subsequent diagnostic evaluations, possible reduction in quality of life for children and parents, and inefficient interventions to lower glucose, insulin, or other risk factors. In the absence of decades-long randomized trials that will likely never occur, decision analytic techniques can help but they are rarely used.10
Against this background emerge the results from the venerable Bogalusa Heart Study published in this issue. 11 It is not surprising that a higher fasting glucose level in childhood predicts prediabetes and diabetes in adulthood. More surprising is that, at least for predicting prediabetes, there appeared to be a threshold rather than a continuous function. The prevalence of prediabetes was 6% to 7% among adults whose childhood glucose exceeded 86 mg/dL but only around 2% for lower childhood glucose levels. For frank diabetes, no clear threshold was apparent.
The authors are appropriately circumspect about recommending lowering glucose cutoff points to diagnose children at risk of developing prediabetes or diabetes. Even if there is a threshold over which children are at substantially higher risk of later prediabetes, it is unclear exactly how high the risk should be to make changing guidelines a good thing. Is 7% high enough, or would it have to be 10%, 25%, or 50% to make branding these children sensible? After all, the right interventions for individuals with prediabetes are still obscure, so identifying more of them may be more trouble than it’s worth. It is also well to keep in mind that obesity was much less common when the Bogalusa study started. In fact, no child in the published study appeared to have a fasting glucose level of more than 100 mg/dL, the currently recommended cutoff point. From this cohort, therefore, it is impossible to know the magnitude of increased risk among children with today’s definition of impaired fasting glucose level compared with children who have lower glucose levels.
While researchers continue to try to solve these complex issues regarding whom to screen and how, there seems to be a seismic shift happening in the United States. For the first time in 30 years, childhood obesity rates appear to have leveled off, at least in some demographic groups. Because excess adiposity is by far the biggest risk factor for diabetes, and it also causes hypertension and lipid abnormalities, a downward shift in the population distribution of childhood and adolescent body mass index is critical for the prevention of diabetes and cardiovascular disease. The coming years will tell if this shift is real, and if it is occurring in lower socioeconomic and minority groups as well as in better-off white individuals. If it is, then support of this movement has the best chance of reversing the trends toward increased diabetes and cardiovascular risk that has been so worrisome in recent years.
Acknowledgments
Funding/Support: This study was supported by grant K24 HL 68041 from the National Institutes of Health.
REFERENCES
Full text links
Read article at publisher's site: https://doi.org/10.1001/archpediatrics.2009.270
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc4350017?pdf=render
Subscription required at archpedi.ama-assn.org
http://archpedi.ama-assn.org/cgi/content/full/164/2/198
Subscription required at archpedi.ama-assn.org
http://archpedi.ama-assn.org/cgi/reprint/164/2/198.pdf
Free to read at archpedi.ama-assn.org
http://archpedi.ama-assn.org/cgi/content/abstract/164/2/198
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1001/archpediatrics.2009.270
Article citations
Cost-effectiveness of screening strategies for identifying pediatric diabetes mellitus and dysglycemia.
JAMA Pediatr, 167(1):32-39, 01 Jan 2013
Cited by: 21 articles | PMID: 23403824 | PMCID: PMC3837695
Lack of exercise is a major cause of chronic diseases.
Compr Physiol, 2(2):1143-1211, 01 Apr 2012
Cited by: 1001 articles | PMID: 23798298 | PMCID: PMC4241367
Review Free full text in Europe PMC
The efficacy and safety study of dietary supplement PURIAM110 on non-insulin taking Korean adults in the stage of pre-diabetes and diabetes mellitus: protocol for a randomized, double-blind, placebo-controlled, and multicenter trial-pilot study.
Trials, 12:38, 11 Feb 2011
Cited by: 1 article | PMID: 21310088 | PMCID: PMC3048555
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Prognostic value of insulin resistance and hyperglycemia biomarkers for long-term risks of cardiometabolic outcomes.
J Diabetes Complications, 37(9):108583, 02 Aug 2023
Cited by: 0 articles | PMID: 37579708 | PMCID: PMC10529933
Phenotyping the Prediabetic Population-A Closer Look at Intermediate Glucose Status and Cardiovascular Disease.
Int J Mol Sci, 22(13):6864, 25 Jun 2021
Cited by: 5 articles | PMID: 34202289 | PMCID: PMC8268766
Review Free full text in Europe PMC
HbA(1c) in the prediction of type 2 diabetes compared with fasting and 2-h post-challenge plasma glucose: The Asturias study (1998-2005).
Diabetes Metab, 37(1):27-32, 08 Oct 2010
Cited by: 15 articles | PMID: 20934897
[Prediabetes as a riskmarker for stress-induced hyperglycemia in critically ill adults].
Rev Med Inst Mex Seguro Soc, 55 Suppl 1:S14-S19, 01 Jan 2017
Cited by: 0 articles | PMID: 28212470
Funding
Funders who supported this work.
NHLBI NIH HHS (1)
Grant ID: K24 HL068041
NIDDK NIH HHS (2)
Grant ID: P30 DK040561-14
Grant ID: P30 DK040561