Abstract
Background
Venous sinus stenting (VSS) is a safe and effective treatment strategy for pulsatile tinnitus (PT) and idiopathic intracranial hypertension (IIH). Although complications are rare, the morbidity associated with the complications is high. Navigating through the venous sinuses poses unique challenges to the interventionalist. There is limited literature regarding device selection to maximize safety and efficiency. We report on the safety and advantages of using a balloon guide catheter (BGC) for venous access in VSS.Methods
Retrospective analysis of all patients undergoing VSS using a BGC over a three-month period.Results
A total of 22 patients were included in the analysis (median age 35; 21 female). The indication for treatment was PT in 10 patients and IIH in 12 patients. The BGC was navigated into the sigmoid and transverse sinuses, enabling successful delivery of the stent in all cases. The BGC balloon was inflated 23 times for navigating past tortuosity or obstructions, and for anchoring. There were no intraprocedural complications.Conclusions
The use of BGC in VSS is safe and feasible. BGCs have features that can be utilized to overcome the unique challenges encountered during VSS.Free full text

The use of balloon guide catheters during venous sinus stenting: A case series
Abstract
Background
Venous sinus stenting (VSS) is a safe and effective treatment strategy for pulsatile tinnitus (PT) and idiopathic intracranial hypertension (IIH). Although complications are rare, the morbidity associated with the complications is high. Navigating through the venous sinuses poses unique challenges to the interventionalist. There is limited literature regarding device selection to maximize safety and efficiency. We report on the safety and advantages of using a balloon guide catheter (BGC) for venous access in VSS.
Methods
Retrospective analysis of all patients undergoing VSS using a BGC over a three-month period.
Results
A total of 22 patients were included in the analysis (median age 35; 21 female). The indication for treatment was PT in 10 patients and IIH in 12 patients. The BGC was navigated into the sigmoid and transverse sinuses, enabling successful delivery of the stent in all cases. The BGC balloon was inflated 23 times for navigating past tortuosity or obstructions, and for anchoring. There were no intraprocedural complications.
Conclusions
The use of BGC in VSS is safe and feasible. BGCs have features that can be utilized to overcome the unique challenges encountered during VSS.
Introduction
Venous sinus stenting (VSS) is an increasingly popular and effective treatment for idiopathic intracranial hypertension (IIH) and pulsatile tinnitus (PT).1–5 It has been shown to be safe and results in improvements in headache, intracranial pressure, and papilledema in many patients with IIH.1,4–6 In patients with PT, VSS has been shown to completely resolve tinnitus in up to 93% of cases. 3 These promising results have led to an 80% increase in VSS since 2016 for the treatment of IIH. 2 Complications rates for VSS range from 1% to 6% and include subdural hematoma, subarachnoid hemorrhage, intracerebral hemorrhage, in-stent thrombosis, and retroperitoneal hemorrhage.1,3–5,7,8 Despite the increasing popularity of VSS, there is a paucity of literature on device selection and the technical aspects of VSS. In addition, there is considerable variability in device selection and technique among interventionalists.7,9 Venous navigation for stenting poses unique challenges to the interventionalist, including retrograde sinus access, which can frequently require substantial force due to obstructions by dural leaflets, webs, granulations, and severe stenoses. Navigating beyond these obstructions may involve exchanging for stiffer catheters and wires or the application of more force, which is inefficient, dangerous, and often ineffective. Due to the significant morbidity associated with complications during VSS, proper device selection to maximize safety and efficiency is critical.
Balloon guide catheters (BGCs) have recently been shown to be superior to conventional guide catheters when used for mechanical thrombectomy while maintaining safety.10–12 Advancements in catheter technology have allowed for the widespread adoption of BGCs in the neuro-interventional field. New BGCs such as the Walrus (Q’apel Medical, Fremont, CA) have thin walls; therefore, they accommodate the largest available aspiration catheters while maintaining a low profile. The Walrus BGCs are resistant to kinking, have increased navigability while maintaining support, and have a larger balloon than other currently available neuro-interventional BGCs. These qualities have proven to be advantageous in mechanical thrombectomy and can apply to VSS procedures as well. Currently, there is no data on the potential utility of BGCs for VSS. Here, we report a single-center, single-interventionalist series reporting outcomes and illustrating the utility of BGCs for VSS.
Methods
Patient selection
Consecutive patients who underwent VSS using the Walrus BGC at a single academic center with a single interventionalist from March 2023 to June 2023 were included in this analysis. The institutional review board approved this retrospective study. Consent was waived due to the retrospective nature of the study.
Data collection and statistical analysis
Demographic, clinical, and radiographic data were recorded, including age, gender, baseline comorbidities, location of stenosis, indication for the procedure, procedural details including access devices, use of balloon angioplasty, complications, and success in catheter navigation in distal venous anatomy. Descriptive statistics were utilized for all variables of interest in statistical analysis.
Procedural details
All patients were placed on dual antiplatelet therapy of aspirin 325 mg and clopidogrel 75 mg for five days prior to the procedure. All patients were evaluated with a catheter cerebral venogram and manometry while awake prior to the VSS procedure. Once a venogram confirmed the presence of a venous stenosis with a gradient, the remainder of the stenting procedure was completed. Under general anesthesia, a hydrophilic 5 French sheath was inserted into the right radial artery and a cerebral angiogram was performed using a Simmons 2 Glide catheter (MicroVention, Aliso Viejo, CA). A 90 cm Walrus BGC was then advanced into the right internal jugular vein over a 180 cm 0.035″ Glide guidewire (MicroVention, Aliso Viejo, CA) and a 5 French 130 cm Neuron Select Berenstein catheter (Penumbra, Alameda, CA). Under fluoroscopic roadmap guidance, a 156 cm Headway 27 microcatheter (Microvention, Aliso Viejo, CA) was then advanced over a 215 cm Synchro 2 microwire (Stryker, Fremont, CA) with a J-curve into the Superior Sagittal Sinus (SSS), taking care to point the wire inferiorly, thereby avoiding the site of cortical vein entry. An intermediate 115 cm Navien 0.072″ catheter (Medtronic, Santa Rosa, CA) along with the Walrus BGC was then advanced over the Headway 27 and Synchro microwire to the sigmoid or transverse sinus. The Synchro 2 microwire was then exchanged for a Balance Heavyweight 0.014″ microwire (Abbot, Plymouth, MN) with a J-curve, which was positioned in the SSS. The Walrus BGC and the Navien intermediate catheter were then also advanced with the Navien positioned past the stenosis. The microcatheter was removed and a Precise Pro stent (Cordis, Miami Lakes, FL) up to an 8 mm width was then advanced over the microwire into the Navien intermediate catheter across the stenosis. If a larger stent was required, the Navien would be removed and the stent would be placed through the Walrus BGC. The Navien or Walrus BGC was then pulled back and the stent was subsequently deployed. The Headway 27 was then advanced over the microwire and post-stenting venography and manometry were performed.
Device description and application
The Walrus BGC has an outer diameter of 0.110″ and an inner diameter of 0.087″. It can be inserted into most 8 French short sheaths and can accommodate the current generation of large bore catheters. The single-wall, variable stiffness construction of the Walrus optimizes distal flexibility without compromising proximal support. It is kink resistant for navigating challenging anatomy. The balloon measures up to a maximum of 11.1 mm.
The Walrus BGC has thin walls to allow the BGC to accommodate large and supportive tri-axial systems, including intermediate catheters such as a Navien 0.072″ . In addition, the large inner diameter gives the operator flexibility in choosing larger stent sizes, such as the 10 mm diameter Precise Pro Stent. The balloon can be inflated to orient the catheter tip towards the center of the lumen of the sinus to allow the catheter to navigate past tortuosity or obstructions within the sinus (Figure 1A). Figure 2 shows images from a case where navigating past the tortuous jugular-sigmoid sinus junction proved challenging, but successful navigation was achieved using balloon inflation. The Walrus BGC can be inflated to anchor the catheter against the rigid sinus walls to allow the intermediate catheter or stent to be more effectively pushed distally if little to no resistance is felt. This technique can be used in conjunction with the “Cobra” technique, which utilizes a smaller monorail sub maximally inflated balloon over a microwire at the tip of the intermediate catheter to decrease the ledge effect and allow for smoother distal navigation past stenoses, obstructions, or tortuous distal anatomy 9 (Figure 3). Figure 4 displays images from a case in which a patient underwent SSS stenting using this technique. Lastly, the large balloon of the Walrus BGC was successfully employed for angioplasty after stent deployment (Figure 1B). Figure 5 shows images from another case where transverse and sigmoid sinus stenting was performed, and angioplasty was used successfully to correct poor stent apposition.
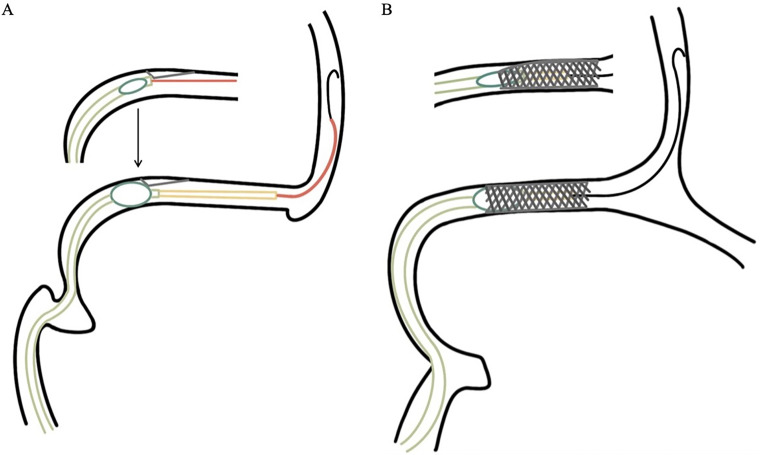
Illustrative depictions of the utility of the Walrus BGC balloon during VSS. The BGC and the intermediate catheter is depicted within the transverse sinus, the microcatheter and microwire in the SSS. (A)The balloon of the guide catheter can be inflated to center the catheter tip within the lumen of the sinus to track past an obstruction over the intermediate catheter. (B)The balloon of the guide catheter can be inflated to angioplasty the proximal or distal tines of the stent post-deployment to improve wall apposition.
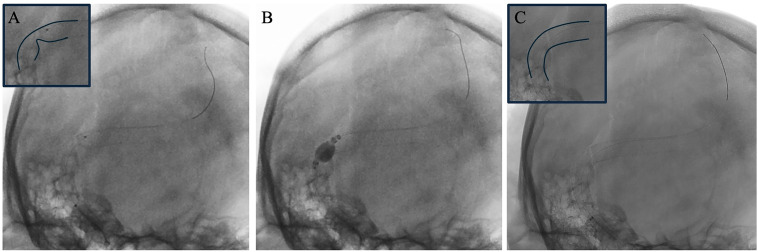
Case example of the utilization of the Walrus BGC balloon for stent angioplasty. (A) An unsubtracted image immediately after the deployment of a venous sinus stent from the transverse to sigmoid sinus showing poor stent wall apposition at the transverse to sigmoid junction. The malapposition is highlighted in the inset at the upper left corner. (B) The Walrus BGC balloon is seen inflated at the point of stent malapposition. (C) The post-angioplasty unsubtracted image is seen, which shows an improved opening of the stent. The improved wall apposition is highlighted in the inset at the top left corner.
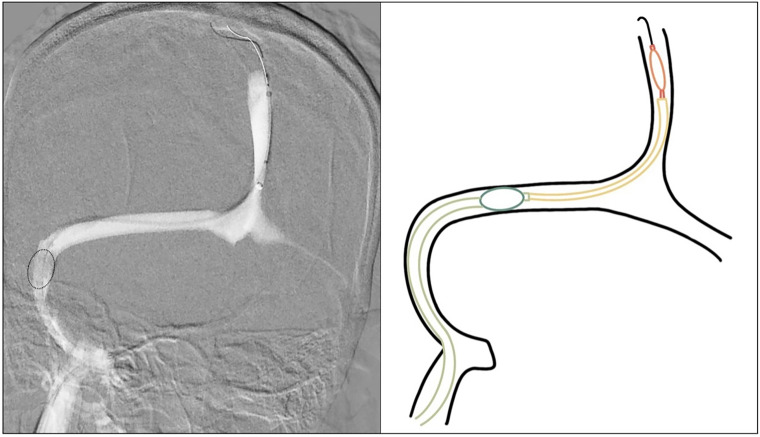
Illustrative depiction of the use of the anchoring technique in conjunction with the Cobra technique to achieve distal venous sinus access. On the left is a roadmap of the right superior sagittal, transverse, sigmoid, and jugular sinuses. To achieve distal access, the guide catheter balloon can be inflated at the transverse sigmoid junction to anchor it against the sinus walls. The balloon is outlined with a dotted line. A smaller monorail balloon can then be sub-maximally inflated over a microwire at the tip of the intermediate catheter to decrease the ledge effect and allow for smoother distal navigation of the intermediate catheter distally into the SSS. On the right is a corresponding graphical depiction with the BGC depicted within the transverse sinus, the intermediate catheter in the SSS, the balloon catheter and microwire in the SSS.
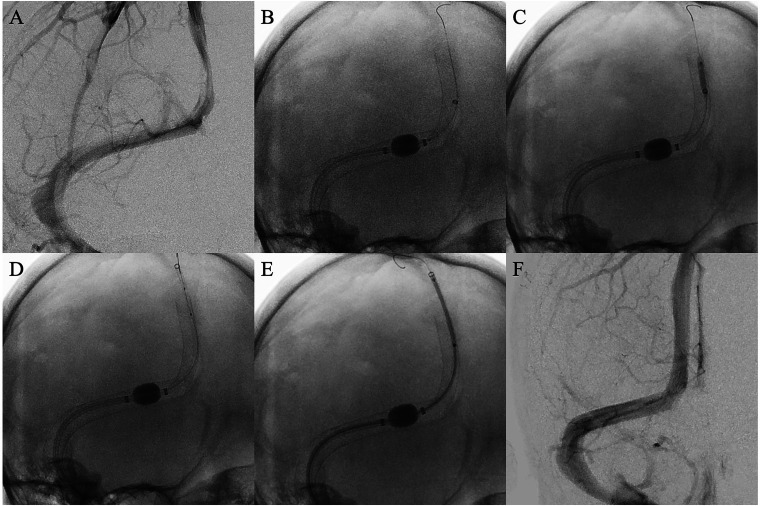
Case example of the utilization of the 90 cm Walrus BGC balloon for challenging distal SSS navigation. (A) A right common carotid artery injection demonstrating stenosis of the SSS and patent stents in the transverse and sigmoid sinuses. (B) Within the BGC is a 115 cm Navien 0.072″ intermediate catheter, which was unable to be navigated into the distal SSS for stent placement. An exchange length support microwire with an atraumatic J-shaped tip is seen in the SSS. The Walrus BGC in the distal transverse sinus is seen with the inflated balloon anchoring it into position as well as centering the catheter in the lumen preventing any ledge effect. (C) A non-compliant over-the-wire Emerge balloon 3 mm × 15 mm is placed at the distal tip of the intermediate catheter and inflated which decreases the ledge effect allowing for smooth navigation distally. (D) The intermediate catheter is now seen in position for stent placement in the SSS after utilizing the “Cobra” technique along with BGC balloon anchoring in the transverse sinus. (E) The Precise Pro stent is seen successfully navigated into appropriate final position prior to deployment. (F) A post-stent deployment right common carotid artery injection demonstrating improved stenosis of the SSS.
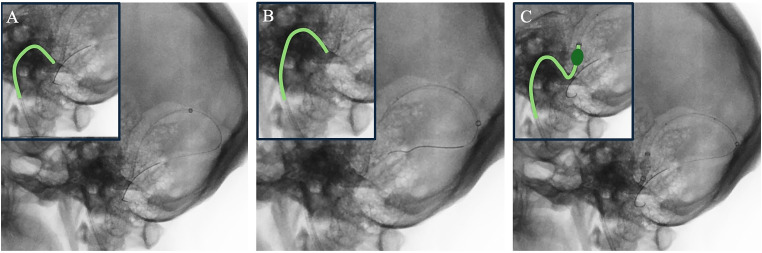
Case example of the utilization of the 90 cm Walrus BGC balloon for navigating past tortuous anatomy. (A) An unsubtracted lateral image shows a 115 cm Navien 0.072″ catheter, a Headway 27 microcatheter, and a Synchro 2 microwire with a J shape navigated past the turns of the jugular bulb with the Navien terminating in the transverse sinus. (B) The guide catheter is unable to pass through the jugular to sigmoid sinus junction and is instead herniating into the jugular bulb. This is despite ample distal wire purchase into the contralateral sigmoid sinus. The position of the guide catheter is highlighted in the inset at the upper left corner. (C) Ultimately, the Walrus was successfully navigated into the sigmoid sinus after submaximal inflation of the balloon of the BGC, which allowed the catheter to easily traverse the tortuous junction into the sigmoid sinus. Without inflation of the balloon, the catheter was unable to pass into the sigmoid sinus.
Results
Baseline characteristics
A total of 22 patients were included in the analysis (median age 35; 21 female). The indication for treatment was PT in 10 patients and IIH in 12 patients. All patients had imaging confirmed venous sinus stenosis with pressure gradients as measured by manometry.
Angiographic and clinical outcomes
Most stents were placed in the transverse sinus (20 patients) with only two being placed in the SSS sinus. The two patients who had SSS stents placed also had a prior stent placed in the dominant right transverse sinus (Table 1). The majority of patients had two stents placed (15 patients), while six patients had one stent placed, and one patient had three stents placed. The sizes of the stents placed ranged from 6 mm ×
× 30 mm to 10 mm
30 mm to 10 mm ×
× 40 mm, with the most common size being 7 mm
40 mm, with the most common size being 7 mm ×
× 40 mm (Table 1). The BGC was successfully navigated into the sigmoid or transverse sinuses allowing for the successful delivery of the stent in all cases. The BGC balloon was used 23 times for a combination of navigating past tortuosity or obstructions, angioplasty, and anchoring (Table 2). Angioplasty was successful in opposing the proximal tines of a deployed stent to the wall of the transverse sinus in three cases. These techniques were used in conjunction with the Cobra technique in three cases.
9
A 10 mm
40 mm (Table 1). The BGC was successfully navigated into the sigmoid or transverse sinuses allowing for the successful delivery of the stent in all cases. The BGC balloon was used 23 times for a combination of navigating past tortuosity or obstructions, angioplasty, and anchoring (Table 2). Angioplasty was successful in opposing the proximal tines of a deployed stent to the wall of the transverse sinus in three cases. These techniques were used in conjunction with the Cobra technique in three cases.
9
A 10 mm ×
× 40 mm stent was deployed in two cases. In the two cases of SSS stenting, the BGC balloon was inflated and used as an anchor to allow for distal navigation of the stent construct in conjunction with the Cobra technique.
9
There were no intraprocedural complications.
40 mm stent was deployed in two cases. In the two cases of SSS stenting, the BGC balloon was inflated and used as an anchor to allow for distal navigation of the stent construct in conjunction with the Cobra technique.
9
There were no intraprocedural complications.
Table 1.
Patient characteristics. PT =
= pulsatile tinnitus. IIH
pulsatile tinnitus. IIH =
= idiopathic intracranial hypertension. The average age of patients was 35.18 years with a range of 16 to 53 years. 95.5% of patients were female, 45.5% had PT, and 54.5% had IIH. 9.1% of patients had already underwent prior stenting. The frequencies for the location of stent deployment, number of stents deployed, size of stents used are listed as well.
idiopathic intracranial hypertension. The average age of patients was 35.18 years with a range of 16 to 53 years. 95.5% of patients were female, 45.5% had PT, and 54.5% had IIH. 9.1% of patients had already underwent prior stenting. The frequencies for the location of stent deployment, number of stents deployed, size of stents used are listed as well.
| Patient Characteristics | |
|---|---|
| Mean age in years (range) | 35.18 (16–53) |
| Females n (%) | 21 (95.5) |
| PT n (%) | 10 (45.5) |
| IIH n (%) | 12 (54.5) |
| Prior stent n (%) | 2 (9.1) |
| Right VSS n (%) | 14 (63.6) |
| Left VSS n (%) | 6 (27.3) |
| SSS VSS n (%) | 2 (9.1) |
| One stent n (%) | 6 (27.3) |
| Two stents n (%) | 15 (68.2) |
| Three stents n (%) | 1 (4.5) |
6 mm × × 30 mm n (%) 30 mm n (%) | 2 (9.1) |
8 mm × × 30 mm n (%) 30 mm n (%) | 4 (18.2) |
9 mm × × 30 mm n (%) 30 mm n (%) | 3 (13.6) |
6 mm × × 40 mm n (%) 40 mm n (%) | 6 (27.3) |
7 mm × × 40 mm n (%) 40 mm n (%) | 11 (50.0) |
8 mm × × 40 mm n (%) 40 mm n (%) | 7 (31.8) |
9 mm × × 40 mm n (%) 40 mm n (%) | 4 (18.2) |
10 mm × × 40 mm n (%) 40 mm n (%) | 2 (9.1) |
Table 2.
Utility of balloon inflation. The indication for balloon catheter use included navigation past tortuosity, anchoring, and angioplasty.
| Use for Balloon | Frequency n (%) |
|---|---|
| Navigation past tortuosity | 11 (48) |
| Anchoring | 9 (39) |
| Angioplasty | 3 (13) |
| Total | 23 |
Discussion
Venous sinus stenting is an effective and increasingly popular treatment method for patients suffering from IIH and PT.1–3,5–8,13 Strategic device selection to overcome the unique challenges of working within the venous sinuses is critical to maximizing safety and efficiency. Despite the rapid adoption of VSS by interventionalists, there is limited literature on device selection.2,13 We present the first case series describing the use of a BGC for VSS. In our series, radiographic and clinical outcomes were favorable, with successful stent deployment and no intraprocedural complications in all cases. The BGC was safely navigated into the sigmoid or transverse sinuses in all cases. In addition, we describe our VSS protocol as well as detail the advantages of utilizing a BGC in these cases.
The venous sinuses can have significant tortuosity, particularly at the junction of the jugular vein and the sigmoid sinus. The Walrus BGC's variable stiffness construction with distal flexibility and proximal support proved advantageous in navigating past this obstacle. Advancing the guide catheter into the sigmoid or transverse sinus can be challenging due to the variable tortuosity of the junction between the sigmoid sinus and the internal jugular vein. The atraumatic tip and trackability of the Walrus BGC allowed for safe navigation over an intermediate catheter. Placing the guide catheter beyond the jugular bulb into the sigmoid or transverse sinus offers stability and support during stent advancement and deployment, especially when using larger diameter stents. Therefore, easily navigating past the jugular bulb offers a major advantage in VSS procedures. The Walrus BGC also allowed for the delivery of large stents up to 10 mm. The strength of the Walrus BGC lies in its combination of characteristics, including its variable stiffness, distal flexibility, and proximal support, alongside the option for balloon inflation. While balloon inflation may be necessary in only a minority of cases, its availability as a strategy to overcome unique obstacles encountered in venous sinus stenting procedures sets BGCs apart.
The balloon of the BGC proved to be advantageous in several situations. In instances where the navigation past tortuosity proved difficult, we found that the submaximal inflation of the BGC allowed for redirection of the catheter tip and smooth passage of the catheter with less force than typically required with alternative guide catheters. The technical steps to successfully utilize this strategy include first advancing the exchange wire with an atraumatic J shaped tip and microcatheter into the SSS and the intermediate catheter into the transverse sinus if possible. Having the option of submaximally inflating the balloon of the BGC to navigate past tortuosity when the catheter is not advancing can save significant time by avoiding the need for an exchange of the entire system. In a similar light, venous sinuses may have intraluminal obstructions (chronic thrombosis, sizeable arachnoid granulations) or shelves that can block the path of a guide catheter. In cases where we reached an obstruction or tortuosity, submaximal inflation decreased the ledge effect, allowing for passage of the catheter. The balloon symmetrically inflates, displacing the tip of the catheter to the center of the sinus, thereby taking the tip of the catheter off the ledge or the wall of the sinus (Figure 1A). Figure 2 showcases an example case in which this technique was successful. We believe this technique can save the operator time and increase the safety of the procedure. In the infrequent situations where the interventionalist is meeting significant resistance to advancing the guide catheter, the option of sub maximal inflation of the balloon offers a safe and dependable alternative to excessive force or opting for a system exchange.
In cases of significant tortuosity or in cases of SSS stenting, significant force can be required to push the stenting system distally. We found that inflating the BGC balloon with apposition to the transverse or sigmoid sinus wall (i.e., full inflation) anchored the BGC in place, which decreased the force needed to push the stenting construct distally and allowed for the successful crossing of the stenosis (Figure 2). This technique was used in conjunction with the Cobra technique, which utilizes a small submaximally inflated non-compliant over-the-wire balloon placed at the lumen of the intermediate catheter to decrease the ledge effect to navigate distally with less force (Figure 2).
9
The system needed to use this strategy includes an exchange wire with an atraumatic J shaped tip in the SSS, a non-compliant over-the-wire balloon (3 mm ×
× 15 mm Emerge, Boston Scientific, Marlborough, MA) placed at the distal tip of the intermediate catheter, and the BGC in the transverse or sigmoid sinus. The BGC is inflated until it is immobilized against the walls of the sinus. The over-the-wire balloon is then submaximally inflated at the tip of the intermediate catheter to decrease any ledge that may be present at the tip. Forward pressure can then be applied on the intermediate catheter over the exchange wire so that it may advance past the stenosis. The use of a proximal balloon anchor to successfully cross stenoses in challenging anatomy has also been described in the cardiac literature for the coronary arteries and in the vascular literature for renal artery stenoses.14,15 The use of the balloon in these situations decreased the force required to push the system forward; therefore, we feel it increases the safety of the procedure. An integral aspect of this technique involves establishing an atraumatic distal system, comprising an intermediate catheter devoid of any ledges and a soft, J-shaped distal microwire tip. This configuration works by stabilizing the system and ensures that the force exerted by the operator is more effectively transmitted to the distal system. In scenarios where the distal system lacks atraumatic features, is not situated within the true lumen of the sinus, and resistance is encountered, employing this technique can pose significant risks. Figure 4 includes representative images from a case in which this technique was utilized. Lastly, we were able to use the BGC balloon for successful post-stenting angioplasty. (Figure 1B). While the balloon for the Walrus BGC is semicompliant and not the ideal angioplasty device, it remains an option due to its immediate availability, ease of positioning after stent deployment, and the flexible, non-rigid properties of the stent requiring angioplasty. Despite its semicompliant construction, we found it to be effective. An example case in which angioplasty utilizing the BGC was successful is seen in Figure 5. We acknowledge that this limited experience using the BGC as an angioplasty device is not evidence of its definitive safety and effectiveness, but we aim to highlight another unique advantage in the setting of VSS. Whether BGCs can definitively be used for effective post-stenting angioplasty remains to be seen with future studies.
15 mm Emerge, Boston Scientific, Marlborough, MA) placed at the distal tip of the intermediate catheter, and the BGC in the transverse or sigmoid sinus. The BGC is inflated until it is immobilized against the walls of the sinus. The over-the-wire balloon is then submaximally inflated at the tip of the intermediate catheter to decrease any ledge that may be present at the tip. Forward pressure can then be applied on the intermediate catheter over the exchange wire so that it may advance past the stenosis. The use of a proximal balloon anchor to successfully cross stenoses in challenging anatomy has also been described in the cardiac literature for the coronary arteries and in the vascular literature for renal artery stenoses.14,15 The use of the balloon in these situations decreased the force required to push the system forward; therefore, we feel it increases the safety of the procedure. An integral aspect of this technique involves establishing an atraumatic distal system, comprising an intermediate catheter devoid of any ledges and a soft, J-shaped distal microwire tip. This configuration works by stabilizing the system and ensures that the force exerted by the operator is more effectively transmitted to the distal system. In scenarios where the distal system lacks atraumatic features, is not situated within the true lumen of the sinus, and resistance is encountered, employing this technique can pose significant risks. Figure 4 includes representative images from a case in which this technique was utilized. Lastly, we were able to use the BGC balloon for successful post-stenting angioplasty. (Figure 1B). While the balloon for the Walrus BGC is semicompliant and not the ideal angioplasty device, it remains an option due to its immediate availability, ease of positioning after stent deployment, and the flexible, non-rigid properties of the stent requiring angioplasty. Despite its semicompliant construction, we found it to be effective. An example case in which angioplasty utilizing the BGC was successful is seen in Figure 5. We acknowledge that this limited experience using the BGC as an angioplasty device is not evidence of its definitive safety and effectiveness, but we aim to highlight another unique advantage in the setting of VSS. Whether BGCs can definitively be used for effective post-stenting angioplasty remains to be seen with future studies.
In our series, there were no intraprocedural complications. Our series had a lower complication rate when compared to the reported major complication rate of 1%–6% in the VSS literature.1,3,6–8 Major complications in VSS can be attributed to excessive use of force against resistance in a subset of cases. 7 We found that the use of the BGC balloon in cases where significant resistance was met decreased the force needed to navigate past obstacles. We believe the lower complication rate in this series can be attributed to our experience, which has informed nuances of our technique and device selection.
While there are no data on the use of BGCs in VSS, there is substantial existing literature in support of using BGCs for carotid stenting and acute ischemic stroke interventions.16–18 The WICkED study (Walrus Large Bore Guide Catheter Impact on Recanalization First Pass Effect and Outcomes), which analyzed the use of the Walrus BGC in 338 patients undergoing mechanical thrombectomy for large vessel occlusions, found that the device-related complication rate was 0.6%. In 71.9% of cases, a large bore aspiration catheter was used. In addition, they found that the device was successfully navigated to the target vasculature in all but three cases (0.9%). 17 These data points highlight the characteristics of the BGC, such as the large inner diameter and its ability to navigate tortuosity, which is advantageous in acute stroke but can also be applied to VSS.
Limitations and future directions
Limitations of this study include its retrospective design, small sample size, and the lack of a comparison group. Future studies should include more patients and compare clinical and radiographic outcomes of patients who undergo VSS with BGCs as compared to other guide catheters. Furthermore, manufacturers of future catheters created specifically for VSS should consider these described advantages to the BGC and can improve upon the characteristics to tailor it for use in the venous system.
Conclusion
In a small series of patients, the use of BGC in VSS is safe and feasible. BGCs possess distinctive features that effectively address the specific challenges encountered in VSS, making them advantageous in select scenarios.
Acknowledgments
We would like to acknowledge Robert Ferrara for his integral support throughout the process.
Footnotes
All authors have contributed to, read, and approved of the manuscript and its submission for publication.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The institutional review board approved this retrospective study (#23-0711-NSUH).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Justin Turpin https://orcid.org/0000-0002-3686-2695
Daniel Toscano https://orcid.org/0000-0002-1805-4416
Jared B. Bassett https://orcid.org/0000-0002-9379-8677
Kevin A. Shah https://orcid.org/0000-0003-0896-2266
Timothy G. White https://orcid.org/0000-0002-3604-4334
References
Articles from Interventional Neuroradiology are provided here courtesy of SAGE Publications
Citations & impact
This article has not been cited yet.
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/169439752
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Resolution of Pulsatile Tinnitus after Venous Sinus Stenting in Patients with Idiopathic Intracranial Hypertension.
PLoS One, 11(10):e0164466, 21 Oct 2016
Cited by: 19 articles | PMID: 27768690 | PMCID: PMC5074492
Challenges in the use of Venous Sinus Stenting in the Treatment of Idiopathic Intracranial Hypertension and Pulsatile Tinnitus.
World Neurosurg, 184:372-386, 01 Apr 2024
Cited by: 0 articles | PMID: 38590071
Safety and Clinical Outcomes after Transverse Venous Sinus Stenting for Treatment of Refractory Idiopathic Intracranial Hypertension: Single Center Experience.
J Vasc Interv Neurol, 11(1):6-12, 01 Jan 2020
Cited by: 5 articles | PMID: 32071666 | PMCID: PMC6998806
Occipital venous sinus stenting for idiopathic intracranial hypertension and pulsatile tinnitus: A case series.
Interv Neuroradiol, 15910199241245451, 07 May 2024
Cited by: 0 articles | PMID: 38715430 | PMCID: PMC11559819
Review Free full text in Europe PMC
 1
1 


