Abstract
Objectives
Cerebral venous sinus stenting (VSS) has emerged as a new surgical procedure for the treatment of severe idiopathic intracranial hypertension (IIH), and its popularity has been anecdotally on the rise. This study explores recent temporal trends of VSS and other surgical IIH treatments in the United States.Methods
Adult patients with IIH were identified from the 2016-2020 National Inpatient Sample databases, and surgical procedures and hospital characteristics were recorded. Temporal trends of procedure numbers for VSS, CSF shunts, and optic nerve sheath fenestrations (ONSFs) were assessed and compared.Results
A total of 46,065 (95% CI 44,710-47,420) patients with IIH were identified, of whom 7,535 patients (95% CI 6,982-8,088) received surgical IIH treatments. VSS procedures increased 80% (150 [95% CI 55-245] to 270 [95% CI 162-378] per year, p < 0.001). Concurrently, the number of CSF shunts decreased by 19% (1,365 [95% CI 1,126-1,604] to 1,105 [95% CI 900-1,310] per year, p < 0.001), and ONSF procedures decreased by 54% (65 [95% CI 20-110] to 30 [95% CI 6-54] per year, p < 0.001).Discussion
Practice patterns for surgical IIH treatment in the United States are rapidly evolving, and VSS is becoming increasingly common. These findings highlight the urgency of randomized controlled trials to investigate the comparative effectiveness and safety of VSS, CSF shunts, ONSF, and standard medical treatments.Free full text

National Trends of Cerebral Venous Sinus Stenting for the Treatment of Idiopathic Intracranial Hypertension
Associated Data
Abstract
Objectives
Cerebral venous sinus stenting (VSS) has emerged as a new surgical procedure for the treatment of severe idiopathic intracranial hypertension (IIH), and its popularity has been anecdotally on the rise. This study explores recent temporal trends of VSS and other surgical IIH treatments in the United States.
Methods
Adult patients with IIH were identified from the 2016–2020 National Inpatient Sample databases, and surgical procedures and hospital characteristics were recorded. Temporal trends of procedure numbers for VSS, CSF shunts, and optic nerve sheath fenestrations (ONSFs) were assessed and compared.
Results
A total of 46,065 (95% CI 44,710–47,420) patients with IIH were identified, of whom 7,535 patients (95% CI 6,982–8,088) received surgical IIH treatments. VSS procedures increased 80% (150 [95% CI 55–245] to 270 [95% CI 162–378] per year, p < 0.001). Concurrently, the number of CSF shunts decreased by 19% (1,365 [95% CI 1,126–1,604] to 1,105 [95% CI 900–1,310] per year, p < 0.001), and ONSF procedures decreased by 54% (65 [95% CI 20–110] to 30 [95% CI 6–54] per year, p < 0.001).
Discussion
Practice patterns for surgical IIH treatment in the United States are rapidly evolving, and VSS is becoming increasingly common. These findings highlight the urgency of randomized controlled trials to investigate the comparative effectiveness and safety of VSS, CSF shunts, ONSF, and standard medical treatments.
Idiopathic intracranial hypertension (IIH) is a burgeoning disease worldwide.1-3 Left untreated, IIH can lead to debilitating headaches and permanent vision loss due to prolonged elevation of intracranial pressure (ICP).4 Venous sinus stenting (VSS), first performed by Higgins et al. in 2002,5 is a relatively new surgical treatment for patients with IIH who are refractory to conservative medical management, and it may lead to a durable reduction of ICP and improve headaches and papilledema in patients with venous sinus stenosis.6,7 While these early results are promising, the pathophysiologic link between venous sinus stenosis and IIH remains poorly understood.8,9 Despite lingering questions and a lack of long-term efficacy data, VSS is increasingly used in clinical practice, and the number of VSS procedures nationwide has anecdotally been on the rise.10 In this cross-sectional study, we queried the 2016–2020 data of the National Inpatient Sample (NIS) to explore temporal trends and practice patterns of surgical IIH treatments in the United States, with a specific focus on VSS procedures.
Methods
Database Characteristics
The Healthcare Cost and Utilization Project's (HCUP) NIS database is a stratified discharge database representing 20% of all inpatient admissions in the United States. The database contains approximately 35 million weighted annual hospitalizations from 48 states and the District of Columbia and covers 97% of the US population.
Patient Population and Hospital Characteristics
The NIS database was queried from 2016 to 2020 for all inpatient admissions for adults aged 18–65 years. The International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis and procedural coding system were used to identify patients with IIH and surgical interventions. The year 2016 was chosen as the start year because it was the first year to use ICD-10-CM for all patients. Patients with a diagnosis of IIH (G93.2) listed as one of the top 5 diagnosis codes were included. Patients with secondary causes of elevated ICP were excluded (eTable 1, links.lww.com/WNL/C715). Patient characteristics (age, sex, medical history, complications, length of stay, and procedure costs) were recorded. Hospital characteristics (region, size, and teaching status) were also recorded. Academic teaching hospitals with a large number of beds, as defined by the HCUP, were classified as large academic hospitals.
Statistical Methods
Discharge-level weights provided by the Agency for Healthcare Research and Quality were used to calculate national estimates. Parametric data were expressed as mean ± SD and compared through 1-way analysis of variance tests. Nominal data were compared with Pearson χ2 analyses. Temporal trends of procedure numbers were assessed for significant changes over time with chi-square goodness-of-fit tests. p Values less than 0.05 were deemed statistically significant. Statistical analyses were performed using R, version 3.6.2.
Standard Protocol Approvals, Registrations, and Patient Consents
The NIS database lacks unique patient identifiers and therefore is exempt from institutional review board and informed consent under the Health Insurance Portability and Accountability Act.
Data Availability
The NIS database is available to the public and can be requested from hcup-us.ahrq.gov.
Results
A total of 46,065 patients with IIH were identified, of whom 7,545 (16.4%) received surgical treatment. There were no in-hospital mortalities or intracranial hemorrhages. Patient characteristics differed significantly among treatment modalities (Table 1). Hospital characteristics are detailed in eTable 2 (links.lww.com/WNL/C716), and patient income and insurance information are detailed in eTable 3 (links.lww.com/WNL/C717). From 2016 to 2020, the number of IIH-related admissions did not significantly change over time (9,610–8,385, p = 0.11) nor did the number of surgical IIH treatments (1,580–1,405, p = 0.47). In the same period, the number of VSS procedures increased 80% (150 procedures in 2016 to 270 procedures in 2020, p < 0.001; Table 2, Figure 1). Concurrently, the number of CSF shunt insertions and ONSF decreased 19% and 54%, respectively (p < 0.001 for both; Table 2, Figure 1). In 2020, VSS accounted for 19.2% of all surgical IIH treatments nationwide.
Table 1
Patient Characteristics
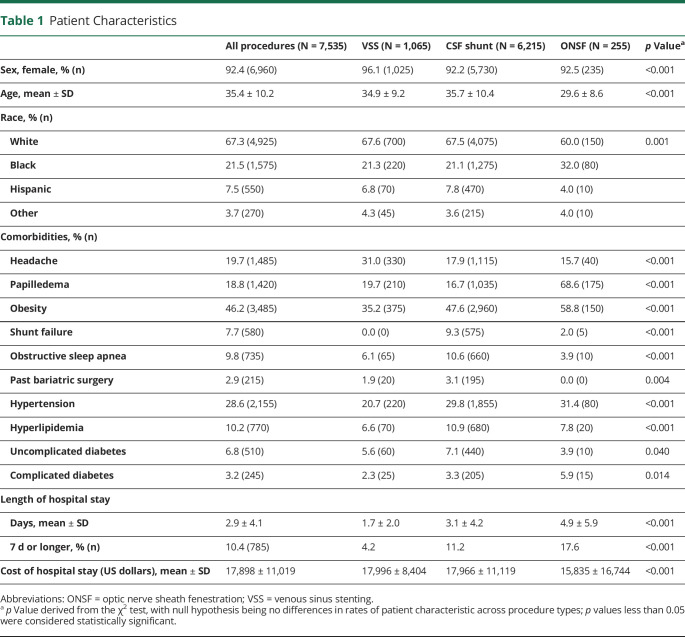
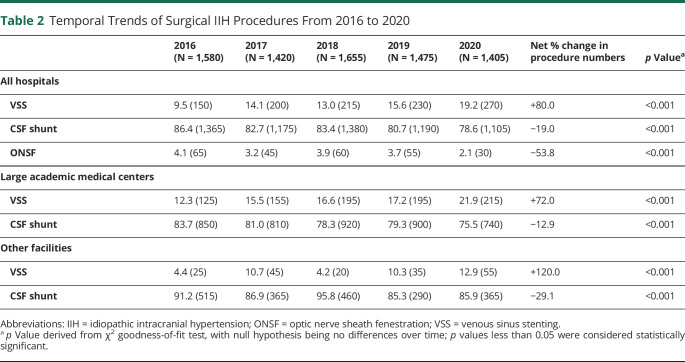
Table 2
Temporal Trends of Surgical IIH Procedures From 2016 to 2020
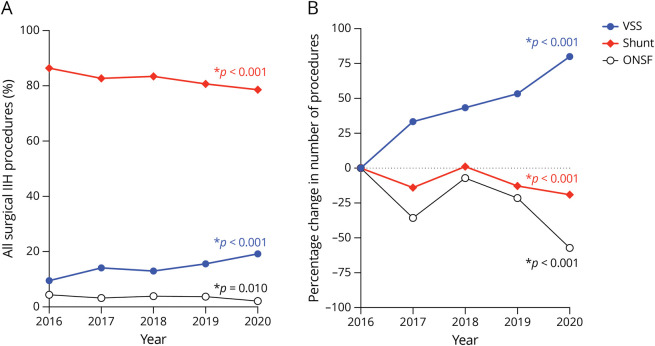
(A) Percentage of shunt, VSS, and ONSF among all surgical IIH procedures over time; p values derived from χ2 analysis. (B) Percentage change of number of procedures from 2016 to 2020; p values derived from comparison number of each procedure as a proportion of total procedures between 2016 and 2020 using the Fisher exact test. IIH = idiopathic intracranial hypertension; ONSF = optic nerve sheath fenestration; VSS = venous sinus stenting.
Over the study period, the number of VSS procedures performed at large urban academic medical centers increased 72%, and the proportion of surgical IIH treatments that were VSS increased from 12.3% to 21.9% (p < 0.001; Table 2). Similarly, the number of VSS procedures performed at smaller academic medical centers and community hospitals increased 120%, and the proportion of surgical IIH treatments that were VSS increased from 4.4% to 12.9%, a near 3-fold increase (p < 0.001; Table 2). Temporal trends of CSF shunting stratified by hospital type are also summarized in Table 2.
Discussion
In this cross-sectional study of 46,065 patients with IIH hospitalized in the United States, we show that VSS procedures increased 80% over the 5-year study period, roughly accounting for 1 in 5 surgical IIH treatments in 2020. There were concurrent decreases in the number of CSF shunts and ONSF procedures, suggesting that the practice patterns for surgical IIH treatment nationwide are rapidly evolving.
The growth of VSS procedures may have been driven by multiple factors. First, increasing number of procedures could reflect increasing incidence of IIH. Second, VSS is minimally invasive and generally considered safe, with low rates of complications.6,7 Furthermore, the neurointerventional workforce has grown considerably in recent years,11 and increased utilization of magnetic resonance and computed tomography venogram studies may have led to increased detection of cerebral venous sinus stenosis. Of importance, CSF shunts and ONSF numbers have significantly declined, suggesting that practitioners may be relatively favoring VSS instead, which may be driven by its superior safety profile6 and patient acceptance due to its minimally invasive nature. While it is presently unclear whether VSS procedures will continue to grow, our results show increasing VSS numbers across all hospital subtypes, particularly in smaller academic medical centers and community hospitals. This trend is likely to continue because the procedure is becoming available widely in the United States and the devices continue to improve.
While past studies have demonstrated VSS's short-term outcomes,6,7 data on long-term comparative efficacy and safety with other treatments are sparse. Uncertainty surrounding the pathophysiologic role of venous sinus stenosis in IIH also remains, particularly regarding whether it is a cause or an effect of severe IIH.8 Prospective clinical trials are urgently needed to investigate the efficacy and safety of VSS compared with medical therapy and/or other surgical options. However, patient recruitment of clinical trials for surgical IIH treatments (e.g., the SIGHT trial12) has been difficult, which may have been driven by both the proven effectiveness of medical therapy13 and the high risks of CSF shunting and ONSF.6,14,15 It is unclear whether VSS's superior safety profile could overcome challenges in recruitment. At a minimum, initiation of a nationwide prospective registry of VSS patients that includes pretreatment and posttreatment neuro-ophthalmological assessments may be helpful in shedding light on the long-term safety and effectiveness of VSS.
Our study has several limitations. First, because the identification of diseases using recorded ICD-10 codes can be inaccurate, the reporting rates of comorbidities may not always reflect the presence/absence of each condition and may instead reflect disease severity. Second, the NIS captures only hospital admissions, and IIH is mainly managed on an outpatient basis. However, CSF shunting, VSS, and ONSF procedures generally require hospital stays, so our estimations of national procedure numbers are likely accurate. Third, the NIS provides only encounter-level data, and we were not able to assess the longitudinal outcomes of patients with IIH treated with VSS. Finally, our findings of increasing VSS procedures were restricted to the United States, and external validity is unclear.
In conclusion, in this cross-sectional study of 46,065 patients with IIH, we found that VSS procedures are rapidly increasing in the United States. These findings highlight the urgency of randomized controlled trials to investigate the comparative effectiveness and safety of VSS compared with standard medical treatments.
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
The authors report no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
Articles from Neurology are provided here courtesy of American Academy of Neurology
Citations & impact
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/144622292
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1212/wnl.0000000000207245
Article citations
Progress and recognition of idiopathic intracranial hypertension: A narrative review.
CNS Neurosci Ther, 30(8):e14895, 01 Aug 2024
Cited by: 0 articles | PMID: 39097911 | PMCID: PMC11298205
Review Free full text in Europe PMC
National Trends of Cerebral Venous Sinus Stenting for the Treatment of Idiopathic Intracranial Hypertension.
Neurology, 102(6):e208069, 23 Feb 2024
Cited by: 0 articles | PMID: 38394607 | PMCID: PMC11383875
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Understanding the complex pathophysiology of idiopathic intracranial hypertension and the evolving role of venous sinus stenting: a comprehensive review of the literature.
Neurosurg Focus, 45(1):E10, 01 Jul 2018
Cited by: 19 articles | PMID: 29961379
Review
Dural Venous Sinus Stenting in Idiopathic Intracranial Hypertension: A National Database Study of 541 Patients.
World Neurosurg, 167:e451-e455, 13 Aug 2022
Cited by: 6 articles | PMID: 35973522
Life-threatening idiopathic intracranial hypertension: the role of venous sinus stenting.
Childs Nerv Syst, 38(8):1433-1443, 10 Jun 2022
Cited by: 2 articles | PMID: 35687167
Review
Management of idiopathic intracranial hypertension in children utilizing venous sinus stenting.
Interv Neuroradiol, 27(2):257-265, 25 Nov 2020
Cited by: 3 articles | PMID: 33236688 | PMCID: PMC8050535




