Abstract
Purpose
The purpose of this study is to examine the cost effect of surgeon and patient discretion in regard to cataract surgery and how this affects population health care costs.Methods
A model of cataract progression was created from preexisting published data and combined with mortality data and Medicare cataract statistics to estimate the effect of mortality on decreasing the rate of cataract surgery if surgery was delayed until any cataract progression occurred.Results
Five-year cataract progression rates were determined for a given patient age, sex, and type of cataract. Combined with 5-year death rates, delaying surgery until progression occurred resulted in a 1.1% decrease in surgery for nuclear sclerosis at age 45 that increased to a 33.8% decrease by age 90; a 1.5% decrease in surgery for cortical cataract at age 45 that increased to a 51.1% decrease by age 90; and a 1.6% decrease in surgery for posterior subcapsular at age 45 that increased to a 59.7% decrease by age 90. The effect of this decrease in surgical volume on Medicare was estimated to result in a 13% overall decrease in cataract surgery annually at a cost of ~$660 million dollars per year.Conclusion
Overall, we conclude that surgeon and patient discretion in regard to cataract surgery has a substantial cost effect with the potential to reduce surgical volume by as much as 13% by the decision to delay surgery as a result of patient mortality.Free full text
Cost effect of surgeon and patient discretion in regard to cataract surgery
Abstract
Purpose
The purpose of this study is to examine the cost effect of surgeon and patient discretion in regard to cataract surgery and how this affects population health care costs.
Methods
A model of cataract progression was created from preexisting published data and combined with mortality data and Medicare cataract statistics to estimate the effect of mortality on decreasing the rate of cataract surgery if surgery was delayed until any cataract progression occurred.
Results
Five-year cataract progression rates were determined for a given patient age, sex, and type of cataract. Combined with 5-year death rates, delaying surgery until progression occurred resulted in a 1.1% decrease in surgery for nuclear sclerosis at age 45 that increased to a 33.8% decrease by age 90; a 1.5% decrease in surgery for cortical cataract at age 45 that increased to a 51.1% decrease by age 90; and a 1.6% decrease in surgery for posterior subcapsular at age 45 that increased to a 59.7% decrease by age 90. The effect of this decrease in surgical volume on Medicare was estimated to result in a 13% overall decrease in cataract surgery annually at a cost of ~$660 million dollars per year.
Conclusion
Overall, we conclude that surgeon and patient discretion in regard to cataract surgery has a substantial cost effect with the potential to reduce surgical volume by as much as 13% by the decision to delay surgery as a result of patient mortality.
Introduction
The decision to pursue cataract surgery is a decision made by both the patient and surgeon in tandem. As cataract surgery techniques and outcomes have improved, patients have increasingly undergone surgery with better preoperative visual acuity and less severe cataracts.1 Accordingly, the rate of cataract surgery has dramatically increased.2 Due to a multitude of factors, patients and surgeons vary in regard to the degree of visual impairment at which the decision to pursue surgery is made.3,4 If a patient presents to a surgeon and the decision is made to delay surgery until the patient’s cataracts worsen, then older patients may not survive long enough to see cataract progression and then undergo cataract surgery. This study aims to examine the cost effect of this decision from a health care population perspective taking into account previously published cataract rates of progression and mortality rates.
Methods
Published data on cataract progression from the Longitudinal Study of Cataract,5,6 the Beaver Dam Eye Study,7 and the Melbourne Visual Impairment Project8 were collected. These studies report rates of cataract progression for different age ranges among both males and females; the Longitudinal Study of Cataract and the Beaver Dam Eye Study report data for all three primary types of cataract, while the Melbourne Visual Impairment Project only reports data for nuclear sclerotic and cortical cataracts. The rates from these data sets were then combined to create a weighted statistical average of cataract progression rate based on cataract type, patient age, and sex. Actuarial life table data from the Social Security Administration were then used to determine population death rates for given patient ages and sexes. Five-year cataract progression rates and death rates were then combined to determine if patients would survive long enough to experience progression of their cataracts. The effect of mortality on decreasing the amount of cataract surgery performed for a given patient age and sex if surgery was delayed until progression occurred was thus estimated. Finally, these data were combined with Medicare cataract surgery statistics9 to estimate the cost effect of delaying surgery.
Results
Cataract surgery progression rates were calculated for both males and females from age 45 to 90 for nuclear sclerosis, cortical, and posterior subcapsular cataracts. For a male with nuclear sclerosis, the 5-year rate of progression was found to increase from 33.9% at age 45 to 46.6% at age 90. For a male with cortical cataract, the 5-year rate of progression was found to increase from 12.6% at age 45 to 19.2% at age 90. For a male with posterior subcapsular cataract, the 5-year rate of progression was found to increase from 2.4% at age 45 to 5.6% at age 90. These data along with corresponding death rate data are presented in Figure 1. Similar data were determined for females as well but are not presented here. For males with nuclear sclerosis, it was calculated that the death rate would decrease the need for cataract surgery by 1.1% among 45-year-olds and 33.8% among 90-year-olds as shown in Table 1. A similar effect occurred for cortical cataracts and posterior subcapsular, and these rates are shown in Table 1. Again, this effect was calculated for both sexes but not presented here. The overall effect of mortality on decreasing surgical volume for a given age is demonstrated in Figure 2. Using Medicare statistics of recent cataract surgery rates and patient demographic data, an overall decrease in surgery volume of 13% or ~449,000 surgical cases among Medicare beneficiaries annually would be expected by delaying surgery until cataract progression occurs. The approximate total cost effect to Medicare would be $660 million dollars per year.
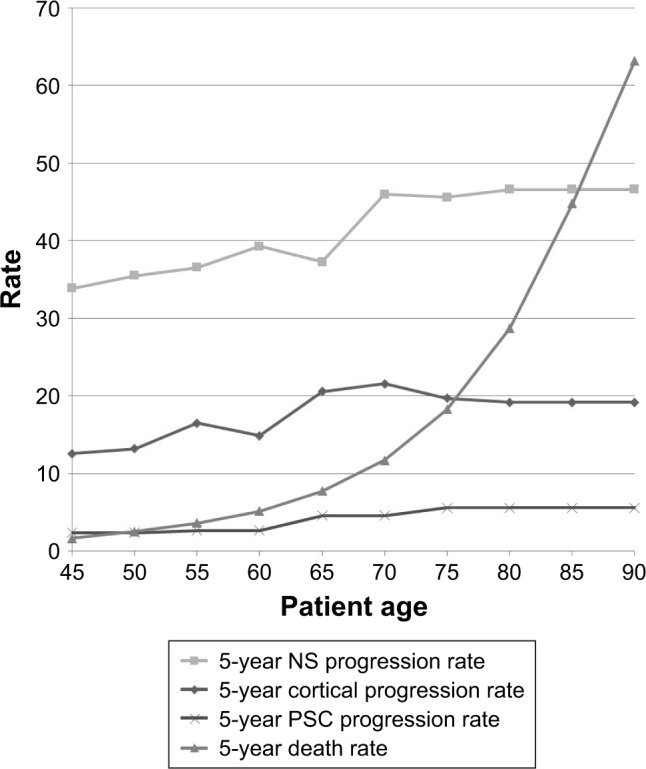
Cataract progression rate and death rate vs age among males.
Abbreviations: NS, nuclear sclerosis; PSC, posterior subcapsular.
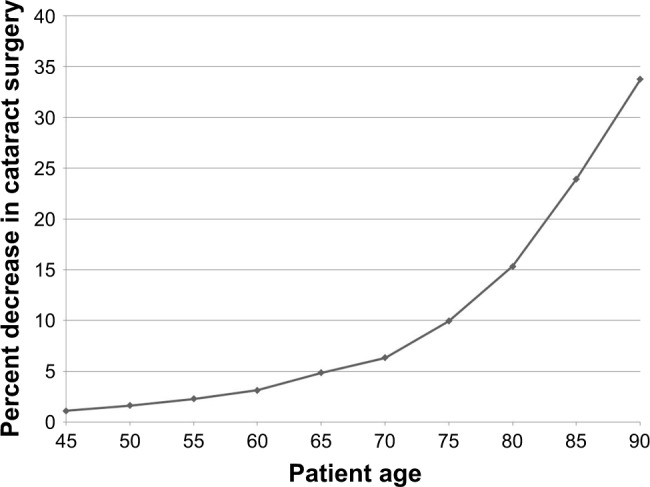
Estimated decrease in surgical volume vs age as a result of delaying surgery until cataract progression due to mortality.
Table 1
Effect of mortality on decreasing surgical volume if surgery is delayed until progression occurs for different types of cataract among males at various ages
| Age | Percent decrease in surgery for NS | Percent decrease in surgery for cortical | Percent decrease in surgery for PSC |
|---|---|---|---|
| 45 | 1.1 | 1.5 | 1.6 |
| 50 | 1.6 | 2.2 | 2.5 |
| 55 | 2.3 | 3.0 | 3.5 |
| 60 | 3.1 | 4.4 | 5.0 |
| 65 | 4.9 | 6.2 | 7.4 |
| 70 | 6.3 | 9.2 | 11.2 |
| 75 | 9.9 | 14.7 | 17.3 |
| 80 | 15.4 | 23.2 | 27.1 |
| 85 | 23.9 | 36.2 | 42.3 |
| 90 | 33.8 | 51.1 | 59.7 |
Abbreviations: NS, nuclear sclerosis; PSC, posterior subcapsular.
Discussion
Numerous studies have demonstrated the cost-effectiveness of cataract surgery.10,11 However, as the population ages, there is an ever increasing need to better utilize limited health care resources. The reimbursement model increasingly being pursued by Medicare is that of a population-based health care payment system as opposed to a fee for service system with the goal of decreasing health care spending.12 As the degree of visual impairment prior to surgery continues to decline and the rate of surgery continues to increase,1,2 surgeon and patient discretion regarding when to pursue surgery has the potential to have an increasingly significant effect on health care costs.
As cataract is an age-related problem, our analysis suggests that a significant decrease in Medicare costs could be obtained by delaying surgery merely from the effect of overall patient mortality. This effect is estimated to result in as much as a 13% reduction in cataract surgery volume among Medicare beneficiaries in the United States on an annual basis.
Our analysis is limited by the type and quality of available cataract progression data. This progression model for cataract utilized lens change based on physical exam and photographs. Moreover, our analysis only looks at economic effects and does not address patient quality-of-life measures. Other studies have suggested that delays in cataract surgery may significantly increase overall patient disability.13
Overall, we conclude that surgeon and patient discretion in regard to cataract surgery has a substantial cost effect with the potential to reduce surgical volume by as much as 13% by the decision to delay surgery as a result of patient mortality.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
Articles from Clinical Ophthalmology (Auckland, N.Z.) are provided here courtesy of Dove Press
Full text links
Read article at publisher's site: https://doi.org/10.2147/opth.s190184
Read article for free, from open access legal sources, via Unpaywall:
https://www.dovepress.com/getfile.php?fileID=46837
Citations & impact
Impact metrics
Article citations
A Mitochondrial Genome-Wide Association Study of Cataract in a Latino Population.
Transl Vis Sci Technol, 9(6):25, 23 May 2020
Cited by: 8 articles | PMID: 32821522 | PMCID: PMC7408807
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
A cost-minimization analysis comparing immediate sequential cataract surgery and delayed sequential cataract surgery from the payer, patient, and societal perspectives in the United States.
JAMA Ophthalmol, 132(11):1282-1288, 01 Nov 2014
Cited by: 19 articles | PMID: 25033037
Prescribing Patterns and Costs Associated with Postoperative Eye Drop Use in Medicare Beneficiaries Undergoing Cataract Surgery.
Ophthalmology, 127(5):573-581, 14 Nov 2019
Cited by: 9 articles | PMID: 31952884
A Revised Estimate of Costs Associated With Routine Preoperative Testing in Medicare Cataract Patients With a Procedure-Specific Indicator.
JAMA Ophthalmol, 136(3):231-238, 01 Mar 2018
Cited by: 13 articles | PMID: 29346472 | PMCID: PMC5885904
Sutureless Aortic Valve Replacement for Treatment of Severe Aortic Stenosis: A Single Technology Assessment of Perceval Sutureless Aortic Valve
Knowledge Centre for the Health Services at The Norwegian Institute of Public Health (NIPH), Oslo, Norway, 20 Mar 2018
Cited by: 0 articles | PMID: 29553663
ReviewBooks & documents Free full text in Europe PMC





