Abstract
Background and objectives
Home nursing is essential for children with medical complexity (CMC), but provision varies substantially across states. Our objectives were to quantify state-to-state variability in distribution of posthospitalization home nursing to commercially insured CMC and to rank-order states.Methods
Retrospective cohort study of hospitalized commercially insured children with ≥1 complex chronic condition from birth to 18 years of age in the Truven MarketScan database. Cohort eligibility criteria were hospital discharge between January 2013 and November 2016 and at least 30 days of follow-up after discharge. Two primary outcome measures were used: receipt of any home nursing within 30 days of hospital discharge (yes or no) and number of days of posthospitalization home nursing (1-30 days). A composite metric encompassing both receipt and quantity was created by evaluating the 95th percentile of days of home nursing (0-30 days).Results
Overall, 9.9% of the sample received home nursing. After we adjusted for patient characteristics, the probability of receiving home nursing varied across states, ranging from 3.4% to 19.2%. Among home nursing recipients, the adjusted median home nursing days across states ranged from 6.6 to 24.5 days. The adjusted 95th percentile of days of home nursing (across the entire of sample, including recipients and nonrecipients of home nursing) ranged from 6.8 to 22.6 days.Conclusions
We observed striking state-to-state variability in receipt of home nursing and mean number of days of posthospitalization home nursing among commercially insured CMC after adjustment for demographic and clinical differences. This suggests opportunities for state-level improvement.Free full text

State Variation in Posthospital Home Nursing for Commercially Insured Medically Complex Children
Abstract
BACKGROUND AND OBJECTIVES:
Home nursing is essential for children with medical complexity (CMC), but provision varies substantially across states. Our objectives were to quantify state-to-state variability in distribution of posthospitalization home nursing to commercially insured CMC and to rank-order states.
METHODS:
Retrospective cohort study of hospitalized commercially insured children with ≥1 complex chronic condition from birth to 18 years of age in the Truven MarketScan database. Cohort eligibility criteria were hospital discharge between January 2013 and November 2016 and at least 30 days of follow-up after discharge. Two primary outcome measures were used: receipt of any home nursing within 30 days of hospital discharge (yes or no) and number of days of posthospitalization home nursing (1–30 days). A composite metric encompassing both receipt and quantity was created by evaluating the 95th percentile of days of home nursing (0–30 days).
RESULTS:
Overall, 9.9% of the sample received home nursing. After we adjusted for patient characteristics, the probability of receiving home nursing varied across states, ranging from 3.4% to 19.2%. Among home nursing recipients, the adjusted median home nursing days across states ranged from 6.6 to 24.5 days. The adjusted 95th percentile of days of home nursing (across the entire of sample, including recipients and nonrecipients of home nursing) ranged from 6.8 to 22.6 days.
CONCLUSIONS:
We observed striking state-to-state variability in receipt of home nursing and mean number of days of posthospitalization home nursing among commercially insured CMC after adjustment for demographic and clinical differences. This suggests opportunities for state-level improvement.
Between 1% and 6% of children are characterized as having medical complexity, defined as chronic conditions, medical fragility, and substantial functional limitation.1–4 This subset of children accounts for 33% to 50% of all pediatric health care costs, in part because of prolonged hospitalizations.1–3,5,6 Home nursing shortages have been implicated as a primary driver of prolonged length of hospital stays among children with medical complexity (CMC).7–15 Moreover, inadequate home nursing has been associated with parental financial instability, social isolation, depression, and sleep loss.7,16,17
Existing estimates of posthospitalization home nursing among CMC are based on hospital discharge data (ie, discharge disposition to home nursing or indication in the hospital chart that home nursing was anticipated) rather than on actual use.3,18,19 In these studies, researchers have evaluated home nursing in terms of the proportion of children anticipated to receive posthospitalization home nursing services, but because of the limitations of hospital chart data, they have not evaluated the quantity of services distributed.
Our objective for this analysis was to establish more precise, specific measures of posthospitalization home nursing on the basis of charges for posthospital home nursing and to quantify days of home nursing delivered among a population of commercially insured CMC. Approximately 30% of CMC have only commercial insurance.20,21 Informed by literature suggesting regional factors may influence distribution of home nursing,19,22 we hypothesized that after accounting for patient and hospitalization characteristics, there would be significant state-to-state variability in the provision of posthospitalization home nursing to medically complex, commercially insured children.
Methods
In this study, we used deidentified administrative data, which does not meet the definition of human subjects’ research and, by policy, did not require Children’s Hospital of Philadelphia Institutional Review Board review.
Study Design and Setting
This study was a retrospective cohort analysis of receipt of posthospitalization home nursing by using claims data from the Truven MarketScan commercial insurance data set (2013–2016) (Truven Health Analytics, New York, NY). The data set includes claims paid by commercial insurance; among duel-eligible children, claims paid by public or secondary insurers are not included. Analyses were conducted in Stata version 14.2 (Stata Corp, College Station, TX).
Study Population
The sample included 126 352 medical and/or surgical hospitalizations by
88
352 medical and/or surgical hospitalizations by
88 139 unique commercially insured children aged 0 to 18 years with at
least 1 complex chronic condition (CCC)23 and at least 30 days of outpatient follow-up
information (no readmission, death, or change of insurance within 30 days of
discharge). A total of 2300 hospitalizations for which no state of residence was
specified were excluded. One hospitalization was randomly selected for each
individual. All 50 US states, the District of Columbia, and Puerto Rico were
represented; however Hawaii and Puerto Rico had <20 cases and were excluded
from analysis.
139 unique commercially insured children aged 0 to 18 years with at
least 1 complex chronic condition (CCC)23 and at least 30 days of outpatient follow-up
information (no readmission, death, or change of insurance within 30 days of
discharge). A total of 2300 hospitalizations for which no state of residence was
specified were excluded. One hospitalization was randomly selected for each
individual. All 50 US states, the District of Columbia, and Puerto Rico were
represented; however Hawaii and Puerto Rico had <20 cases and were excluded
from analysis.
Patient Demographic, Clinical, and Hospitalization Characteristics
The primary exposure of interest was state of residence. Patient characteristics included age, sex, type(s) of CCC(s), and number of CCCs (Table 1). Hospitalization characteristics included type (surgical or medical), length of stay (LOS), and year (Table 1).
TABLE 1
Sample Characteristics and Adjusted Odds Ratios of Receiving Posthospitalization Home Nursing
Overall (N =
88 139) 139) | No Home Nursing (n =
79 413) 413) | Home Nursing (n = 8726) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|
| Age, y | |||||
 <2 <2 | 19 663 663 | 16 843 (21.2%) 843 (21.2%) | 2820 (32.3%) | Reference | Reference |
 2–5 2–5 | 14 043 043 | 12 681 (16.0%) 681 (16.0%) | 1362 (15.6%) | 0.64 (0.60 to 0.69) | 0.63 (0.59 to 0.68) |
 6–11 6–11 | 17 481 481 | 15 834 (19.9%) 834 (19.9%) | 1647 (18.9%) | 0.62 (0.58 to 0.66) | 0.64 (0.60 to 0.69) |
 12–15 12–15 | 18 762 762 | 17 237 (21.7%) 237 (21.7%) | 1525 (17.5%) | 0.53 (0.49 to 0.56) | 0.60 (0.56 to 0.65) |
 16–18 16–18 | 18 190 190 | 16 818 (21.2%) 818 (21.2%) | 1372 (15.7%) | 0.49 (0.46 to 0.52) | 0.55 (0.51 to 0.59) |
| Sex | |||||
 Male Male | 45 756 756 | 40 929 (51.5%) 929 (51.5%) | 4827 (55.3%) | Reference | Reference |
 Female Female | 42 383 383 | 38 484 (48.5%) 484 (48.5%) | 3899 (44.7%) | 0.86 (0.82 to 0.90) | 0.91 (0.86 to 0.95) |
| Year | |||||
 2013 2013 | 30 910 910 | 27 463 (34.6%) 463 (34.6%) | 3447 (39.5%) | Reference | Reference |
 2014 2014 | 26 897 897 | 24 180 (30.4%) 180 (30.4%) | 2717 (31.1%) | 0.90 (0.85 to 0.94) | 0.88 (0.83 to 0.93) |
 2015 2015 | 15 816 816 | 14 471 (18.2%) 471 (18.2%) | 1345 (15.4%) | 0.74 (0.69 to 0.79) | 0.75 (0.70 to 0.81) |
 2016 2016 | 14 516 516 | 13 299 (16.7%) 299 (16.7%) | 1217 (13.9%) | 0.73 (0.68 to 0.78) | 0.71 (0.66 to 0.76) |
| Hospitalization type | |||||
 Surgical Surgical | 33 709 709 | 30 711 (38.7%) 711 (38.7%) | 2998 (34.4%) | Reference | Reference |
 Medical Medical | 54 430 430 | 48 702 (61.3%) 702 (61.3%) | 5728 (65.6%) | 1.20 (1.15 to 1.26) | 1.55 (1.47 to 1.64) |
| Mean hospital days | 5.31 (SD 0.04) | 4.69 (SD 0.03) | 10.91(SD 0.21) | 1.03 per day (1.03 to 1.04) | 1.03 per day (1.02 to 1.03) |
| >1 CCC | 20 751 751 | 16 831 (21.2%) 831 (21.2%) | 3920 (44.9%) | 3.03 (2.90 to 3.17) | 1.38 (1.25 to 1.52) |
| CCC type(s) | |||||
 Cardiovasculara,b Cardiovasculara,b | 21 392 392 | 19 275 (24.3%) 275 (24.3%) | 2117 (24.3%) | 1.00 (0.95 to 1.05) | 1.18 (1.09 to 1.28) |
 Neuromusculara,b Neuromusculara,b | 20 639 639 | 18 547 (23.4%) 547 (23.4%) | 2092 (24.0%) | 1.03 (0.98 to 1.09) | 1.20 (1.10 to 1.30) |
 Congenital or geneticc Congenital or geneticc | 15 785 785 | 14 376 (18.1%) 376 (18.1%) | 1409 (16.1%) | 0.87 (0.82 to 0.92) | 1.04 (0.96 to 1.14) |
 Technology dependence Technology dependence | 15 402 402 | 12 944 (16.3%) 944 (16.3%) | 2458 (28.2%) | 2.01 (1.91 to 2.11) | 1.78 (1.67 to 1.89) |
 Gastrointestinal Gastrointestinal | 12 661 661 | 10 532 (13.3%) 532 (13.3%) | 2129 (24.4%) | 2.11 (2.00 to 2.23) | 2.10 (1.93 to 2.28) |
 Hematology or immunology Hematology or immunology | 10 194 194 | 9047 (11.4%) | 1147 (13.1%) | 1.18 (1.10 to 1.26) | 1.31 (1.19 to 1.44) |
 Malignancy Malignancy | 9312 | 7566 (9.5%) | 1746 (20.0%) | 2.38 (2.24 to 2.52) | 3.34 (3.05 to 3.66) |
 Metabolica,b Metabolica,b | 8728 | 7865 (9.9%) | 863 (9.9%) | 1.00 (0.93 to 1.08) | 1.18 (1.07 to 1.31) |
 Renal Renal | 6773 | 6149 (7.7%) | 624 (7.2%) | 0.92 (0.84 to 1.00) | 1.12 (1.01 to 1.25) |
 Respiratory Respiratory | 6204 | 4667 (5.9%) | 1537 (17.6%) | 3.42 (3.22 to 3.65) | 2.80 (2.55 to 3.06) |
 Neonatal Neonatal | 2329 | 1785 (2.2%) | 544 (6.2%) | 2.89 (2.62 to 3.19) | 1.54 (1.35 to 1.75) |
 Transplant Transplant | 1906 | 1536 (1.9%) | 370 (4.2%) | 2.25 (2.00 to 2.52) | 1.62 (1.41 to 1.85) |
For state of residence, see Supplemental Table 3. OR, odds ratio.
Outcome Measures
The proportion of children receiving posthospitalization home nursing and the quantity of home nursing distributed were evaluated. The proportion of children receiving home nursing was determined by using a binary outcome (yes or no) indicating ≥1 charge for home nursing within 30 days of hospital discharge. The probability of receipt of home nursing was determined for each state. Quantity of home nursing was evaluated on the basis of the number of days of home nursing (1–30 days) among home nursing recipients. The median (50th percentile) days of home nursing (among recipients) in each state was used to assess quantity of home nursing.
State Rankings
The distribution of days of home nursing (0–30) by state among all children in the sample was used to derive a composite metric encompassing both the proportion of children receiving home nursing (ie, children who received 0 days of home nursing versus those who received >0 days of home nursing) and the quantity of home nursing days delivered. Graphic plots for each percentile (1–99) displayed the days of home nursing (on the x-axis) for each state (on the y-axis) at a given percentile. Graphic analysis was verified computationally by applying Simpson’s diversity index,24 which measures the number of different subtypes within a sample, at each percentile (1–99) to identify the percentile with maximal diversity between states in terms of days of home nursing. The percentile with maximal diversity was selected as a point of state-to-state comparison encompassing a measure of both proportion and quantity.
Data Analysis
Bivariable analysis by using χ2 tests was used to examine the relationship between hospital and patient characteristics (including state of residence) and receipt of home nursing. Logistic regression models that included indicator variables for each state were fit for receipt of home nursing. Virginia served as a reference because Virginia was near the average in terms of both size and unadjusted proportion receiving home nursing. Models included patient and hospital characteristics associated with receipt of home nursing in bivariable analyses (P < .20). The likelihood ratio, Akaike information criterion, and Bayesian information criterion were used to assess model fit.
The distribution of home nursing days among patients who received home nursing was severely skewed, with the mean duration of home nursing frequently exceeding the median (Supplemental Table 3). Quantile regression was performed to evaluate factors that influenced the number of days of home nursing among those who received home nursing. Quantile regression is used to model the relationship between predictors and an outcome at a specific percentile. Median quantile regression was performed to specify the impact of the state on the 50th percentile of home nursing days among recipients. Quantile regression was performed at the 95th percentile of home nursing days among all children in the sample to rank states’ home nursing performance.
After logistic and quantile regression, marginal effects were calculated for each state at the mean value of other predictor variables in the model by using the Stata margins postestimation command. In the margins command, the δ method is used to obtain SEs, on which the 95% confidence intervals (CIs) for the estimated probabilities (marginal effects) are based. Adjusted estimates of the percentage of children receiving home nursing, the median number of days of home nursing among recipients, and the 95th percentile days of home nursing among all children in the sample were computed for each state.
Results
A total of 88 139 unique patient hospitalizations were analyzed (Table 1). The mean age was 8.7 years (95% CI:
8.7 to 8.8), with a fairly uniform distribution across age categories. The mean
length of hospitalization was 5.3 days (95% CI: 5.2 to 5.4). Patients had a mean of
1.3 CCCs (95% CI: 1.29 to 1.30). The most common CCCs were neuromuscular disorders
(23.4%) and cardiovascular disorders (24.3%). Posthospitalization home nursing was
provided after 8726 (9.9%) admissions.
139 unique patient hospitalizations were analyzed (Table 1). The mean age was 8.7 years (95% CI:
8.7 to 8.8), with a fairly uniform distribution across age categories. The mean
length of hospitalization was 5.3 days (95% CI: 5.2 to 5.4). Patients had a mean of
1.3 CCCs (95% CI: 1.29 to 1.30). The most common CCCs were neuromuscular disorders
(23.4%) and cardiovascular disorders (24.3%). Posthospitalization home nursing was
provided after 8726 (9.9%) admissions.
In the unadjusted bivariate analysis (Table 1) receipt of home nursing was associated with patient age, patient sex, year, admission type (surgical versus medical), each additional hospital day, having >1 CCC, and most CCC types (P < .001). In the multivariable adjusted analysis (Table 1), the same associations were identified. The addition of state of residence improved model fit significantly (likelihood ratio test, P < .001). Across states with an adequate sample size, the average adjusted marginal probability of receiving any posthospital home nursing across the states of residence ranged from 3.4% to 19.2% (Fig 1, Supplemental Table 3).

Adjusted marginal probability of receiving posthospitalization home nursing by state (among states with at least 20 observations). The widths of the 95% CIs are largely due to the sample size in each state, with smaller states having wider CIs.
Regarding the quantity of home nursing days delivered to the 8726 recipients of home nursing, the overall mean days of home nursing delivered was 15.4 days (95% CI: 15.2 to 15.6) per child. Age, year, having >1 CCC, LOS, and state of residence were included in a quantile regression model of median days of home nursing among home nursing recipients. On the basis of marginal effects at the mean value of other predictor variables, the adjusted median predicted days of home nursing (across the 42 states with >20 observations with home nursing) ranged from 6.6 to 24.5 days (Fig 2, Supplemental Table 4).

Adjusted predicted median number of days of home nursing among recipients by state (among states with at least 20 observations). The widths of the 95% CIs are largely due to the sample size in each state, with smaller states having wider CIs. Values for the adjusted 95% CIs <0 have been truncated.
Some common combinations of ages and conditions were selected to illustrate the degree of difference between states regarding receipt of any home nursing and the quantity of home nursing days (Table 2). Within those categories, the (unadjusted) proportion of patients receiving any home nursing and, among patients who did receive home nursing, the median number of days received in the 30 days after hospital discharge were identified. For instance, in the fifth highest state (among states with >20 observations), 41.0% of children aged 0 to 2 years with technology dependence received home nursing, in contrast to 16.8% of similar children in the fifth lowest state. In this population, the median days of home nursing among recipients in the fifth lowest state was 7 days, compared with 25 days in the fifth highest state. There was a 2.5-fold difference in the proportion of children aged 16 to 19 with malignancies who receive home nursing between the fifth highest and the fifth lowest states.
TABLE 2
Illustrative Examples of Differences in the Distribution of Posthospitalization Home Nursing Across States (Among States With >20 Cases)
| Age, y | CCC Type | n | Proportion Receiving Home Nursing, % | Median No. Days of Home Nursing (Among Recipients) | ||
|---|---|---|---|---|---|---|
| Fifth Lowest State | Fifth Highest State | Fifth Lowest State | Fifth Highest State | |||
| 0–2 | Technology dependence | 2878 | 16.8 | 41.0 | 8 | 25 |
| 2–5 | Respiratory | 930 | 14.3 | 26.1 | 14.5 | 21 |
| 6–11 | Neuromuscular | 5523 | 3.6 | 16.9 | 8.5 | 29 |
| 12–15 | Gastrointestinal | 2718 | 7.7 | 19.1 | 8 | 28 |
| 16–19 | Malignancy | 1970 | 8.7 | 22.0 | 7.5 | 24.5 |
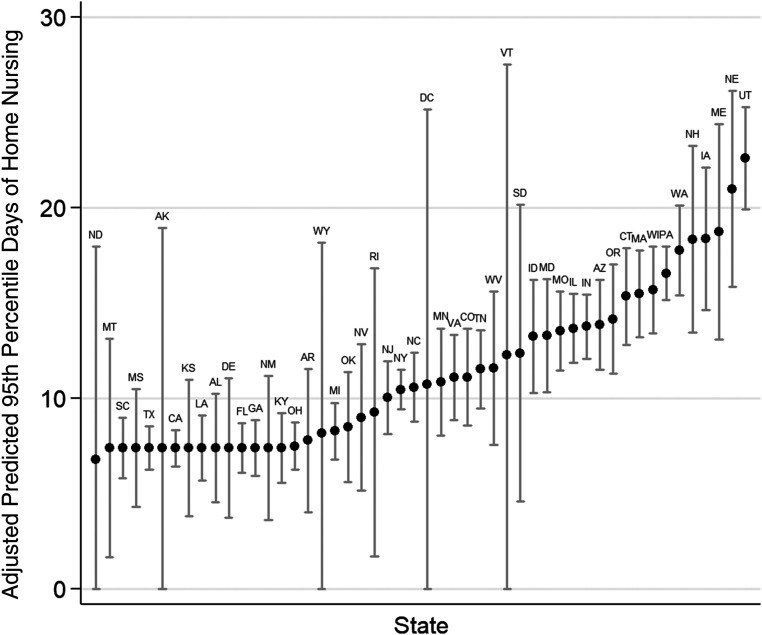
Quantile regression provided a single framework for examining state-level variation in both receipt of any home nursing and the quantity of days of home nursing distributed. In our sample, the 95th percentile of observed number of days of home nursing (range: 0–30 days) exhibited the maximal diversity between states. Although the 95th percentile of days of home nursing across the entire sample was 14 days, the 95th percentile for some states was 0 days, and for other states, it was 30 days, with other states at points between. Therefore the 95th percentile was selected as the maximal diversity point of comparison across states, encompassing both home nursing receipt and quantity. Age, year, having >1 CCC, LOS, and state of residence were included in a quantile regression model of the 95th percentile of home nursing days across the entire sample. On the basis of marginal effects at the mean value of other predictor variables, the adjusted 95th percentile predicted days of home nursing ranging from 6.8 to 22.6 days (Fig 3, Supplemental Table 5).
Discussion
After accounting for clinical and hospitalization characteristics, we found that significant state-to-state variability exists in the proportion and quantity of posthospitalization home nursing received by commercially insured CMC in this large national cohort. There is more than a fivefold difference in the adjusted marginal probability of receiving home nursing between states. Ranking of the 95th percentile of home nursing days allows for a reproducible assessment of both probability and quantity of home nursing delivery.
Our results are consistent with those of previous studies. Our unadjusted national receipt of posthospitalization home nursing (~10%) is concordant with estimates from a single-center chart audit study which identified an overall home nursing receipt of 7.5% (25% in children who were technology dependent).18 Similarly, an analysis of the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Kids’ Inpatient Database revealed that 7.6% of children with at least 1 CCC had a hospital discharge disposition code indicating discharge to home nursing, with wide state variability.19 Both studies included patients of all insurance statuses (Medicaid, private, uninsured, and dual coverage).
These findings should be interpreted in light of the study’s strengths and limitations. Strengths include an updated national perspective on home nursing services based on actual claims from a well-curated data source. Whereas in previous work rates of home nursing receipt have been discussed, using claims data allowed us to examine the quantity of home nursing delivered.
This is a study of commercially insured children, who make up ~30% of all CMC.20,21 A majority of children who receive home nursing are state Medicaid waiver beneficiaries. Children with commercial or private insurance may have lower odds of receiving home nursing than children with public insurance19; therefore, these findings may not be generalizable to children with other types of insurance. Despite these theoretical differences, our overall estimates are in line with data from samples that included both Medicaid-insured and commercially insured patients.18,19 Interactions between state Medicaid policies (including Medicaid expansion efforts) and commercial insurance benefits have not been characterized.
The identifier for home nursing used in this analysis does not differentiate between skilled nursing visits and private-duty nursing shifts. Skilled nursing visits (for tasks such as wound care, medication administration, or line care) last on the order of minutes to hours, whereas private-duty nursing shifts provide hours up to a full day of patient care. Across states, we cannot determine if fewer days of home nursing was offset by more hours per day. Although there are, to our knowledge, no data to suggest that such a trade-off is occurring, this possibility should be examined in future work.
Analysis was limited by the availability of patient and clinical information within this administrative data set. The data set does not include information about whether families self-paid for additional home care services. The desired or optimal number of days of home nursing could not be ascertained in this administrative data set. Race, ethnicity, or family socioeconomic factors are not included in the data set, precluding analysis of these potentially important sources of disparity. No information about hospital or facility or clinician was available.
Keeping the study’s strengths and limitations in mind, we identified 5 aspects of these findings that warrant discussion. First, to a limited degree, clinical and demographic factors influence the distribution of posthospitalization home nursing to commercially insured CMC, all in accordance with previously identified associations. Younger children with multiple CCCs and longer, more costly hospital stays were most likely to receive home nursing.19,25 Families rely on home nursing to safely care for these children who are medically fragile. For some, hospital discharge may be contingent on securing appropriate home nursing care.7 Yet despite evidence of the need for home nursing, no standards exist to guide distribution, and thus there remain disparities in who receives home nursing and how much home nursing they receive.
Second, pediatric posthospitalization home nursing is infrequent. Even in this sample of CMC with commercial insurance, the proportion of children receiving home nursing was far smaller than the estimated 29.2% of older adult Medicare beneficiaries who are referred to posthospital home health care.26 A dearth of trained pediatric home nurses with skills in providing care to children who are technology dependent, wide variation in state coverage programs for children, and the ability to rely on informal labor provided by family caregivers are potential contributors to the relative paucity of pediatric home nursing.22 Although the optimal rate of home nursing distribution is not known, this difference suggests that there may be opportunity to provide more support for families of CMC.
Third, the substantial variation across states, both in terms of providing any home nursing and the amount of home nursing distributed, raises the question of why. Proposed drivers of these differences include regional differences in referral patterns, the availability of home nursing services, scope-of-practice regulation differences in who is eligible to provide home nursing, payer coverage of services, home nurse wage rates, and the accessibility of inpatient rehabilitation and skilled nursing facilities (which are alternatives to home health care).22,26
Fourth, there are observed differences in state distribution, as measured by proportion versus by quantity; in some states, home nursing is more common, but the median days of home nursing is lower and vice versa. It is possible that because we do not distinguish between episodic-visiting nursing and long-term private-duty nursing, state variation may in part reflect differences in the balance between these 2 types of services. Nonetheless, in light of the well-documented shortages and state-level differences in licensure and reimbursement,22 it is important to consider whether CMC who qualify for and seek posthospital home nursing are receiving adequate coverage or whether these differences reflect gaps in home nursing shifts that are difficult to fill. Ultimately, adequacy of home nursing distribution is measured both by the proportion and quantity of home nursing delivered, which is why a combined metric is important.
Fifth, although this is a study of commercially insured CMC, these state-level differences suggest opportunities for policy and programmatic approaches to increase access to home nursing services beyond expansion of Medicaid. In adults, a county-level analysis of home health agencies revealed that in addition to sociodemographic factors, there was an association between increased number of agencies and increased home nursing reimbursement rates.27 Although the same association has not been explored in pediatrics, there are known regional disparities in both availability of qualified pediatric home nurses7,19,22 and Medicaid reimbursement rates for home nursing.28–30
In future work, researchers should evaluate potential drivers of the observed variation among states and over time regarding the provision of home nursing, including more direct regulatory and market-based mechanisms and, potentially, more complex policy mechanisms. For example, the relative size of the home nursing labor supply in any given state may be directly due to the restrictiveness of that state’s scope-of-practice regulations or due to the local prevailing differential of wages between home and hospital nursing.22 At the level of policy, levels of home nursing among commercially insured children might be driven by Medicaid policies but, potentially, in divergent directions. On the one hand, more expansive Medicaid coverage policies regarding home nursing might increase the pool of available home nurses in an area, allowing for improved access to home nursing among both Medicaid-insured and commercially insured children. On the other hand, in states with more expansive Medicaid programs, because children would be more likely to have Medicaid coverage, commercial insurance plans might be more restrictive regarding the provision of home nursing. All of these factors and others that could potentially influence the receipt of home nursing could be examined by using our reproducible state-level comparison methodology.
Conclusions
By quantifying and rank-ordering state performance, we hope to motivate and inform efforts to ensure appropriate access to home nursing. The degree of variability in home nursing delivery, after adjustment for clinical and demographic factors, suggests that state-level factors may contribute to delivery of home nursing and that there may be opportunities for improvement in access to this vital service.
Glossary
| CCC | complex chronic condition |
| CI | confidence interval |
| CMC | children with medical complexity |
| LOS | length of stay |
Footnotes
Dr Rasooly conducted the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Drs Shults, Guevara, and Feudtner reviewed the analyses and critically reviewed the manuscript for important intellectual content; and all authors conceptualized and designed the study, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Rasooly was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (award T32HD060550). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-0791.
References
Full text links
Read article at publisher's site: https://doi.org/10.1542/peds.2019-2465
Read article for free, from open access legal sources, via Unpaywall:
https://pediatrics.aappublications.org/content/pediatrics/146/2/e20192465.full.pdf
Citations & impact
Impact metrics
Article citations
Bridging the gaps in pediatric complex healthcare: the case for home nursing care among children with medical complexity.
BMC Health Serv Res, 24(1):814, 15 Jul 2024
Cited by: 0 articles | PMID: 39010079 | PMCID: PMC11251302
Sociodemographic disparities and healthcare utilization in pediatric obstructive sleep apnea management.
Sleep Med, 109:211-218, 13 Jul 2023
Cited by: 0 articles | PMID: 37478657 | PMCID: PMC10528094
Home Health Care Utilization in Children With Medicaid.
Pediatrics, 149(2):e2021050534, 01 Feb 2022
Cited by: 1 article | PMID: 35028664 | PMCID: PMC9003864
Allocation of Pediatric Home Care Nursing Hours: The Minnesota Experience.
Home Healthc Now, 40(1):27-39, 01 Jan 2022
Cited by: 0 articles | PMID: 34994718 | PMCID: PMC8740033
Qualitative indications for tracheostomy and chronic mechanical ventilation in patients with severe bronchopulmonary dysplasia.
J Perinatol, 41(11):2651-2657, 04 Aug 2021
Cited by: 10 articles | PMID: 34349231 | PMCID: PMC8331995
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Pediatric Hospital Discharges to Home Health and Postacute Facility Care: A National Study.
JAMA Pediatr, 170(4):326-333, 01 Apr 2016
Cited by: 34 articles | PMID: 26902773
A national and state profile of leading health problems and health care quality for US children: key insurance disparities and across-state variations.
Acad Pediatr, 11(3 suppl):S22-33, 01 May 2011
Cited by: 79 articles | PMID: 21570014
Skilled Nursing Facility Patients Discharged to Home Health Agency Services Spend More Days at Home.
J Am Geriatr Soc, 68(7):1573-1578, 15 Apr 2020
Cited by: 8 articles | PMID: 32294239 | PMCID: PMC7363542
Health care for children and youth in the United States: 2001 annual report on access, utilization, quality, and expenditures.
Ambul Pediatr, 2(6):419-437, 01 Nov 2002
Cited by: 52 articles | PMID: 12437388
 a,b
a,b