Abstract
Background
Patients with COVID-19 or post-COVID-19 will most probably have a need for rehabilitation during and directly after the hospitalisation. Data on safety and efficacy are lacking. Healthcare professionals cannot wait for published randomised controlled trials before they can start these rehabilitative interventions in daily clinical practice, as the number of post-COVID-19 patients increases rapidly. The Convergence of Opinion on Recommendations and Evidence process was used to make interim recommendation for the rehabilitation in the hospital and post-hospital phase in COVID-19 and post-COVID-19 patients, respectively.Methods
93 experts were asked to fill out 13 multiple choice questions. Agreement of directionality was tabulated for each question. At least 70% agreement on directionality was necessary to make consensus suggestions.Results
76 experts (82%) reached consensus on all questions based upon indirect evidence and clinical experience on the need for early rehabilitation during the hospital admission, the screening for treatable traits with rehabilitation in all patients at discharge and 6-8 weeks after discharge, and around the content of rehabilitation for these patients. It advocates for assessment of oxygen needs at discharge and more comprehensive assessment of rehabilitation needs including physical as well as mental aspects 6-8 weeks after discharge. Based on the deficits identified multidisciplinary rehabilitation should be offered with attention for skeletal muscle and functional as well as mental restoration.Conclusions
This multinational task force recommends early, bedside rehabilitation for patients affected by severe COVID-19. The model of pulmonary rehabilitation may suit as a framework, particularly in a subset of patients with long term respiratory consequences.Free full text

COVID-19: interim guidance on rehabilitation in the hospital and post-hospital phase from a European Respiratory Society- and American Thoracic Society-coordinated international task force
Abstract
Background
Patients with coronavirus disease 2019 (COVID-19) or post-COVID-19 will probably have a need for rehabilitation during and directly after the hospitalisation. Data on safety and efficacy are lacking. Healthcare professionals cannot wait for published randomised controlled trials before they can start these rehabilitative interventions in daily clinical practice, as the number of post-COVID-19 patients increases rapidly. The Convergence of Opinion on Recommendations and Evidence process was used to make interim recommendations for rehabilitation in the hospital and post-hospital phases in COVID-19 and post-COVID-19 patients, respectively.
Methods
93 experts were asked to fill out 13 multiple-choice questions. Agreement of directionality was tabulated for each question. ≥70% agreement on directionality was necessary to make consensus suggestions.
Results
76 (82%) experts reached consensus on all questions based upon indirect evidence and clinical experience on the need for early rehabilitation during the hospital admission, the screening for treatable traits with rehabilitation in all patients at discharge and 6–8 weeks after discharge, and around the content of rehabilitation for these patients. It advocates for assessment of oxygen needs at discharge and more comprehensive assessment of rehabilitation needs, including physical as well as mental aspects 6–8 weeks after discharge. Based on the deficits identified, multidisciplinary rehabilitation should be offered with attention on skeletal muscle and functional as well as mental restoration.
Conclusions
This multinational task force recommends early, bedside rehabilitation for patients affected by severe COVID-19. The model of pulmonary rehabilitation may suit as a framework, particularly in a subset of patients with long-term respiratory consequences.
Short abstract
Experts recommend identification of unmet rehabilitation needs in patients with COVID-19 who are discharged from the hospital, and consequent tailored rehabilitative interventions, accompanied by compliance with the highest biosecurity standards https://bit.ly/3geBsPE
Introduction
Globally, millions of people are infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing coronavirus disease 2019 (COVID-19) [1]. A proportion of the confirmed COVID-19 patients are admitted to the hospital for acute care, due to severe respiratory symptoms and in some cases even acute respiratory distress requiring prolonged mechanical ventilation [2].
It is very likely that a proportion of the COVID-19 patients will have a need for rehabilitative interventions during and directly after the hospitalisation [3–6]. This approach is recommended by the World Health Organization [7]. However, data on safety and efficacy of rehabilitation during and/or after hospitalisation in these patients are lacking. Equally, healthcare professionals cannot wait for well-designed randomised controlled trials to be published before they can start these rehabilitative interventions in daily clinical practice, as the number of COVID-19 patients increases rapidly every day.
Recently, Wilson et al. [8] used the Convergence of Opinion on Recommendations and Evidence (CORE) process to make recommendations for the management of COVID-19. The CORE process is a consensus-based approach to making clinical recommendations that has been shown to yield recommendations that are concordant with recommendations developed using Institute of Medicine-adherent methodology [9]. The same methodology was used to develop interim guidance on rehabilitative interventions in the hospital and post-hospital phase in COVID-19 patients pending empirical evidence.
Methods
An ad hoc international task force was assembled, including the European Respiratory Society (ERS) and American Thoracic Society (ATS) key opinion leaders as well as key opinion leaders and clinical experts from other relevant societies in the field of pulmonary rehabilitation. Invitations were sent to 93 experts within the field of pulmonary rehabilitation, respiratory and critical care medicine of physical medicine and rehabilitation. 76 (82%) agreed to participate. As described before [8], the SurveyMonkey platform (SurveryMonkey, San Mateo, CA, USA) was used to create a 13-question multiple-choice survey. Each question consisted of three parts: 1) presentation of the question in a modified PICO (patient, intervention, comparator, outcomes) format; 2) a multiple-choice question asking for strong or conditional recommendation for or against a course of action or no recommendation; and 3) a free-text box for comments.
After publishing an initial web-based blog on April 3, 2020 and seeking global input [10], the core team of experts (MA Spruit, AE Holland, SJ Singh, T Troosters) put together a list of possible relevant questions, and during three teleconferences, consensus was reached about which question to maintain. Wording of the questions was adapted with input of ERS and ATS methodology teams to ensure unequivocal interpretation and consistency. The survey was not piloted in order to have more timely recommendations.
The survey was administered once from April 27 to May 11, 2020, including several reminders. Agreement of directionality was tabulated for each multiple-choice question. ≥70% agreement on directionality was necessary to make consensus suggestions. The proportion of respondents per choice per question was calculated and expressed as a percentage of the total number of respondents. As >70% agreement on directionality was reached in all questions from the first round, no second round was necessary.
Results
The international task force suggests that hospitalised patients with COVID-19 should receive rehabilitation at/around the bedside (critical care and/or ward based) until safe for discharge to the home environment
Rationale
While most people infected with the COVID-19 virus have mild disease [11], some have more severe symptoms requiring hospital admission, and 20% of those admitted may require intensive care [12]. Hospitalised COVID-19 patients often have comorbidities, such as cardiovascular disease and diabetes [13] and may have prolonged hospital stays [14]. Some COVID-19 survivors have physical impairments that may be exacerbated by prolonged immobility, including muscle weakness, neurological impairment and/or nutritional disturbance [15]. In-hospital rehabilitation could effectively address these problems [16]. However, there may be added challenges for rehabilitation delivery in the setting of COVID-19, related to infection prevention and changes to availability of existing rehabilitation services.
Results
The majority of the experts recommended strongly (55%) or conditionally (37%) for hospitalised patients with COVID-19 receiving rehabilitation at/around the bedside (critical care and/or ward based) until safe discharge to the home environment (figure 1a and table 1).
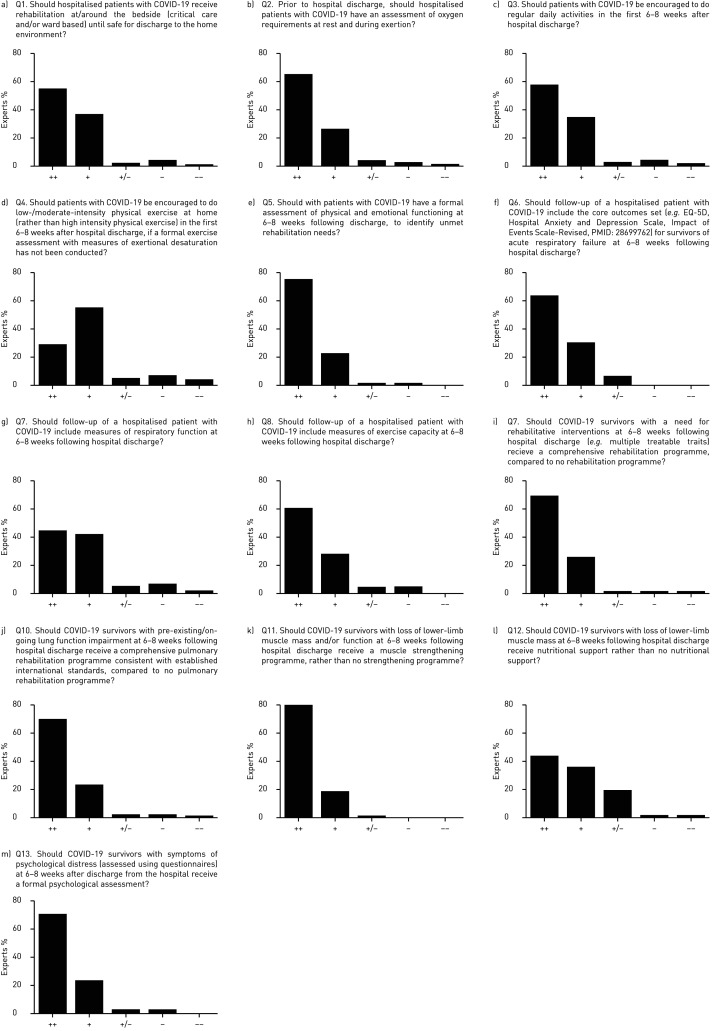
Experts’ responses to the 13 questions. COVID-19: coronavirus disease 2019; ++: strong recommendation for; +: conditional recommendation for; +/−: no recommendation for or against; −: conditional recommendation against; −−: strong recommendation against.
TABLE 1
Interim recommendations
|
COVID-19: coronavirus disease 2019.
Experts commented that patient-tailored early rehabilitative interventions similar to other critically ill patients should start after an assessment, including early mobilisation and airway clearance. This may prevent and/or slow down the expected rapid deterioration in physical and emotional functioning. Some experts did express concerns about patients’ safety, due to the limited understanding of underlying pathophysiology and the possible impact of rehabilitative interventions. For example, it is unclear if there is any “threshold of illness severity” or any particular features of illness, which pose greater risk of patients undertaking rehabilitative interventions during hospitalisation, including pulmonary, cardiovascular and/or neurological manifestations of COVID-19 infection, in particular, the risk of clotting (microthrombosis and venous thromboembolism). Moreover, the importance of appropriate personal protective equipment (PPE) for the healthcare professional was mentioned by multiple experts as a clear safety issue.
The international task force suggests that prior to hospital discharge, hospitalised patients with COVID-19 should have an assessment of oxygen requirements at rest and during exertion
Rationale
Hypoxaemia is common in hospitalised patients with COVID-19, with hypoxic respiratory failure a prominent feature of severe cases [17]. While supplemental oxygen requirements reduce over time, alongside improvements in the underlying lung pathology [18], it is likely that some patients will have ongoing oxygen needs at hospital discharge. Moreover, some patients in the recovery phase may have oxygen desaturation on exertion, which is not associated with resting oxygen saturation, the degree of dyspnoea or feeling unwell.
Results
A majority of the experts recommended strongly (66%) or conditionally (26%) for hospitalised patients with COVID-19 having an assessment of oxygen requirements at rest and during exertion prior to hospital discharge (figure 1b).
Experts commented that assessment of oxygen requirements during exertion may vary between hospitals. However, low oxygen saturation may be a reason for additional assessment for pulmonary and cardiovascular comorbidities. Moreover, some patients do show a severe oxygen desaturation during physical exercise of only moderate intensity. Assessment of oxygen requirement prior to hospital discharge is necessary to prepare the individual COVID-19 patient with the needed equipment upon discharge home. A follow-up assessment on the re-evaluation of oxygen requirement should also be scheduled following hospital discharge, as supplemental oxygen may no longer be needed as the underlying lung pathology resolves.
The international task force suggests that patients with COVID-19 should be encouraged to do regular daily activities in the first 6–8 weeks after hospital discharge
Rationale
Some patients with COVID-19 will resume daily activities without difficulty in the period following hospitalisation, but this may be more challenging in those who have had severe disease, prolonged hospital stays and/or persistent symptoms [19]. Approximately two-thirds of the survivors of other critical illnesses experience moderate-to-good recovery of physical function over the first 2 months [20]. However, recovery trajectories vary, with ongoing impairments most likely in older patients with longer intensive care unit (ICU) stays and greater sedation time [20].
Results
A majority of the experts recommended strongly (58%) or conditionally (34%) for encouraging patients with COVID-19 to do regular daily activities in the first 6–8 weeks after hospital discharge (figure 1c).
Experts commented that recommencing daily physical activity as early as possible may positively affect functional recovery. However, patients may vary in physical, emotional and/or cognitive functioning, so further assessment should be performed. Moreover, the encouragement to do regular daily activities should be in line with the local regulations for physical distancing and should go along with advice to take time for recovery and rest periods, and taking an acceptable level of perceived exertion and dyspnoea and oxygen desaturation into consideration.
The international task force suggests that patients with COVID-19 should be encouraged to do low-/moderate-intensity physical exercise at home (rather than high-intensity physical exercise) in the first 6–8 weeks after hospital discharge, if a formal exercise assessment with measures of exertional desaturation has not been conducted
Rationale
COVID-19 infection is associated with a high inflammatory burden [21], which could persist beyond hospital discharge. Exertional desaturation may also persist, even in those without the requirement for supplemental oxygen at rest. While moderate-intensity exercise training is safe and feasible in survivors of critical illness [22], the safety of high-intensity exercise in patients recovering from COVID-19 is unknown. During the early post-hospital period it may not always be possible to conduct a robust exercise assessment or deliver supervised rehabilitation services, with uncertainties regarding the duration of time that patients remain infectious [23] and/or the need to maintain physical distancing.
Results
A majority of the experts recommended strongly (29%) or conditionally (55%) for encouraging patients with COVID-19 to do low-/moderate-intensity physical exercise at home (rather than high-intensity physical exercise) in the first 6–8 weeks after hospital discharge, if a formal exercise assessment with measures of exertional desaturation has not been conducted (figure 1d).
Some experts stated that the potential benefits of low-/moderate-physical activity in preventing physical deterioration outweighed any perceived risks of undertaking such exercise without formal assessment. The low-/moderate-intensity physical exercises should be based on symptom limitation and tailored to the individual needs and limitations of the patients, which may vary greatly. In addition to oxygen desaturation on exertion, experts encouraged health professionals to be aware of other possible causes of caution, such as cardiomyopathy and (post-)pulmonary embolism.
The international task force suggests that patients with COVID-19 should have a formal assessment of physical and emotional functioning at 6–8 weeks following discharge, to identify unmet rehabilitation needs
Rationale
While good recovery of physical function should be expected over the first 8 weeks in most COVID-19 survivors, it is highly likely that there will be some with ongoing impairments in physical functioning [20]. The high prevalence of post-traumatic stress disorder (PTSD), cognitive impairment, chronic pain, sleep disorders, fibromyalgia and fatigue in survivors of critical illness have been well documented [24–26]. The COVID-19 pandemic gives rise to new psychosocial and emotional stressors for recovering patients, including social isolation, physical distancing, loss of employment and uncertainties about the future.
Results
A majority of the experts recommended strongly (75%) or conditionally (22%) for patients with COVID-19 having a formal assessment of physical and emotional functioning at 6–8 weeks following discharge (figure 1e).
Experts stated that post-hospitalisation recovery may vary considerably between patients, which justifies a formal assessment (including physical, emotional and cognitive functioning and return to work) to customise rehabilitation care. In addition, some experts proposed an evaluation at hospital discharge to ensure that patients were discharged to the appropriate setting (e.g. home, rehabilitation centre, nursing home), and for formal assessment only in symptomatic patients with limitations in daily functioning.
The international task force suggests that follow-up of a hospitalised patient with COVID-19 should include the core outcomes set for survivors of acute respiratory failure at 6–8 weeks following hospital discharge
Rationale
Post-hospital outcomes of COVID-19 survivors are not yet understood. Assessment of physical and psychosocial outcomes following hospitalisation for COVID-19 will allow unmet rehabilitation needs to be addressed. A core outcome set allows essential outcomes to be consistently assessed using the same measurement instruments, so that data can be pooled and confident conclusions drawn. A core outcome set for survivors of acute respiratory failure has already been defined using a consensus process, and includes the EQ-5D, Hospital Anxiety and Depression Scale and Impact of Events Scale – Revised [27]. The core outcome set does not include measures of cognition, muscle function, physical function or pulmonary function.
Results
A majority of the experts recommended strongly (63%) or conditionally (30%) for the follow-up of a hospitalised patient with COVID-19 including the core outcomes set for survivors of acute respiratory failure at 6–8 weeks following hospital discharge (figure 1f)
Experts recognised the importance of administering outcome measures that will help to identify the patients’ need in order to direct, plan and devise appropriate interventions and resources to the patients and their caregivers. This may require multiple re-assessments at different time points (e.g. 3, 6 and 12 months after hospital discharge). Individual experts suggested the addition of a tool to measure exertional breathlessness (e.g. the Medical Research Council dyspnoea grading scale) and cognitive screening (Montreal Cognitive Assessment) and alternative tools to assess the same domains as identified by Needham et al. [27] (e.g. Short-Form 36 to assess generic health status; the primary care PTSD questionnaire to assess symptoms of PTSD; Patient Health Questionnaire 9, General Anxiety Disorder 7 or the Depression Anxiety Stress Scale 21 to assess symptoms of anxiety and/or depression). Some experts believed that assessment at 6–8 weeks following hospital discharge is too soon, as some sequelae may manifest at later time points. Moreover, some experts indicted that community-managed patients may also need a supported recovery programme.
The international task force suggests that follow-up of a hospitalised patient with COVID-19 should include measures of respiratory function at 6–8 weeks following hospital discharge
Rationale
High-resolution computed tomography scans of the chest in patients with COVID-19 infection have shown significant respiratory abnormalities including ground-glass opacities, inter- and intra-lobular septal thickening and consolidation. These changes start to resolve after 14 days, but may persist past hospital discharge [18]. Long-term follow-up of survivors of other severe viral pneumonias (SARS-CoV-1 and Middle East respiratory syndrome (MERS)-CoV) suggests that many had normal respiratory function at 1 year, although impaired diffusing capacity was evident in a minority [28, 29]. Respiratory function testing is necessary to document ongoing impairments and guide future management, but it is considered an aerosol-generating procedure, which may limit its availability in the COVID-19 era.
Results
A majority of the experts recommended strongly (45%) or conditionally (42%) for the follow-up of a hospitalised patient with COVID-19 including measures of respiratory function at 6–8 weeks following hospital discharge (figure 1g).
Experts recognised the importance of measuring respiratory function, as missing respiratory abnormalities are likely to lead to further decline, and perhaps downstream, new respiratory chronic disease. Experts emphasised the need to perform assessment only in patients with lingering respiratory symptoms and who were tested COVID-negative in the post-hospitalisation phase. Indeed, standard operating procedures need to be in place to prevent possible infection of other patients and/or the lung-function technician. Some experts questioned whether local infection control protocols would allow measurements of respiratory function to be obtained.
The international task force suggests that follow-up of a hospitalised patient with COVID-19 should include measures of exercise capacity at 6–8 weeks following hospital discharge
Rationale
While the long-term consequences of COVID-19 are not fully understood, we know that the impact of an ICU stay for acute respiratory distress syndrome (ARDS) has a significant impact on physical function [30]. Equally, a protracted period of bed rest can have similar detrimental but partially reversible effects in chronic respiratory disease [31]. There is some evidence that recovery in physical function is variable in ARDS survivors; however, the greatest recovery appeared to occur within the first 2 months [20]. An objective measure of exercise capacity [31] is important to document the degree of disability, identify the limitations to exercise and form the foundation of a subsequent rehabilitation programme.
Results
A majority of the experts recommended strongly (61%) or conditionally (29%) for the follow-up of a hospitalised patient with COVID-19 including measures of exercise capacity at 6–8 weeks following hospital discharge (figure 1h).
Many experts considered the measurement of exercise capacity to be very important in COVID-19 survivors, but some experts believe that this measurement should be limited to patients who remain physically limited 6–8 weeks following hospital discharge and who are tested negative at the time testing the exercise capacity. Experts emphasised that assessors should be aware of the possible presence of cardiopulmonary sequelae. Some experts questioned whether local infection control protocols would allow measurements of exercise capacity to be obtained.
The international task force suggests that COVID-19 survivors with a need for rehabilitative interventions at 6–8 weeks following hospital discharge (e.g. multiple treatable traits) should receive a comprehensive rehabilitation programme, compared to no rehabilitation programme
Rationale
Existing data from survivors of viral pneumonias indicates the wide range of challenges that patients face [20, 24, 25]. It is unlikely that a unidimensional programme of physical training will meet the needs of COVID-19 survivors as they will exhibit multiple treatable traits that a comprehensive rehabilitation programme has the potential to modify favourably. There is a limited evidence base for pulmonary rehabilitation post-H1N1-ARDS [32]. The programme will potentially be wider in scope than current pulmonary rehabilitation programmes [33] to meet the needs of these individuals and consider the additional burden placed upon survivors as a consequence of this unique virus, e.g. social isolation strategies and the associated emotional burden. Survivors may be of a different age group to the “usual” pulmonary rehabilitation population and supporting a successful return to work will be important.
Results
A majority of the experts recommended strongly (70%) or conditionally (26%) for COVID-19 survivors with a need for rehabilitative interventions at 6–8 weeks following hospital discharge receiving a comprehensive rehabilitation programme (figure 1i).
Many experts commented on the diverse needs of COVID-19 survivors, such that not all survivors will need a comprehensive programme. Some experts commented that a comprehensive rehabilitation programme may not be available in all locations during the COVID-19 pandemic.
The international task force suggests that COVID-19 survivors with pre-existing/ongoing lung function impairment at 6–8 weeks following hospital discharge should receive a comprehensive pulmonary rehabilitation programme consistent with established international standards, compared to no pulmonary rehabilitation programme
Rationale
For patients with COPD there is evidence to indicate that recovery after an admission is supported by a structured rehabilitation programme. We know that this is both safe and clinically effective and is recommended in national and international guidelines [33, 34]. The current guidance for routine post-exacerbation pulmonary rehabilitation is 4 weeks post-discharge; however, the recommendation to delay this until 6–8 weeks post-discharge was based upon the following considerations: there is a lack of data about the decay of the levels of infection in the COVID-19 survivor; the data suggest that at 2 months a proportion of physical recovery will have occurred [20]; and we know that is a challenge for services to recruit patients to a post-exacerbation rehabilitation programme 4 weeks post-discharge [35].
Results
A majority of the experts recommended strongly (70%) or conditionally (24%) for COVID-19 survivors with pre-existing/ongoing lung function impairment at 6–8 weeks following hospital discharge receiving a comprehensive pulmonary rehabilitation programme consistent with established international standards (figure 1j).
Experts recommended taking patient's individual needs and preferences into consideration when decisions regarding comprehensive pulmonary rehabilitation programmes are made.
The international task force suggests that COVID-19 survivors with loss of lower-limb muscle mass and/or function at 6–8 weeks following hospital discharge should receive a muscle-strengthening programme, rather than no strengthening programme
Rationale
For patients with ARDS, prolonged stay in the ICU (mostly including prolonged mechanical ventilation) is known to have significant impact on peripheral muscle function, reflected in a loss of muscle mass and power neuropathy and/or myopathy, better known as ICU-acquired muscle weakness [30], and occurs early on in the ICU stay [36]. Equally, a prolonged period of bed rest can also have a significant effect in chronic respiratory disease [31]. The lack of peripheral muscle strength can severely compromise functional ability and should be evaluated and treated as indicated [33].
Results
A majority of the experts recommended strongly (80%) or conditionally (18%) for COVID-19 survivors with loss of lower limb muscle mass and/or function at 6–8 weeks following hospital discharge receiving a muscle strengthening programme (figure 1k).
Experts agreed that a muscle strengthening programme was important to optimise recovery. Moreover, muscle strength needs to be assessed prior to commencement, to enable accurate prescription and tailoring of the strengthening programme.
The international task force suggests that COVID-19 survivors with loss of lower-limb muscle mass at 6–8 weeks following hospital discharge should receive nutritional support rather than no nutritional support
Rationale
It is well established that optimising caloric and protein intake is important to support recovery of functional muscle mass. The post-ICU COVID-19 survivor will face commonly reported problems with nutrition (e.g. loss of appetite, swallowing disorders), and the additional symptoms of loss of taste (ageusia) and smell (anosmia) are now recognised symptoms of COVID-19 [37]. In general, for those with chronic respiratory disease, weight loss and wasting of muscle and bone tissue may be induced or accelerated during severe acute exacerbations of respiratory disease requiring hospitalisation, due to the combination of malnutrition, physical inactivity, hypoxia, systemic inflammation and/or systemic glucocorticoids [38]; this is likely to be mirrored in the COVID patient.
Results
A majority of the experts recommended strongly (43%) or conditionally (36%) for COVID-19 survivors with loss of lower-limb muscle mass at 6–8 weeks following hospital discharge receiving nutritional support (figure 1l).
Experts stated that rebuilding muscle mass requires that nutritional support be combined with a training stimulus. Moreover, experts believed that nutritional support may be less well established in some centres and guidance may be needed from expert sources.
The international task force suggests that COVID-19 survivors with symptoms of psychological distress (assessed using questionnaires) at 6–8 weeks after discharge from the hospital should receive a formal psychological assessment
Rationale
Common symptoms reported 1 year later by ICU survivors, including patient with ARDS, include anxiety (34%), depression (33%) and PTSD (19%) [39]. This is compounded for the post-COVID-19 survivor by the emotional stress associated with social isolation from family and friends for a protracted period of time as a consequence of government lockdown policies. There are questionnaires recommended in the core outcome dataset that cover these aspects of anxiety and depression, alongside PTSD [27]. In addition, it is acknowledged that the emotional burden of COVID-19 is likely to extend beyond the individual to family and friends [40].
Results
A majority of the experts recommended strongly (71%) or conditionally (24%) for COVID-19 survivors with symptoms of psychological distress at 6–8 weeks after discharge from the hospital receiving a formal psychological assessment (figure 1m).
Experts believed that symptoms of anxiety, depression and PTSD occur commonly in persons after a major life event. Therefore, screening and monitoring of the course of symptoms of psychological distress is important. Experts also emphasised that those patients who show high levels of anxiety or depressive symptoms need to be referred to psychologist or psychiatrist for further assessment, and treatment may be indicated when symptoms continue to exist after 10–12 weeks. Psychological assessment and support for the family of the infected patient was also emphasised by the experts.
Discussion
The present study provides consensus-based suggestions for the screening and the rehabilitation process during and after a hospital admission for severe COVID-19 infection. Experts reached consensus based upon indirect evidence and nonsystematic clinical observations (i.e. clinical experience) on the need for early rehabilitation during the hospital admission, the screening for treatable traits with rehabilitation in all patients at discharge and 6–8 weeks after discharge, and around the content of rehabilitation for these patients. In absence of a formal evidence-based approach, these findings provide interim guidance for referral and multidisciplinary rehabilitation in a subgroup of patients after hospital admission. Altogether, the data cast a strong claim on the need for screening and rehabilitation options for patients who have been hospitalised. Besides lung function testing (e.g. spirometry, whole-body plethysmography and carbon monoxide transfer factor) [41, 42], this screening should also contain at least an exercise test (cardiopulmonary exercise test, 6-min walk test or shuttle walk test), muscle strength testing and patient-reported outcome measures [19, 43–46]. This cannot be ignored by healthcare systems organising the care around this pandemic respiratory infection. It should be noted that several experts identified that during the pandemic there has been an absence of rehabilitation options for patients who suffered from COVID-19.
Early mobilisation and re-engagement in physical activity is important in the prevention of systemic consequences of a critical care and hospital admission. Whenever possible, patients should re-engage in physical exercise tailored to their possibilities. In patients suffering from COVID-19, such early interventions have to be balanced with the critical illness of the patient and the availability of PPE for caregivers engaged in the early mobilisation protocols [5, 6, 47]. Where rehabilitation staff are not available or cannot access PPE, some rehabilitation tasks at the bedside may be provided by other members of the multidisciplinary team, with appropriate instruction. At discharge from hospital, experts advise a first screening, particularly to investigate the need for oxygen supplementation, in order to guide the first weeks post-discharge. Patients may still be infectious [48, 49], which may complicate testing outside the patient's room. A 1-min sit-to-stand test has been proposed as a way to evaluate hypoxia on exertion in the patient's room as an alternative to a 6-min walk test [50], but needs further validation.
After discharge, patients with COVID-19 should be encouraged to do low-/moderate-intensity physical exercise at home in the first 6–8 weeks. Usually, these tasks range between 1.5 and 6 metabolic equivalents; Ainsworth and co-workers [51, 52] describe numerous examples.
Moreover, the guidance provided by the ATS/ERS statement on pulmonary rehabilitation [33] may serve as a good framework. In this statement, pulmonary rehabilitation is defined as “…a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies, which include, but are not limited to, exercise training, education, and behaviour change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence of health-enhancing behaviours”. Experts seem to agree that this definition also applies to patients who have suffered severe COVID-19. Clearly there is a need for physiological (statements 2, 5, 7, 8 and 11), psychological (statements 5, 6 and 13) and nutritional (statement 13) assessment. For some patients there is a need for an individually tailored rehabilitation intervention (statement 9) and in the case of a pre-existing of remaining respiratory deficit, a pulmonary rehabilitation programme (statement 10). Pulmonary rehabilitation programmes are indeed well equipped to service this group of patients. Adaptations may need to be made to the rehabilitation programme if the programme typically deals with patients with obstructive lung disease, to cater more to patients with gas-exchange abnormalities. The self-management or education modules may also need to be adapted. It is expected that many patients who have suffered from severe COVID-19, and particularly those with an ICU admission, will have significant skeletal muscle weakness. Following muscle strength testing [46], specific skeletal muscle training programmes, typically offered with resistance training, are advised by experts. This is also the case in conventional pulmonary rehabilitation [53].
To date, no prospective studies exist in COVID-19 patients on the proportion of patients in need of some form of (multidisciplinary) rehabilitation. However, symptoms like fatigue and dyspnoea still occur frequently ~30 days after discharge from the hospital, and are accompanied by reduced quality of life in ~40% of COVID-19 patients [19]. In some cases, the programme offered could be outside the pulmonary rehabilitation setting. Indeed, early studies from China and confirmed later [54] indicated that >30% of patients suffered from some neurological and neuromuscular sequelae [55]. It is yet unknown how much of this recovers spontaneously. The progression of functional, skeletal muscle and mental health status after an admission for COVID-19 is not yet well described. Nevertheless, observational studies after SARS [56] or MERS [57] report an impaired 6-min walk distance in 18% of the patients, and 43.6% had psychological comorbidity. Hence, healthcare systems need to prepare to accommodate an increased number of referrals.
The exact proportion of COVID-19 patients requiring rehabilitation is difficult to predict, but assuming that patients who received mechanical ventilation would be a minimum set of patients that require rehabilitation post-discharge may provide a conservative estimate of the number of new rehabilitation cases. Taking the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC), UK-based database as an example, 10% of hospitalised patients required mechanical ventilation [58]. In a United States (New York)-based cohort, 23% of patients required mechanical ventilation [59]. Unfortunately, large proportions died in the ICU (e.g. up to 60% in a study from New York, and similar numbers in the ISARIC cohort), still rendering 40% of patients admitted to ICU as minimal numbers of new candidates for multidisciplinary rehabilitation, representing 5–10% of patients referred to hospital. It is likely that a fraction of patients not mechanically ventilated (including patients on high-flow oxygen therapy) will need to be added, as some of these still have significant functional consequences of the hospital admission ([60]; M Paneroni, Respiratory Rehabilitation of the Institute of Lumezzane, Instituti Clinici Scientifici Maugeri IRCCS, Lumezzane, Italy; personal communication). We strongly encourage countries to take action to organise rehabilitation for this influx of patients, in addition to the many patients with chronic respiratory disease who already qualify for pulmonary rehabilitation [61].
An issue that is unresolved, but of importance to the organisation of rehabilitation for these patients, is the duration for which patients should be considered infectious. There is currently no consensus on how long patients should be self-isolating. Local infection prevention recommendations should be followed and this may require significant adaptation of the rehabilitation programme with, for example, the adoption of “tele-rehabilitation” [62]. The task force has adopted a 6–8-week time window for reassessment. At this time point (and probably even sooner) many patients will be considered noninfectious [48, 49, 63].
A last point of attention is that despite the robust opinion in favour of rehabilitation after severe COVID-19 disease, these patients may be difficult to reach. Unfortunately, several factors may preclude referral or uptake of rehabilitation. An important element that may impair uptake of rehabilitation is that at a population level, rehabilitation might be hampered by pre-infection risk factors for admission to hospital with COVID-19, which include obesity, smoking and living an inactive lifestyle [64]. Moreover, it is known that COVID-19 disproportionately affects disadvantaged communities [65], many of whom have poor access to rehabilitation [66]. These factors are known to impair uptake of rehabilitation. Therefore, the offer of rehabilitation must be made to patients in a personalised and targeted manner, to maximise the likelihood of acceptance.
Strengths and weaknesses
While the present expert opinion article followed rigorous methodology to reach consensus, and consensus was reached on all questions, some remarks need to be taken into account. It would be good to offer respondents the option of no response, as respondents may feel that they do not have adequate expertise to respond to a question or they may not understand the question wording. Indeed, some experts stated that there were composite questions, combining a question about the content of care with a question about timing. Moreover, sometimes questions may not have been very specific (e.g. “measures of respiratory function”, “measures of exercise capacity”, “comprehensive pulmonary rehabilitation programme” or “nutritional support”). See supplementary table S1 for all details. This may complicate interpretation of survey responses. Where possible, we have taken written comments of the respondents into account.
The current methodology also has strengths. It is fast and provides an interim guidance when randomised controlled studies are not yet available. Moreover, the current sample experts came from all over the world and had a diverse professional background, including but not limited to medical specialists, physiotherapists, nurses and psychologists.
Conclusion
This multinational task force recommends early bedside rehabilitation for patients affected by severe COVID-19. It advocates for assessment of oxygen needs at discharge and more comprehensive assessment of rehabilitation needs including physical as well as mental aspects 6–8 weeks after discharge. Based on the deficits identified multidisciplinary rehabilitation should be offered with attention for skeletal muscle and functional as well as mental restoration. The model of pulmonary rehabilitation may suit as a framework, particularly in a subset of patients with pre-existing or COVID-19-induced long-term respiratory consequences.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
All comments by the members of the expert panel ERJ-02197-2020.Table_S1
List of participating experts ERJ-02197-2020.Table_S2
Shareable PDF
Acknowledgements
The authors would like to thank Alessandra Marguerat (European Respiratory Society, Lausanne, Switzerland) for her logistical support. Moreover, they would like to acknowledge the experts (supplementary table S2) for their time and input.
Footnotes
This article has an editorial commentary: https://doi.org/10.1183/13993003.02889-2020
This article has supplementary material available from erj.ersjournals.com
The goal of consensus guidance is to standardise care, thereby improving outcomes and facilitating research. The suggestions in this document do not constitute official positions of the American Thoracic Society, European Respiratory Society, or the institutions of the task force members. They should not be considered mandates as no suggestion can incorporate all potential clinical circumstances. The suggestions are interim guidance that should be re-evaluated as evidence accumulates.
Conflict of interest: M.A. Spruit reports grants from Netherlands Lung Foundation and Stichting Astma Bestrijding, grants and personal fees from AstraZeneca and Boehringer Ingeheim, outside the submitted work.
Conflict of interest: A.E. Holland has nothing to disclose.
Conflict of interest: S.J. Singh has nothing to disclose.
Conflict of interest: T. Tonia acts as an ERS methodologist.
Conflict of interest: K.C. Wilson reports other possible conflicts of interest as ATS Chief of Guidelines and Documents, and as developer of the CORE process, outside the submitted work.
Conflict of interest: T. Troosters has nothing to disclose.
References
Full text links
Read article at publisher's site: https://doi.org/10.1183/13993003.02197-2020
Read article for free, from open access legal sources, via Unpaywall:
https://erj.ersjournals.com/content/erj/56/6/2002197.full.pdf
Citations & impact
Impact metrics
Article citations
Understanding hospital rehabilitation using electronic health records in patients with and without COVID-19.
BMC Health Serv Res, 24(1):1245, 17 Oct 2024
Cited by: 0 articles | PMID: 39415208 | PMCID: PMC11484221
Clinical practice guidelines and expert consensus statements on rehabilitation for patients with COVID-19: a systematic review.
BMJ Open, 14(9):e086301, 10 Sep 2024
Cited by: 0 articles | PMID: 39260851 | PMCID: PMC11409320
Review Free full text in Europe PMC
Effectiveness of post-COVID-19 primary care attendance in improving survival in very old patients with multimorbidity: a territory-wide target trial emulation.
Fam Med Community Health, 12(3):e002834, 14 Jul 2024
Cited by: 0 articles | PMID: 39004436 | PMCID: PMC11253766
Long-term oxygen therapy to reduce length of hospital stay in COVID-19.
Rev Assoc Med Bras (1992), 70(7):e20231379, 19 Jul 2024
Cited by: 0 articles | PMID: 39045926 | PMCID: PMC11262311
Post-COVID conditions response: a collaborative approach to -establishing multidisciplinary clinics in Ecuador.
Multidiscip Respir Med, 19, 01 Jul 2024
Cited by: 0 articles | PMID: 38953789 | PMCID: PMC11229825
Go to all (178) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Updated guidance on the management of COVID-19: from an American Thoracic Society/European Respiratory Society coordinated International Task Force (29 July 2020).
Eur Respir Rev, 29(157):200287, 01 Sep 2020
Cited by: 67 articles | PMID: 33020069 | PMCID: PMC7537943
Review Free full text in Europe PMC
Therapeutic respiratory and functional rehabilitation protocol for intensive care unit patients affected by COVID-19: a structured summary of a study protocol for a randomised controlled trial.
Trials, 22(1):268, 12 Apr 2021
Cited by: 2 articles | PMID: 33845878 | PMCID: PMC8039799
[Standard technical specifications for methacholine chloride (Methacholine) bronchial challenge test (2023)].
Zhonghua Jie He He Hu Xi Za Zhi, 47(2):101-119, 01 Feb 2024
Cited by: 0 articles | PMID: 38309959
Testing the efficacy and safety of BIO101, for the prevention of respiratory deterioration, in patients with COVID-19 pneumonia (COVA study): a structured summary of a study protocol for a randomised controlled trial.
Trials, 22(1):42, 11 Jan 2021
Cited by: 11 articles | PMID: 33430924 | PMCID: PMC7797700





