Abstract
Purpose
The purpose of this trial was to evaluate the role of radiation therapy with concurrent gemcitabine (GEM) compared with GEM alone in patients with localized unresectable pancreatic cancer.Patients and methods
Patients with localized unresectable adenocarcinoma of the pancreas were randomly assigned to receive GEM alone (at 1,000 mg/m(2)/wk for weeks 1 to 6, followed by 1 week rest, then for 3 of 4 weeks) or GEM (600 mg/m(2)/wk for weeks 1 to 5, then 4 weeks later 1,000 mg/m(2) for 3 of 4 weeks) plus radiotherapy (starting on day 1, 1.8 Gy/Fx for total of 50.4 Gy). Measurement of quality of life using the Functional Assessment of Cancer Therapy-Hepatobiliary questionnaire was also performed.Results
Of 74 patients entered on trial and randomly assigned to receive GEM alone (arm A; n = 37) or GEM plus radiation (arm B; n = 34), patients in arm B had greater incidence of grades 4 and 5 toxicities (41% v 9%), but grades 3 and 4 toxicities combined were similar (77% in A v 79% in B). No statistical differences were seen in quality of life measurements at 6, 15 to 16, and 36 weeks. The primary end point was survival, which was 9.2 months (95% CI, 7.9 to 11.4 months) and 11.1 months (95% CI, 7.6 to 15.5 months) for arms A and B, respectively (one-sided P = .017 by stratified log-rank test).Conclusion
This trial demonstrates improved overall survival with the addition of radiation therapy to GEM in patients with localized unresectable pancreatic cancer, with acceptable toxicity.Free full text

Gemcitabine Alone Versus Gemcitabine Plus Radiotherapy in Patients With Locally Advanced Pancreatic Cancer: An Eastern Cooperative Oncology Group Trial
Abstract
Purpose
The purpose of this trial was to evaluate the role of radiation therapy with concurrent gemcitabine (GEM) compared with GEM alone in patients with localized unresectable pancreatic cancer.
Patients and Methods
Patients with localized unresectable adenocarcinoma of the pancreas were randomly assigned to receive GEM alone (at 1,000 mg/m2/wk for weeks 1 to 6, followed by 1 week rest, then for 3 of 4 weeks) or GEM (600 mg/m2/wk for weeks 1 to 5, then 4 weeks later 1,000 mg/m2 for 3 of 4 weeks) plus radiotherapy (starting on day 1, 1.8 Gy/Fx for total of 50.4 Gy). Measurement of quality of life using the Functional Assessment of Cancer Therapy–Hepatobiliary questionnaire was also performed.
Results
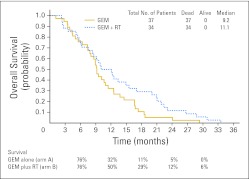
Of 74 patients entered on trial and randomly assigned to receive GEM alone (arm A; n = 37) or GEM plus radiation (arm B; n = 34), patients in arm B had greater incidence of grades 4 and 5 toxicities (41% v 9%), but grades 3 and 4 toxicities combined were similar (77% in A v 79% in B). No statistical differences were seen in quality of life measurements at 6, 15 to 16, and 36 weeks. The primary end point was survival, which was 9.2 months (95% CI, 7.9 to 11.4 months) and 11.1 months (95% CI, 7.6 to 15.5 months) for arms A and B, respectively (one-sided P = .017 by stratified log-rank test).
Conclusion
This trial demonstrates improved overall survival with the addition of radiation therapy to GEM in patients with localized unresectable pancreatic cancer, with acceptable toxicity.
INTRODUCTION
In the United States, adenocarcinoma of the pancreas represents the fourth leading cause of death resulting from cancer.1 For patients with locally unresectable disease, systemic therapy with or without radiotherapy has been a standard of care over the past several decades, with median survival of 6 to 9 months and less than 10% surviving beyond 2 years.2 Surprisingly, a paucity of prospective randomized trials have evaluated the impact of combined-modality therapy in locally advanced disease.
Two decades ago, the Gastrointestinal Tumor Study Group conducted a trial in locally advanced pancreatic cancer in which patients were randomly assigned to receive radiation alone (60 Gy) or radiation (60 or 40 Gy) plus fluorouracil (FU). Both combined-modality arms were superior to radiation alone (median survival, 10 v 6 months). Several years later, the Eastern Cooperative Oncology Group (ECOG) randomly assigned patients with locally advanced pancreatic and gastric cancers to receive FU alone with or without involved field radiotherapy. No improvement in local progression or progression-free (PFS) or overall survival (OS) was noted.3
Combined-modality therapy has not universally produced improved outcome. The European Society for Pancreatic Adenocarcinoma reported worse survival for resected patients receiving radiation compared with those who did not receive radiotherapy.4 The Fédération Francophone de Cancérologie Digestive and Société Française de Radiothérapie Oncologique compared gemcitabine alone with an experimental chemoradiotherapy regimen (cisplatin plus high-dosage FU) followed by gemcitabine also demonstrated worse outcome with chemoradiotherapy (8.6 v 13 months; P = .03).5 Median OS in the gemcitabine-alone arm (13 months) was unusual for patients with locally advanced disease, as reported in other randomized trials. In neither trial was gemcitabine used with concurrent radiotherapy.
Because gemcitabine is superior to FU in patients with symptomatic advanced pancreatic cancer, the substitution of gemcitabine with concurrent radiotherapy has been evaluated in several phase I and II trials.6–16 One multi-institutional phase I trial demonstrated that weekly bolus gemcitabine (600 mg/m2) was safe to administer with concurrent radiation (total dose, 50.4 Gy), which was later confirmed through the Hoosier Oncology Group.17 This intergroup trial was subsequently initiated to determine whether radiation improves survival or provides additional benefit (ie, response rate, quality of life [QOL]) compared with gemcitabine alone in patients with locally advanced pancreatic cancer.
PATIENTS AND METHODS
Patient Selection
Eligibility included cytologic or histologic evidence of locally unresectable adenocarcinoma of the pancreas, not amenable for complete surgical resection based on clinical or radiographic evaluation (laparoscopy was not required). Patients with small-cell carcinoma, mucinous cystadenocarcinoma, or islet cell or papillary cystic neoplasm were not eligible. Patients must also have been at least 18 years of age, had an ECOG performance score of 0 to 2, and received no prior chemotherapy or radiotherapy. Eligible patients had an absolute granulocyte count of 2.0 × 109/μL or greater, platelet count greater than 100,000/μL, total bilirubin of less than 3 mg/dL (unless secondary to biliary obstruction or cholangitis), AST less than 5× upper limit of normal, albumin greater than 2.5 g/dL, and serum creatinine 1.5× or less than upper limit of normal. Patients were not eligible if they had a history of active collagen vascular disease or signs of recent peptic or duodenal ulcer (eg, < 3 months). Other contradictions included serious concomitant systemic disorders or active infections. Women of childbearing potential had to have had a negative pregnancy test within 2 weeks of study entry and were strongly encouraged to use effective methods of contraception. All patients provided written informed consent before initiation of therapy. This was an intergroup study lead by the ECOG through the National Cancer Institute. No industry support was involved in the conduct of the study or analysis.
Treatment
After registration, patients were stratified by performance status (0 v 1) and prior weight loss within previous 6 months (< 10% v ≥ 10%) and randomly assigned to receive gemcitabine alone (arm A) or gemcitabine plus radiotherapy (arm B). Patients in arm A received gemcitabine 1,000 mg/m2 intravenously (over approximately 30 minutes) per week for 6 weeks, followed by a 1-week rest. After the week of rest, treatment was resumed at 1,000 mg/m2 weekly for 3 weeks, followed by 1 week rest, for five additional 4-week cycles. All dosages of gemcitabine were based on calculated body-surface area, using actual height and weight.
Patients in arm B received gemcitabine 600 mg/m2 intravenously (over 30 to 60 minutes) beginning on the first day of radiation therapy (before radiation), then weekly thereafter during radiation. The radiation dose was 1.8 Gy per daily fraction, 5 days per week, for a total dose of 50.4 Gy administered in 28 fractions over 5.5 weeks, with a required field reduction after 39.6 Gy. Three-dimensional (3D) treatment planning (with conformal radiotherapy capabilities) was highly encouraged. A 3D benchmark was to be completed and submitted to the Quality Assurance Review Center, which conducted two separate reviews: a rapid review (at initiation of radiation) and final review (at completion of radiation). Intensity modulated radiation therapy was not permitted in this study. Patients underwent computed tomography (CT) simulation. The initial large fields, designed to encompass the planning target volume, received 39.6 Gy in 22 fractions. This included the gross target volume (GTV; defined by CT scan and/or surgically placed clips) plus a 3-cm margin but had to be less than 400 cm2 in anterior-posterior to posterior-anterior projection. In addition, the local/regional lymph nodes adjacent to the GTV were included, with at least a 1.5-cm margin, primarily the peripancreatic and pancreatoduodenal defined by the duodenal loop, celiac nodes, porta hepatis, and nodes around the superior mesenteric vessels. Smaller margins were allowed to accommodate normal tissue dose requirements, providing target coverage was adequate.
As part of the 3D treatment planning, surrounding normal tissues including liver, each kidney separately, and spinal cord were reconstructed, and dose-volume histograms for those critical structures were submitted for review. The small or boost fields encompassing the planning target volume included the GTV with a 2-cm margin and received an additional 10.8 Gy delivered in six fractions at 1.8 Gy per fraction. Approximately 4 weeks after completion of radiation, gemcitabine was resumed at full dosage (arm A) for a total of five cycles.
Patient Evaluation
History was taken and physical examination performed before initiation of therapy, at week 6, and then at day 1 of each cycle of gemcitabine. Patients were deemed unresectable after surgical consultation based on presence of superior mesenteric vein or portal vein occlusion, superior mesenteric artery or hepatic artery encasement, gross regional lymphadenopathy, or metastatic disease. Abdominal CT scan for tumor evaluation was performed before study entry, at week 8, and within 4 weeks of chemotherapy completion. Other scans were to be performed as warranted by symptoms of clinical progression or to document response (> 4 weeks after first response noted). During therapy, hematologic parameters and chemistries were collected weekly along with height, weight, and performance status. Chemistries were repeated monthly during therapy. Patient-reported health-related QOL (HRQOL) was assessed using the Functional Assessment of Cancer Therapy–Hepatobiliary (FACT-Hep) questionnaire, which includes 27 items to assess physical, functional, emotional, and social well-being and 18 items to assess hepatobiliary-specific concerns.18 The FACT-Hep was administered at baseline, week 6, week 15 or 16, and 9 months after baseline, even if therapy had been discontinued.
For all patients experiencing grade 3 or 4 toxicities (except grade 3 nausea/vomiting), one dose level was decreased, as listed in Table 1. If patients experienced grade 3 or 4 febrile neutropenia (≥ 38.3°C), gemcitabine was delayed until ANC was 1,000 μL or greater, and when restarted, gemcitabine was reduced by one level (Table 1). If either ANC was less than 1,000/mm2 or platelets were less than 50,000, gemcitabine was delayed until resolution and reinstituted at one dose level reduction. Dose reductions based on nonhematologic toxicities (such as nausea and/or vomiting) applied to the remainder of treatment. If gemcitabine was delayed because of grade 4 nonhematologic toxicity, it could be resumed at one dose level reduction once the toxicity improved to less than grade 2. Doses held back because of toxicity would not be administered at a later time. If toxicity did not resolve to less than grade 2 within 2 weeks or if more than two dose reductions of gemcitabine were required, the patient's protocol treatment was to be discontinued.
Table 1.
Gemcitabine Dose Levels
| Dose Level | Gemcitabine Dose (mg/m2) | |
|---|---|---|
| Arms A and B (consolidation) | Arm B (with radiation) | |
| 0 | 1,000 | 600 |
| −1 | 800 | 480 |
| −2 | 600 | 380 |
| −3 | Treatment discontinued | Treatment discontinued |
Statistical Analysis
The primary end point of this trial was OS in patients treated with gemcitabine alone versus gemcitabine plus radiation therapy. Secondary objectives included objective response rate as per RECIST (Response Evaluation Criteria in Solid Tumors), PFS, toxicity, and HRQOL.
The proposed sample size of 316 eligible patients was planned to provide at least 88% power to detect a 50% difference in median survival while maintaining a significance level of 2.5% in a one-sided log-rank test, assuming exponential failure and median survival of 8 months with gemcitabine alone and 12 months with gemcitabine and radiation. The one-sided test was prespecified in the design phase of the study to evaluate the main objective to test whether combined-modality therapy improved survival. Interim evaluations of the study were planned at 25%, 50%, and 75% of mortalities as well as the final analysis. Group sequential methods based on an O'Brien-Fleming and DeMets approach were also employed to adjust the boundaries if the actual interim analyses did not correspond with the projected information times provided in the design.12,13
This study was monitored for early stopping in favor of the null hypothesis using repeated CI methodology similar to that described by Jennison et al.19 At each interim analysis, the nominal (1 to 2 × alpha) CI on the OS hazard ratio comparing the gemcitabine alone arm with the gemcitabine plus radiation therapy arm was computed, where alpha was the nominal one-sided significance level of the use-function boundary at the information fraction for the particular analysis time. If the CI did not contain the target alternative of 1.50, then the data monitoring committee would consider closing an arm of the trial or stopping the study early for overall lack of treatment differences.
HRQOL was assessed using the 45-item FACT-Hep, administered at baseline, week 6, week 15 or 16, and 9 months postbaseline. FACT-Hep total scores were calculated to obtain a total measure of HRQOL including hepatobiliary symptoms. The FACT-Hep subscale score was calculated to indicate disease-specific concerns. Subscales from the FACT were calculated to assess physical and functional well-being. The trial outcome index was calculated by summing the FACT physical well-being, functional well-being, and hepatobiliary subscale scores to provide a more focused assessment of HRQOL, disease symptoms, and functional status. FACT-Hep scoring was performed according to manual instructions (http://www.facit.org).14 Standard descriptive and graphical analyses were used initially to explore unusual observations, missing data patterns, and the relationship between variables. At each time point, QOL of two treatment groups and QOL change from baseline were compared using the Wilcoxon two-sample tests with a two-sided significance level of .05. Nine individual items from the FACT-Hep were selected to examine the proportion of participants with clinically significant symptoms.
RESULTS
Patient Characteristics
From April 2003 to December 2005, 74 patients were enrolled onto the trial. In December 2005, the data monitoring committee terminated accrual to the study because of the poor accrual rate (ie, < 10 entries per month). Three patients (one, arm A; two, arm B) were deemed ineligible because of metastatic disease at presentation. All eligible patients were evaluable for survival. Patient characteristics are listed in Table 2.
Table 2.
Baseline Characteristics of Eligible Patients
| Characteristic | Total | Arm A (gemcitabine) | Arm B (gemcitabine + radiation) | P | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| No. of patients | 71 | 37 | 34 | ||||
| Age, years | .48* | ||||||
    Mean Mean | 66.2 | 67.0 | 65.34 | ||||
    SD SD | 9.5 | 8.7 | 10.3 | ||||
    Median Median | 68 | 69 | 66 | ||||
    Range Range | 46.9-83.7 | 49.7-83.7 | 46.9-83.5 | ||||
    < 67.5 < 67.5 | 35 | 49.3 | 16 | 43.2 | 19 | 55.9 | .29† |
    > 67.5 > 67.5 | 36 | 50.7 | 21 | 56.8 | 15 | 44.1 | |
| Sex | .54† | ||||||
    Male Male | 37 | 52.1 | 18 | 48.6 | 19 | 55.9 | |
    Female Female | 34 | 47.9 | 19 | 51.4 | 15 | 44.1 | |
| ECOG performance status | .49† | ||||||
    0 0 | 15 | 21.1 | 9 | 24.3 | 6 | 17.6 | |
    1 1 | 56 | 78.9 | 28 | 75.7 | 28 | 82.4 | |
| Race | .32† | ||||||
    Non-Hispanic white Non-Hispanic white | 65 | 91.5 | 35 | 94.6 | 30 | 88.2 | |
    Non-Hispanic black Non-Hispanic black | 4 | 5.6 | 2 | 5.4 | 2 | 5.9 | |
    Other Other | 2 | 2.8 | 0 | 0 | 2 | 5.9 | |
| Weight loss, % of body weight | .75† | ||||||
    < 10 < 10 | 39 | 54.9 | 21 | 56.8 | 18 | 52.9 | |
    ≥ 10 ≥ 10 | 32 | 45.1 | 16 | 43.2 | 16 | 47.1 | |
| Pathology | .36†‡ | ||||||
    Carcinoma NOS Carcinoma NOS | 35 | 49.3 | 22 | 59.5 | 13 | 38.2 | |
    Well differentiated Well differentiated | 10 | 14.1 | 4 | 10.8 | 6 | 17.6 | |
    Moderately differentiated Moderately differentiated | 14 | 19.7 | 6 | 16.2 | 8 | 23.5 | |
    Poorly differentiated Poorly differentiated | 12 | 16.9 | 5 | 13.5 | 7 | 20.6 | |
| Location of primary tumor | .71† | ||||||
    Head of pancreas Head of pancreas | 45 | 63.4 | 25 | 67.6 | 20 | 58.8 | |
    Body of pancreas Body of pancreas | 9 | 12.7 | 3 | 8.1 | 6 | 17.6 | |
    Tail of pancreas Tail of pancreas | 5 | 7.0 | 2 | 5.4 | 3 | 8.8 | |
    Uncinate process Uncinate process | 8 | 11.3 | 4 | 10.8 | 4 | 11.8 | |
    Pancreas NOS Pancreas NOS | 1 | 1.4 | 1 | 2.7 | 0 | 0 | |
    Other (includes > one primary site) Other (includes > one primary site) | 3 | 4.2 | 2 | 5.4 | 1 | 2.9 | |
Abbreviations: ECOG, Eastern Cooperative Oncology Group; NOS, not otherwise specified; SD, standard deviation.
Outcome Measures
Toxicity.
Sixty-nine patients (35, arm A; 34, arm B) were evaluated for toxicity. Two patients in arm A were not evaluable for toxicity. Grade 3 or greater hematologic and nonhematologic adverse events are outlined in Table 3. The most frequently reported toxicities were fatigue and GI toxicities (although discrimination from disease-related symptoms was frequently not possible). Occurrence of grade 3 elevation of transaminases or alkaline phosphatase was less than 5% in both arms. Overall grades 3 and 4 toxicities were common in both arms (77% v 79%; P = 1.0, Fisher's exact test), but as expected, grades 4 and 5 toxicities were greater in arm B (41%) versus arm A (9%). One grade 5 toxicity occurred in each arm (arm A, cardiac; arm B, acute respiratory distress syndrome).
Table 3.
Toxicity Summary
| Toxicity Type | Treatment Arm (grade) | |||||
|---|---|---|---|---|---|---|
| A (n = 35) | B (n = 34) | |||||
| 3 | 4 | 5 | 3 | 4 | 5 | |
| Hemoglobin | 2 | — | — | 3 | 3 | — |
| Leukocytes | 5 | — | — | 8 | 3 | — |
| Lymphopenia | — | — | — | 1 | — | — |
| Neutrophils | 11 | 1 | — | 9 | 4 | — |
| Platelets | 2 | — | — | 5 | 2 | — |
| Transfusion | ||||||
    Platelets Platelets | — | — | — | 1 | — | — |
    PRBCS PRBCS | 2 | — | — | 6 | — | — |
| Cardiac ischemia | — | — | 1 | — | — | — |
| Edema | 1 | — | — | — | — | — |
| Hypotension | 1 | — | — | 1 | 1 | — |
| Thrombosis/embolism | 1 | — | — | — | — | — |
| Fatigue | 2 | — | — | 8 | 3 | — |
| Weight loss | — | — | — | 2 | — | — |
| Rash/desquamation | — | — | — | 1 | — | — |
| Constitutional | — | — | 1 | — | — | — |
| Anorexia | 1 | — | — | 6 | — | — |
| Ascites | 1 | — | — | — | — | — |
| Colitis | 1 | — | — | — | — | — |
| Dehydration | — | — | — | 2 | — | — |
| Nausea | 3 | — | — | 8 | 2 | — |
| Vomiting | 3 | — | — | 7 | 2 | — |
| Diarrhea without prior colostomy | 1 | — | — | 2 | — | — |
| Melena/GI bleeding | — | — | — | 2 | — | — |
| Infection with grade 3 or 4 neutropenia | 1 | — | — | — | 1 | — |
| Alkaline phosphatase | 1 | — | — | 2 | — | — |
| Bilirubin | 1 | — | — | 1 | — | — |
| GGT | 1 | — | — | — | — | — |
| Hypoalbuminemia | — | — | — | 3 | — | — |
| Asparitate transaminase | 1 | — | — | — | — | — |
| Alanine transaminase | 1 | — | — | 1 | — | — |
| Infection with grade 3 or 4 neutropenia | 1 | — | — | — | 1 | — |
| Infection with unknown ANC | 1 | — | — | — | — | — |
| Infection without neutropenia | 2 | — | — | 1 | — | — |
| Hyperglycemia | 1 | — | — | — | — | — |
| Hypocalcemia | — | — | — | 1 | 1 | — |
| Hypokalemia | 2 | — | — | 2 | 2 | — |
| Muscle weakness | — | — | — | 1 | — | — |
| Abdominal pain | — | — | — | 1 | 1 | — |
| ARDS | — | — | — | — | — | 1 |
| Apnea | — | 1 | — | — | — | — |
| Pulmonary (other) | — | 1 | — | — | — | — |
| Worst degree | 25 | 2 | 1 | 14 | 13 | 1 |
Abbreviations: ARDS, acute respiratory distress syndrome; GGT, gamma-glutamul transpeptidase; PRBCS, packed red blood cells.
HRQOL
As shown in Table 4, a Wilcoxon two-sample test indicated statistically significant decline in HRQOL among participants in both treatment arms from baseline to week 6 on FACT-Hep total scores (P = .02) and on individual components of the FACT-Hep, including hepatobiliary-specific symptoms (P = .04) and physical (P = .01) and functional (P = .01) well-being. No statistically significant differences were observed between treatment arms from baseline comparison beyond week 6. Using Fisher's exact test to evaluate treatment arm differences on individual items, a significantly higher proportion of participants in arm B reported appetite problems, abdominal swelling or cramps, and bother by treatment adverse effects at week 6 (P < .05). HRQOL findings must be interpreted with caution given attrition at follow-up, as indicated in Table 4.
Table 4.
HRQOL Score Differences Between Treatment Arms and Changes During and After Treatment
| HRQOL Measure* | Arm A | Arm B | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Week 6 | Week 15 or 16 | 9 Months | Baseline | Week 6 | Week 15 or 16 | 9 Months | |||||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Trial outcome index | ||||||||||||||||
    Mean Mean | 86.0 | 84.3 | 90.0 | 86.0 | 89.7 | 75.8 | 90.4 | 92.4 | ||||||||
    SD SD | 19.0 | 17.9* | 17.7 | 18.9 | 16.1 | 23.4* | 18.6 | 16.6 | ||||||||
| FACT-Hep total score | ||||||||||||||||
    Mean Mean | 124.3 | 124.1 | 130.9 | 126.4 | 130.2 | 116.9 | 132.7 | 133.8 | ||||||||
    SD SD | 23.8 | 24.6* | 21.3 | 26.2 | 19.9 | 27.1* | 24.0 | 20.9 | ||||||||
| Hepatibiliary cancer subscale | ||||||||||||||||
    Mean Mean | 50.7 | 50.5 | 53.0 | 51.0 | 52.2 | 48.1 | 54.8 | 54.2 | ||||||||
    SD SD | 9.5 | 9.3* | 9.7 | 10.3 | 7.7 | 10.0* | 8.6 | 8.6 | ||||||||
| Physical well-being | ||||||||||||||||
    Mean Mean | 19.5 | 17.8 | 19.9 | 18.8 | 21.3 | 14.5 | 20.4 | 20.2 | ||||||||
    SD SD | 6.1 | 5.1* | 4.7 | 5.7 | 5.4 | 7.8* | 5.6 | 5.3 | ||||||||
| Functional well-being | ||||||||||||||||
    Mean Mean | 15.9 | 16.3 | 17.2 | 16.2 | 16.2 | 13.2 | 15.9 | 17.9 | ||||||||
    SD SD | 5.5 | 5.4* | 5.5 | 6.6 | 6.1 | 7.7* | 6.9 | 4.8 | ||||||||
| Individual item analysis† | ||||||||||||||||
    Good appetite Good appetite | 29.4 | 10 | 33.3 | 9 | 5.9 | 1 | 16.7 | 1 | 44.1 | 15 | 65.2 | 15‡ | 20.0 | 4 | 9.1 | 1 |
    Nausea Nausea | 8.8 | 3 | 11.1 | 3 | 5.9 | 1 | 16.7 | 1 | 5.9 | 2 | 30.4 | 7 | 0 | 0 | 0 | 0 |
    Weight loss Weight loss | 29.4 | 10 | 14.8 | 4 | 11.8 | 2 | 50.0 | 3 | 23.5 | 8 | 39.1 | 9 | 20.0 | 4 | 27.3 | 3 |
    Diarrhea Diarrhea | 5.9 | 2 | 14.8 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 13.0 | 3 | 10.0 | 2 | 18.2 | 2 |
    Constipation Constipation | 20.6 | 7 | 14.8 | 4 | 5.9 | 1 | 0 | 0 | 14.7 | 5 | 17.4 | 4 | 5.0 | 1 | 18.2 | 2 |
    Abdominal swelling or cramps Abdominal swelling or cramps | 5.9 | 2 | 0 | 0 | 17.6 | 3 | 16.7 | 1 | 8.8 | 3 | 17.4 | 4‡ | 5.0 | 1 | 9.1 | 1 |
    Abdominal pain Abdominal pain | 44.1 | 15‡ | 7.4 | 2 | 23.5 | 4 | 50.0 | 3 | 17.6 | 6 | 21.7 | 5 | 5.0 | 1 | 9.1 | 1 |
    Fatigue Fatigue | 26.5 | 9 | 55.6 | 15 | 29.4 | 5 | 16.7 | 1 | 29.4 | 10 | 65.2 | 15 | 30.0 | 6 | 18.2 | 2 |
    Bothered by treatment side effects Bothered by treatment side effects | 0 | 0 | 14.8 | 4 | 0 | 0 | 16.7 | 1 | 0 | 0 | 43.5 | 10‡ | 20.0 | 4 | 27.3 | 3 |
Abbreviations: FACT-Hep, Functional Assessment of Cancer Therapy–Hepatobiliary; HRQOL, health-related quality of life; QOL, quality of life; SD, standard deviation.
Dose Intensity
A median number of three cycles of gemcitabine were administered in both arms, with 30% of patients in arm A and 29% of patients in arm B completing all of the planned cycles of chemotherapy, (including after induction). Dose reductions occurred in 43% and 38% of patients in arms A and B, respectively. The average mean radiation dose administered to patients in arm B was 45.9 Gy (range, 14.4 to 50.4 Gy). Eight patients received less than 45 Gy. Mean treatment time for the patients receiving radiation was 5.5 weeks (range, 2 to 8.3 weeks). Twenty-one patients completed postinduction chemotherapy without overt increased toxicity with the additional gemcitabine after gemcitabine plus radiation therapy.
Response Rate and Survival
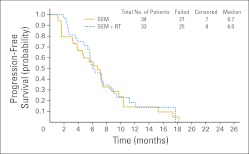
Response rates (RECIST) were determined by post-therapy CT scans. Progression was determined by radiographic findings or clinical deterioration (eg, marked decline in performance status, increased pain, severe weight loss). The overall rates for objective response (complete plus partial responses) and stable disease (no progression within 3 months) for arm A were 5% and 35% and for arm B 6% and 68%, respectively. Median PFS was 6.7 and 6 months for arms A and B, respectively (Fig 1). Of note, 46% and 21% of patients in arms A and B, respectively, did not have scans performed at adequate intervals to appropriately assess response duration. In retrospect, comparison of PFS was compromised; precise measurement of tumor size was difficult in many patients, because margins were often obscured by local inflammatory processes. Local recurrences were at the documented first site of metastasis in 11 and four patients in arms A and B, respectively (not statistically significant [Fisher's exact test]). Only two patients in arm B had metastatic disease at first measurement after induction therapy.
OS is shown in Figure 2. Median survival was 9.2 months (95% CI, 7.9 to 11.4 months) for arm A and 11.1 months (95% CI, 7.6 to 15.5 months) for arm B (one-sided P value = .017 by stratified log-rank test). Given the prespecified type I error of 2.5% of the study, the associated P value is considered positive. When we compared OS and PFS within subsets of patients, there were no statistically significant treatment differences by sex or age. In addition, age- and sex-by-treatment interactions were not significant for either OS or PFS in the multivariate Cox model. Survival time for both arms measured at 6-month intervals is shown in Figure 2.
DISCUSSION
Underpowered randomized trials conducted by cooperative groups in the United States and Europe have produced conflicting results regarding the role of radiation for patients with locally advanced pancreatic cancer. Furthermore, these trials have typically used fluoropyrimidine-based chemotherapy, with radiation dosages and schedules not considered adequate by today's standards. Preclinical data support marked radiosensitization with gemcitabine in various human cancer cell lines (including pancreatic), later evaluated in the clinic.7–16,20–23 These latter trials have typically been conducted in patients with unresectable disease using conventional or rapid fractionation radiotherapy with varying schedules of gemcitabine-based therapies.6–19,24–34 Response rates have ranged from 12% to 40%, and median survival times have ranged from 8 to 18.7 months. Toxicity has varied, but it seems proportional to the extent of radiotherapy fields.23 A lead-in period of chemotherapy alone (eg, 2 months) before chemoradiotherapy in locally advanced disease may result in selection of those patients with subclinical metastatic disease, as currently being evaluated in the LAP 07 (Locally Advanced Pancreatic Cancer 07) trial lead by Louvet et al.35
To our knowledge, this is the first prospective randomized trial to evaluate the best single agent in the disease (ie, gemcitabine) plus concurrent radiotherapy in unresectable pancreatic cancer and demonstrate an improvement in OS. The cost of this survival advantage was greater grade 4 toxicity in the radiotherapy arm but similar total grades 3 and 4 toxicities. The strength of this study was that actual, rather than estimated, survival was used. The major limitation of this trial was the failure to reach the planned accrual goals, although statistical difference for the primary end point of survival was reached. A variety of explanations for this exist, including preconceived notions of excessive toxicity; omission or use of radiotherapy being considered unethical, or a general reluctance to randomly assign patients to trials that did not include radiation in both arms.
Our results are consistent with those of other contemporaneous cooperative group studies. In a number of recent randomized clinical trials evaluating gemcitabine-based chemotherapy alone, patients with locally advanced disease had median survival durations of between 9.1 and 9.9 months.36,37 Additionally, median survival (between 11.3 and 11.9 months) was achieved in the last three phase II Radiation Therapy Oncology Group trials evaluating fractionated chemoradiotherapy.38,39 The lack of difference in PFS may be in part secondary to study design, because the primary end point was survival. CTs were performed at 8 weeks and completion of chemotherapy so as to mirror what was done in clinical practice.
For patients with locally advanced disease, radiation therapy when administered with concurrent gemcitabine seems to be an important component of first-line therapy without significant adverse effects on QOL or serious toxicities. Because no patient in either arm sustained durable disease-free survival, this trial further emphasizes that more novel approaches with improved systemic therapy tested in large populations are needed for the treatment of locally advanced pancreatic cancer.
Footnotes
See accompanying editorial on page 4066
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: Al B. Benson III, Eli Lilly (C) Stock Ownership: None Honoraria: Patrick Flynn, Eli Lilly; Christopher H. Crane, Varian Medical Systems Research Funding: Patrick J. Loehrer Sr, Eli Lilly Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Patrick J. Loehrer Sr, Higinia Cardenes, Lynne Wagner, Joanna M. Brell, David Cella, Patrick Flynn, Ramesh K. Ramanathan, Christopher H. Crane, Steven R. Alberts,Al B. Benson III
Administrative support: Al B. Benson III
Provision of study materials or patients: Patrick J. Loehrer Sr, Higinia Cardenes, Joanna M. Brell, Patrick Flynn, Al B. Benson III
Collection and assembly of data: Patrick J. Loehrer Sr, Yang Feng, Al B. Benson III
Data analysis and interpretation: Patrick J. Loehrer Sr, Yang Feng, Higinia Cardenes, Lynne Wagner, Al B. Benson III
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
Articles from Journal of Clinical Oncology are provided here courtesy of American Society of Clinical Oncology
Full text links
Read article at publisher's site: https://doi.org/10.1200/jco.2011.34.8904
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc3525836?pdf=render
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1200/jco.2011.34.8904
Article citations
Stereotactic Radiotherapy Plus Nivolumab in Patients with Locally Advanced Pancreatic Cancer: Results from Phase 1/2 Clinical CA209-9KH Trial.
Oncol Ther, 12(4):817-831, 23 Oct 2024
Cited by: 0 articles | PMID: 39441483
Sharing Mono-Institutional Experience of Treating Pancreatic Cancer with Stereotactic Body Radiation Therapy (SBRT).
Curr Oncol, 31(10):5974-5986, 04 Oct 2024
Cited by: 0 articles | PMID: 39451750 | PMCID: PMC11506591
Consensus, debate, and prospective on pancreatic cancer treatments.
J Hematol Oncol, 17(1):92, 10 Oct 2024
Cited by: 0 articles | PMID: 39390609 | PMCID: PMC11468220
Review Free full text in Europe PMC
Survival benefits of radiotherapy in locally advanced unresectable and metastatic pancreatic cancer: a single-institution cohort and SEER database analysis.
Front Oncol, 14:1473251, 16 Sep 2024
Cited by: 0 articles | PMID: 39359428 | PMCID: PMC11445777
The Role of Tumor Microenvironment in Pancreatic Cancer Immunotherapy: Current Status and Future Perspectives.
Int J Mol Sci, 25(17):9555, 03 Sep 2024
Cited by: 0 articles | PMID: 39273502 | PMCID: PMC11395109
Review Free full text in Europe PMC
Go to all (454) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Gemcitabine alone or with cisplatin for the treatment of patients with locally advanced and/or metastatic pancreatic carcinoma: a prospective, randomized phase III study of the Gruppo Oncologia dell'Italia Meridionale.
Cancer, 94(4):902-910, 01 Feb 2002
Cited by: 244 articles | PMID: 11920457
Postoperative adjuvant gemcitabine and concurrent radiation after curative resection of pancreatic head carcinoma: a phase II study.
Int J Radiat Oncol Biol Phys, 56(4):974-980, 01 Jul 2003
Cited by: 33 articles | PMID: 12829132
Randomized phase III trial of gemcitabine plus cisplatin compared with gemcitabine alone in advanced pancreatic cancer.
J Clin Oncol, 24(24):3946-3952, 01 Aug 2006
Cited by: 403 articles | PMID: 16921047
Gemcitabine Compared With Gemcitabine and S-1 Combination Therapy in Advanced Pancreatic Cancer: A Systematic Review and Meta-Analysis.
Medicine (Baltimore), 94(35):e1345, 01 Sep 2015
Cited by: 6 articles | PMID: 26334891 | PMCID: PMC4616522
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NCI NIH HHS (1)
Grant ID: P30 CA082709
NCRR NIH HHS (1)
Grant ID: UL1 RR025741