Abstract
Free full text
Socio-economic deprivation and the risk of death after ICU admission with COVID-19: The poor relation
To the Editor,
The mortality of coronavirus-2019 disease (COVID-19) in hospitalised patients is currently reported as being 26% in the United Kingdom. 1 Increased severity of COVID-19 has been associated with advanced age, male gender, obesity, and comorbidities such as diabetes and chronic cardiac disease. 1 In addition, the incidence of COVID-19 is higher in those who are socio-economically disadvantaged. 2 The relationship between deprivation and health inequality is established, with a national study of admissions to critical care in the United Kingdom demonstrating an association between increased mortality and greater degree of socioeconomic deprivation. 3 To date, little is known about the effect of existing deprivation on the outcomes of patients admitted to ICU with COVID-19. Here, we report from Glasgow, a city with some of the highest levels of socio-economic deprivation in Western Europe. 4
We studied all consecutive patients admitted to the ICU of the Queen Elizabeth II University Hospital, Glasgow, with confirmed SARS-CoV-2 infection, between 19 March 2020, and 15 June 2020. Data were collected on patient demographics, pre-morbid health status, clinical parameters, and laboratory variables. Each patient was assigned to a Scottish Index of Multiple Deprivation (SIMD) quintile based on the location of their primary residence.
5
To explore the relationship between severe deprivation and outcome, we used a Cox proportional hazards regression model. This estimated the association of deprivation with 30-day mortality in those in the bottom quintile (quintile 1, most deprived) versus those who were less deprived (quintiles 2–5). Age at admission, sex, and APACHE II score in the first 24 hours of ICU, were included as potential confounders. P values <0.05 were considered significant. Analyses were conducted in R (R Core Team, 2017).
hours of ICU, were included as potential confounders. P values <0.05 were considered significant. Analyses were conducted in R (R Core Team, 2017).
In total, 62 patients were admitted to ICU with COVID-19. The majority were male (n =
= 47, 75.8%), with a median age of 58 (IQR 52–63) years. All received invasive mechanical ventilation, with a median PaO2/FiO2 ratio of 15 (IQR 10.6–20.8) kPa at commencement. The median APACHE II score in the first 24
47, 75.8%), with a median age of 58 (IQR 52–63) years. All received invasive mechanical ventilation, with a median PaO2/FiO2 ratio of 15 (IQR 10.6–20.8) kPa at commencement. The median APACHE II score in the first 24 hours was 19 (IQR 15–24). The most deprived SIMD quintile accounted for 29 (46.8%) of patients. Overall, the 30-day mortality was 50% (SIMD Q1 62% vs. SIMD Q2–5 39%). The association between SIMD on 30-day mortality is presented in Figure 1. After adjusting for age, sex, and APACHE II score, socio-economic deprivation was associated with an almost 3 times higher hazard in this cohort (HR 2.9, 95% CI 1.3–6.5, p
hours was 19 (IQR 15–24). The most deprived SIMD quintile accounted for 29 (46.8%) of patients. Overall, the 30-day mortality was 50% (SIMD Q1 62% vs. SIMD Q2–5 39%). The association between SIMD on 30-day mortality is presented in Figure 1. After adjusting for age, sex, and APACHE II score, socio-economic deprivation was associated with an almost 3 times higher hazard in this cohort (HR 2.9, 95% CI 1.3–6.5, p =
= 0.04). Age and sex were also independently associated with an increased hazard of death.
0.04). Age and sex were also independently associated with an increased hazard of death.
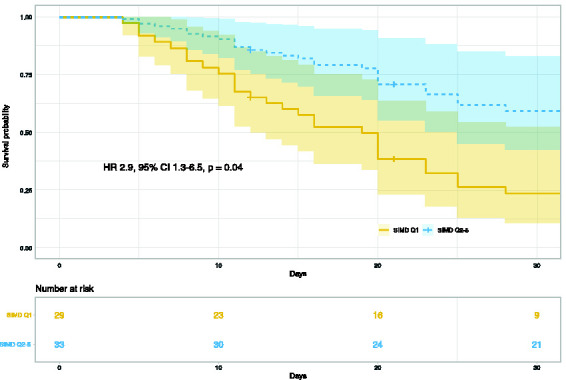
Kaplan-Meier plot of SIMD (Quintile 1 vs. Quintile 2–5) and 30-day mortality following ICU admission adjusted for age, sex and APACHE II score at admission.
Shaded areas indicate the 95% confidence intervals.
These data are limited by several factors, including the number of patients, the single-centre nature of this study, and the presence of other potential confounders, such as pre-existing conditions, which have not been corrected for. However, the possibility that some of the most vulnerable in society remain at increased risk of adverse outcomes after COVID-19, when age, sex, and disease severity are accounted for, should provoke urgent investigation. Socio-economic deprivation should not remain the poor relation of COVID-19 risk factors.
Ethics approval
This study was deemed not to require formal ethical approval by NHS Greater & Glasgow Clyde Research & Development under a public health exception. Permission for the study was sought from and granted by the local Caldicott Guardian.
Availability of data and material
The authors will share de-identified data on reasonable request.
Code availability
The authors will share reproducible R code for the study analyses on reasonable request.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ
2020;
369: m1985. [Europe PMC free article] [Abstract] [Google Scholar]
133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ
2020;
369: m1985. [Europe PMC free article] [Abstract] [Google Scholar]Articles from Journal of the Intensive Care Society are provided here courtesy of SAGE Publications
Full text links
Read article at publisher's site: https://doi.org/10.1177/1751143720978855
Read article for free, from open access legal sources, via Unpaywall:
https://journals.sagepub.com/doi/pdf/10.1177/1751143720978855
Citations & impact
Impact metrics
Article citations
Modeling Years of Life Lost Due to COVID-19, Socioeconomic Status, and Nonpharmaceutical Interventions: Development of a Prediction Model.
JMIRx Med, 3(2):e30144, 12 Apr 2022
Cited by: 1 article | PMID: 35438949 | PMCID: PMC9007225
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Association of socio-economic deprivation with COVID-19 incidence and fatality during the first wave of the pandemic in Italy: lessons learned from a local register-based study.
Int J Health Geogr, 22(1):10, 04 May 2023
Cited by: 1 article | PMID: 37143110 | PMCID: PMC10157567
Cardiac Parameters Better Predict ICU Admission and Short-Term Mortality in Hospitalized Patients With COVID-19.
Cureus, 15(9):e46141, 28 Sep 2023
Cited by: 0 articles | PMID: 37900381 | PMCID: PMC10612987
Difference in determinants of ICU admission and death among COVID-19 hospitalized patients in two epidemic waves in Portugal: possible impact of healthcare burden and hospital bed occupancy on clinical management and outcomes, March-December 2020.
Front Public Health, 11:1215833, 29 Jun 2023
Cited by: 1 article | PMID: 37501943 | PMCID: PMC10370276
COVID-19 incidence and outcome by affluence/deprivation across three pandemic waves in Ireland: A retrospective cohort study using routinely collected data.
PLoS One, 18(7):e0287636, 21 Jul 2023
Cited by: 1 article | PMID: 37478117 | PMCID: PMC10361474
 1
1 




