Abstract
Aims and objectives
To determine the health-related quality of life (HRQoL) of COVID-19 patients after discharge and its predicting factors.Background
COVID-19 has caused a worldwide pandemic and led a huge impact on the health of human and daily life. It has been demonstrated that physical and psychological conditions of hospitalised COVID-19 patients are impaired, but the studies focus on physical and psychological conditions of COVID-19 patients after discharge from hospital are rare.Design
A multicentre follow-up study.Methods
This was a multicentre follow-up study of COVID-19 patients who had discharged from six designated hospitals. Physical symptoms and HRQoL were surveyed at first follow-up (the third month after discharge). The latest multiple laboratory findings were collected through medical examination records. This study was performed and reported in accordance with STROBE checklist.Results
Three hundred eleven patients (57.6%) were reported with one or more physical symptoms. The scores of HRQoL of COVID-19 patients at third month after discharge, except for the dimension of general health, were significantly lower than Chinese population norm (p < .001). Results of logistic regression showed that female (odds ratio (OR): 1.79, 95% confidence interval (CI): 1.04-3.06), older age (≥60 years) (OR: 2.44, 95% CI: 1.33-4.47) and the physical symptom after discharge (OR: 40.15, 95% CI: 9.68-166.49) were risk factors for poor physical component summary; the physical symptom after discharge (OR: 6.68, 95% CI: 4.21-10.59) was a risk factor for poor mental component summary.Conclusions
Health-related quality of life of discharged COVID-19 patients did not come back to normal at third month after discharge and affected by age, sex and the physical symptom after discharge.Relevance to clinical practice
Healthcare workers should pay more attention to the physical and psychological rehabilitation of discharged COVID-19 patients. Long-term follow-up on COVID-19 patients after discharge is needed to determine the long-term impact of COVID-19.Free full text
Health‐related quality of life of COVID‐19 patients after discharge: A multicenter follow‐up study
Abstract
Aims and Objectives
To determine the health‐related quality of life (HRQoL) of COVID‐19 patients after discharge and its predicting factors.
Background
COVID‐19 has caused a worldwide pandemic and led a huge impact on the health of human and daily life. It has been demonstrated that physical and psychological conditions of hospitalised COVID‐19 patients are impaired, but the studies focus on physical and psychological conditions of COVID‐19 patients after discharge from hospital are rare.
Design
A multicentre follow‐up study.
Methods
This was a multicentre follow‐up study of COVID‐19 patients who had discharged from six designated hospitals. Physical symptoms and HRQoL were surveyed at first follow‐up (the third month after discharge). The latest multiple laboratory findings were collected through medical examination records. This study was performed and reported in accordance with STROBE checklist.
Results
Three hundred eleven patients (57.6%) were reported with one or more physical symptoms. The scores of HRQoL of COVID‐19 patients at third month after discharge, except for the dimension of general health, were significantly lower than Chinese population norm (p < .001). Results of logistic regression showed that female (odds ratio (OR): 1.79, 95% confidence interval (CI): 1.04–3.06), older age (≥60 years) (OR: 2.44, 95% CI: 1.33–4.47) and the physical symptom after discharge (OR: 40.15, 95% CI: 9.68–166.49) were risk factors for poor physical component summary; the physical symptom after discharge (OR: 6.68, 95% CI: 4.21–10.59) was a risk factor for poor mental component summary.
Conclusions
Health‐related quality of life of discharged COVID‐19 patients did not come back to normal at third month after discharge and affected by age, sex and the physical symptom after discharge.
Relevance to clinical practice
Healthcare workers should pay more attention to the physical and psychological rehabilitation of discharged COVID‐19 patients. Long‐term follow‐up on COVID‐19 patients after discharge is needed to determine the long‐term impact of COVID‐19.
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is a novel pneumonia infection with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), a member of the betacoronavirus genus. The main clinical characteristics of COVID‐19 are fever, cough and shortness of breath (Chen, Zhou, et al., 2020), and a proportion of patients may accompany with new loss of taste or smell (Dawson et al., 2020), diarrhoea, nausea, vomiting and other symptoms (Chen, Zhou, et al., 2020; Kim et al., 2020; Tian et al., 2020). Currently, COVID‐19 has caused a worldwide pandemic and led a huge impact on the health of human and daily life. To date, there are more than twenty million confirmed cases and seven hundred thousand cases died with COVID‐19 infection worldwide according to the reports of World Health Organization (WHO) (World Health Organization, 2020).
Previous studies have revealed some positive laboratory findings and reactivated clinical features of discharged COVID‐19 patients (Zheng et al., 2020). As reviewed by Zheng and colleagues (Zheng et al., 2020), approximately 3.2% to 9.1% of discharged patients may experience SARS‐COV‐2 reactivation but without specific clinical features to distinguish them. Some clinical symptoms including fever, cough, sore throat and fatigue were also observed among discharged patients with SARS‐COV‐2 reactivation (Ye et al., 2020; Zheng et al., 2020). In addition, due to incomplete recovery of pulmonary injury, present palpitation, shortness of breath or dyspnoea may still occur after physical activity for discharged patients (Zheng et al., 2020). Another concern is that considering the impact of coronavirus infection on the daily life and work, a considerable number of COVID‐19 patients may still have psychological problems after discharge from hospital (Yuan et al., 2020). Therefore, all mentioned above suggests that the physical and mental functions of some discharged patients do not come back to normal and at the risk of deterioration.
2. BACKGROUND
Health‐related quality of life (HRQoL) has aroused much interest in the social progress and the transformation of medical care and service systems, which refers to the impact of disease and treatment on patients' function and overall life satisfaction (Gill & Feinstein, 1994; Schipper et al., 1996). Similar to other diseases, it has been demonstrated in several studies that COVID‐19 can affect HRQoL of patients and general populations (Nguyen et al., 2020; Zhang & Ma, 2020). Physical symptoms are still observed among COVID‐19 patients after discharged from hospital (Carfì et al., 2020), which may also affect their normal life and lead to poor HRQoL. However, only few studies have reported HRQoL of patients after discharge. One previous cross‐sectional study has revealed that HRQoL was poor among COVID‐19 patients at the first‐month follow‐up and several risk factors are determined (Chen et al., 2020). Garrigues et al., (2020) have found that there are few differences for HRQoL between ward and ICU COVID‐19 patients after discharge.
Considering studies reporting physical and psychological conditions of COVID‐19 patients after discharge from hospital are rare, this multicentre study was performed to investigate the physical condition and HRQoL of COVID‐19 patients after discharge. Meanwhile, factors associated with poor health‐related quality of life were also explored.
3. METHODS
3.1. Study design and participants
This study was performed and reported in accordance with Strengthening the Reporting of Observational Studies in Epidemiology guideline for cohort studies (Supplementary File 1). This was a multicentre follow‐up study of COVID‐19 patients who had been discharged from designated hospitals in Anhui Province and Hubei Province. Six designated hospitals in Anhui Province and Hubei Province for the treatment of COVID‐19 were selected to recruit discharged patients with COVID‐19 infection. The inclusion criteria of participants were as follows: (1) the patients were definitely diagnosed with SARS‐CoV‐2 infection on hospital admission (the diagnosis of SARS‐CoV‐2 infection was based on guideline for the diagnosis and treatment of 2019 novel coronavirus (2019‐nCoV) infected pneumonia of Chinese: positive for the 2019‐nCoV by the real‐time PCR test for nucleic acid in respiratory or blood samples); (2) hospitalisation for the following reasons: fever (axillary temperature was 36.7°C and above, or oral temperature was 38.0°C and above, or anal temperature or ear temperature was 38.6°C and above) and respiratory rate was more than 24 times/min or cough (at least one of shortness of breath and cough); (3) the clinical type of COVID‐19 at hospital admission was mild to severe according to the Chinese management guideline for COVID‐19 (Sixth edition); and (4) participants were required to meet the standard hospital discharge criteria (no fever for at least 3 days; substantial resolution of pneumonia with a CT scan, two negative SARS‐CoV‐2 RT‐qPCR tests done at least 1 day apart on nasopharyngeal and oropharyngeal swabs, and no concurrent acute medical issues requiring transfer to another medical facility). The exclusion criteria of participants were as follows: (1) confirmed hepatitis B, C, AIDS and other viral infections; (2) women who were in pregnancy (positive pregnancy test for women of childbearing age); (3) subjects with other unsuitable factors considered by the researchers; and (4) discharged patients were unwilling to participate in this study.
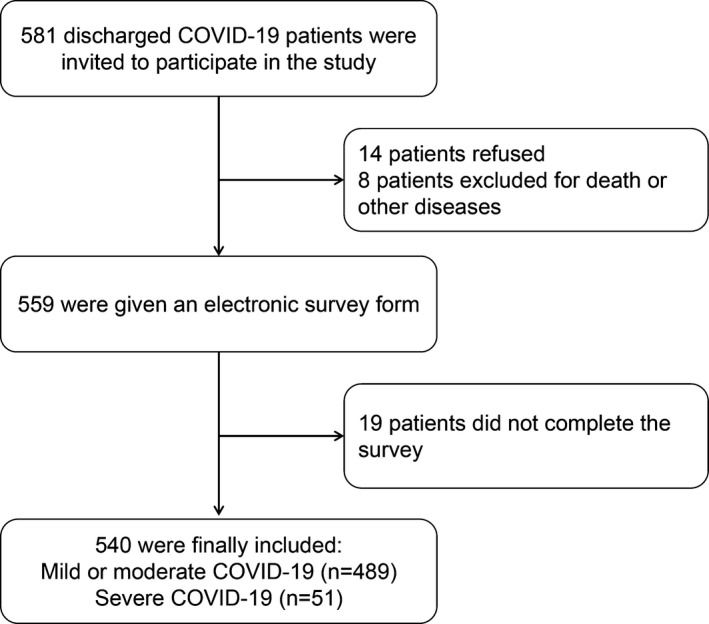
Five hundred eighty one discharged patients (including 511 mild or moderate COVID‐19 patients and 70 severe COVID‐19 patients) were invited to participate in this study and would be first informed of the purpose and benefits of this study through telephone, and after obtaining the patients' verbal consent, an electronic survey form would be given to patients to collect interest data. For younger participants (aged less than 18), the survey was conducted in the company of parents and with the consent of parents and children. Finally, a total of 540 discharged patients were included in our study (Figure (Figure1).1). All included patients had been discharged between 1 February 2020–8 March 2020 (the latest patient was discharged from hospitals). The study was started on 5 May 2020 and ended on 8 June 2020. This study was approved by the Research Ethics Commission of the First Affiliated Hospital of Anhui Medical University (PJ‐2020–03–19). Written informed consent was waived by the Ethics Commission for emerging infectious diseases.
3.2. Data collection
Data were collected at the first follow‐up hospital appointment following discharge which is routinely offered to patients at 3 months. An electronic survey form was administered to discharged COVID‐19 patients to collect the information of physical symptoms and HRQoL. Physical symptoms were self‐reported by patients. According to the discharge regulations of COVID‐19, patients should undergo routine examination after discharge in community hospitals or grade A hospitals with inspection qualifications. Results of multiple laboratory examination were collected through medical examination records. Times from hospital discharge to laboratory examination were recorded. In our study, the collected medical laboratory examination results include SARS‐CoV‐2 RNA detection (positive or negative), blood routine examination (white blood cell count, haemoglobin, platelet, C‐reactive protein, neutrophil‐to‐lymphocyte ratio), and renal and liver function (aspartate aminotransferase, alanine aminotransferase, total bilirubin, blood urea nitrogen, serum creatinine). All data were collected by the physicians who managed and took the most care of COVID‐19 patients and checked by the third researchers. There were no missing data collected in our study.
3.3. Health‐related quality of life
Health‐related quality of life was assessed using the scale of MOS 36‐item Short‐Form Health Survey (SF‐36). SF‐36 is a generic widely validated scale to measure HRQoL of inpatient or discharged patients which include eight health concepts (Brazier et al., 1992): physical function (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social function (SF), role emotion (RE) and mental health (MH). The assessed scores of each concept were ranged from 0–100, and higher scores represent better quality. In addition, eight health concepts of SF‐36 can be classified into two categories: physical component summary (PCS) and mental component summary (MCS), and the poor HRQoL was defined as scores of PCS or MCS less than 50 (Chen, Li, et al., 2020). In our study, the overall Cronbach's alpha of this scale was 0.547. The Chinese population norm (Rui et al., 2011) was used as the comparison to determine whether the HRQoL of COVID‐19 patients after discharge was poorer than general population.
3.4. Statistical analyses
Continuous variables were described as median and interquartile range (IQR) or mean and standard deviation (SD). Count variables were presented as number and percentage. The HRQoL scores were compared between two groups using t tests, and Cohen's d effect size was calculated. The magnitudes of absolute Cohen's d effect size was classified into four categories: negligible (<0.2), small (0.2–0.49), moderate (0.5–0.79) and large (>0.79) (Cohen, 1988). The chi‐squared tests or Fisher's exact tests were used to compare the difference in categorical variables. Furthermore, univariate and multivariate logistic regressions were conducted to explore the factors associated with poor HRQoL. All variables that were significant (p < .05) in univariate logistic regression models would be included in multivariate logistic regression models. All statistical analyses were performed using SPSS software, version 23.0, and significance was set at p < .05 (two‐sided).
4. RESULTS
4.1. Characteristics of patients
Demographic characteristics of patients and physical symptoms are presented in Table Table1.1. Of the 540 discharged COVID‐19 patients who had participated in this study, 489 patients were diagnosed with mild or moderate COVID‐19, and 51 patients were diagnosed severe COVID‐19 patients. The median age of all discharged patients was 47.50 years (IQR: 37.00–57.00), and male patients accounted for 50.0%, and the sex ratio of our study samples was similar to Chinese general population, but the proportion of patients for the age group 40–99 years was higher than the general Chinese population (Table (Table1).1). In total, 311 patients (57.6%) were reported with one or more uncomfortable physical symptoms. Fatigue (29.4%) was the most common symptom reported by discharged COVID‐19 patients, followed by shortness of breath after light physical activity (26.1%) and joint pain (24.3%). In addition, 32 patients (5.9%) presented with SARS‐COV‐2 reactivation, mainly within 1–2 weeks after discharge from the hospital (timeline of 32 patients with SARS‐COV‐2 reactivation is presented in Figure S1).
TABLE 1
Characteristics of discharged COVID‐19 patients and the Chinese general population
| Variables | Number | Percentage (%) | Chinese general population (%) a |
|---|---|---|---|
| Sex | |||
| Male | 270 | 50.0 | 51.1 |
| Female | 270 | 50.0 | 48.9 |
| Age (years) | |||
| 10–19 | 8 | 1.5 | 11.9 |
| 20–39 | 166 | 30.7 | 33.1 |
| 40–59 | 257 | 47.6 | 34.8 |
| 60–79 | 105 | 19.4 | 17.8 |
| 80–99 | 4 | 0.7 | 2.4 |
| Severity of COVID−19 | |||
| Mild or moderate | 489 | 90.6 | NA |
| Severe | 51 | 9.4 | NA |
| Physical symptoms | |||
| Fatigue | 159 | 29.4 | NA |
| Cough | 63 | 11.7 | NA |
| Sputum | 54 | 10.0 | NA |
| Dyspnoea | 38 | 7.0 | NA |
| Diarrhoea | 36 | 6.7 | NA |
| Shortness of breath | 141 | 26.1 | NA |
| Joint pain | 131 | 26.3 | NA |
| Dysbasia | 22 | 4.1 | NA |
| Palpitations | 110 | 20.4 | NA |
| Other symptoms | 120 | 22.2 | NA |
| Number of physical symptoms | |||
| 0 | 229 | 42.4 | NA |
| 1 | 93 | 17.2 | NA |
| 2 | 72 | 13.3 | NA |
| 3 | 48 | 8.9 | NA |
| 4 | 49 | 9.1 | NA |
| ≥5 | 49 | 9.1 | NA |
Abbreviation: NA, not applicable.
4.2. HRQoL of COVID‐19 patients after discharge
The comparison of scores HRQoL scores among different groups is presented in Table Table2.2. Compared with Chinese population norm, except for GH dimension, all scores of other dimensions of SF‐36 in COVID‐19 patients were significantly lower (p < .001) and the values of effect size showed that the discrepancy was small for BP (absolute Cohen's d: 044.), moderate for PF, RP and RE (absolute Cohen's d: 0.51 to 0.64), and large for VT (absolute Cohen's d: 0.81) and MH (absolute Cohen's d: 3.66). Severe COVID‐19 patients had lower scores of PF than mild or moderate COVID‐19 patients after discharge (p = .030), and the discrepancy was small (absolute Cohen's d: 0.40). For different sex of patients, significant difference in physical and mental health status found that except for SF, male patients had higher scores of PF, RP, GH and VT and lower scores of MH than female, and the discrepancy was small (absolute Cohen's d: 0.21 to 0.39), which meant that male had better quality of physical and mental health after discharge. We also found that patients younger than 60 years had significant higher scores of PF and GH, than those older than 60 years, and the discrepancy was small (absolute Cohen's d: 0.45 and 0.25, respectively), which indicated that older patients may have poor physical and mental health recovery status than younger patients. In addition, COVID‐19 patients without physical symptoms after discharge showed significantly higher HRQoL scores than those with physical symptoms (p < .001), and all discrepancies were moderate or large (absolute Cohen's d: 0.69 to 1.26).
TABLE 2
Comparison of HRQoL scores among discharged COVID‐19 patients with different characteristics and Chinese population norm
| PF | RP | BP | GH | VT | SF | RE | MH | PCS | MCS | |
|---|---|---|---|---|---|---|---|---|---|---|
| Participants | ||||||||||
| Patients in this study | 87.17 ± 14.57 | 66.30 ± 41.04 | 79.48 ± 20.73 | 68.90 ± 22.16 | 55.35 ± 14.58 | 66.41 ± 24.51 | 71.30 ± 38.70 | 22.86 ± 14.00 | 75.46 ± 20.45 | 53.98 ± 13.87 |
| Chinese norm | 94.02 ± 12.44 | 88.79 ± 28.49 | 88.18 ± 19.02 | 69.74 ± 20.95 | 68.92 ± 18.78 | 88.03 ± 16.00 | 89.57 ± 27.95 | 77.61 ± 15.85 | NA | NA |
| p value* | <.001 | <.001 | <.001 | .393 | <.001 | <.001 | <.001 | <.001 | NA | NA |
| Cohen's d | −0.51 | −0.64 | −0.44 | −0.04 | −0.81 | −1.04 | −0.54 | −3.66 | NA | NA |
| Severity of COVID−19 | ||||||||||
| Mild or moderate | 87.90 ± 12.89 | 66.31 ± 40.76 | 79.78 ± 20.32 | 69.03 ± 21.96 | 55.48 ± 14.26 | 66.36 ± 24.27 | 71.30 ± 39.49 | 22.87 ± 13.87 | 75.75 ± 19.86 | 54.00 ± 13.70 |
| Severe | 80.10 ± 24.69 | 66.18 ± 44.11 | 76.63 ± 24.34 | 67.71 ± 24.16 | 54.12 ± 17.46 | 66.91 ± 26.90 | 71.24 ± 41.11 | 22.74 ± 15.38 | 72.65 ± 25.52 | 53.75 ± 15.56 |
| p value* | .03 | .983 | .376 | .685 | .526 | .879 | .992 | .951 | .403 | .913 |
| Cohen's d | 0.40 | 0.003 | 0.14 | 0.06 | 0.09 | −0.02 | 0.001 | 0.01 | 0.14 | 0.02 |
| Sex of patients | ||||||||||
| Male | 89.24 ± 13.85 | 72.59 ± 38.73 | 82.99 ± 20.03 | 72.67 ± 21.09 | 56.85 ± 14.35 | 68.06 ± 23.72 | 76.05 ± 36.73 | 21.39 ± 13.30 | 79.37 ± 19.19 | 55.59 ± 13.33 |
| Female | 85.09 ± 14.99 | 60.00 ± 42.37 | 75.97 ± 20.85 | 65.13 ± 22.59 | 53.85 ± 14.67 | 64.77 ± 25.21 | 66.54 ± 40.08 | 24.33 ± 14.55 | 71.55 ± 20.96 | 52.37 ± 14.23 |
| p value* | .001 | <.001 | <.001 | <.001 | .017 | .119 | .004 | .015 | <.001 | .007 |
| Cohen's d | 0.29 | 0.31 | 0.34 | 0.35 | 0.21 | 0.13 | 0.25 | −0.21 | 0.39 | 0.23 |
| Age of patients | ||||||||||
| <60 years | 88.58 ± 13.35 | 67.40 ± 40.55 | 80.23 ± 20.67 | 69.97 ± 22.73 | 55.29 ± 14.73 | 65.66 ± 24.02 | 71.23 ± 39.08 | 22.86 ± 14.16 | 76.55 ± 20.31 | 53.76 ± 13.90 |
| ≥60 years | 81.56 ± 17.61 | 61.93 ± 42.84 | 76.50 ± 20.77 | 64.70 ± 19.24 | 55.60 ± 14.04 | 69.38 ± 26.27 | 71.56 ± 37.36 | 22.86 ± 13.42 | 71.17 ± 20.55 | 54.85 ± 13.76 |
| p value* | <.001 | .214 | .093 | .015 | .845 | .157 | .937 | .998 | .014 | .464 |
| Cohen's d | 0.45 | 0.13 | 0.18 | 0.25 | −0.02 | −0.15 | −0.01 | 0 | 0.26 | −0.08 |
| Physical symptoms | ||||||||||
| No | 94.17 ± 9.43 | 88.21 ± 26.34 | 91.76 ± 14.22 | 82.37 ± 16.03 | 63.14 ± 11.45 | 75.66 ± 22.93 | 90.54 ± 23.42 | 16.94 ± 11.59 | 89.13 ± 11.56 | 61.57 ± 9.28 |
| Yes | 82.01 ± 15.51 | 50.16 ± 42.45 | 70.44 ± 20.12 | 58.99 ± 20.79 | 49.61 ± 13.97 | 59.61 ± 23.41 | 57.13 ± 41.54 | 27.22 ± 14.04 | 65.40 ± 19.74 | 48.39 ± 14.04 |
| p value* | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| Cohen's d | 0.95 | 1.08 | 1.22 | 1.26 | 1.06 | 0.69 | 0.99 | −0.80 | 1.47 | 1.11 |
| SARS‐COV−2 reactivation | ||||||||||
| No | 87.02 ± 14.66 | 65.99 ± 41.20 | 79.30 ± 20.71 | 68.88 ± 22.23 | 55.35 ± 14.74 | 66.19 ± 24.76 | 71.00 ± 38.70 | 22.99 ± 14.08 | 75.30 ± 20.55 | 53.88 ± 14.00 |
| Yes | 89.53 ± 12.97 | 71.09 ± 38.68 | 82.34 ± 21.03 | 69.22 ± 21.32 | 55.31 ± 11.77 | 69.92 ± 20.04 | 76.04 ± 39.02 | 20.75 ± 12.71 | 78.05 ± 19.06 | 55.51 ± 11.67 |
| p value* | .344 | .496 | .421 | .934 | .987 | .404 | .475 | .380 | .462 | .521 |
| Cohen's d | −0.18 | −0.13 | −0.15 | −0.02 | 0.003 | −0.17 | −0.13 | 0.17 | −0.14 | −0.13 |
Abbreviations: BP, bodily pain; GH, general health; HRQoL, health‐related quality of life; MCS, mental component summary; MH, mental health; NA, not available; PCS, physical component summary; PF, physical function; RE, role emotion; RP, role physical; SF, social function; VT, vitality.
Bold values indicate that the comparison between groups is statistically significant.
4.3. Variables associated with HRQoL
In our study, 83 patients had poor PCS (15.4%) and 176 patients had poor MCS (32.6%). The comparison of laboratory findings among patients with different classification of HRQoL is shown in Table Table3.3. We found that patients with poor PCS only had poor haemoglobin and albumin. Several factors associated with poor PCS and MCS were identified in univariate logistic regression models (Table S1). Results of multivariate logistic regression indicated that female (odds ratio (OR): 1.79, 95% CI: 1.04–3.06, p = .035), older age (≥ 60 years) (OR: 2.44, 95% CI: 1.33–4.47, p = .004) and physical symptoms (OR: OR: 40.15, 95% CI: 9.68–166.49, p < .001) were risk factors for poor PCS; the physical symptom after discharge (OR: 6.68, 95% CI: 4.21–10.59, p < .001) was a risk factor for poor MCS (Table (Table44).
TABLE 3
Comparison of laboratory findings among different classification of HRQoL
| Laboratory findings | Poor PCS | Poor MCS | ||||
|---|---|---|---|---|---|---|
| Yes | No | p value | Yes | No | p value | |
| White blood cell count (109/L) | 5.81 ± 1.25 | 6.13 ± 1.42 | .055 | 5.94 ± 1.34 | 6.16 ± 1.43 | .091 |
| <4 | 7 (8.4%) | 19 (4.2%) | .128 | 12 (6.8%) | 14 (3.9%) | .183 |
| 4–10 | 76 (91.6%) | 428 (94.1%) | 163 (92.6%) | 341 (94.2%) | ||
| >10 | 0 (0.0%) | 8 (1.8%) | 1 (0.6%) | 7 (1.9%) | ||
| Haemoglobin (g/L) | 134.63 ± 24.39 | 140.05 ± 21.30 | .038 | 137.71 ± 20.89 | 139.91 ± 22.32 | .268 |
| <113 | 9 (10.8) | 27 (5.9) | .165 | 14 (8.0%) | 22 (6.1%) | .728 |
| 113–172 | 72 (86.7) | 423 (93.0) | 160 (90.9%) | 335 (92.5%) | ||
| >172 | 2 (2.4) | 5 (1.1) | 2 (1.1%) | 5 (1.4%) | ||
| Platelet (109/L) | 217.95 ± 54.59 | 221.84 ± 54.68 | .551 | 217.67 ± 53.61 | 222.98 ± 55.11 | .291 |
| ≥100 | 82 (98.8%) | 452 (99.3%) | .489 | 175 (99.4%) | 359 (99.2%) | 1.000 |
| <100 | 1 (1.2%) | 3 (0.7%) | 1 (0.6%) | 3 (0.8%) | ||
| C‐reactive protein (mg/L) | 6.84 ± 8.87 | 5.44 ± 12.01 | .320 | 5.97 ± 9.84 | 5.50 ± 12.38 | .663 |
| ≤5 | 51 (63.0%) | 316 (72.6%) | .078 | 115 (65.7%) | 252 (73.9%) | .052 |
| >5 | 30 (37.0%) | 119 (27.4) | 60 (34.3%) | 89 (26.1%) | ||
| Aspartate aminotransferase (U/L) | 24.17 ± 9.86 | 26.97 ± 16.00 | .125 | 26.18 ± 14.50 | 26.71 ± 15.60 | .707 |
| ≤40 | 78 (95.1%) | 412 (92.2) | .347 | 162 (94.2%) | 328 (91.9%) | .341 |
| >40 | 4 (4.9%) | 35 (7.8%) | 10 (5.8%) | 29 (8.1%) | ||
| Alanine aminotransferase (U/L) | 30.93 ± 20.18 | 33.24 ± 22.58 | .387 | 32.88 ± 22.69 | 32.88 ± 22.03 | .998 |
| ≤40 | 58 (70.7%) | 325 (72.2%) | .782 | 119 (68.8%) | 264 (73.5%) | .253 |
| >40 | 24 (29.3%) | 125 (27.8%) | 54 (31.2%) | 95 (26.5%) | ||
| Total bilirubin (µmol/L) | 12.86 ± 4.76 | 12.87 ± 4.74 | .990 | 12.92 ± 4.47 | 12.84 ± 4.87 | .858 |
| ≤21 | 78 (95.1%) | 416 (93.5%) | .574 | 163 (94.2%) | 331 (93.5%) | .750 |
| >21 | 4 (4.9%) | 29 (6.5%) | 10 (5.8%) | 23 (6.5%) | ||
| Albumin (g/L) | 46.14 ± 9.37 | 46.48 ± 6.01 | .676 | 46.21 ± 7.78 | 46.53 ± 6.01 | .605 |
| <40 | 6 (7.3%) | 22 (4.9%) | .047 | 10 (5.8%) | 18 (5.1%) | .414 |
| 40–55 | 70 (85.4%) | 412 (92.6%) | 155 (89.6%) | 327 (92.4%) | ||
| >55 | 6 (7.3%) | 11 (2.5%) | 8 (4.6%) | 9 (2.5%) | ||
| Blood urea nitrogen (mmol/L) | 4.62 ± 1.43 | 4.49 ± 1.37 | .438 | 4.45 ± 1.38 | 4.54 ± 1.38 | .504 |
| ≤7.5 | 80 (97.6%) | 432 (99.5%) | .121 | 171 (98.3%) | 341 (99.7%) | .114 |
| >7.5 | 2 (2.4%) | 2 (0.5%) | 3 (1.7%) | 1 (0.3%) | ||
| Serum creatinine (mmol/L) | 59.98 ± 11.80 | 60.73 ± 10.16 | .559 | 60.35 ± 12.02 | 60.75 ± 9.51 | .684 |
| ≤133 | 77 (100.0%) | 406 (100.0%) | NA | 166 (100.0%) | 317 (100.0%) | NA |
| >133 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
Abbreviations: HRQoL, health‐related quality of life; MCS, mental component summary; PCS, physical component summary.
TABLE 4
Results of multivariate logistic regression for HRQoL of discharged COVID‐19 patients.
| Outcomes | Variables | OR (95% CI) | p value |
|---|---|---|---|
| Poor PCS | Sex (female vs. male) | 1.79 (1.04–3.06) | .035 |
| Age (≥60 years vs. <60 years) | 2.44 (1.33–4.47) | .004 | |
| Physical symptoms (yes vs. no) | 40.15 (9.68–166.49) | <.001 | |
| Albumin (g/L) (<40 or >55 vs. 40–50) | 1.78 (0.80–3.98) | .158 | |
| Poor MCS | Sex (female vs. male) | 1.27 (0.86–1.88) | .233 |
| Physical symptoms (yes vs. no) | 6.68 (4.21–10.59) | <.001 |
Abbreviations: CI, confidence interval; COVID‐19, coronavirus disease 2019; HRQoL, health‐related quality of life; MCS, mental component summary; OR, odds ratio; PCS, physical component summary.
5. DISCUSSION
Most of the researches have focused on the HRQoL of hospitalised COVID‐19 patients, but few have revealed HRQoL in post‐discharge COVID‐19 patients. Our study comprehensively investigated the HRQoL of COVID‐19 patients after discharge from hospital and also explored its risk factors. For the HRQoL of discharged COVID‐19 patients, we found that except for GH dimension, scores of all other dimensions of SF‐36 were significantly lower than Chinese norm, which indicated that the HRQoL of COVID‐19 patients was impaired and did not come back to normal even at three months after discharge. These findings were consistent with previous studies (Santus et al., 2020; van der Sar‐van der Brugge et al., 2020). Healthcare workers need to pay attention to physical and psychological conditions at long‐term recovery of COVID‐19 patients. Nevertheless, the finding of our study was partly different with a follow‐up study conducted by Chen, Li, et al., (2020) who found that at one month after discharge, there was no difference in PF score between COVID‐19 patients and Chinese population norm, but the scores of BP, GH, VT and MH were significantly higher and scores of RP, SF and RE were significantly lower in COVID‐19 patients than the Chinese population norm. Possible causes for these differences can be explained by the differences in population characteristics that our study included more older COVID‐19 patients and HRQoL of COVID‐19 patients was investigated at three months after discharge.
Results of multivariate logistical regression indicated that HRQoL of discharged COVID‐19 patients was affected by some factors, that is, female, older age (≥60 years) and physical symptoms after discharge were risk factors for poor PCS, and the physical symptom after discharge was a risk factor for poor MCS. These findings were in line with a previous follow‐up study that older age and female were risk factors for poor HRQoL (Chen, Li, et al., 2020). As we all know, physical symptoms are closely related to poor physical function and great psychological burden (Nunes et al., 2017; Speed et al., 2017; Storm Van’s Gravesande et al., 2019); therefore, it is not surprising that our study found the physical symptom to be a risk factor for poor HRQoL. In our study, compared with male patients, female patients presented with significant lower scores of all dimensions of SF‐36, which indicated that HRQoL of female was much poorer than male. However, results of multivariate logistical regression indicated that female was a risk factor for poor PCS but not for poor MCS. A previous study has demonstrated that women had a worse PCS recovery than men because women perceived greater psychological stress (Xu et al., 2015). Therefore, this may be why poorer PCS in women was observed in our study. However, with the outbreak of COVID‐19, women have perceived a significant higher level of post‐traumatic stress than men (Liu et al., 2020). It has been demonstrated that in general population, women are more susceptible to a series of psychological problems (such as anxiety and depression) than men during the outbreak of COVID‐19 (Wang et al., 2020; Zhou et al., 2020). In addition, it has been proposed that differences in coping strategies and differential neural network activation between women and men may explain gender differences in mental problems (Olff et al., 2007; Schmied et al., 2015). Therefore, women who had experienced the infection of COVID‐19 appear to be more likely to develop psychological problems and have worse recovery of physical health, which suggest that appropriate psychological intervention and care should be made for this vulnerable population even after discharge.
Several limitations in our study should be noted. First, multiple confounding factors (such as chronic diseases) affected the physiological function of the body have not been collected; therefore, multivariate analysis could not be adjusted the potential confounding factors. Second, HRQoL of COVID‐19 patients was only investigated at 3 months after discharge, which may only reflect short‐term physical and psychological recovery of the discharged patients. Long‐term follow‐up can provide more comprehensive information to observe changes in physical and mental health in patients. Third, the overall Cronbach's alpha of SF‐36 in our study was at a low level, which may be contributed for the proportion of older patients (≥40 years old) among our study which was higher than Chinese general population, while it should be noted that Cronbach's alphas of most dimensions of SF‐36 were greater than 0.70, except for SF (0.56) and MH (0.17) dimensions, which were similar to the validity and reliability that has been well verified among the Chinese population (Rui et al., 2011; Yan et al., 2011). Fourth, because the subjects of this study were all Chinese COVID‐19 patients, the conclusion can be generalised to the Chinese population, but it may be not allowed for other countries owing to population cultural difference. Finally, although this study was the follow‐up design, the information of patients was collected at first time of follow‐up and cross‐sectional surveyed which makes it difficult to make causal inferences.
6. CONCLUSION
In conclusion, physical symptoms were common among COVID‐19 patients after discharge, which needs much attention. HRQoL of COVID‐19 patients was impaired and did not come back to normal at third month after discharge. HRQoL was significantly associated with age, sex and physical symptoms after discharge.
7. RELEVANCE TO CLINICAL PRACTICE
Healthcare workers should pay more attention to the physical and psychological rehabilitation of discharged COVID‐19 patients, especially for female and older patients. Long‐term follow‐up on COVID‐19 patients is needed to determine the dynamic recovery of HRQoL.
Supporting information
Table S1
Supplementary Material
Figure S1
Notes
Qu, Zhen, Wang, Fan, Wu and Zhang contributed equally to this manuscript.
Funding information
This study was supported by the National Ten Thousand‐Person Program for Leading Talents in Science and Technology Innovation and the Research Fund of Anhui Institute of Translational Medicine (ZHYX2020A005).
Contributor Information
Liangdan Sun, Email: moc.361@dlsumha, Email: ten.haey@ude_umha_nushy.
Yehuan Sun, Email: ten.haey@ude_umha_nushy.
REFERENCES
- Brazier J. E., Harper R., Jones N. M., O'Cathain A., Thomas K. J., Usherwood T., Westlake L. (1992). Validating the SF‐36 Health Survey Questionnaire: New outcome measure for primary care. BMJ, 305(6846), 160–164. [Europe PMC free article] [Abstract] [Google Scholar]
- Carfì A., Bernabei R., & Landi F., Gemelli Against COVID‐19 Post‐Acute Care Study Group . (2020). Persistent symptoms in patients after acute COVID‐19. JAMA, 324(6), 603–605. [Europe PMC free article] [Abstract] [Google Scholar]
- Chen K. Y., Li T., Gong F. H., Zhang J. S., & Li X. K. (2020). Predictors of health‐related quality of life and influencing factors for COVID‐19 patients, a follow‐up at one month. Frontiers in Psychiatry, 11, 668. [Europe PMC free article] [Abstract] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., & Zhang L. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A descriptive study. Lancet, 395(10223), 507–513. [Europe PMC free article] [Abstract] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates. [Google Scholar]
- Dawson P., Rabold E. M., Laws R. L., Conners E. E., Gharpure R., Yin S., Buono S. A., Dasu T., Bhattacharyya S., Westergaard R. P., Pray I. W., Ye D., Nabity S. A., Tate J. E., & Kirking H. L. (2020). Loss of taste and smell as distinguishing symptoms of COVID‐19. Clinical Infectious Diseases, 72(4):682–685. 10.1093/cid/ciaa799 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Garrigues E., Janvier P., Kherabi Y., Le B. A., Hamon A., Gouze H., Doucet L., Berkani S., Oliosi E., Mallart E., Corre F., Zarrouk V., Moyer J. D., Galy A., Honsel V., Fantin B., Nguyen Y. A., Hamon A., & Gouze H. (2020). Post‐discharge persistent symptoms and health‐related quality of life after hospitalization for COVID‐19. Journal of Infection, 81(6), e4–e6. [Europe PMC free article] [Abstract] [Google Scholar]
- Gill T. M., & Feinstein A. R. (1994). A critical appraisal of the quality of quality‐of‐life measurements. JAMA, 272(8), 619–626. [Abstract] [Google Scholar]
- Kim J., Thomsen T., Sell N., & Goldsmith A. J. (2020). Abdominal and testicular pain: An atypical presentation of COVID‐19. American Journal of Emergency Medicine, 38(7), 1542. [Europe PMC free article] [Abstract] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., & Liu W. (2020). Prevalence and predictors of PTSS during COVID‐19 outbreak in China hardest‐hit areas: Gender differences matter. Psychiatry Research, 287, 112921. [Europe PMC free article] [Abstract] [Google Scholar]
- Nguyen H. C., Nguyen M. H., Do B. N., Tran C. Q., Nguyen T. T. P., Pham K. M., Pham L. V., Tran K. V., Duong T. T., Tran T. V., Duong T. H., Nguyen T. T., Nguyen Q. H., Hoang T. M., Nguyen K. T., Pham T. T. M., Yang S. H., Chao J. C., & Duong T. V. (2020). People with suspected COVID‐19 symptoms were more likely depressed and had lower health‐related quality of life: the potential benefit of health literacy. Journal of Clinical Medicine, 9(4), 965. [Europe PMC free article] [Abstract] [Google Scholar]
- Nunes M. D. R., Jacob E., Bomfim E. O., Lopes‐Junior L. C., de Lima R. A. G., Floria‐Santos M., Nascimento L. C. (2017). Fatigue and health related quality of life in children and adolescents with cancer. European Journal of Oncology Nursing, 29, 39–46. [Europe PMC free article] [Abstract] [Google Scholar]
- Olff M., Langeland W., Draijer N., & Gersons B. P. (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183–204. [Abstract] [Google Scholar]
- Rui W., Cheng W. U., Ma X. Q., Zhao Y. F., Yan X. Y., & Jia H. E. (2011). Health‐related quality of life in Chinese people: A population‐based survey of five cities in China. Scandinavian Journal of Public Health, 39(4), 410–418. [Abstract] [Google Scholar]
- Santus P., Tursi F., Croce G., Di Simone C., Frassanito F., Gaboardi P., Airoldi A., Pecis M., Negretto G., & Radovanovic D. (2020). Changes in quality of life and dyspnoea after hospitalization in COVID‐19 patients discharged at home. Multidisciplinary Respiratory Medicine, 15(1), 713. [Europe PMC free article] [Abstract] [Google Scholar]
- Schipper H., Clinch J., & Powell V. (1996). Quality of life studies: Definitions and conceptual issues. In B. Spilker , editor. (Ed.), Quality of life and pharmacoeconomics in clinical trials (pp. 11–24). Lippincott‐Raven. [Google Scholar]
- Schmied E. A., Padilla G. A., Thomsen C. J., Lauby M. D., Harris E., & Taylor M. K. (2015). Sex differences in coping strategies in military survival school. Journal of Anxiety Disorders, 29, 7–13. [Abstract] [Google Scholar]
- Speed T. J., Mathur V. A., Hand M., Christensen B., Sponseller P. D., Williams K. A., & Campbell C. M. (2017). Characterization of pain, disability, and psychological burden in Marfan syndrome. American Journal of Medical Genetics. Part A, 173(2), 315–323. [Europe PMC free article] [Abstract] [Google Scholar]
- Storm Van's Gavesande S. V., Blaschek A., Calabrese P., Rostásy K., Huppke P., Kessler J. J., Kalbe E., Mall V. & MUSICADO Study Group . (2019). Fatigue and depression predict health‐related quality of life in patients with pediatric‐onset multiple sclerosis. Multiple Sclerosis and Related Disorders, 36, 101368. [Abstract] [Google Scholar]
- Tian Y., Rong L., Nian W., & He Y. (2020). Review article: gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Alimentary Pharmacology & Therapeutics, 51(9), 843–851. [Europe PMC free article] [Abstract] [Google Scholar]
- van der Sar‐van der Brugge S., Talman S., Boonman‐de Winter L., de Mol M., Hoefman E., van Etten R. W., & De Backer I. C. (2020). Pulmonary function and health‐related quality of life after COVID‐19 pneumonia. Respiratory Medicine, 176, 106272. [Europe PMC free article] [Abstract] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C. S., Ho R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. [Europe PMC free article] [Abstract] [Google Scholar]
- World Health Organization (2020). Coronavirus disease 2019 (COVID‐19). Situation report – 204. World Health Organization. 11 August, 2020. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200811‐covid‐19‐sitrep‐204.pdf?sfvrsn=1f4383dd_2 [Google Scholar]
- Xu X., Bao H., Strait K., Spertus J. A., Lichtman J. H., D'Onofrio G., Spatz E., Bucholz E. M., Geda M., Lorenze N. P., Bueno H., Beltrame J. F., & Krumholz H. M. (2015). Sex differences in perceived stress and early recovery in young and middle‐aged patients with acute myocardial infarction. Circulation, 131(7), 614–623. [Europe PMC free article] [Abstract] [Google Scholar]
- Yan S., Lian Z., Sun G., Bao Y., Ge Y., & Liu Z. (2011). Assessment of the Chinese‐version SF‐36 in the Chinese opiate addicts. Substance Use and Misuse, 46(13), 1561–1568. [Abstract] [Google Scholar]
- Ye G., Pan Z., Pan Y., Deng Q., Chen L., Li J., Li Y., & Wang X. (2020). Clinical characteristics of Severe Acute Respiratory Syndrome Coronavirus 2 reactivation. Journal of Infection, 80(5), e14–e17. [Europe PMC free article] [Abstract] [Google Scholar]
- Yuan B., Li W., Liu H., Cai X., Song S., Zhao J., Hu X., Li Z., Chen Y., Zhang K., Liu Z., Peng J., Wang C., Wang J., & An Y. (2020). Correlation between immune response and self‐reported depression during convalescence from COVID‐19. Brain, Behavior, and Immunity, 88, 39–43. [Europe PMC free article] [Abstract] [Google Scholar]
- Zhang Y., & Ma Z. F. (2020). Impact of the COVID‐19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross‐sectional study. International Journal of Environmental Research and Public Health, 17(7), 2381. [Europe PMC free article] [Abstract] [Google Scholar]
- Zheng Z., Yao Z., Wu K., & Zheng J. (2020). Patient follow‐up after discharge after COVID‐19 Pneumonia: Considerations for infectious control. Journal of Medical Virology, 92(11):2412–2419. 10.1002/jmv.25994 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Zhou S. J., Zhang L. G., Wang L. L., Guo Z. C., Wang J. Q., Chen J. C., Liu M., Chen X., & Chen J. X. (2020). Prevalence and socio‐demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID‐19. European Child and Adolescent Psychiatry, 29(6), 749–758. [Europe PMC free article] [Abstract] [Google Scholar]
Full text links
Read article at publisher's site: https://doi.org/10.1111/jocn.15733
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8013595
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/101289057
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1111/jocn.15733
Article citations
Socio-demographic and clinical predictors of post-acute, mid-and long-term psychological sequelae of COVID-19: a two-year cross-sectional investigation on 1317 patients at the University Hospital of Verona.
Arch Public Health, 82(1):198, 31 Oct 2024
Cited by: 0 articles | PMID: 39482728 | PMCID: PMC11526637
Predictors of health-related quality of Life for COVID-19 survivors living in Dhaka, Bangladesh: A repeated Follow-Up after 18 months of their recovery.
PLOS Glob Public Health, 4(8):e0003472, 28 Aug 2024
Cited by: 0 articles | PMID: 39197043 | PMCID: PMC11356435
Development of a Risk Predictive Model for Erectile Dysfunction at 12 Months after COVID-19 Recovery: A Prospective Observational Study.
J Clin Med, 13(19):5757, 27 Sep 2024
Cited by: 0 articles | PMID: 39407818 | PMCID: PMC11477077
Protocol for a longitudinal study examining the trajectory of COVID-19, post-COVID, multidimensional disadvantage and health-related quality of life in India: the IndiQol Project.
BMJ Open, 14(7):e080985, 15 Jul 2024
Cited by: 0 articles | PMID: 39009459 | PMCID: PMC11253756
Enhancing quality of life in severe post-COVID-19 survivors through multidisciplinary care.
ERJ Open Res, 10(4):214-2024, 01 Jul 2024
Cited by: 0 articles | PMID: 39104955 | PMCID: PMC11299004
Go to all (81) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Impact of COVID-19 on Quality of Life After Hospital Discharge in Patients Treated With Noninvasive Ventilation/Continuous Positive Airway Pressure: An Observational, Prospective Multicenter Study.
Dimens Crit Care Nurs, 43(1):3-12, 01 Jan 2024
Cited by: 0 articles | PMID: 38059706
Psychological distress and health-related quality of life in patients after hospitalization during the COVID-19 pandemic: A single-center, observational study.
PLoS One, 16(8):e0255774, 11 Aug 2021
Cited by: 40 articles | PMID: 34379644 | PMCID: PMC8357130
1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study.
Lancet, 398(10302):747-758, 01 Aug 2021
Cited by: 566 articles | PMID: 34454673 | PMCID: PMC8389999
CO-FLOW: COvid-19 Follow-up care paths and Long-term Outcomes Within the Dutch health care system: study protocol of a multicenter prospective cohort study following patients 2 years after hospital discharge.
BMC Health Serv Res, 21(1):847, 21 Aug 2021
Cited by: 17 articles | PMID: 34419032 | PMCID: PMC8379596
Funding
Funders who supported this work.
National Ten Thousand-Person Program for Leading Talents in Science and Technology Innovation
Research Fund of Anhui Institute of Translational Medicine (1)
Grant ID: ZHYX2020A005

 14
and
14
and